Cessation of Care for Frail Older Adults: Physical, Psychological and Economic Outcomes for Family Carers
Abstract
1. Introduction
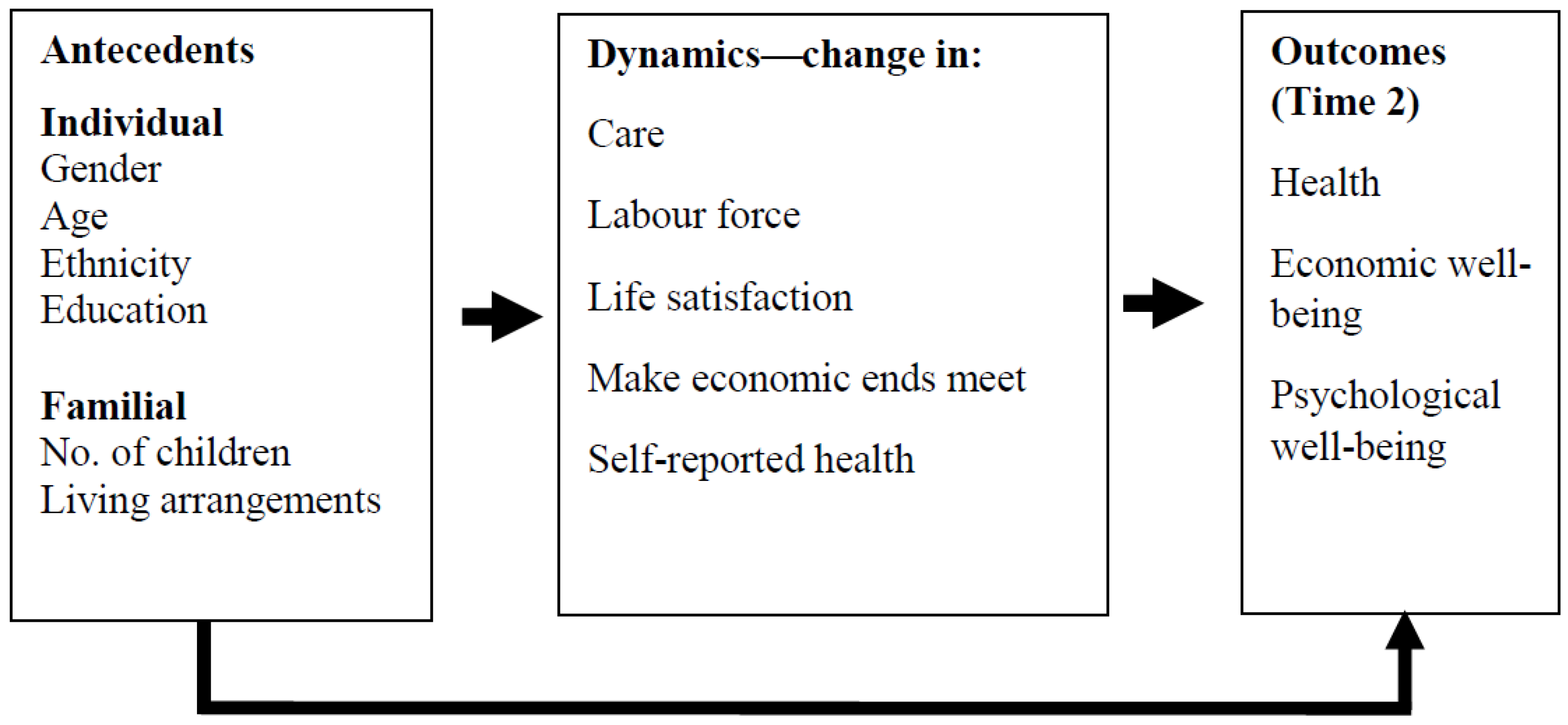
2. Conceptual Framework
3. Elders and Families in Israel
4. Methods
4.1. Data Source and Study Sample
4.2. Research Variables
4.2.1. Dependent Variables
- (a)
- State of health—self-rated health (1 = very bad, to 5 = excellent);
- (b)
- An economic variable—subjective evaluation of household economic wellbeing: making ends meet (1 = with great difficulty to 4 = easily);
- (c)
- Psychological wellbeing—life satisfaction (0 = not at all satisfied to 10 = very satisfied).
