Dual Use of Public and Private Health Care Services in Brazil
Abstract
1. Introduction
2. Materials and Methods
2.1. Survey Design, Sampling, and Fieldwork
2.2. Definition of Dual Use
2.3. Variable Coding
2.4. Data Analysis
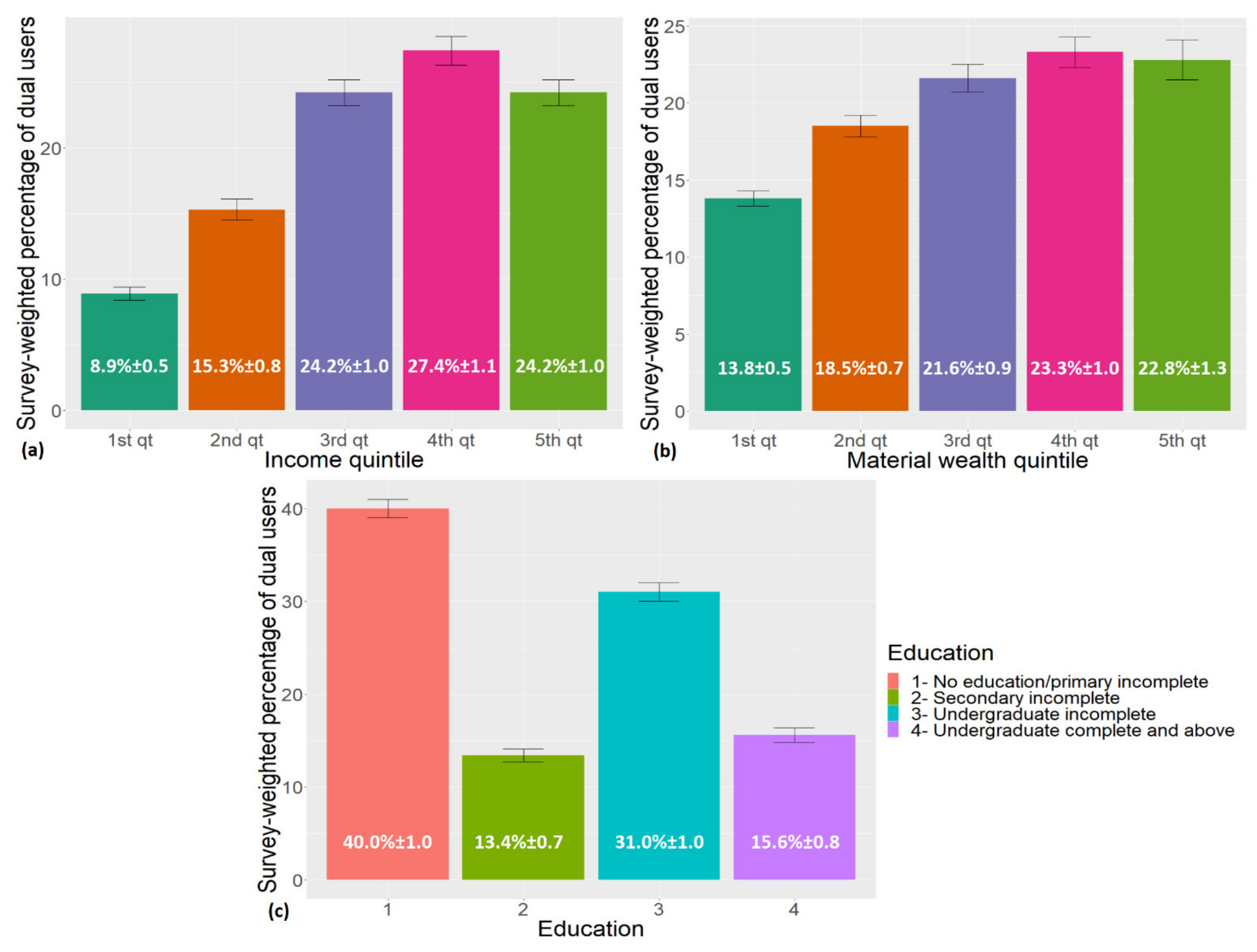
3. Results
3.1. Description of Dual Users vs. Non-Dual Users
3.2. Multinomial Regression Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| Variables | Degrees of Freedom | Chi-Square Test | p Value |
|---|---|---|---|
| (Intercept) | 1 | 55.7621 | <0.0001 |
| FHS | 1 | 0.0782 | 0.7797 |
| Usual Source of Care | 7 | 142.2408 | <0.0001 a |
| Sex | 1 | 11.0762 | 0.0009 a |
| Age | 7 | 17.7745 | 0.0130 b |
| Race | 1 | 1.2613 | 0.2614 |
| Education | 3 | 6.8839 | 0.0756 |
| Income | 4 | 35.3663 | <0.0001 a |
| Health Status | 4 | 12.4082 | 0.0020 b |
| Region | 4 | 29.1328 | <0.0001 a |
| Dwelling | 1 | 10.1889 | 0.0014 b |
| Material Wealth | 4 | 12.5951 | 0.0134 b |
| Sex × income | 4 | 15.5228 | 0.0037 b |
| Race × income | 4 | 18.4893 | 0.0010 b |
| FHS × income | 4 | 22.6198 | 0.0001 a |
| Variable | OR | 99% CI |
|---|---|---|
| FHS | ||
| Not enrolled/does not know | - | (ref) |
| Enrolled | 1.05 | 0.65–1.70 |
| Usual source of care | ||
| Other | - | (ref) |
| Public primary care | 0.69 | 0.45–1.04 |
| Public secondary care | 1.15 | 0.62–2.14 |
| Public emergency care | 0.96 | 0.60–1.52 |
| Public outpatient hospital care | 1.12 | 0.70–1.79 |
| Private outpatient care | 0.84 | 0.54–1.30 |
| Private emergency care | 0.42 | 0.23–0.74 |
| No USC | 1.34 | 0.87–2.05 |
| Sex | ||
| Male | - | (ref) |
| Female | 0.61 | 0.42–0.89 |
| Age | ||
| 0–14 | - | (ref) |
| 15–24 | 1.08 | 0.80–1.45 |
| 25–34 | 1.15 | 0.85–1.54 |
| 35–44 | 1.08 | 0.83–1.41 |
| 45–54 | 1.24 | 0.95–1.62 |
| 55–64 | 1.25 | 0.94–1.66 |
| 65–74 | 1.20 | 0.90–1.60 |
| 75+ | 1.53 | 1.13–2.06 |
| Race | ||
| White | - | (ref) |
| Non-white | 0.84 | 0.56–1.25 |
| Education | ||
| No education/primary incomplete | - | (ref) |
| Secondary incomplete | 1.06 | 0.88–1.28 |
| Undergraduate incomplete | 1.17 | 0.98–1.39 |
| Undergraduate complete and above | 1.01 | 0.79–1.27 |
| Income | ||
| 1st quintile | - | (ref) |
| 2nd quintile | 1.11 | 0.58–2.11 |
| 3rd quintile | 1.49 | 0.80–2.74 |
| 4th quintile | 1.56 | 0.84–2.88 |
| 5th quintile | 0.69 | 0.38–1.25 |
| Health status | ||
| Good/Very good | - | (ref) |
| Fair | 0.88 | 0.77–1.00 |
| Bad/Very bad | 0.76 | 0.61–0.94 |
| Region | ||
| North | - | (ref) |
| Northeast | 1.03 | 0.86–1.23 |
| Southeast | 0.79 | 0.64–0.98 |
| South | 1.04 | 0.82–1.31 |
| Center-west | 0.78 | 0.63–0.97 |
| Dwelling | ||
| Urban | - | (ref) |
| Rural | 1.24 | 1.04–1.48 |
| Material wealth | ||
| 1st quintile | - | (ref) |
| 2nd quintile | 1.15 | 1.01–1.30 |
| 3rd quintile | 1.15 | 0.97–1.36 |
| 4th quintile | 1.30 | 1.05–1.60 |
| 5th quintile | 1.18 | 0.91–1.53 |
| Effect of income on women (Income × Sex) | ||
| 1st quintile | - | (ref) |
| 2nd quintile | 1.77 | 1.11–2.81 |
| 3rd quintile | 1.72 | 1.10–2.69 |
| 4th quintile | 1.83 | 1.18–2.83 |
| 5th quintile | 1.92 | 1.23–3.00 |
| Effect of income on non-white persons (Income × Race) | ||
| 1st quintile | - | (ref) |
| 2nd quintile | 0.99 | 0.60–1.64 |
| 3rd quintile | 1.14 | 0.69–1.87 |
| 4th quintile | 1.20 | 0.74–1.93 |
| 5th quintile | 1.70 | 1.07–2.70 |
| Effect of income on those enrolled in FHS (Income × FHS) | ||
| 1st quintile | - | (ref) |
| 2nd quintile | 0.89 | 0.50–1.57 |
| 3rd quintile | 0.89 | 0.52–1.51 |
| 4th quintile | 0.88 | 0.50–1.54 |
| 5th quintile | 1.50 | 0.88–2.57 |
| Variables | Degrees of Freedom | Chi-Square Test | p Value |
|---|---|---|---|
| (Intercept) | 1 | 20.3941 | <0.0001 |
| FHS | 1 | 1.6693 | 0.1963 |
| Usual Source of Care | 7 | 28.7590 | 0.0002 a |
| Sex | 1 | 15.5698 | <0.0001a |
| Age | 7 | 18.9972 | 0.0082 b |
| Race | 1 | 0.9309 | 0.3346 |
| Education | 3 | 7.4231 | 0.0596 |
| Income | 4 | 1.1649 | 0.8838 |
| Health Status | 2 | 1.3973 | 0.4972 |
| Region | 4 | 11.5259 | 0.0212 c |
| Dwelling | 4 | 5.7336 | 0.2199 |
| Material Wealth | 1 | 0.5562 | 0.4557 |
| FHS × Dwelling | 1 | 5.7318 | 0.0167 c |
| FHS × Income | 4 | 13.0130 | 0.0112 c |
| FHS × Region | 4 | 15.3595 | 0.0040 b |
| USC × Education | 21 | 64.7627 | <0.0001 a |
| USC × Income | 28 | 111.7669 | <0.0001 a |
| USC × Health status | 14 | 39.2372 | 0.0003 a |
| USC × Dwelling | 7 | 26.1131 | 0.0005 a |
| Sex × Income | 4 | 20.9392 | 0.0003 a |
| Age × wealth | 28 | 44.7698 | 0.0232 c |
| Race × Income | 4 | 10.6655 | 0.0306 c |
| Education × Income | 12 | 25.4481 | 0.0128 b |
| Region × wealth | 16 | 34.3421 | 0.0049 b |
| Variable | OR | 99% CI |
|---|---|---|
| FHS | ||
| Not enrolled/does not know | - | (ref) |
| Enrolled | 1.29 | 0.77–2.15 |
| Usual source of care | ||
| Other | - | (ref) |
| Public primary care | 1.06 | 0.26–4.39 |
| Public secondary care | 0.82 | 0.15–4.51 |
| Public emergency care | 1.04 | 0.22–4.85 |
| Public outpatient hospital care | 1.78 | 0.39–8.22 |
| Private outpatient care | 5.38 | 1.13–25.56 |
| Private emergency care | 1.60 | 0.13–19.41 |
| No USC | 1.40 | 0.33–5.83 |
| Sex | ||
| Male | - | (ref) |
| Female | 0.55 | 0.38–0.81 |
| Age | ||
| 0–14 | - | (ref) |
| 15–24 | 1.09 | 0.78–1.50 |
| 25–34 | 1.25 | 0.92–1.71 |
