Effects of Exergaming in Patients with Cardiovascular Disease Compared to Conventional Cardiac Rehabilitation: A Systematic Review and Meta-Analysis
Abstract
:1. Introduction
2. Methods
2.1. Data Search and Sources
2.2. Study Selection
2.3. Data Extraction and Coding Study Characteristics
2.4. Risk of Bias Assessment
2.5. Computation of Effect Size and Statistical Analyses
3. Results
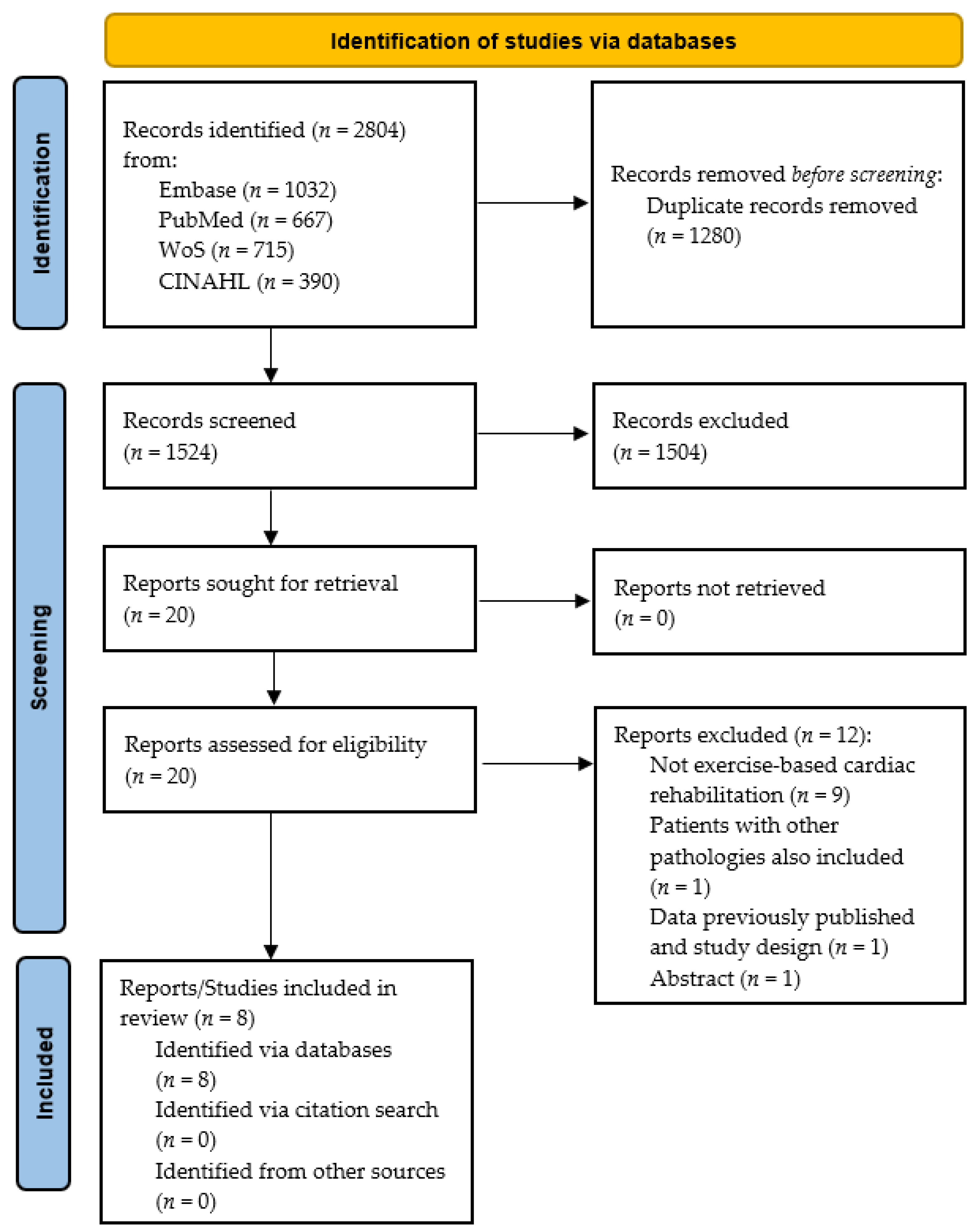
3.1. Study Selection
3.2. Study Characteristics
3.3. Risk of Bias Assessment
3.4. Outcome Measures
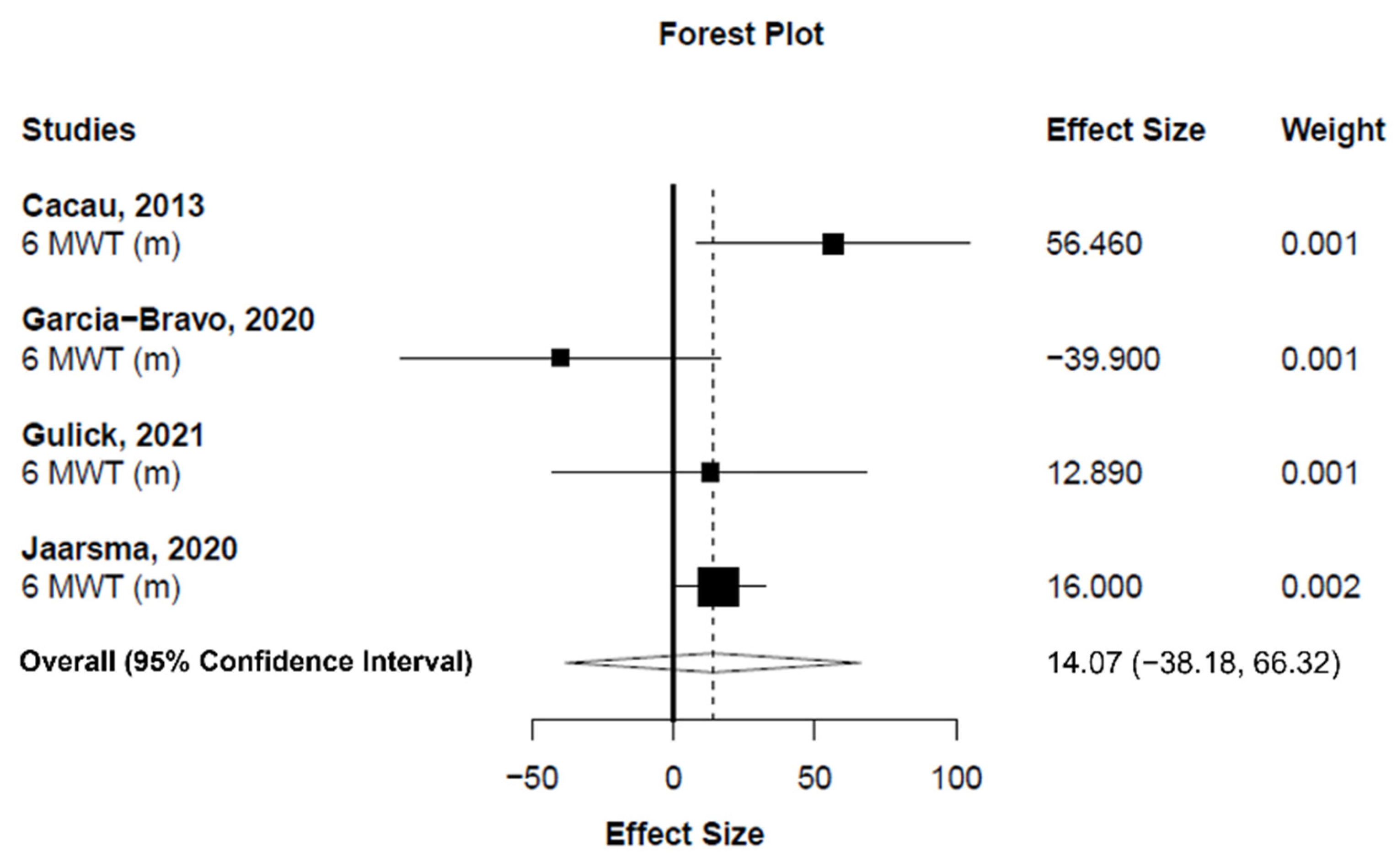
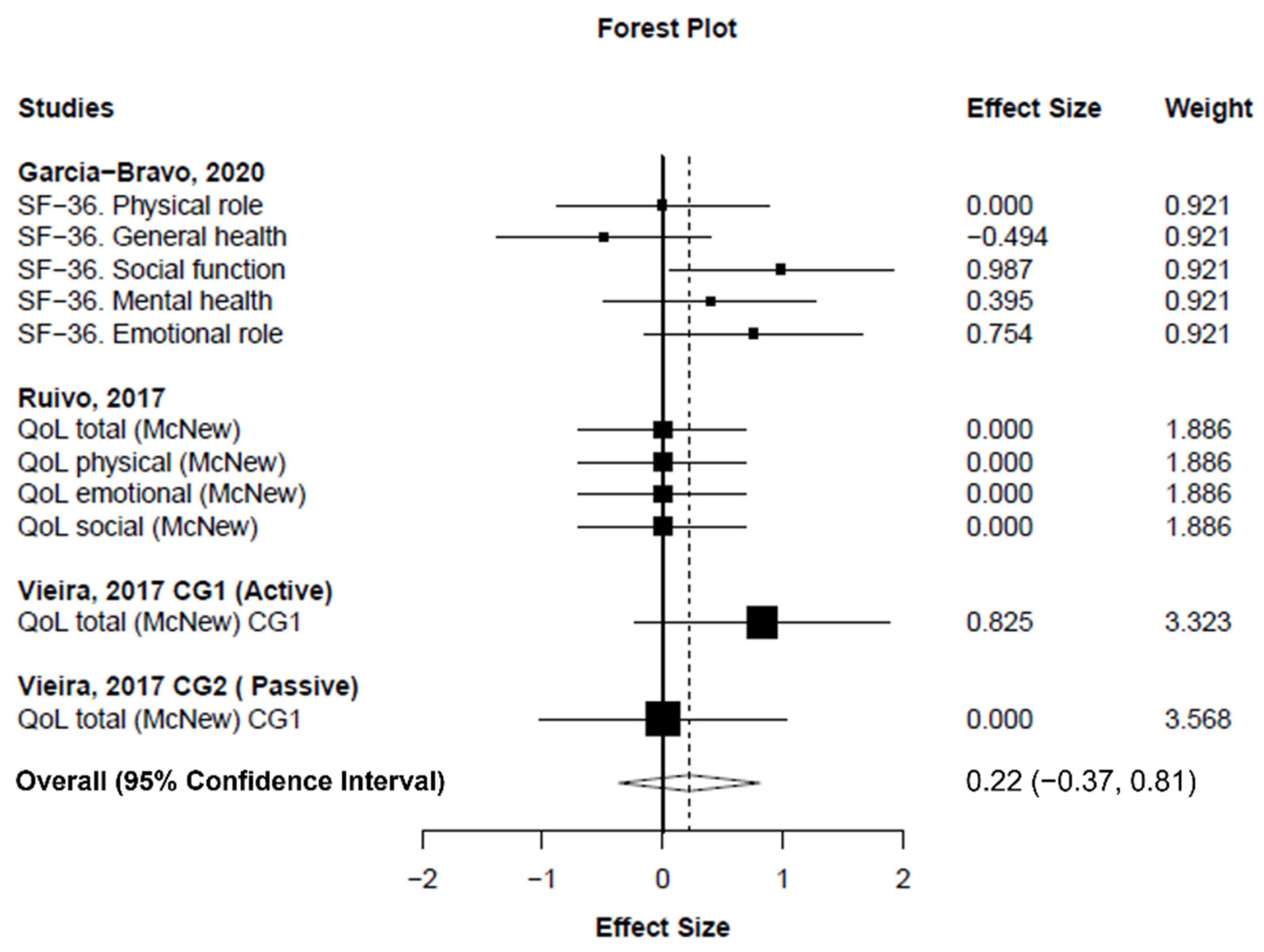
3.5. Pooled Analyses