4.2.2. Explanatory Variables
- (a)
- ‘Stop giving care’ (cessation of care): 0 = helped an older family member at both Time 1 and Time 2; 1 = helped an older family member at Time 1 and stopped care at Time 2.
- (b)
- Socio-demographic attributes: age, gender (0 = female, 1 = male), living arrangements (0 = living alone, 1 = living with others), children (0 = none, 1 = having), years of education, and ethnicity (0 = Jewish, 1 = Arab). Data regarding all socio-demographic explanatory variables were harvested from Time 1 only.
- (c)
- Interaction variables between the different socio-demographic attributes and cessation-of-care opportunities were also included. This allowed us to identify the combined effect of the two variables on each of the research variables in the model, yielding a subjective picture of the care process before it began, when it was in place, and after it was over.
- (d)
- Changes in carers’ labor force participation between the caregiving period and the cessation-of-care period (−1 = left labor force, 0 = no change, 1 = enter labor force).
- (e)
- Changes in the aforementioned dependent variables (self-rated health, life satisfaction, making ends meet) between the caregiving period and the cessation-of-care period, a higher score signifying a positive change.
5. Results
6. Discussion
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Bengtson, V.L.; Giarrusso, R.; Mabry, J.B.; Silverstein, M. Solidarity, conflict, and ambivalence: Complementary or competing perspectives on intergenerational relationships? J. Marriage Fam. 2002, 64, 568–576. [Google Scholar] [CrossRef]
- World Health Organization. Active Aging: A Policy Framework; WHO: Geneva, Switzerland, 2002. [Google Scholar]
- Ben-David, N.; Halperin, D.; Katz, R.; Lowenstein, A.; Tur-Sinai, A. A method for estimating the participation rate of elder care. Theor. Econ. Lett. 2016, 6, 474–479. [Google Scholar] [CrossRef][Green Version]
- Caserta, M.S.; Utz, R.L.; Lund, D.A. Spousal bereavement following cancer death. Illn. Crisis Loss 2013, 21, 185–202. [Google Scholar] [CrossRef] [PubMed]
- Schulz, R.; Eden, J. National Academies of Sciences, Engineering, and Medicine. Economic impact of family caregiving. In Families Caring for an Aging America; National Academies Press (US): Washington, DC, USA, 2016. [Google Scholar]
- Biggs, S.; Lowenstein, A. Toward generational Intelligence: Linking cohorts, families and experience. In Cohorts, Families, and Experience; Silverstein, M., Ed.; John Hopkins University Press: Baltimore, MD, USA, 2011. [Google Scholar]
- Guberman, N.; Lavoie, J.-P.; Blein, L.; Olazabal, I. Baby boom caregivers: Care in the age of individualization. Gerontologist 2012, 52, 210–218. [Google Scholar] [CrossRef] [PubMed]
- Lowenstein, A.; Katz, R.; Gur-Yatish, N. Cross-national variations in elder care: Antecedents and outcomes. In Caregiving Contexts: Cultural, Familial, and Societal Implications; Szinovacz, M.E., Davey, A., Eds.; Springer Publishing Company: New York, NY, USA, 2008; pp. 93–114. [Google Scholar]
- Szinovacz, M.E. Children in caregiving families. In Caregiving Contexts: Cultural, Familial, and Societal Implications; Szinovacz, M.E., Davey, A., Eds.; Springer Publishing Company: New York, NY, USA, 2008; pp. 161–190. [Google Scholar]
- Lee, Y.; Tang, F.; Kim, K.H.; Albert, S.M. Exploring gender differences in the relationships between eldercare and labor force participation. Can. J. Aging 2015, 34, 14–25. [Google Scholar] [CrossRef] [PubMed]