| 35–44 | 1.32 | 0.98–1.77 |
| 45–54 | 1.52 | 1.13–2.05 |
| 55–64 | 1.36 | 1.00–1.84 |
| 65–74 | 1.36 | 0.98–1.89 |
| 75+ | 1.44 | 1.01–2.04 |
| Race | ||
| White | - | (ref) |
| Non–white | 0.86 | 0.56–1.29 |
| Education | ||
| No education/primary incomplete | - | (ref) |
| Secondary incomplete | 1.04 | 0.26–4.15 |
| Undergraduate incomplete | 2.34 | 0.83–6.63 |
| Undergraduate complete and above | 0.57 | 0.12–2.79 |
| Income | ||
| 1st quintile | - | (ref) |
| 2nd quintile | 0.84 | 0.12–6.06 |
| 3rd quintile | 1.32 | 0.29–6.09 |
| 4th quintile | 0.83 | 0.18–3.84 |
| 5th quintile | 1.00 | 0.20–4.91 |
| Health status | ||
| Good/Very good | - | (ref) |
| Fair | 1.32 | 0.55–3.17 |
| Bad/Very bad | 1.65 | 0.41–6.58 |
| Region | ||
| North | - | (ref) |
| Northeast | 1.10 | 0.79–1.53 |
| Southeast | 1.41 | 0.97–2.05 |
| South | 1.71 | 1.07–2.73 |
| Center–west | 1.25 | 0.86–1.81 |
| Material wealth | ||
| 1st quintile | - | (ref) |
| 2nd quintile | 1.38 | 0.84–2.29 |
| 3rd quintile | 1.52 | 0.72–3.19 |
| 4th quintile | 1.64 | 0.46–5.86 |
| 5th quintile | 0.42 | 0.03–5.55 |
| Dwelling | ||
| Urban | - | (ref) |
| Rural | 1.45 | 0.40–5.20 |
| Effect of living in an urban/rural dwelling on those enrolled in FHS (Dwelling × FHS) | ||
| Urban | - | (ref) |
| Rural | 1.43 | 0.97–2.10 |
| Effect of income on those enrolled in FHS (Income × FHS) | ||
| 1st quintile | - | (ref) |
| 2nd quintile | 0.96 | 0.55–1.70 |
| 3rd quintile | 0.95 | 0.56–1.61 |
| 4th quintile | 0.92 | 0.53–1.61 |
| 5th quintile | 1.42 | 0.83–2.42 |
| Effect of region on those enrolled in FHS (FHS × Region) | ||
| North | - | (ref) |
| Northeast | 0.87 | 0.59–1.29 |
| Southeast | 0.72 | 0.49–1.07 |
| South | 0.56 | 0.37–0.84 |
| Center–west | 0.77 | 0.50–1.18 |
| Effect of USC on those with education “secondary incomplete” (USC × Education) | ||
| Other | - | (ref) |
| Public primary care | 1.08 | 0.29–4.03 |
| Public secondary care | 1.16 | 0.23–5.81 |
| Public emergency care | 1.75 | 0.45–6.84 |
| Public outpatient hospital care | 1.66 | 0.38–7.13 |
| Private outpatient care | 0.88 | 0.23–3.35 |
| Private emergency care | 0.58 | 0.09–3.76 |
| No USC | 1.06 | 0.28–3.94 |
| Effect of USC on those with education “Undergraduate incomplete” (USC × Education) | ||
| Other | - | (ref) |
| Public primary care | 0.62 | 0.22–1.72 |
| Public secondary care | 1.04 | 0.29–3.70 |
| Public emergency care | 0.72 | 0.24–2.19 |
| Public outpatient hospital care | 0.83 | 0.28–2.47 |
| Private outpatient care | 0.34 | 0.12–0.99 |
| Private emergency care | 0.58 | 0.15–2.24 |
| No USC | 0.57 | 0.20–1.59 |
| Effect of USC on those with education “Undergraduate incomplete and above” (USC × Education) | ||
| Other | - | (ref) |
| Public primary care | 2.15 | 0.63–7.30 |
| Public secondary care | 2.62 | 0.63–10.77 |
| Public emergency care | 3.32 | 0.89–12.40 |
| Public outpatient hospital care | 1.09 | 0.28–4.17 |
| Private outpatient care | 0.71 | 0.22–2.25 |
| Private emergency care | 0.97 | 0.22–4.22 |
| No USC | 1.14 | 0.35–3.65 |
| Effect of USC on those on the 2nd quintile of income (USC × Income) | ||
| Other | - | (ref) |
| Public primary care | 1.01 | 0.14–7.11 |
| Public secondary care | 1.86 | 0.20–17.48 |
| Public emergency care | 1.10 | 0.14–8.82 |
| Public outpatient hospital care | 0.66 | 0.08–5.33 |
| Private outpatient care | 0.59 | 0.08–4.47 |
| Private emergency care | 1.68 | 0.08–34.17 |
| No USC | 1.76 | 0.24–12.89 |
| Effect of USC on those on the 3rd quintile of income (USC × Income) | ||
| Other | - | (ref) |
| Public primary care | 0.97 | 0.22–4.21 |
| Public secondary care | 1.71 | 0.27–10.97 |
| Public emergency care | 1.10 | 0.22–5.54 |
| Public outpatient hospital care | 0.98 | 0.18–5.27 |
| Private outpatient care | 0.44 | 0.08–2.31 |
| Private emergency care | 0.62 | 0.04–8.50 |
| No USC | 1.46 | 0.33–6.51 |
| Effect of USC on those in the 4th quintile of income (USC × Income) | ||
| Other | - | (ref) |
| Public primary care | 1.72 | 0.38–7.77 |
| Public secondary care | 1.51 | 0.24–9.62 |
| Public emergency care | 1.70 | 0.34–8.55 |
| Public outpatient hospital care | 2.11 | 0.40–11.02 |
| Private outpatient care | 0.42 | 0.08–2.16 |
| Private emergency care | 0.64 | 0.05–8.56 |
| No USC | 2.10 | 0.47–9.48 |
| Effect of USC on those in the 5th quintile of income (USC × Income) | ||
| Other | - | (ref) |
| Public primary care | 0.95 | 0.20–4.55 |
| Public secondary care | 3.04 | 0.37–24.96 |
| Public emergency care | 1.06 | 0.19–5.85 |
| Public outpatient hospital care | 1.66 | 0.31–8.98 |
| Private outpatient care | 0.15 | 0.03–0.81 |
| Private emergency care | 0.26 | 0.02–3.71 |
| No USC | 1.03 | 0.22–4.94 |
| Effect of USC on those with health status “regular” (USC × Health status) | ||
| Other | - | (ref) |
| Public primary care | 0.51 | 0.20–1.29 |
| Public secondary care | 0.61 | 0.18–2.01 |
| Public emergency care | 0.63 | 0.24–1.65 |
| Public outpatient hospital care | 0.47 | 0.17–1.32 |
| Private outpatient care | 0.86 | 0.34–2.18 |
| Private emergency care | 0.64 | 0.19–2.12 |
| No USC | 0.76 | 0.31–1.87 |
| Effect of USC on those with health status “bad/very bad” (USC × Health status) | ||
| Other | - | (ref) |
| Public primary care | 0.37 | 0.09–1.57 |
