Changes in Inequality in Use of Maternal Health Care Services: Evidence from Skilled Birth Attendance in Mauritania for the Period 2007–2015
Abstract
1. Introduction
2. Materials and Methods
2.1. Data Sources and Sample
2.2. Measuring and Decomposing Socio-Economic Inequalities in SBA
2.2.1. Measuring Inequality
2.2.2. Decomposing Inequality
- is skilled birth attendance (= 1 if birth was attended by a skilled health professional and = 0 if not)
- is a set of k explanatory variables for skilled birth attendance;
- is the regression coefficient of the explanatory variables ;
- is the error term.
2.2.3. Decomposing Changes in Inequality
2.3. Definition of Variables
2.3.1. Outcome Variable
2.3.2. Socioeconomic Indicator
2.3.3. Social Determinants of SBA
3. Results
3.1. Descriptive Statistics
3.2. Measuring Inequality
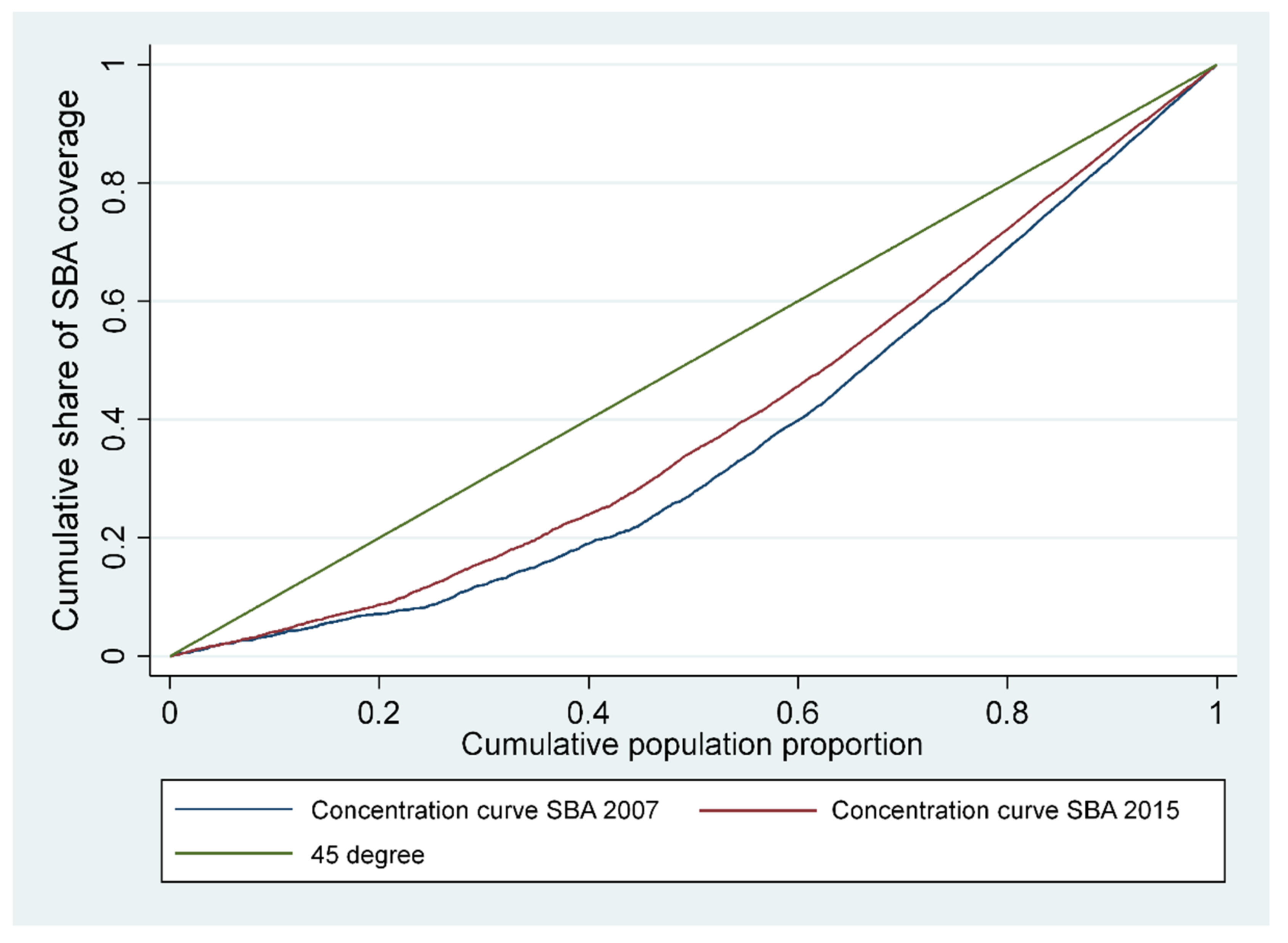
3.3. Decomposition of SBA Inequalities
3.4. Decomposing Changes in Inequality
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- National Office of Statistics. Report of the 2008 Permanent Survey of Household Living Conditions; National Office of Statistics: Nouakchott, Mauritania, 2009. (In French)
- National Office of Statistics. Report of the 2014 Permanent Survey of Household Living Conditions; National Office of Statistics: Nouakchott, Mauritania, 2015. (In French)
- World Bank. Poverty Dynamics and Social Mobility 2008–2014; World Bank: Washington, DC, USA, 2016. [Google Scholar]
- National Office of Statistics. General Census of Population and Housing 2013: Mortality; National Office of Statistics: Nouakchott, Mauritania, 2015. (In French)
- Programme des Nations Unies pour le Développement. Rapport sur le Progrès dans la Mise en œuvre des Objectifs du Millénaire pour le Développement en Mauritanie. 2008. Available online: https://www.undp.org/content/dam/undp/library/MDG/english/MDG%20Country%20Reports/Mauritania/RapportOMD2008Mauritanie.pdf (accessed on 20 July 2021).