- Choi, H.; Marks, N. Transition to caregiving, marital disagreement, and psychological wellbeing: A prospective US national study. J. Fam. Issues 2006, 27, 1701–1722. [Google Scholar] [CrossRef]
- Lau, K.M.; Au, A. Correlates of informal caregiver distress in Parkinson’s disease: A meta-analysis. Clin. Gerontol. 2011, 34, 117–131. [Google Scholar] [CrossRef]
- Larkin, M. Life after caring: The post caring experiences of former carers. Br. J. Soc. Work 2009, 39, 1026–1042. [Google Scholar] [CrossRef]
- Nolan, M.R.; Davies, S.; Brown, J.; Keady, J.; Nolan, J. Beyond ‘person-centred’care: A new vision for gerontological nursing. J. Clin. Nurs. 2004, 13, 45–53. [Google Scholar] [CrossRef]
- Montgomery, R.; Kosloski, K. Caregiving as a process of changing identity: Implications for caregiver support. Generations 2009, 33, 47–52. [Google Scholar]
- Hegland, M.E. Aging and the elderly: Diminishing family care systems and need for alternatives. In The Routledge Handbook of Islam and Gender; Routledge: London, UK, 2020; pp. 358–374. [Google Scholar]
- Crespo, M.; Piccini, A.T.; Bernaldo-de-Quiros, M. When the care ends: Emotional state of Spanish bereaved caregivers of persons with Dementia. Span. J. Psychol. 2013, 16, 1–8. [Google Scholar] [CrossRef]
- Kenny, P.; King, M.T.; Hall, J. The physical functioning and mental health of informal carers: Evidence of care-giving impacts from an Australian population-based cohort. Health Soc. Care Community 2014, 22, 646–659. [Google Scholar] [CrossRef]
- Thomas, G.P.A.; Saunders, C.L.; Roland, M.O.; Paddison, C.A.M. Informal carers’ health-related quality of life and patient experience in primary care: Evidence from 195,364 carers in England responding to a national survey. BMC Fam. Pract. 2015, 16, 62–71. [Google Scholar] [CrossRef]
- Silverstein, M.; Parrott, T.M. Attitudes toward government policies that assist informal caregivers: The link between personal troubles and public issues. Res. Aging 2001, 23, 349–374. [Google Scholar] [CrossRef]
- Uhlenberg, P.; Cheuk, M. Demographic change and the future of informal caregiving. In Caregiving Contexts: Cultural, Familial, and Societal Implications; Szinovacz, M.E., Davey, A., Eds.; Springer Publishing Company: New York, NY, USA, 2008; pp. 9–33. [Google Scholar]
- United Nations. World Population Ageing 2007; United Nations: New York, NY, USA, 2007. [Google Scholar]
- Pickard, L. A growing care gap? The supply of unpaid care for older people by their adult children in England to 2032. Ageing Soc. 2015, 35, 96–123. [Google Scholar] [CrossRef]
- Cavaye, J.; Watts, J.H. Former carers: Issues from the literature. Fam. Relatsh. Soc. 2018, 7, 141–157. [Google Scholar] [CrossRef]
- Orzeck, P.; Silverman, M. Recognizing post-caregiving as part of the caregiving career: Implications for practice. J. Soc. Work Pract. 2008, 22, 211–220. [Google Scholar] [CrossRef]
- McDonald, L.; Donahue, P.; Moore, B. The Economic Casualties of Retiring to Caregive; McMaster University: Hamilton, Canada, 1998. [Google Scholar]
- Cronin, P.; Hynes, G.; Breen, M.; McCarron, M.; McCallion, P.; O’Sullivan, L. ‘Between worlds’: The experiences and needs of former family carers. Health Soc. Care Community 2015, 23, 88–96. [Google Scholar] [CrossRef] [PubMed]
- Zarit, S.H.; Pearlin, L.I.; Schaie, K.W. (Eds.) Caregiving Systems: Informal and Formal Helpers; Psychology Press: New York, NY, USA, 1993. [Google Scholar]
- Ume, E.P.; Evans, C.B. Chaos and uncertainty: The post-caregiving transition. Geriatr. Nurs. 2011, 32, 288–294. [Google Scholar] [CrossRef] [PubMed]