| Public secondary care | 0.36 | 0.06–2.26 |
| Public emergency care | 0.41 | 0.09–1.93 |
| Public outpatient hospital care | 0.16 | 0.03–0.81 |
| Private outpatient care | 0.76 | 0.18–3.26 |
| Private emergency care | 0.16 | 0.02–1.13 |
| No USC | 0.54 | 0.13–2.24 |
| Effect of USC on those living in a rural dwelling (USC × Dwelling) | ||
| Other | - | (ref) |
| Public primary care | 0.68 | 0.19–2.36 |
| Public secondary care | 0.58 | 0.11–3.03 |
| Public emergency care | 0.43 | 0.11–1.63 |
| Public outpatient hospital care | 0.35 | 0.09–1.42 |
| Private outpatient care | 1.10 | 0.30–4.06 |
| Private emergency care | 1.34 | 0.15–11.68 |
| No USC | 0.56 | 0.15–2.07 |
| Effect of income on women (Sex × Income) | ||
| 1st quintile | - | (ref) |
| 2nd quintile | 1.92 | 1.19–3.08 |
| 3rd quintile | 1.87 | 1.18–2.95 |
| 4th quintile | 1.96 | 1.26–3.05 |
| 5th quintile | 2.22 | 1.41–3.50 |
| Effect of age on those in the 2nd quintile of material wealth (Age × Wealth) | ||
| 0–14 | - | (ref) |
| 15–24 | 1.24 | 0.73–2.10 |
| 25–34 | 1.06 | 0.65–1.71 |
| 35–44 | 1.07 | 0.66–1.73 |
| 45–54 | 0.72 | 0.44–1.17 |
| 55–64 | 1.06 | 0.64–1.73 |
| 65–74 | 1.07 | 0.63–1.80 |
| 75+ | 1.25 | 0.71–2.18 |
| Effect of age on those in the 3rd quintile of material wealth (Age × Wealth) | ||
| 0–14 | - | (ref) |
| 15–24 | 1.13 | 0.64–2.02 |
| 25–34 | 0.89 | 0.51–1.54 |
| 35–44 | 0.79 | 0.47–1.33 |
| 45–54 | 0.79 | 0.46–1.34 |
| 55–64 | 0.97 | 0.57–1.65 |
| 65–74 | 1.01 | 0.56–1.82 |
| 75+ | 1.03 | 0.55–1.93 |
| Effect of age on those in the 4th quintile of material wealth (Age × Wealth) | ||
| 0–14 | - | (ref) |
| 15–24 | 0.75 | 0.38–1.45 |
| 25–34 | 0.76 | 0.40–1.45 |
| 35–44 | 0.54 | 0.28–1.02 |
| 45–54 | 0.53 | 0.28–0.98 |
| 55–64 | 0.63 | 0.32–1.21 |
| 65–74 | 0.53 | 0.26–1.06 |
| 75+ | 0.70 | 0.34–1.46 |
| Effect of age on those in the 5th quintile of material wealth (Age × Wealth) | ||
| 0–14 | - | (ref) |
| 15–24 | 1.37 | 0.57–3.25 |
| 25–34 | 1.42 | 0.59–3.39 |
| 35–44 | 1.45 | 0.71–2.96 |
| 45–54 | 1.84 | 0.89–3.79 |
| 55–64 | 1.77 | 0.79–3.98 |
| 65–74 | 1.39 | 0.58–3.31 |
| 75+ | 1.55 | 0.54–4.40 |
| Effect of income on those of non–white race (Income × Race) | ||
| 1st quintile | - | (ref) |
| 2nd quintile | 0.97 | 0.59–1.62 |
| 3rd quintile | 1.14 | 0.69–1.90 |
| 4th quintile | 1.22 | 0.75–1.97 |
| 5th quintile | 1.51 | 0.94–2.42 |
| Effect of education on those in the 2nd quintile of income (Education × Income) | ||
| No education/primary incomplete | - | (ref) |
| Secondary incomplete | 0.99 | 0.52–1.85 |
| Undergraduate incomplete | 0.85 | 0.52–1.39 |
| Undergraduate complete and above | 1.71 | 0.49–5.96 |
| Effect of education on those in the 3rd quintile of income (Education × Income) | ||
| No education/primary incomplete | - | (ref) |
| Secondary incomplete | 0.61 | 0.31–1.19 |
| Undergraduate incomplete | 0.81 | 0.50–1.33 |
| Undergraduate complete and above | 0.95 | 0.28–3.28 |
| Effect of education on those in the 4th quintile of income (Education × Income) | ||
| No education/primary incomplete | - | (ref) |
| Secondary incomplete | 1.03 | 0.54–1.95 |
| Undergraduate incomplete | 0.82 | 0.49–1.37 |
| Undergraduate complete and above | 2.14 | 0.65–6.97 |
| Effect of education on those in the 5th quintile of income (Education × Income) | ||
| No education/primary incomplete | - | (ref) |
| Secondary incomplete | 0.96 | 0.48–1.92 |
| Undergraduate incomplete | 0.82 | 0.48–1.40 |
| Undergraduate complete and above | 1.19 | 0.37–3.87 |
| Effect of region on those in the 2nd quintile of material wealth (Region × Wealth) | ||
| North | - | (ref) |
| Northeast | 0.83 | 0.56–1.22 |
| Southeast | 0.62 | 0.40–0.97 |
| South | 0.71 | 0.42–1.19 |
| Center–west | 0.74 | 0.47–1.16 |
| Effect of region on those in the 3rd quintile of material wealth (Region × Wealth) | ||
| North | - | (ref) |
| Northeast | 0.91 | 0.46–1.77 |
| Southeast | 0.62 | 0.31–1.22 |
| South | 0.70 | 0.34–1.46 |
| Center–west | 0.48 | 0.23–1.01 |
| Effect of region on those in the 4th quintile of material wealth (Region × Wealth) | ||
| North | - | (ref) |
| Northeast | 1.41 | 0.41–4.84 |
| Southeast | 0.85 | 0.25–2.84 |
| South | 1.34 | 0.39–4.64 |
| Center–west | 0.82 | 0.21–3.15 |
| Effect of region on those in the 5th quintile of material wealth (Region × Wealth) | ||
| North | - | (ref) |
| Northeast | 3.01 | 0.23–39.21 |
| Southeast | 1.30 | 0.11–15.86 |
| South | 1.79 | 0.14–22.75 |
| Center–west | 1.33 | 0.10–18.46 |
References
- Michael, T.; Filc, D.; Davidovitch, N. What Motivates Physicians to Propose Private Services in a Mixed Private-Public Healthcare System? A Mixed Methods Study. BMC Health Serv. Res. 2022, 22, 51. [Google Scholar] [CrossRef] [PubMed]
- Filc, D.; Davidovitch, N. Rethinking the Private-Public Mix in Health Care: Analysis of Health Reforms in Israel during the Last Three Decades. J. Health Serv. Res. Policy 2016, 21, 249–256. [Google Scholar] [CrossRef] [PubMed]
- di Matteo, L. The Determinants of the Public-Private Mix in Canadian Health Care Expenditures: 1975–1996. Health Policy 2000, 52, 87–112. [Google Scholar] [CrossRef]
- Bernales-Baksai, P. Tackling Segmentation to Advance Universal Health Coverage: Analysis of Policy Architectures of Health Care in Chile and Uruguay. Int. J. Equity Health 2020, 19, 106. [Google Scholar] [CrossRef]