- UNFPA; World Health Organization; UNICEF; World Bank Group; The United Nations Population Division. Trends in Maternal Mortality 2000 to 2017: Estimates by WHO, UNICEF, UNFPA, World Bank Group and the United Nations Population Division; World Health Organization: Geneva, Switzerland, 2019; Licence: CC. [Google Scholar]
- World Bank. World Bank Open Data. Available online: https://data.worldbank.org/indicator/EN.POP.DNST?locations=ZG (accessed on 20 July 2021).
- Ministry of Health. National Health Development Plan Preparation Process (2012–2020): Health Sector Situation Analysis Report; Ministry of Health: Nouakchott, Mauritania, 2011. (In French)
- Ministry of Health. Service Availability and Readiness Assessment Survey 2018; Ministry of Health: Nouakchott, Mauritania, 2019. (In French)
- Waelkens, M.P.; Coppieters, Y.; Laokri, S.; Criel, B. An in-depth investigation of the causes of persistent low membership of community-based health insurance: A case study of the mutual health organisation of Dar Naïm, Mauritania. BMC Health Serv. Res. 2017, 17, 535. [Google Scholar] [CrossRef] [PubMed]
- Philibert, A.; Ravit, M.; Ridde, V.; Dossa, I.; Bonnet, E.; Bedecarrats, F.; Dumont, A. Maternal and neonatal health impact of obstetrical risk insurance scheme in Mauritania: A quasi experimental before-and-after study. Health Policy Plan. 2017, 32, 405–417. [Google Scholar] [CrossRef] [PubMed]
- Ministry of Health. Evaluation Report of the First Phase of the National Health Development Plan (2012–2020); Ministry of Health: Nouakchott, Mauritania, 2016.
- World Health Organization. Global Health Expenditure Database. World Health Organization. 2017. Available online: http://apps.who.int/nha/database (accessed on 23 July 2021).
- United Nations. Sustainable Development Goals Volunteer—Mauritania. Available online: https://sustainabledevelopment.un.org/content/documents/23447Mauritania_REVISED_AS_OF_24JUNERevueNationalVolontaire_Mauritanie2_medium.pdf (accessed on 23 July 2021). (In French).