- Roberts, R.E.L.; Bengtson, V.L. Intergenerational cohesion and psychic well-being: Implications over the adult life course. In Proceedings of the Annual Meeting of the American Sociological Association, San Francisco, CA, USA, 24–28 August 1988. [Google Scholar]
- Rossi, A.S. Intergenerational relations: Gender, norms, and behavior. In The Changing Contract across Generations; Publisher: Piscataway, NJ, USA, 1993; pp. 191–212. [Google Scholar]
- Bengtson, V.L. Beyond the nuclear family: The increasing importance of multigenerational bonds: The burgess award lecture. J. Marriage Fam. 2001, 63, 1–16. [Google Scholar] [CrossRef]
- Lowenstein, A.; Katz, R.; Tur-Sinai, A. Intergenerational family relationships and successful aging. In The Cambridge Handbook of Successful Aging; Fernandez-Ballesteros, R., Robine, J.M., Benetos, A., Eds.; Cambridge University Press: Cambridge, UK, 2019; pp. 455–474. [Google Scholar]
- McChesney, K.Y.; Bengtson, V.L. Solidarity, Integration, and Cohesion in Families: Concepts and Theories; Sage Publications, Inc.: Thousand Oaks, CA, USA, 1988. [Google Scholar]
- Roberts, R.E.; Bengtson, V.L. Is intergenerational solidarity a unidimensional construct? A second test of a formal model. J. Gerontol. 1990, 45, S12–S20. [Google Scholar] [CrossRef] [PubMed]
- Bengtson, V.L.; Schrader, S.S. Parent-child relations. Res. Instrum. Soc. Gerontol. 1982, 2, 115–186. [Google Scholar]
- Katz, R.; Lowenstein, A.; Phillips, J.; Daatland, S.O.; Bengtson, V.L.; Acock, A.C.; Allen, K.R.; Anderson, P.D.; Klein, D.M. Theorizing Intergenerational family relations: Solidarity, conflict and ambivalence in cross-national contexts. In Sourcebook of Family Theory & Research; Bengtson, L., Ed.; Sage Publications: Thousand Oaks, CA, USA, 2005; pp. 393–407. [Google Scholar]
- Silverstein, M.; Chen, X.; Heller, K. Too much of a good thing? Intergenerational social support and the psychological well-being of older parents. J. Marriage Fam. 1996, 58, 970–982. [Google Scholar] [CrossRef]
- Katz, R.; Lowenstein, A.; Halperin, D.; Tur-Sinai, A. Generational Solidarity in Europe and Israel. Can. J. Aging/La Rev. Can. Du Vieil. 2015, 34, 342–355. [Google Scholar] [CrossRef] [PubMed]
- Lowenstein, A. Intergenerational solidarity: Strengthening economic and social ties. In Background Paper, Department of Economic and Social Affairs Division for Social Policy and Development; United Nations Headquarters: New York, NY, USA, 2007. [Google Scholar]
- Szydlik, M. Sharing Lives: Adult Children and Parents; Routledge: New York, NY, USA, 2018. [Google Scholar]
- Katz, R.; Lavee, Y. Families in Israel. In Handbook of World Families; Adams, B.N., Trost, J., Eds.; Sage Publications: Thousand Oaks, CA, USA, 2005; pp. 486–506. [Google Scholar]
- Katz, R.; Lowenstein, A. Solidarity between generations and elders’ life satisfaction: Comparing Jews and Arabs in Israel. J. Intergener. Relatsh. 2012, 10, 5–21. [Google Scholar] [CrossRef]
- Lowenstein, A.; Katz, R. Intergenerational family relations in the multi-cultural society of Israel: Editorial Comments. J. Intergener. Relat. 2015, 13, 1–5. [Google Scholar]
- Carmel, S. Prologue—Aging in Israel: Demographic changes, societal adaptation and remaining challenges. In Aging in Israel—Research, Policy and Practice; Carmel, S., Ed.; Transaction Publishers: New Brunswick, NJ, USA, 2010; pp. 3–23. [Google Scholar]