- Yassine, A.; Hangouche, A.J.; El Malhouf, N.; Maarouf, S.; Taoufik, J. Assessment of the Medical Expenditure of the Basic Health Insurance in Morocco. Pan Afr. Med. J. 2020, 35, 115. [Google Scholar] [CrossRef] [PubMed]
- Javed, S.A.; Ilyas, F. Service Quality and Satisfaction in Healthcare Sector of Pakistan- the Patients’ Expectations. Int. J. Health Care Qual. Assur. 2018, 31, 489–501. [Google Scholar] [CrossRef] [PubMed]
- Gordon, T.; Booysen, F.; Mbonigaba, J. Socio-Economic Inequalities in the Multiple Dimensions of Access to Healthcare: The Case of South Africa. BMC Public Health 2020, 20, 289. [Google Scholar] [CrossRef]
- Konde-Lule, J.; Gitta, S.N.; Lindfors, A.; Okuonzi, S.; Onama, V.O.; Forsberg, B.C. Private and Public Health Care in Rural Areas of Uganda. BMC Int. Health Hum. Rights 2010, 10, 29. [Google Scholar] [CrossRef]
- Basu, S.; Andrews, J.; Kishore, S.; Panjabi, R.; Stuckler, D. Comparative Performance of Private and Public Healthcare Systems in Low- and Middle-Income Countries: A Systematic Review. PLoS Med. 2012, 9, e1001244. [Google Scholar] [CrossRef]
- Neto, F.L.D.; Rosa, R.G.; Duso, B.A.; Haas, J.S.; Savi, A.; Cabral, C.R.; Maccari, J.G.; Oliveira, R.P.; Antônio, A.C.P.; Castro, P.S.; et al. Public versus Private Healthcare Systems Following Discharge from the ICU: A Propensity Score-Matched Comparison of Outcomes. BioMed Res. Int. 2016, 2016, 6568531. [Google Scholar] [CrossRef]
- Stuckler, D.; Basu, S. The International Monetary Fund’s Effects on Global Health: Before and after the 2008 Financial Crisis. Int. J. Health Serv. 2009, 39, 771–781. [Google Scholar] [CrossRef] [PubMed]
- Brasil. Constituição Da República Federativa Do Brasil de 1988. Available online: http://www.planalto.gov.br/ccivil_03/constituicao/constituicao.htm (accessed on 13 August 2021).
- Viacava, F.; de Oliveira, R.A.D.; de Campos Carvalho, C.; Laguardia, J.; Bellido, J.G. SUS: Oferta, Acesso e Utilização de Serviços de Saúde Nos Últimos 30 Anos. Ciência Saúde Coletiva 2018, 23, 1751–1762. [Google Scholar] [CrossRef] [PubMed]
- Instituto Brasileiro de Geografia e Estatistica. Pesquisa Nacional de Saúde 2019—Informações Sobre Domicílios, Acesso e Utilização Dos Serviços de Saúde; Instituto Brasileiro de Geografia e Estatistica: Rio de Janeiro, Brazil, 2020; ISBN 9786587201184. [Google Scholar]
- Giovanella, L.; Bousquat, A.; Schenkman, S.; de Almeida, P.F.; Sardinha, L.M.V.; Vieira, M.L.F.P. Cobertura Da Estratégia Saúde Da Família No Brasil: O Que Nos Mostram as Pesquisas Nacionais de Saúde 2013 e 2019. Ciência Saúde Coletiva 2021, 26, 2543–2556. [Google Scholar] [CrossRef] [PubMed]
- Paim, J.; Travassos, C.; Almeida, C.; Bahia, L.; MacInko, J. The Brazilian Health System: History, Advances, and Challenges. Lancet 2011, 377, 1778–1797. [Google Scholar] [CrossRef]
- Gusso, G.D.F.; Knupp, D.; Trindade, T.G.; Junior, N.L.; Neto, P.P. Bases Para Um Novo Sanitarismo. Rev. Bras. Med. Família Comunidade 2015, 10, 1–10. [Google Scholar] [CrossRef]
- Agência Nacional de Saúde. Dados e Indicadores Do Setor. Available online: https://www.gov.br/ans/pt-br/acesso-a-informacao/perfil-do-setor/dados-e-indicadores-do-setor (accessed on 7 August 2021).
- Organisation for Economic Co-operation and Development. Health at a Glance 2019: OECD Indicators; OECD Publishing: Paris, France, 2019; ISBN 9789264382084. [Google Scholar]
- Organisation for Economic Co-operation and Development. Private Health Insurance in OECD Countries; OECD Publishing: Paris, France, 2004; ISBN 9789264006683. [Google Scholar]
- Organisation for Economic Co-operation and Development. OECD Reviews of Health Systems: Brazil 2021; OECD Publishing: Paris, France, 2021. [Google Scholar] [CrossRef]
- Bahia, L. Planos Privados de Saúde: Luzes e Sombras No Debate Setorial Dos Anos 90. Ciência Saúde Coletiva 2001, 6, 329–339. [Google Scholar] [CrossRef]
- Bahia, L.; Scheffer, M.; Poz, M.D.; Travassos, C.; Cruz, B.F.O. Planos privados de saúde com coberturas restritas: Atualização da agenda privatizante no contexto de crise política e econômica no Brasil. Cadernos Saude Publica 2016, 32, e00184516. [Google Scholar] [CrossRef] [PubMed]
- Bahia, L. O Sistema de Saúde Brasileiro Entre Normas e Fatos: Universalização Mitigada e Estratificação Subsidiada. Cienc. Saude Coletiva 2009, 14, 753–762. [Google Scholar] [CrossRef]
- Santos, I.S.; Ugá, M.A.D.; Porto, S.M. O Mix Público-Privado No Sistema de Saúde Brasileiro: Financiamento, Oferta e Utilização de Serviços de Saúde. Cienc. Saude Coletiva 2008, 13, 1431–1440. [Google Scholar] [CrossRef]
- Cavalcanti, G. Mais Da Metade Dos Usuários Que Não Têm Plano de Saúde Já Foi Beneficiária No Passado—Jornal O Globo. Available online: https://oglobo.globo.com/economia/mais-da-metade-dos-usuarios-que-nao-tem-plano-de-saude-ja-foi-beneficiaria-no-passado-23837771 (accessed on 19 June 2020).
- Agência Nacional de Saúde. Os Medicamentos Receitados Pelo Meu Médico e Que Podem Ser Comprados Em Farmácia Estão Cobertos? Available online: http://www.ans.gov.br/aans/index.php?option=com_centraldeatendimento&view=pergunta&resposta=487&historico=29789105 (accessed on 13 August 2021).