- Ministry of Health. The National Health Development Plan 2012–2020. [Plan National de Développement Sanitaire 2012–2020]; Ministry of Health: Nouakchott, Mauritanie, 2012. (In French)
- Ministry of Economy and Finance. National Strategy for Accelerated Growth and Shared Prosperity 2016–2030 [Stratégie Nationale de Croissance Accélérée et de Prospérité Partagée 2016–2030]; Ministry of Economy and Finance: Nouakchott, Mauritanie, 2017. (In French)
- World Health Organization. Making Pregnancy Safer: The Critical Role of the Skilled Attendant: A Joint Statement by WHO, ICM and FIGO; World Health Organization: Geneva, Switzerland, 2004. [Google Scholar]
- Nghargbu, R.; Olaniyan, O. Inequity in maternal and child Health care utilization in Nigeria. Afr. Dev. Rev. 2017, 29, 630–647. [Google Scholar] [CrossRef]
- Collin, S.M.; Anwar, I.; Ronsmans, C. A decade of inequality in maternity care: Antenatal care, professional attendance at delivery, and caesarean section in Bangladesh (1991–2004). Int. J. Equity Health 2007, 6, 9. [Google Scholar] [CrossRef] [PubMed]
- Van Malderen, C.; Ogali, I.; Khasakhala, A.; Muchiri, S.N.; Sparks, C.; Van Oyen, H.; Speybroeck, N. Decomposing Kenyan socio-economic inequalities in skilled birth attendance and measles immunization. Int. J. Equity Health 2013, 12, 3. [Google Scholar] [CrossRef]
- Zere, E.; Oluwole, D.; Kirigia, J.M.; Mwikisa, C.N.; Mbeeli, T. Inequities in skilled attendance at birth in Namibia: A decomposition analysis. BMC Pregnancy Childbirth 2011, 11, 34. [Google Scholar] [CrossRef]
- Abekah-Nkrumah, G. Trends in utilisation and inequality in the use of reproductive health services in Sub-Saharan Africa. BMC Public Health 2019, 19, 1541. [Google Scholar] [CrossRef]
- Gebre, E.; Worku, A.; Bukola, F. Inequities in maternal health services utilization in Ethiopia 2000–2016: Magnitude, trends, and determinants. Reprod. Health 2018, 15, 119. [Google Scholar] [CrossRef]
- Goland, E.; Hoa, D.T.P.; Målqvist, M. Inequity in maternal health care utilization in Vietnam. Int. J. Equity Health 2012, 11, 24. [Google Scholar] [CrossRef] [PubMed]
- Harris, B.; Goudge, J.; Ataguba, J.; McIntyre, D.; Nxumalo, N.; Jikwana, S.; Chersich, M. Inequities in access to health care in South Africa. J. Public Health Policy 2011, 32, S102–S123. [Google Scholar] [CrossRef]
- Joseph, G.; da Silva, I.C.M.; Barros, A.J.D.; Victora, C. Socioeconomic inequalities in access to skilled birth attendance among urban and rural women in low-income and middle-income countries. BMJ Glob Health 2018, 3, e000898. [Google Scholar] [CrossRef] [PubMed]
- Nawal, D.; Goli, S. Inequalities in utilization of maternal health care services in Nepal. Ethn. Inequal. Health Soc. Care 2013, 6, 3–15. [Google Scholar] [CrossRef]
- Khan, M.N.; Islam, M.M.; Rahman, M.M. Inequality in utilization of cesarean delivery in Bangladesh: A decomposition analysis using nationally representative data. Public Health 2018, 157, 111–120. [Google Scholar] [CrossRef] [PubMed]
- Målqvist, M.; Pun, A.; Raaijmakers, H.; Kc, A. Persistent inequity in maternal health care utilization in Nepal despite impressive overall gains. Glob. Health Action 2017, 10, 1356083. [Google Scholar] [CrossRef] [PubMed]
- Mezmur, M.; Navaneetham, K.; Letamo, G.; Bariagaber, H. Socioeconomic inequalities in the uptake of maternal healthcare services in Ethiopia. BMC Health Serv. Res. 2017, 17, 367. [Google Scholar] [CrossRef] [PubMed]