- Brodsky, J.; Shnoor, Y.; Be’er, S. The Elderly in Israel: Statistical Abstract 2016; Myers-JDC-Brookdale Institute (Hebrew): Jerusalem, Israel, 2017. [Google Scholar]
- Silverstein, M.; Lowenstein, A.; Katz, R.; Gans, D.; Fan, Y.-K.; Oyama, P. Intergenerational support and the emotional well-being of older Jews and Arabs in Israel. J. Marriage Fam. 2014, 75, 950–963. [Google Scholar] [CrossRef] [PubMed]
- Azaiza, F. The perception and utilization of social support in times of cultural change: The case of Arabs in Israel. Int. J. Soc. Welf. 2008, 17, 198–203. [Google Scholar] [CrossRef]
- Khalaila, R.; Litwin, H. Modernization and future care preferences: A crosssectional survey of Arab Israeli caregivers. J. Adv. Nurs. 2011, 67, 1614–1624. [Google Scholar] [CrossRef]
- Litwin, H.; Zoabi, S. Modernization and elder abuse in an Arab-Israeli context. In Aging in Israel: Research, Policy & Practice; Carmel, S., Ed.; Transaction Publisher: London, UK, 2010; pp. 357–396. [Google Scholar]
- Sharabi, M.; Shdema, I.; Abboud-Armaly, O. Nonfinancial employment commitment among Muslims and Jews in Israel: Examination of the core–periphery model on majority and minority groups. Empl. Relat. Int. J. 2020, 43, 227–243. [Google Scholar] [CrossRef]
- Halperin, D. Aging, families and preferences for care among old Jews and Arabs. Isr. Stud. Rev. 2013, 28, 102–121. [Google Scholar]
- Halperin, D. Intergenerational relations: The view of older Jews and Arabs. J. Intergener. Relatsh. 2015, 13, 51–74. [Google Scholar] [CrossRef]
- Achdut, L.; Tur-Sinai, A.; Troitsky, R. Transitions among States of Labor Force Participation in the Old Age. Eur. J. Ageing 2015, 12, 39–49. [Google Scholar] [CrossRef] [PubMed]
- Dwolatzky, T.; Brodsky, J.; Azaiza, F.; Clarfield, A.M.; Jacobs, J.M.; Litwin, H. Coming of age: Health-care challenges of an ageing population in Israel. Lancet 2017, 389, 2542–2550. [Google Scholar] [CrossRef]
- Israel Central Bureau of Statistics. Complete Life Tables of Israel 2015–2019; Central Bureau of Statistics: Jerusalem, Israel, 2021. [Google Scholar]
- Casanova, G.; Tur-Sinai, A.; Lamura, G. Innovating long-term care provision in Mediterranean welfare states: A comparison between Italy and Israel. J. Aging Soc. Policy 2020, 32, 55–82. [Google Scholar] [CrossRef] [PubMed]
- Lowenstein, A.; Katz, R.; Daatland, S. Filial norms and intergenerational support in a comparative cross-national perspective. In Annual Review of Gerontology and Geriatrics; Silverstein, M., Ed.; Springer: New York, NY, USA, 2004. [Google Scholar]
- Asiskovitch, S. The Long-Term Care Insurance Program in Israel: Solidarity with the elderly in a changing society. Isr. J. Health Policy Res. 2013, 2, 1–19. [Google Scholar] [CrossRef] [PubMed]
- Lowenstein, A.; Katz, R. Family and age in a global perspective. In Sage Handbook of Social Gerontology; Dannefer, D., Phillipson, C., Eds.; Sage Publications: London, UK, 2010; pp. 190–202. [Google Scholar]
- Börsch-Supan, A.; Brandt, M.; Hunkler, C.; Kneip, T.; Korbmacher, J.; Malter, F.; Zuber, S. Data resource profile: The Survey of Health, Ageing and Retirement in Europe (SHARE). Int. J. Epidemiol. 2013, 42, 992–1001. [Google Scholar] [CrossRef] [PubMed]
- Carmel, S.; Tur-Sinai, A. Cognitive decline among European retirees: Impact of early retirement, nation-related and personal characteristics. Ageing Soc. 2021, 1–27. [Google Scholar] [CrossRef]
- Tur-Sinai, A.; Soskolne, V. Socioeconomic status and health behaviors as predictors of changes in self-rated health among older persons in Israel. Health Soc. Care Community 2021, 29, 1461–1472. [Google Scholar] [CrossRef]