- Szwarcwald, C.L.; Júnior, P.R.B.D.S.; Marques, A.P.; Almeida, W.; Montilla, D.E.R. Inequalities in healthy life expectancy by Brazilian geographic regions: Findings from the National Health Survey, 2013. Int. J. Equity Health 2016, 15, 141. [Google Scholar] [CrossRef]
- Viacava, F.; Bellido, J.G. Health, Access to Services and Sources of Payment, According to Household Surveys. Cienc. E Saude Coletiva 2016, 21, 351–370. [Google Scholar] [CrossRef]
- Boccolini, C.S.; de Souza, P.R.B. Inequities in Healthcare Utilization: Results of the Brazilian National Health Survey, 2013. Int. J. Equity Health 2016, 15, 150. [Google Scholar] [CrossRef] [PubMed]
- Dourado, I.; Medina, M.G.; Aquino, R. The Effect of the Family Health Strategy on Usual Source of Care in Brazil: Data from the 2013 National Health Survey (PNS 2013). Int. J. Equity Health 2016, 15, 151. [Google Scholar] [CrossRef] [PubMed]
- Szwarcwald, C.L.; Stopa, S.R.; Damacena, G.N.; da Silva de Almeida, W.; de Souza, P.R.B.; Vieira, M.L.F.P.; Pereira, C.A.; Sardinha, L.M.V.; Macário, E.M. Mudanças No Padrão de Utilização de Serviços de Saúde No Brasil Entre 2013 e 2019. Ciência Saúde Coletiva 2021, 26, 2515–2528. [Google Scholar] [CrossRef] [PubMed]
- Júnior, P.R.B.D.S.; Szwarcwald, C.L.; Damacena, G.N.; Stopa, S.R.; Vieira, M.L.F.P.; Almeida, W.D.S.D.; de Oliveira, M.M.; Sardinha, L.M.V.; Macário, E.M. Cobertura de plano de saúde no Brasil: Análise dos dados da Pesquisa Nacional de Saúde 2013 e 2019. Ciência Saúde Coletiva 2021, 26, 2529–2541. [Google Scholar] [CrossRef] [PubMed]
- Mullachery, P.; Silver, D.; Macinko, J. Changes in Health Care Inequity in Brazil between 2008 and 2013. Int. J. Equity Health 2016, 15, 140. [Google Scholar] [CrossRef]
- Silva, Z.P.; Ribeiro, M.C.S.A.; Barata, R.B.; Almeida, M.F. Perfil Sociodemográfico e Padrão de Utilização Dos Serviços de Saúde Do Sistema Único de Saúde (SUS), 2003–2008. Ciência Saúde Coletiva 2011, 16, 3807–3816. [Google Scholar] [CrossRef]
- Macinko, J.; Mendonça, C.S. Estratégia Saúde Da Família, Um Forte Modelo de Atenção Primária à Saúde Que Traz Resultados. Saúde Em Debate 2018, 42, 18–37. [Google Scholar] [CrossRef]
- Gonçalves, R.F.; de Sousa, I.M.C.; Tanaka, O.Y.; Dos Santos, C.R.; Brito-Silva, K.; Santos, L.X.; Bezerra, A.F.B. The Mais Médicos (More Doctors) Program in Northeast: Evaluation of Hospitalizations for Primary Healthcare-Sensitive Conditions. Ciência Saúde Coletiva 2016, 21, 2815–2824. [Google Scholar] [CrossRef]
- Agência Nacional de Saúde. Boletim Informativo. Available online: https://www.gov.br/ans/pt-br/centrais-de-conteudo/completo-boletim-8-edicao-online-alterada-pdf (accessed on 26 January 2021).
- Fontenelle, L.F.; Sarti, T.D.; De Camargo, M.B.J.; Maciel, E.L.N.; Barros, A.J.D. Utilization of the Brazilian Public Health System by Privately Insured Individuals: A Literature Review. Cad. Saúde Pública 2019, 35, e00004118. [Google Scholar] [CrossRef]
- Meneses, C.S.; Cecilio, L.C.O.; Andreazza, R.; Carapinheiro, G.; Andrade, M.G.G.; Santiago, S.M.; Araújo, E.C.; Souza, A.L.M.; Reis, D.O.; Pinto, N.R.S.; et al. O Agir Leigo e a Produção de Mapas de Cuidado Mistos Público-Privados. Cienc. Saude Coletiva 2017, 22, 2013–2024. [Google Scholar] [CrossRef]
- Castiglione, D.; Lovasi, G.S.; Carvalho, M.S. Perceptions and Uses of Public and Private Health Care in a Brazilian Favela. Qual. Health Res. 2018, 28, 159–172. [Google Scholar] [CrossRef] [PubMed]
- Conill, E.M.; Pires, D.; Sisson, M.C.; de Oliveira, M.C.; Boing, A.F.; Fertonani, H.P. O Mix Público-Privado Na Utilização de Serviços de Saúde: Um Estudo Dos Itinerários Terapêuticos de Beneficiários Do Segmento de Saúde Suplementar Brasileiro. Cienc. Saude Coletiva 2008, 13, 1501–1510. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Instituto Brasileiro de Geografia e Estatística. Pesquisa Nacional de Saúde. Available online: https://www.ibge.gov.br/estatisticas/sociais/saude/9160-pesquisa-nacional-de-saude.html?edicao=9163&t=resultados (accessed on 26 October 2020).
- Stopa, S.R.; Szwarcwald, C.L.; Oliveira, M.M.; Gouvea, E.C.D.P.; Vieira, M.L.F.P.; Freitas, M.P.S.; Sardinha, L.M.V.; Macário, E.M. National Health Survey 2019: History, Methods and Perspectives. Epidemiol. Serviços Saúde 2020, 29, e2020315. [Google Scholar] [CrossRef]
- IBGE. Pesquisa Nacional de Saúde: 2019 : Informações Sobre Domicílios, Acesso Utilização Dos Serviços de Saúde : Brasil, Grandes Regiões e Unidades Federação. IBGE: Rio de Janeiro, Brazil, 2020; ISBN 9786587201184. [Google Scholar]
- Andersen, R.M. Revisiting the Behavioral Model and Access to Medical Care: Does It Matter? J. Health Soc. Behav. 1995, 36, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Rutstein, S.O.; Johnson, K. The DHS Wealth Index; ORC Macro: Calverton, MD, USA, 2004. [Google Scholar]
- Armstrong, R.A. When to Use the Bonferroni Correction. Ophthalmic Physiol. Opt. 2014, 34, 502–508. [Google Scholar] [CrossRef] [PubMed]
- Freijomil-Vázquez, C.; Gastaldo, D.; Coronado, C.; Movilla-Fernández, M.-J. When Risk Becomes Illness: The Personal and Social Consequences of Cervical Intraepithelial Neoplasia Medical Surveillance. PLoS ONE 2019, 14, e0226261. [Google Scholar] [CrossRef]
- Gomes, R.; Nascimento, E.F.; Araújo, F.C. Por Que Os Homens Buscam Menos Os Serviços de Saúde Do Que as Mulheres? As Explicações de Homens Com Baixa Escolaridade e Homens Com Ensino Superior. Cad. Saúde Pública 2007, 23, 565–574. [Google Scholar] [CrossRef]
- Stopa, S.R.; Malta, D.C.; Monteiro, C.N.; Szwarcwald, C.L.; Goldbaum, M.; Cesar, C.L.G. Use of and Access to Health Services in Brazil, 2013 National Health Survey. Rev. Saúde Pública 2017, 51, 1S–10S. [Google Scholar] [CrossRef]
- Ministério da Saúde. Política Nacional de Atenção Básica. Available online: http://189.28.128.100/dab/docs/publicacoes/geral/pnab.pdf (accessed on 7 August 2021).
- Pilotto, L.M.; Celeste, R.K. The Relationship between Private Health Plans and Use of Medical and Dental Health Services in the Brazilian Health System. Ciência Saúde Coletiva 2019, 24, 2727–2736. [Google Scholar] [CrossRef]