- Molina, H.F.; Nakamura, K.; Kizuki, M.; Seino, K. Reduction in inequality in antenatal-care use and persistence of inequality in skilled birth attendance in the Philippines from 1993 to 2008. BMJ Open 2013, 3, e002507. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Rama, P.A. Inequality in Maternal Health Care Utilization in India: A Shapley Decomposition Analysis? J. Int. Dev. 2015, 27, 1141–1152. [Google Scholar]
- Amporfu, E.; Grépin, K.A. Measuring and explaining changing patterns of inequality in institutional deliveries between urban and rural women in Ghana: A decomposition analysis. Int. J. Equity Health 2019, 18, 123. [Google Scholar] [CrossRef] [PubMed]
- Ambel, A.A.; Andrews, C.; Bakilana, A.M.; Foster, E.M.; Khan, Q.; Wang, H. Examining changes in maternal and child health inequalities in Ethiopia. Int. J. Equity Health 2017, 16, 152. [Google Scholar] [CrossRef]
- National Office of Statistics. Multiple Indicator Cluster Survey (MICS) 2007; National Office of Statistics: Nouakchott, Mauritania, 2007. (In French)
- National Office of Statistics. Multiple Indicator Cluster Survey (MICS) 2015; National Office of Statistics: Nouakchott, Mauritania, 2016. (In French)
- Wagstaff, A.; van Doorslaer, E.; Paci, P. On the measurement of horizontal inequity in the delivery of health care. J. Health Econ. 1991, 10, 169–205. [Google Scholar] [CrossRef]
- Wagstaff, A. The bounds of the concentration index when the variable of interest is binary, with an application to immunization inequality. Health Econ. 2005, 14, 429–432. [Google Scholar] [CrossRef] [PubMed]
- Errygers, G. Correction the concentration index. J. Health Econ. 2009, 12, 511–516. [Google Scholar]
- Erreygers, G.; Van Ourti, T. Measuring socioeconomic inequality in health, health care and health financing by means of rank-dependent indices: A recipe for good practice. J. Health Econ. 2011, 30, 685–694. [Google Scholar] [CrossRef] [PubMed]
- Wagstaff, A. Correcting the concentration index: A comment. J. Health Econ. 2009, 28, 516–520. [Google Scholar] [CrossRef] [PubMed]
- Erreygers, G.; Van Ourti, T. Putting the cart before the horse. A comment on Wagstaff on inequality measurement in the presence of binary variables. Health Econ. 2011, 20, 1161–1165. [Google Scholar] [CrossRef] [PubMed]
- Kakwani, N.; Wagstaff, A.; Van Doorslaer, E. Socioeconomic inequalities in health: Measurement, computation, and statistical inference. J. Econ. 1997, 77, 87–103. [Google Scholar] [CrossRef]
- Wagstaff, A.; van Doorslaer, E.; Watanabe, N. On decomposing the causes of health sector inequalities with an application to malnutrition inequalities in Vietnam. J. Econ. 2003, 112, 207–223. [Google Scholar] [CrossRef]
- Hangoma, P.; Aakvik, A.; Robberstad, B. Explaining changes in child health inequality in the run up to the 2015 Millennium Development Goals (MDGs): The case of Zambia. PLoS ONE 2017, 12, e0170995. [Google Scholar] [CrossRef]
- Khaled, M.A.; Makdissi, P.; Tabri, R.V.; Yazbeck, M. A framework for testing the equality between the health concentration curve and the 45-degree line. Health Econ. 2018, 27, 887–896. [Google Scholar] [CrossRef]
- Kjellsson, G.; Gerdtham, U.-G. Measuring Health Inequalities Using the Concentration Index Approach. Encycl. Health Econ. 2014, 2, 240–246. [Google Scholar] [CrossRef]
- StataCorp. Stata Statistical Software: Release 15; StataCorp LLC: College Station, TX, USA, 2017. [Google Scholar]
- World Health Organization. What Are the Latest Statistics on Health Workforce Availability? Why Does the Latest HRH Report (A Universal Truth—No health without a Workforce, 2013) Use a Different Threshold (33.45/10,000) From the WHO 2006 Report (22.8/10,000)? Available online: https://www.who.int/workforcealliance/media/qa/05/en/ (accessed on 23 July 2021).