- Tur-Sinai, A.; Spivak, A. How generous are societies toward their elderly? A European comparative study of replacement rates, well-being and economic adequacy. Soc. Indic. Res. 2021. [Google Scholar] [CrossRef]
- Tur-Sinai, A.; Lewin-Epstein, N. Transitions in giving and receiving intergenerational financial support in middle and old age. Soc. Indic. Res. 2020, 150, 765–791. [Google Scholar] [CrossRef]
- Hocking, R.R. A Biometrics invited paper. The analysis and selection of variables in linear regression. Biometrics 1976, 32, 1–49. [Google Scholar] [CrossRef]
- Draper, N.; Smith, H. Applied Regression Analysis, 2nd ed.; John Wiley & Sons: New York, NY, USA, 1981. [Google Scholar]
- Chernichovsky, D.; Bisharat, B.; Bowers, L.; Brill, A.; Sharony, C. The Health of the Arab Israeli Population; Taub Center for Social Policy Studies in Israel: Jerusalem, Israel, 2017. [Google Scholar]
- Tur-Sinai, A.; Magnezi, R.; Grinvald-Fogel, H. Assessing the determinants of healthcare expenditure in single-person households. Isr. J. Health Policy Res. 2018, 7, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Tur-Sinai, A.; Kolobov, T.; Tesler, R.; Baron-Epel, O.; Dvir, K.; Harel-Fisch, Y. Associations between socioeconomic and family determinants and weight-control behaviours among adolescents. Int. J. Public Health 2020, 65, 1689–1698. [Google Scholar] [CrossRef] [PubMed]
- Seltzer, M.M.; Li, L.W. The dynamics of caregiving: Transitions during a three-year prospective study. Gerontologist 2000, 40, 165–178. [Google Scholar] [CrossRef] [PubMed]
- Silverstein, M.; Conroy, S.J.; Wang, H.; Giarrusso, R.; Bengtson, V.L. Reciprocity in parent–child relations over the adult life course. J. Gerontol. Ser. B Psychol. Sci. Soc. Sci. 2002, 57, S3–S13. [Google Scholar] [CrossRef] [PubMed]
- Lowenstein, A.; Katz, R. Rural Arab families coping with caregiving. Marriage Fam. Rev. 2000, 30, 179–197. [Google Scholar] [CrossRef]
- Lyons, J.G.; Cauley, J.A.; Fredman, L. The effect of transitions in caregiving status and intensity on perceived stress among 992 female caregivers and noncaregivers. J. Gerontol. Med. Sci. 2015, 70, 1018–1023. [Google Scholar] [CrossRef] [PubMed]
- Van Groenou, M.I.B.; De Boer, A. Providing informal care in a changing society. Eur. J. Ageing 2016, 13, 271–279. [Google Scholar] [CrossRef] [PubMed]
- Bauer, J.M.; Sousa-Poza, A. Impacts of Informal Caregiving on Caregiver Employment, Health, and Family. IZA Discussion Papers, No. 8851. 2015. Available online: http://hdl.handle.net/10419/110154 (accessed on 15 February 2022).
- Carmichael, F.; Ercolan, M. Unpaid caregiving and paid work over life-courses: Different pathways, diverging outcomes. Soc. Sci. Med. 2016, 156, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Pei, X.; Luo, H.; Lin, Z.; Keating, N.; Fast, J. The impact of eldercare on adult children’s health and employment in transitional China. J. Cross-Cult. Gerontol. 2017, 32, 357–372. [Google Scholar] [CrossRef] [PubMed]
- Jenkinson, A. Past Caring: The Beginning and Not the End; Polperro Heritage Press: Leominster, MA, USA, 2004. [Google Scholar]

| Distribution of Informal Care Recipients | Type of Informal Care Provided | |||
|---|---|---|---|---|
| Personal Care | Practical Household Help | Help with Paperwork | ||
| Mother/mother-in-law | 73.9 | 60.0 | 74.8 | 76.0 |
| Father/father in-law | 17.5 | 23.7 | 16.9 | 15.7 |
| Spouse/partner/siblings | 8.6 | 16.3 | 8.3 | 8.3 |