- Instituto Brasileiro de Geografia e Estatística. Pesquisa Nacional de Saude—2013 V0015. Módulo A—Informações Do Domicílio; Ministério da Saúde: Rio de Janeiro, Brazil, 2017; pp. 1–52. [Google Scholar]
- Starfield, B.; Shi, L.; Macinko, J. Contribution of Primary Care to Health Systems and Health. Milbank Q. 2005, 83, 457–502. [Google Scholar] [CrossRef]
- Macinko, J.; Starfield, B.; Shi, L. The Contribution of Primary Care Systems to Health Outcomes within Organization for Economic Cooperation and Development (OECD) Countries, 1970–1998. Health Serv. Res. 2003, 38, 831–865. [Google Scholar] [CrossRef] [PubMed]
- Hart, J.T. The Inverse Care Law. Lancet 1971, 297, 405–412. [Google Scholar] [CrossRef]
- Vaccarella, S.; Davies, L. The Inverse Care Law: Overutilization of Health Services and Overdiagnosis. In Reducing Social Inequalities in Cancer: Evidence and Priorities for Research; Vaccarella, S., Lortet-Tieulent, J., Saracci, R., Eds.; International Agency for Research on Cancer: Lyon, France, 2019. [Google Scholar]
- Wammes, J.J.G.; van der Wees, P.J.; Tanke, M.A.C.; Westert, G.P.; Jeurissen, P.P.T. Systematic Review of High-Cost Patients’ Characteristics and Healthcare Utilisation. BMJ Open 2018, 8, e023113. [Google Scholar] [CrossRef] [PubMed]
- Costa, S.M.; Ferreira, A.; Xavier, L.R.; Guerra, P.N.S.; Rodrigues, C.A.Q. Referencia e Contrareferencia na Saude da Familia: Percepcao dos Profissionais de Saude. Rev. APS 2013, 16, 287–293. [Google Scholar]
- Protasio, A.P.L.; Da Silva, P.B.; De Lima, E.C.; Machado, L.D.S.; Valença, A.M.G.; Gomes, L.B. Avaliação do sistema de referência e contrarreferência do estado da Paraíba segundo os profissionais da Atenção Básica no contexto do 1° ciclo de avaliação externa do PMAQ-AB. Saúde Debate 2014, 38, 209–220. [Google Scholar] [CrossRef]
- Serra, C.G.; Rodrigues, P.H.A. Avaliação Da Referência e Contrarreferência No Programa Saúde Da Família Na Região Metropolitana Do Rio de Janeiro (RJ, Brasil). Ciência Saúde Coletiva 2010, 15, 3579–3586. [Google Scholar] [CrossRef]
- Bahia, L. As Contradições Entre o SUS Universal e as Transferências de Recursos Públicos Para Os Planos e Seguros Privados de Saúde. Ciência Saúde Coletiva 2008, 13, 1385–1397. [Google Scholar] [CrossRef][Green Version]
| Variable | Definition |
|---|---|
| Dual use | True: individual without private health insurance who used a private source for the last care episode individual with private health insurance who used a public source for the last care episode |
| False: individual without private health insurance who used a public source for the last care episode individual with private health insurance who used a private source for the last care episode | |
| Sex | Male |
| Female | |
| Age groups (in years of age) | 0–14 |
| 15–24 | |
| 25–34 | |
| 35–44 | |
| 45–54 | |
| 65–74 | |
| 75+ | |
| Race/skin color | White |
| Non-white | |
| Dwelling | Rural |
| Urban | |
| Geographic Region | North |
| Northeast | |
| Southeast | |
| South | |
| Center-west | |
| Self-reported Health Status | Good/very good |
| Fair | |
| Bad/very bad | |
| Household Enrollment in the FHS | Yes |
| No/does not know | |
| USC | Public primary care |
| Public secondary care | |
| Public emergency care | |
| Public hospital outpatient care | |
| Private outpatient care | |
| Private emergency care | |
| Other | |
| No USC | |
| Educational attainment | No education/primary incomplete |
| Secondary incomplete | |
| Undergraduate incomplete | |
| Undergraduate complete and above | |
| Monthly income | Quintiles |
| Material wealth | Quintiles |
| Variable | Respondents Who Sought Care in the 2 Weeks Prior to the Survey | All | p Value | ||||
|---|---|---|---|---|---|---|---|
| N | WN | % ± SE | N | WN | % ± SE | ||
| Total | 46,914 | 39,039,016 | 100 (18.6 ± 0.2) | 279,382 | 209,589,607 | 100 | -- |
| Dwelling | <0.0001 | ||||||
| Urban | 38,027 | 34,514,587 | 88.4 ± 0.3 | 174,259 | 144,517,015 | 84.7 ± 0.2 | |
| Rural | 8887 | 4,524,429 | 11.6 ± 0.3 | 58,209 | 26,033,576 | 15.3 ± 0.2 | |
| Sex | <0.0001 | ||||||
| Male | 17,624 | 14,816,032 | 37.9 ± 0.3 | 116,818 | 85,342,077 | 50.0 ± 0.1 | |
| Female | 29,290 | 24,222,984 | 62.0 ± 0.3 | 115,650 | 85,208,514 | 50.0 ± 0.1 | |
| Race | <0.0001 | ||||||
| White | 18,497 | 18,350,812 | 47.0 ± 0.5 | 80,522 | 72,686,910 | 42.6 ± 0.3 | |
| Non-white | 28,410 | 20,683,376 | 53.0 ± 0.5 | 151,929 | 97,854,237 | 57.4 ± 0.3 | |
| Age | <0.0001 | ||||||
| 0–14 | 6920 | 5,653,355 | 14.7 ± 0.3 | 48,018 | 33,091,415 | 19.6 ± 0.2 | |
| 15–24 | 5036 | 4,037,134 | 10.5 ± 0.2 | 38,791 | 27,289,832 | 16.2 ± 0.1 | |
| 25–34 | 5513 | 4,435,939 | 11.6 ± 0.3 | 34,341 | 25,569,937 | 15.1 ± 0.1 | |
| 35–44 | 6738 | 5,693,580 | 14.8 ± 0.3 | 34,722 | 25,852,008 | 15.3 ± 0.1 | |
| 45–54 | 7147 | 6,086,616 | 15.9 ± 0.3 | 29,070 | 22,338,009 | 13.2 ± 0.1 | |
| 55–64 | 6705 | 5,700,443 | 14.9 ± 0.3 | 22,845 | 17,627,126 | 10.4 ± 0.1 | |
| 65–74 | 4819 | 4,007,847 | 10.4 ± 0.2 | 13,814 | 10,495,985 | 6.2 ± 0.1 | |
| +75 | 3116 | 2,714,413 | 7.1 ± 0.2 | 8437 | 6,576,903 | 3.9 ± 0.1 | |
| Material wealth | <0.0001 | ||||||
| 1st quintile | 21,894 | 6,258,532 | 16.0 ± 0.2 | 124,048 | 35,659,389 | 21.0 ± 0.2 | |
| 2nd quintile | 10,318 | 7,161,698 | 18.3 ± 0.3 | 49,094 | 34,754,593 | 20.4 ± 0.3 | |
| 3rd quintile | 6789 | 8,110,930 | 20.8 ± 0.4 | 28,734 | 33,806,841 | 19.8 ± 0.3 | |
| 4th quintile | 4695 | 8,276,514 | 21.2 ± 0.5 | 18,840 | 33,646,716 | 19.7 ± 0.3 | |
| 5th quintile | 3218 | 9,231,342 | 23.6 ± 0.7 | 11,752 | 32,683,053 | 19.2 ± 0.4 | |
| Income | <0.0001 | ||||||
| 1st quintile | 9236 | 6,062,530 | 15.7 ± 0.4 | 60,624 | 34,924,549 | 20.7 ± 0.3 | |
| 2nd quintile | 8956 | 6,903,809 | 17.8 ± 0.4 | 49,755 | 34,076,163 | 20.1 ± 0.3 | |
| 3rd quintile | 9203 | 7,882,833 | 20.4 ± 0.4 | 43,964 | 34,169,054 | 20.2 ± 0.3 | |
| 4th quintile | 8595 | 8,101,195 | 20.9 ± 0.4 | 38,708 | 33,722,160 | 20.0 ± 0.3 | |
| 5th quintile | 10,500 | 9,752,815 | 25.2 ± 0.6 | 37,087 | 32,045,680 | 19.0 ± 0.3 | |
| Education | <0.0001 | ||||||
| No education/primary incomplete | 19,355 | 15,598,252 | 43.0 ± 0.5 | 101,988 | 70,237,162 | 43.8 ± 0.3 | |
| Secondary incomplete | 5727 | 4,866,029 | 13.4 ± 0.3 | 32,837 | 24,683,737 | 15.4 ± 0.1 | |