- Ministry of Health. Statistical Yearbook, 2016; Ministry of Heath: Nouakchott, Mauritania, 2016. (In French)
- Ministry of Health. Statistical Yearbook, 2013; Ministry of Heath: Nouakchott, Mauritania, 2013. (In French)
- Adjiwanou, V.; Le Grand, T. Does antenatal care matter in the use of skilled birth attendance in rural Africa: A multi-country analysis. Soc. Sci. Med. 2013, 86, 26–34. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.; Gao, W.; Yan, H. Measuring and decomposing the inequality of maternal health services utilization in Western Rural China. BMC Health Serv. Res. 2014, 14, 102. [Google Scholar] [CrossRef] [PubMed]
- Nwosu, C.O.; Ataguba, J.E. Socioeconomic inequalities in maternal health service utilisation: A case of antenatal care in Nigeria using a decomposition approach. BMC Public Health 2019, 19, 1493. [Google Scholar] [CrossRef]
- Omani-Samani, R.; Amini Rarani, M.; Sepidarkish, M.; Khedmati Morasae, E.; Maroufizadeh, S.; Almasi-Hashiani, A. Socioeconomic inequality of unintended pregnancy in the Iranian population: A decomposition approach. BMC Public Health 2018, 18, 607. [Google Scholar] [CrossRef] [PubMed]
- Onarheim, K.H.; Taddesse, M.; Norheim, O.F.; Abdullah, M.; Miljeteig, I. Towards universal health coverage for reproductive health services in Ethiopia: Two policy recommendations. Int. J. Equity Health 2015, 14, 86. [Google Scholar] [CrossRef]
- Khadr, Z. Monitoring socioeconomic inequity in maternal health indicators in Egypt: 1995–2005. Int. J. Equity Health 2009, 8, 38. [Google Scholar] [CrossRef]
| 2007 | 2015 | |||||
|---|---|---|---|---|---|---|
| n = 3539 | % | SBA Weighted Mean | n = 4172 | % | SBA Weighted Mean | |
| Age | ||||||
| 15–24 | 1167 | 33% | 63% | 1195 | 28% | 66% |
| 25–34 | 1583 | 45% | 55% | 1958 | 47% | 65% |
| 35–44 | 736 | 21% | 54% | 946 | 23% | 62% |
| 45–49 | 53 | 1% | 31% | 73 | 2% | 50% |
| Birth order | ||||||
| 0 | 38 | 1% | 80% | 34 | 1% | 68% |
| 1 | 644 | 18% | 70% | 789 | 19% | 77% |
| 2 | 633 | 18% | 65% | 731 | 18% | 70% |
| 3 | 569 | 16% | 56% | 682 | 16% | 69% |
| 4 | 1655 | 47% | 49% | 1936 | 46% | 56% |
| Prenatal | ||||||
| yes | 2860 | 81% | 66% | 3641 | 87% | 70% |
| no | 679 | 19% | 18% | 531 | 13% | 27% |
| Place of residence | ||||||
| urban | 1509 | 43% | 86% | 1877 | 45% | 87% |
| rural | 2030 | 57% | 36% | 2 295 | 55% | 46% |
| Region | ||||||
| Hodh Charghy | 423 | 12% | 34% | 502 | 12% | 40% |
| Hodh Gharby | 340 | 10% | 27% | 412 | 10% | 38% |
| Assaba | 371 | 10% | 35% | 479 | 11% | 55% |
| Gorgol | 341 | 10% | 32% | 508 | 12% | 49% |
| Brakna | 331 | 9% | 58% | 428 | 10% | 82% |
| Trarza | 333 | 9% | 80% | 299 | 7% | 82% |
| Adrar | 61 | 2% | 64% | 20 | 0% | 66% |
| Nouadibou | 119 | 3% | 86% | 137 | 3% | 96% |
| Tagant | 76 | 2% | 39% | 23 | 1% | 55% |
| Guidimagha | 177 | 5% | 25% | 329 | 8% | 25% |
| Tirs-Zemour | 63 | 2% | 88% | 20 | 1% | 89% |