| Total | 100.0 | 100.0 | 100.0 | 100.0 |
| Time 1—Giving; Time 2—Not Giving | Time 1—Giving; Time 2—Giving | F/χ2 | ||
|---|---|---|---|---|
| Dependent variables | ||||
| Self-reported health (mean) | 2.57 | 3.11 | 10.12 *** | |
| −1.13 | −1.04 | |||
| Household makes ends meet (mean) | 2.62 | 2.83 | 1.37 | |
| −1.04 | −0.99 | |||
| Life satisfaction (mean) | 6.79 | 7.85 | 6.32 *** | |
| −3.25 | −1.94 | |||
| Explanatory variables | ||||
| Age (mean) | 67.83 | 64.15 | 10.91 *** | |
| −10.10 | −7.52 | |||
| Gender (pct.) | Female | 58.21 | 56.24 | 0.07 |
| Male | 41.79 | 43.76 | ||
| Living Status (pct.) | Living alone | 24.26 | 25.39 | 0.16 |
| Living with someone | 75.74 | 74.61 | ||
| Children (pct.) | No | 4.37 | 5.83 | 0.13 |
| Yes | 95.63 | 94.17 | ||
| Ethnicity | Jews | 79.11 | 81.14 | 0.00 |
| Non-Jews | 20.89 | 18.86 | ||
| Education (mean) | 12.76 | 13.77 | 2.11 | |
| −4.23 | −4.33 | |||
| Self-reported health—change (mean) | −0.35 | −0.34 | 0.01 | |
| −0.94 | −0.91 | |||
| Life Satisfaction—change (mean) | −0.29 | −0.09 | 1.00 | |
| −1.69 | −1.47 | |||
| Household makes ends meet—change (mean) | 0.21 | 0.28 | 0.08 | |
| −0.97 | −0.98 | |||
| Labor force (pct.) | Non-participants | 62.44 | 50.21 | 4.49 ** |
| Participants | 37.56 | 49.79 | ||
| Labor force—change (pct.) | Left labor force | 11.28 | 13.23 | 0.04 |
| No change | 86.19 | 83.92 | ||
| Enter labor force | 2.53 | 2.84 | ||
| Model 1 | Model 2 | Model 3 | Model 4 | |||||
|---|---|---|---|---|---|---|---|---|
| Odds Ratio (Std. Error) | 95% CI | Odds Ratio (Std. Error) | 95% CI | Odds Ratio (Std. Error) | 95% CI | Odds Ratio (Std. Error) | 95% CI | |
| Age | 0.961 *** (0.00) | [0.954, 0.968] | 0.962 *** (0.00) | [0.955, 0.969] | 0.963 *** (0.00) | [0.956, 0.970] | 0.967 *** (0.00) | [0.959, 0.975] |
| Male | 1.131 ** (0.07) | [1.007, 1.271] | ||||||
| Arab | 0.816 *** (0.06) | [0.701, 0.949] | 0.828 * (0.06) | [0.711, 0.964] | ||||
| Education | 1.053 *** (0.01) | [1.037, 1.068] | 1.046 *** (0.01) | [1.031, 1.062] | 1.028 *** (0.01) | [1.012, 1.043] | 1.032 *** (0.01) | [1.016, 1.048] |
| In labor force—change | 1.516 * (0.32) | [0.998, 2.303] | 1.522 * (0.33) | [0.998, 2.322] | 1.622 * (0.35) | [1.063, 2.477] | ||
| Life satisfaction—change | 1.236 *** (0.03) | [1.173, 1.303] | 1.222 *** (0.03) | [1.158, 1.290] | 1.212 *** (0.03) | [1.148, 1.279] | ||
| Make ends meet—change | 2.175 *** (0.13) | [1.933, 2.447] | 2.114 *** (0.13) | [1.872, 2.386] | 2.071 *** (0.13) | [1.834, 2.338] | ||
| Stop giving care | 1.234 *** (0.02) | [1.188, 1.282] | 1.228 *** (0.02) | [1.182, 1.275] | ||||
| Age*Stop giving care | 0.975 *** (0.01) | [0.961, 0.989] | ||||||
| Children*Stop giving care | 3.109 * (1.53) | [1.185, 8.158] | ||||||
| Log-likelihood | −5419.8506 | −5291.3720 | −4975.1555 | −4958.6279 | ||||
| N | 1471 | 1462 | 1282 | 1282 | ||||
| Model1 | Model 2 | Model 3 | Model 4 | |||||
|---|---|---|---|---|---|---|---|---|
| Odds Ratio (Std. Error) | 95% CI | Odds Ratio (Std. Error) | Odds Ratio (Std. Error) | Odds Ratio (Std. Error) | 95% CI | Odds Ratio (Std. Error) | 95% CI | |
| Male | 1.166 ** (0.07) | [1.035, 1.314] | 1.133 ** (0.07) | [1.005, 1.278] | 1.127 * (0.07) | [0.995, 1.277] | 1.125 (0.07) | [0.991, 1.277] |
| Arab | 0.506 *** (0.04) | [0.435, 0.588] | 0.486 *** (0.04) | [0.418, 0.566] | 0.672 *** (0.06) | [0.571, 0.790] | 0.659 *** (0.06) | [0.559, 0.777] |
| Children | 0.684 *** (0.07) | [0.553, 0.847] | 0.716 *** (0.08) | [0.577, 0.888] | 0.726 *** (0.08) | [0.581, 0.907] | 0.717 ** (0.08) | [0.574, 0.896] |