| Undergraduate incomplete | 11,679 | 9,927,810 | 27.4 ± 0.4 | 59,363 | 46,330,722 | 28.9 ± 0.2 | |
| Undergraduate complete and above | 6749 | 5,857,799 | 16.2 ± 0.5 | 23,897 | 19,241,167 | 12.0 ± 0.2 | |
| Region | <0.0001 | ||||||
| North | 8372 | 2,476,537 | 6.3 ± 0.1 | 53,075 | 15,648,213 | 9.9 ± 0.0 | |
| Northeast | 15,925 | 9,427,647 | 24.1 ± 0.3 | 83,628 | 47,522,444 | 27.9 ± 0.1 | |
| Southeast | 11,324 | 18,509,818 | 47.4 ± 0.5 | 45,016 | 69,877,525 | 41.0 ± 0.1 | |
| South | 6145 | 5,921,489 | 15.1 ± 0.3 | 25,093 | 24,021,083 | 14.1 ± 0.1 | |
| Center-west | 5148 | 2,703,525 | 6.9 ± 0.2 | 25,656 | 13,481,326 | 7.9 ± 0.0 | |
| FHS | 0.8701 | ||||||
| Enrolled | 30,866 | 24,408,374 | 62.5 ± 0.8 | 152,206 | 106,793,241 | 62.6 ± 0.5 | |
| Not enrolled/does not know | 16,048 | 14,630,642 | 37.5 ± 0.8 | 80,262 | 63,757,350 | 37.4 ± 0.5 | |
| Health insurance | <0.0001 | ||||||
| Yes | 14,049 | 13,512,509 | 34.6 ± 0.6 | 44,548 | 41,075,465 | 24.1 ± 0.3 | |
| No | 32,865 | 25,526,507 | 65.4 ± 0.6 | 187,920 | 129,475,126 | 75.9 ± 0.3 | |
| Health status | <0.0001 | ||||||
| Very good or good | 25,635 | 22,293,108 | 57.1 ± 0.4 | 173,046 | 130,710,571 | 76.6 ± 0.2 | |
| Fair | 15,856 | 12,529,640 | 32.1 ± 0.4 | 50,949 | 34,291,030 | 20.1 ± 0.2 | |
| Bad or very bad | 5423 | 4,216,268 | 10.8 ± 0.2 | 8473 | 5,548,990 | 3.3 ± 0.1 | |
| Usual source of care | <0.0001 | ||||||
| Public primary care | 17,273 | 13,578,307 | 34.8 ± 0.6 | 90,192 | 61,561,878 | 36.1 ± 0.4 | |
| Public secondary care | 1104 | 926,077 | 2.4 ± 0.2 | 4236 | 3,260,442 | 1.9 ± 0.1 | |
| Public emergency care | 4286 | 3,869,702 | 9.9 ± 0.4 | 23,195 | 18,805,982 | 11.0 ± 0.3 | |
| Public outpatient hospital care | 2388 | 1,698,374 | 4.4 ± 0.2 | 12,833 | 8,420,497 | 4.9 ± 0.2 | |
| Private outpatient care | 9453 | 8,651,236 | 22.2 ± 0.5 | 32,254 | 28,000,797 | 16.4 ± 0;3 | |
| Private emergency care | 1720 | 1,805,915 | 4.6 ± 0.3 | 4975 | 5,254,904 | 3.1 ± 0.2 | |
| No USC | 9762 | 7,758,115 | 19.9 ± 0.4 | 59,523 | 41,435,080 | 24.3 ± 0.3 | |
| Other | 928 | 751,291 | 1.9 ± 0.1 | 5260 | 3,811,011 | 2.2 ± 0.1 | |
| Variable | Dual Users | Non-Dual Users | p Value | ||||
|---|---|---|---|---|---|---|---|
| N | WN | % ± SE | N | WN | % ± SE | ||
| Total | 6484 | 5,586,216 | 14.7 ± 0.3 | 39,161 | 32,464,691 | 85.3 ± 0.3 | --- |
| Source of care in the last care episode | --- | ||||||
| Public | 1855 | 1,824,075 | 32.7 ± 1.2 | 27,198 | 20,986,190 | 64.6 ± 0.7 | |
| Public primary care | 1091 | 1,056,345 | 18.9 ± 0.9 | 17,326 | 13,131,253 | 40.4 ± 0.6 | |
| Public secondary care | 165 | 164,875 | 3.0 ± 0.5 | 1975 | 1,581,826 | 4.9 ± 0.2 | |
| Public emergency care | 299 | 332,130 | 5.9 ± 0.6 | 4308 | 3,682,936 | 11.3 ± 0.4 | |
| Public outpatient hospital care | 300 | 270,725 | 4.8 ± 0.4 | 3589 | 2,590,176 | 8.0 ± 0.3 | |
| Private | 4629 | 3,762,141 | 67.3 ± 1.2 | 11,963 | 11,478,500 | 35.4 ± 0.7 | |
| Private outpatient care | 4510 | 3,649,346 | 65.3 ± 1.2 | 10,909 | 10,368,736 | 31.9 ± 0.7 | |
| Private emergency care | 119 | 112,795 | 2.0 ± 0.3 | 1054 | 1,109,765 | 3.4 ± 0.2 | |
| Dwelling | 0.8326 | ||||||
| Urban | 5302 | 4,936,837 | 88.4 ± 0.6 | 31,772 | 28,735,906 | 88.5 ± 0.3 | |
| Rural | 1182 | 649,379 | 11.6 ± 0.6 | 7389 | 3,728,784 | 11.5 ± 0.3 | |
| Sex | 0.4349 | ||||||
| Male | 2421 | 2,080,070 | 37.2 ± 0.9 | 14,684 | 12,330,217 | 38.0 ± 0.4 | |
| Female | 4063 | 3,506,146 | 62.8 ± 0.9 | 24,477 | 20,134,474 | 62.0 ± 0.4 | |
| Race | 0.3707 | ||||||
| White | 2,723 | 2,678,337 | 47.9 ± 1.2 | 15,346 | 15,205,573 | 46.8 ± 0.6 | |
| Non-white | 3,760 | 2.906,404 | 52.0 ± 1.2 | 23,809 | 17,255,764 | 53.1 ± 0.6 | |
| Age | <0.0001 | ||||||
| 0–14 | 704 | 603,867 | 11.0 ± 0.6 | 6031 | 4,917,455 | 15.4 ± 0.4 | |
| 15–24 | 689 | 562,366 | 10.2 ± 0.6 | 4237 | 3,386,684 | 10.6 ± 0.3 | |
| 25–34 | 807 | 661,781 | 12.0 ± 0.6 | 4567 | 3,685,894 | 11.6 ± 0.3 | |
| 35–44 | 931 | 791,971 | 14.4 ± 0.7 | 5622 | 4,749,581 | 14.9 ± 0.3 | |
| 45–54 | 1035 | 938,279 | 17.0 ± 0.8 | 5915 | 4,995,966 | 15.7 ± 0.3 | |
| 55–64 | 980 | 872,479 | 15.8 ± 0.8 | 5563 | 4,695,428 | 14.7 ± 0.3 | |
| 65–74 | 730 | 604,638 | 11.0 ± 0.6 | 3967 | 3,303,700 | 10.4 ± 0.3 | |
| +75 | 524 | 468,207 | 8.5 ± 0.6 | 2441 | 2,114,412 | 6.6 ± 0.2 | |
| Material wealth | 0.0238 | ||||||
| 1st quintile | 2730 | 770,606 | 13.8 ± 0.5 | 18,473 | 5,290,345 | 16.3 ± 0.3 | |
| 2nd quintile | 1546 | 1,031,484 | 18.5 ± 0.7 | 8536 | 5,960,294 | 18.4 ± 0.3 | |
| 3rd quintile | 1039 | 1,206,076 | 21.6 ± 0.9 | 5590 | 6,708,142 | 20.7 ± 0.4 | |
| 4th quintile | 733 | 1,302,748 | 23.3 ± 1.0 | 3855 | 6,787,801 | 20.9 ± 0.5 | |
| 5th quintile | 436 | 1,275,302 | 22.8 ± 1.3 | 2707 | 7,718,109 | 23.8 ± 0.7 | |
| Income | <0.0001 | ||||||
| 1st quintile | 674 | 493,170 | 8.9 ± 0.5 | 8274 | 5,435,607 | 16.9 ± 0.4 | |
| 2nd quintile | 1077 | 847,354 | 15.3 ± 0.8 | 7634 | 5,914,432 | 18.4 ± 0.5 | |
| 3rd quintile | 1499 | 1,340,608 | 24.2 ± 1.0 | 7444 | 6,336,868 | 19.7 ± 0.4 | |
| 4th quintile | 1638 | 1,515,270 | 27.4 ± 1.1 | 6735 | 6,359,361 | 19.8 ± 0.5 | |
| 5th quintile | 1548 | 1,342,525 | 24.2 ± 1.0 | 8709 | 8,135,141 | 25.3 ± 0.6 | |
| Education | 0.0005 | ||||||
| No education/primary incomplete | 2554 | 2,125,761 | 40.0 ± 1.0 | 16,167 | 13,016,696 | 43.4 ± 0.5 | |
| Secondary incomplete | 799 | 710,452 | 13.4 ± 0.7 | 4793 | 4,057,513 | 13.5 ± 0.3 | |
| Undergraduate incomplete | 1877 | 1,649,275 | 31.0 ± 1.0 | 9519 | 8,040,664 | 26.8 ± 0.4 | |
| Undergraduate complete and above | 966 | 831,863 | 15.6 ± 0.8 | 5639 | 4,896,515 | 16.3 ± 0.5 | |
| Region | 0.0001 | ||||||
| North | 1001 | 329,207 | 5.9 ± 0.3 | 7036 | 2,050,520 | 6.3 ± 0.1 | |
| Northeast | 2130 | 1,360,014 | 24.3 ± 0.9 | 13,336 | 7,816,474 | 24.1 ± 0.4 | |
| Southeast | 1613 | 2,522,940 | 45.2 ± 1.2 | 9492 | 15,553,599 | 47.9 ± 0.5 | |
| South | 1007 | 1,022,744 | 18.3 ± 0.8 | 5011 | 4,759,052 | 14.7 ± 0.3 | |
| Center-west | 733 | 351,311 | 6.3 ± 0.3 | 4286 | 2,285,045 | 7.0 ± 0.2 | |
| FHS | 0.4941 | ||||||
| Enrolled | 4288 | 3,525,913 | 63.1 ± 1.2 | 25,687 | 20,215,961 | 62.3 ± 0.8 | |