| Inchiri | 8 | 1% | 85% | 5 | 1% | 81% |
| Nouakchott | 896 | 25% | 90% | 1010 | 24% | 95% |
| Education | 0% | |||||
| No | 1042 | 29% | 40% | 1055 | 25% | 50% |
| Primary | 1992 | 56% | 58% | 2371 | 57% | 61% |
| Secondary | 451 | 13% | 88% | 655 | 16% | 89% |
| University | 54 | 2% | 89% | 91 | 2% | 90% |
| Wealth index | ||||||
| Q1 (Poorest) | 857 | 24% | 19% | 879 | 21% | 25% |
| Q2 | 694 | 20% | 36% | 875 | 21% | 48% |
| Q3 | 657 | 19% | 67% | 829 | 20% | 71% |
| Q4 | 681 | 19% | 86% | 838 | 20% | 90% |
| Q5 | 650 | 18% | 90% | 751 | 18% | 94% |
| SBA | 3539 | 57.12% | 4172 | 64.41% | ||
| 2007 | 2015 | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| n = 3539 | n = 4172 | ||||||||||
| Variables | Marginal Effects dy/dx | Elasticity | CIE | Absolute Contribution | Percentage Contribution (%) | Marginal Effects dy/dx | Elasticity | CIE | Absolute Contribution | Percentage Contribution (%) | Change |
| Age | |||||||||||
| 15–24 | Ref. | Ref. | |||||||||
| 25–34 | −0.0249 | −0.0445 | 0.0167 | −0.0007 | −0.12% | 0.0281 | 0.0527 | 0.0718 | 0.0038 | 0.6% | 0.0045 |
| 35–44 | 0.0495 | 0.0412 | −0.0437 | −0.0018 | −0.28% | 0.0712 ** | 0.0646 | −0.0398 | −0.0026 | −0.4% | −0.0008 |
| 45–49 | −0.0663 | −0.0040 | −0.0200 | 0.0001 | 0.01% | 0.1136 * | 0.0080 | −0.0212 | −0.0002 | 0.0% | −0.0002 |
| Birth order | |||||||||||
| Child (0) | Ref. | Ref. | |||||||||
| Child (1) | −0.1908 * | −0.1392 | 0.1054 | −0.0147 | −2.32% | −0.0226 | −0.0171 | 0.1077 | −0.0018 | −0.3% | 0.0128 |
| Child (2) | −0.2391 ** | −0.1713 | 0.0832 | −0.0143 | −2.25% | −0.0712 | −0.0499 | 0.0650 | −0.0032 | −0.6% | 0.0110 |
| Child (3) | −0.2661 ** | −0.1714 | 0.0097 | −0.0017 | −0.26% | −0.0801 | −0.0524 | 0.0624 | −0.0033 | −0.6% | −0.0016 |
| Child (4+) | −0.2807 ** | −0.5251 | −0.2033 | 0.1068 | 16.88% | −0.1251 | −0.2321 | −0.2323 | 0.0539 | 9.2% | −0.0528 |
| Prenatal | |||||||||||
| yes | 0.2052 *** | 0.6632 | 0.3234 | 0.2145 | 33.91% | 0.1386 *** | 0.4837 | 0.1823 | 0.0882 | 15.1% | −0.1263 |
| no | Ref. | Ref. | |||||||||
| Place of residence | |||||||||||
| Rural | −0.1001 *** | −0.2296 | −0.8207 | 0.1884 | 29.80% | −0.0626 ** | −0.1378 | −0.8494 | 0.1170 | 20.0% | −0.0714 |
| Urban | Ref. | Ref. | |||||||||
| Region | |||||||||||
| Hodh Charghy | −0.1506 *** | −0.0719 | −0.1999 | 0.0144 | 2.27% | −0.1947 *** | −0.0937 | −0.2172 | 0.0204 | 3.5% | 0.0060 |
| Hodh Gharby | −0.1715 *** | −0.0660 | −0.1580 | 0.0104 | 1.65% | −0.1947 *** | −0.0768 | −0.1518 | 0.0117 | 2.0% | 0.0012 |
| Assaba | −0.1548 *** | −0.0650 | −0.1616 | 0.0105 | 1.66% | −0.1221 *** | −0.0561 | −0.1186 | 0.0067 | 1.1% | −0.0038 |
| Gorgol | −0.1552 *** | −0.0598 | −0.1343 | 0.0080 | 1.27% | −0.1951 *** | −0.0951 | −0.1281 | 0.0122 | 2.1% | 0.0042 |
| Brakna | −0.0681 | −0.0254 | −0.0537 | 0.0014 | 0.22% | 0.0235 | 0.0096 | −0.0355 | −0.0003 | −0.1% | −0.0017 |