| Education | 1.135 *** (0.01) | [1.118, 1.152] | 1.146 *** (0.01) | [1.129, 1.163] | 1.117 *** (0.01) | [1.100, 1.135] | 1.109 *** (0.01) | [1.091, 1.128] |
| Life satisfaction—change | 1.514 *** (0.07) | [1.382, 1.658] | 1.407 *** (0.07) | [1.280, 1.547] | 1.484 *** (0.12) | [1.265, 1.741] | ||
| Stop giving care | 1.456 *** (0.03) | [1.399, 1.516] | 1.459 *** (0.03) | [1.401, 1.519] | ||||
| Age*Stop giving care | 0.982 *** (0.00) | [0.972, 0.992] | ||||||
| Education*Stop giving care | 1.110 *** (0.03) | [1.061, 1.161] | ||||||
| Log-likelihood | −4670.9813 | −4611.5884 | −4196.3078 | −4185.505 | ||||
| N | 1475 | 1463 | 1283 | 1283 | ||||
| Model 1 | Model 2 | Model 3 | Model 4 | |||||
|---|---|---|---|---|---|---|---|---|
| Coefficient (Std. Error) | 95% CI | Coefficient (Std. Error) | 95% CI | Coefficient (Std. Error) | 95% CI | Coefficient (Std. Error) | 95% CI | |
| Age | −0.011 *** (0.00) | [−0.018, −0.004] | −0.009 *** (0.00) | [−0.016, −0.002] | −0.007 * (0.00) | [−0.014, 0.000] | ||
| Education | 0.061 *** (0.01) | [0.047, 0.074] | 0.061 *** (0.01) | [0.045, 0.074] | 0.064 *** (0.01) | [0.050, 0.077] | 0.054 *** (0.01) | [0.040, 0.068] |
| Arab | 0.369 *** (0.07) | [0.231, 0.506] | 0.364 *** (0.07) | [0.227, 0.501] | 0.384 *** (0.07) | [0.247, 0.520] | 0.360 *** (0.07) | [0.226, 0.494] |
| Make ends meet—change | 0.085 ** (0.04) | [0.016, 0.154] | 0.097 *** (0.04) | [0.029, 0.166] | 0.076 * (0.03) | [0.009, 0.144] | ||
| Self-rated health—change | 0.099 *** (0.03) | [0.040, 0.158] | 0.092 *** (0.03) | [0.033, 0.150] | 0.094 ** (0.03) | [0.036, 0.152] | ||
| Stop giving care | −0.485 *** (0.11) | [−0.691, −0.278] | −0.325 * (0.96) | [−0.545, −0.194] | ||||
| Age*Stop giving care | −0.083 *** (0.01) | [−0.103, −0.063] | ||||||
| Children*Stop giving care | 1.987 *** (0.54) | [0.933, 3.040] | ||||||
| Education*Stop giving care | 0.083 *** (0.02) | [0.036, 0.129] | ||||||
| Constant | 7.429 *** (0.27) | [6.906, 7.952] | 7.340*** (0.27) | [6.818, 7.862] | 7.178 *** (0.27) | [6.653, 7.703] | 6.884 *** (0.10) | [6.683, 7.084] |
| R2-Adjusted | 0.0329 | 0.0360 | 0.0411 | 0.0677 | ||||
| N | 1474 | 1461 | 1461 | 1461 | ||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tur-Sinai, A.; Halperin, D.; Ben David, N.; Lowenstein, A.; Katz, R. Cessation of Care for Frail Older Adults: Physical, Psychological and Economic Outcomes for Family Carers. Int. J. Environ. Res. Public Health 2022, 19, 3570. https://doi.org/10.3390/ijerph19063570
Tur-Sinai A, Halperin D, Ben David N, Lowenstein A, Katz R. Cessation of Care for Frail Older Adults: Physical, Psychological and Economic Outcomes for Family Carers. International Journal of Environmental Research and Public Health. 2022; 19(6):3570. https://doi.org/10.3390/ijerph19063570
Chicago/Turabian StyleTur-Sinai, Aviad, Dafna Halperin, Nissim Ben David, Ariela Lowenstein, and Ruth Katz. 2022. "Cessation of Care for Frail Older Adults: Physical, Psychological and Economic Outcomes for Family Carers" International Journal of Environmental Research and Public Health 19, no. 6: 3570. https://doi.org/10.3390/ijerph19063570
APA StyleTur-Sinai, A., Halperin, D., Ben David, N., Lowenstein, A., & Katz, R. (2022). Cessation of Care for Frail Older Adults: Physical, Psychological and Economic Outcomes for Family Carers. International Journal of Environmental Research and Public Health, 19(6), 3570. https://doi.org/10.3390/ijerph19063570