| Not enrolled/does not know | 2196 | 2,060,303 | 36.9 ± 1.2 | 13,474 | 12,248,730 | 37.7 ± 0.8 | |
| Health insurance | --- | ||||||
| Yes | 1855 | 1,824,075 | 32.6 ± 1.2 | 11,963 | 11,478,500 | 35.4 ± 0.7 | |
| No | 4629 | 3,762,141 | 67.3 ± 1.2 | 27,198 | 20,986,190 | 64.6 ± 0.7 | |
| Health status | 0.0691 | ||||||
| Very good or good | 3658 | 3,273,005 | 58.6 ± 1.0 | 21,355 | 18,514,420 | 57.0 ± 0.5 | |
| Fair | 2172 | 1,786,910 | 32.0 ± 0.9 | 13,249 | 10,411,676 | 32.1 ± 0.4 | |
| Bad or very bad | 654 | 526,302 | 9.4 ± 0.6 | 4557 | 3,538,595 | 10.9 ± 0.3 | |
| Usual source of care | <0.0001 | ||||||
| Public primary care | 1744 | 1,504,077 | 26.9 ± 1.0 | 15,070 | 11,744,325 | 36.2 ± 0.7 | |
| Public secondary care | 148 | 151,909 | 2.7 ± 0.4 | 937 | 760,471 | 2.3 ± 0.2 | |
| Public emergency care | 595 | 562,753 | 10.1 ± 0;7 | 3577 | 3,207,923 | 9.9 ± 0.4 | |
| Public outpatient hospital care | 351 | 281,898 | 5.0 ± 0.4 | 1967 | 1,373,239 | 4.2 ± 0.2 | |
| Private outpatient care | 1499 | 1,294,930 | 23.2 ± 1.0 | 7842 | 7,254,370 | 22.3 ± 0.6 | |
| Private emergency care | 139 | 139,193 | 2.5 ± 0.3 | 1555 | 1,640,989 | 5.0 ± 0.3 | |
| No USC | 1870 | 1,559,743 | 27.9 ± 1.0 | 7629 | 6,005,851 | 18.5 ± 0.4 | |
| Other | 138 | 91,714 | 1.6 ± 0.2 | 584 | 477,522 | 1.5 ± 0.1 | |
| Variables | Degrees of Freedom | Chi-Square Test | p Value |
|---|---|---|---|
| (Intercept) | 1 | 157.0421 | <0.0001 |
| FHS | 1 | 2.7118 | 0.0980 |
| Usual Source of Care | 7 | 148.8832 | <0.0001 a |
| Sex | 1 | 1.5545 | 0.2125 |
| Age | 7 | 16.9408 | 0.0177 c |
| Race | 1 | 0.4276 | 0.5132 |
| Education | 3 | 7.7329 | 0.0519 |
| Income | 4 | 125.2728 | <0.0001 a |
| Health Status | 4 | 11.6643 | 0.0290 c |
| Region | 4 | 27.7091 | <0.0001 a |
| Dwelling | 1 | 9.8556 | 0.0017 b |
| Material Wealth | 4 | 12.9843 | 0.0113 c |
| Comparison | Odds Ratio | p Value * |
|---|---|---|
| Region | ||
| Southeast—North | 0.79 | 0.0590 |
| Center-west—North | 0.79 | 0.0548 |
| Southeast—Northeast | 0.78 | 0.0049 |
| Center-west—Northeast | 0.77 | 0.0040 |
| South—Southeast | 1.31 | 0.0016 |
| Center-west—South | 0.76 | 0.0054 |
| Income | ||
| 2nd quintile—1st quintile | 1.47 | 0.0002 |
| 3rd quintile—1st quintile | 2.16 | <0.0001 |
| 4th quintile—1st quintile | 2.43 | <0.0001 |
| 5th quintile—1st quintile | 1.70 | <0.0001 |
| 3rd quintile—2nd quintile | 1.46 | <0.0001 |
| 4th quintile—2nd quintile | 1.65 | <0.0001 |
| 5th quintile—3rd quintile | 0.78 | 0.0442 |
| 5th quintile—4th quintile | 0.70 | 0.0001 |
| Usual source of care | ||
| Private emergency care—Other | 0.41 | 0.0017 |
| Public emergency care—Public primary care | 1.42 | 0.0106 |
| Public outpatient hospital care—Public primary care | 1.64 | 0.0001 |
| Private emergency care—Public primary care | 0.60 | 0.0502 |
| No USC—Public primary care | 1.97 | <0.0001 |
| Private emergency care—Public secondary care | 0.35 | 0.0002 |
| Private emergency care—Public emergency care | 0.42 | <0.0001 |
| No USC—Public emergency care | 1.39 | 0.0245 |
| Private emergency care—Public outpatient hospital care | 0.36 | <0.0001 |
| Private emergency care—Private outpatient care | 0.49 | 0.0001 |
| No USC—Private outpatient care | 1.62 | <0.0001 |
| No USC—Private emergency care | 3.31 | <0.0001 |
| Variable | OR | 99% CI |
|---|---|---|
| Dwelling | ||
| Urban | - | (ref) |
| Rural | 1.24 | 1.03–1.47 |
| Sex | ||
| Male | - | (ref) |
| Female | 1.06 | 0.971–1.15 |
| Race | ||
| White | - | (ref) |
| Non–white | 1.04 | 0.95–1.18 |
| Age | ||
| 0–14 | - | (ref) |
| 15–24 | 1.05 | 0.78–1.42 |
| 25–34 | 1.12 | 0.83–1.51 |
| 35–44 | 1.06 | 0.82–1.39 |
| 45–54 | 1.23 | 0.94–1.60 |
| 55–64 | 1.22 | 0.92–1.62 |
| 65–74 | 1.18 | 0.89–1.57 |
| +75 | 1.49 | 1.10–2.00 |
| Material wealth | ||
| 1st quintile | - | (ref) |
| 2nd quintile | 1.15 | 1.01–1.31 |
| 3rd quintile | 1.16 | 0.97–1.37 |
| 4th quintile | 1.30 | 1.06–1.61 |
| 5th quintile | 1.17 | 0.90–1.53 |
| Income | ||
| 1st quintile | - | (ref) |
| 2nd quintile | 1.47 | 1.16–1.86 |
| 3rd quintile | 2.16 | 1.71–2.73 |
| 4th quintile | 2.43 | 1.91–3.08 |
| 5th quintile | 1.69 | 1.26–2.26 |
| Education | ||
| No education/primary incomplete | - | (ref) |
| Secondary incomplete | 1.06 | 0.88–1.28 |
| Undergraduate incomplete | 1.16 | 0.98–1.39 |
| Undergraduate complete and above | 0.98 | 0.77–1.24 |
| Region | ||
| North | - | (ref) |
| Northeast | 1.02 | 0.85–1.23 |
| Southeast | 0.79 | 0.64–0.99 |
| South | 1.05 | 0.83–1.32 |
| Center–west | 0.78 | 0.63–0.98 |
| FHS | ||
| Not enrolled/does not know | - | (ref) |
| Enrolled | 1.10 | 0.95–1.26 |
| Health status | ||
| Very good or good | - | (ref) |
| Fair | 0.88 | 0.77–1.01 |
| Bad or very bad | 0.77 | 0.62–0.95 |
| Usual source of care | ||
| Other | - | (ref) |
| Public primary care | 0.683 | 0.45–1.04 |
| Public secondary care | 1.15 | 0.62–2.14 |
| Public emergency care | 0.970 | 0.61–1.54 |
| Public outpatient hospital care | 1.12 | 0.70–1.79 |
| Private outpatient care | 0.832 | 0.54–1.29 |
| Private emergency care | 0.406 | 0.23–0.72 |
| No USC | 1.35 | 0.88–2.07 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Silva, B.; Hens, N.; Gusso, G.; Lagaert, S.; Macinko, J.; Willems, S. Dual Use of Public and Private Health Care Services in Brazil. Int. J. Environ. Res. Public Health 2022, 19, 1829. https://doi.org/10.3390/ijerph19031829
Silva B, Hens N, Gusso G, Lagaert S, Macinko J, Willems S. Dual Use of Public and Private Health Care Services in Brazil. International Journal of Environmental Research and Public Health. 2022; 19(3):1829. https://doi.org/10.3390/ijerph19031829
Chicago/Turabian StyleSilva, Bianca, Niel Hens, Gustavo Gusso, Susan Lagaert, James Macinko, and Sara Willems. 2022. "Dual Use of Public and Private Health Care Services in Brazil" International Journal of Environmental Research and Public Health 19, no. 3: 1829. https://doi.org/10.3390/ijerph19031829
APA StyleSilva, B., Hens, N., Gusso, G., Lagaert, S., Macinko, J., & Willems, S. (2022). Dual Use of Public and Private Health Care Services in Brazil. International Journal of Environmental Research and Public Health, 19(3), 1829. https://doi.org/10.3390/ijerph19031829