| Trarza | 0.0196 | 0.0074 | 0.0697 | 0.0005 | 0.08% | −0.0634 | −0.0182 | 0.0506 | −0.0009 | −0.2% | −0.0014 |
| Adrar | −0.0153 | −0.0011 | 0.0009 | 0.0000 | 0.00% | −0.1386 | −0.0026 | 0.0016 | 0.0000 | 0.0% | 0.0000 |
| Nouadibou | −0.0784 | −0.0105 | 0.0883 | −0.0009 | −0.15% | 0.0681 | 0.0089 | 0.0947 | 0.0008 | 0.1% | 0.0018 |
| Tagant | −0.0893 | −0.0077 | −0.0216 | 0.0002 | 0.03% | −0.1564 * | −0.0034 | −0.0022 | 0.0000 | 0.0% | −0.0002 |
| Guidimagha | −0.2419 *** | −0.0484 | −0.0664 | 0.0032 | 0.51% | −0.3264 *** | −0.1028 | −0.1114 | 0.0114 | 2.0% | 0.0082 |
| Tirs-Zemour | −0.0140 | −0.0010 | 0.0392 | 0.0000 | −0.01% | −0.0978 | −0.0019 | 0.0140 | 0.0000 | 0.0% | 0.0000 |
| Inchiri | 0.0009 | 0.0000 | 0.0033 | 0.0000 | 0.00% | −0.1298 | −0.0006 | 0.0027 | 0.0000 | 0.0% | 0.0000 |
| Nouakchott | Ref. | Ref. | |||||||||
| Education Level | |||||||||||
| Primary | 0.0258 | 0.0467 | 0.0466 | 0.0022 | 0.34% | 0.0479 * | 0.0928 | −0.1097 | −0.0102 | −1.7% | −0.0123 |
| Secondary | 0.0704 ** | 0.0508 | 0.3340 | 0.0170 | 2.68% | 0.0831 *** | 0.0698 | 0.3569 | 0.0249 | 4.3% | 0.0079 |
| High | Ref. | Ref. | |||||||||
| Wealth Quintile | |||||||||||
| Q1 (Poorest) | −0.1888 *** | −0.1830 | −0.7342 | 0.1343 | 21.24% | −0.2423 *** | −0.2043 | −0.6655 | 0.1360 | 23.2% | 0.0016 |
| Q2 | −0.1328 *** | −0.1042 | −0.2506 | 0.0261 | 4.13% | −0.1308 *** | −0.1097 | −0.3092 | 0.0339 | 5.8% | 0.0078 |
| Q3 | −0.0126 | −0.0094 | 0.0464 | −0.0004 | −0.07% | −0.0355 | −0.0282 | 0.0314 | −0.0009 | −0.2% | −0.0005 |
| Q4 | 0.0293 | 0.0225 | 0.3392 | 0.0076 | 1.21% | 0.0092 | 0.0074 | 0.3530 | 0.0026 | 0.4% | −0.0050 |
| Q5 (Richest) | Ref. | Ref. | |||||||||
| Total observed | 0.711 | 112% | 0.5000 | 85% | |||||||
| Residual | −0.0786 | −12% | 0.0851 | 15% | |||||||
| CIE | 0.6324 | 100% | 0.5852 | 100% | |||||||
| Equation (7) | Equation (8) | |||||
|---|---|---|---|---|---|---|
| Weighted Δ in Elasticity | Weighted Δ in CIE | Weighted Δ in CIE | Weighted Δ in Elasticity | Total Δ | %Δ | |
| Age | ||||||
| 15–24 | Ref. | |||||
| 25–34 | 0.0029 | 0.0016 | −0.0025 | 0.0070 | 0.0045 | −9.6% |
| 35–44 | 0.0003 | −0.0010 | 0.0002 | −0.0009 | −0.0008 | 1.6% |
| 45–49 | 0.0000 | −0.0002 | 0.0000 | −0.0003 | −0.0002 | 0.5% |
| Birth order | ||||||
| Child (0) | Ref. | |||||
| Child (1) | 0.0000 | 0.0129 | −0.0003 | 0.0132 | 0.0128 | −27.2% |
| Child (2) | 0.0009 | 0.0101 | 0.0031 | 0.0079 | 0.0110 | −23.3% |
| Child (3) | −0.0028 | 0.0012 | −0.0090 | 0.0074 | −0.0016 | 3.4% |
| Child (4+) | 0.0067 | −0.0596 | 0.0152 | −0.0681 | −0.0528 | 111.8% |
| Prenatal | ||||||
| yes | −0.0682 | −0.0580 | −0.0936 | −0.0327 | −0.1263 | 267.2% |
| no | Ref. | |||||
| Place of residence | ||||||
| Rural | 0.0040 | −0.0753 | 0.0066 | −0.0780 | −0.0714 | 151.1% |
| Urban | Ref. | |||||
| Region | ||||||
| Hodh Charghy | 0.0016 | 0.0044 | 0.0012 | 0.0047 | 0.0060 | −12.6% |
| Hodh Gharby | −0.0005 | 0.0017 | −0.0004 | 0.0016 | 0.0012 | −2.6% |
| Assaba | −0.0024 | −0.0014 | −0.0028 | −0.0010 | −0.0038 | 8.1% |
| Gorgol | −0.0006 | 0.0047 | −0.0004 | 0.0045 | 0.0042 | −8.8% |
| Brakna | 0.0002 | −0.0019 | −0.0005 | −0.0012 | −0.0017 | 3.6% |
| Trarza | 0.0003 | −0.0018 | −0.0001 | −0.0013 | −0.0014 | 3.0% |
| Adrar | 0.0000 | 0.0000 | 0.0000 | 0.0000 | 0.0000 | 0.0% |
| Nouadibou | 0.0001 | 0.0017 | −0.0001 | 0.0018 | 0.0018 | −3.8% |
| Tagant | −0.0001 | −0.0001 | −0.0001 | 0.0000 | −0.0002 | 0.3% |
| Guidimagha | 0.0046 | 0.0036 | 0.0022 | 0.0061 | 0.0082 | −17.4% |
| Tirs−Zemour | 0.0000 | 0.0000 | 0.0000 | 0.0000 | 0.0000 | 0.0% |
| Inchiri | 0.0000 | 0.0000 | 0.0000 | 0.0000 | 0.0000 | 0.0% |
| Nouakchott | Ref. | |||||
| Education Level | ||||||
| Primary | −0.0145 | 0.0021 | −0.0073 | −0.0051 | −0.0123 | 26.1% |
| Secondary | 0.0016 | 0.0063 | 0.0012 | 0.0068 | 0.0079 | −16.8% |
| High | Ref. | |||||
| Wealth Quintile | ||||||
| Q1 (Poorest) | −0.0140 | 0.0157 | −0.0126 | 0.0142 | 0.0016 | −3.5% |
| Q2 | 0.0064 | 0.0014 | 0.0061 | 0.0017 | 0.0078 | −16.5% |
| Q3 | 0.0004 | −0.0009 | 0.0001 | −0.0006 | −0.0005 | 1.0% |
| Q4 | 0.0001 | −0.0051 | 0.0003 | −0.0053 | −0.0050 | 10.6% |
| Q5 (Richest) | Ref. | |||||
| Total observed | −0.0730 | −0.1380 | −0.0934 | −0.1176 | −0.2110 | 446% |
| Residual | 0.1637 | −346% | ||||
| CIE | −0.0473 | 100% | ||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Taleb El Hassen, M.V.; Cabases, J.M.; Zine Eddine El Idrissi, M.D.; Mills, S. Changes in Inequality in Use of Maternal Health Care Services: Evidence from Skilled Birth Attendance in Mauritania for the Period 2007–2015. Int. J. Environ. Res. Public Health 2022, 19, 3566. https://doi.org/10.3390/ijerph19063566
Taleb El Hassen MV, Cabases JM, Zine Eddine El Idrissi MD, Mills S. Changes in Inequality in Use of Maternal Health Care Services: Evidence from Skilled Birth Attendance in Mauritania for the Period 2007–2015. International Journal of Environmental Research and Public Health. 2022; 19(6):3566. https://doi.org/10.3390/ijerph19063566
Chicago/Turabian StyleTaleb El Hassen, Mohamed Vadel, Juan M. Cabases, Moulay Driss Zine Eddine El Idrissi, and Samuel Mills. 2022. "Changes in Inequality in Use of Maternal Health Care Services: Evidence from Skilled Birth Attendance in Mauritania for the Period 2007–2015" International Journal of Environmental Research and Public Health 19, no. 6: 3566. https://doi.org/10.3390/ijerph19063566
APA StyleTaleb El Hassen, M. V., Cabases, J. M., Zine Eddine El Idrissi, M. D., & Mills, S. (2022). Changes in Inequality in Use of Maternal Health Care Services: Evidence from Skilled Birth Attendance in Mauritania for the Period 2007–2015. International Journal of Environmental Research and Public Health, 19(6), 3566. https://doi.org/10.3390/ijerph19063566