4. Discussion
5. Strengths and Limitations
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Virani, S.S.; Alonso, A.; Aparicio, H.J.; Benjamin, E.J.; Bittencourt, M.S.; Callaway, C.W.; Carson, A.P.; Chamberlain, A.M.; Cheng, S.; Delling, F.N.; et al. Heart Disease and Stroke Statistics-2021 Update: A Report from the American Heart Association. Circulation 2021, 143, e254–e743. [Google Scholar] [CrossRef]
- Nelson, S.; Whitsel, L.; Khavjou, O.; Phelps, D.; Leib, A. Projections of Cardiovascular Disease Prevalence and Costs; Technical Report; RTI International Research: Triangle Park, NC, USA, 2016; p. 214680. [Google Scholar]
- Rauch, B.; Salzwedel, A.; Bjarnason-Wehrens, B.; Albus, C.; Meng, K.; Schmid, J.P.; Benzer, W.; Hackbusch, M.; Jensen, K.; Schwaab, B.; et al. Cardiac Rehabilitation in German Speaking Countries of Europe-Evidence-Based Guidelines from Germany, Austria and Switzerland LLKardReha-DACH-Part 1. J. Clin. Med. 2021, 10, 2192. [Google Scholar] [CrossRef]
- Papathanasiou, J.; Troev, T.; Ferreira, A.S.; Tsekoura, D.; Elkova, H.; Kyriopoulos, E.; Ilieva, E. Advanced Role and Field of Competence of the Physical and Rehabilitation Medicine Specialist in Contemporary Cardiac Rehabilitation. Hell. J. Cardiol. 2016, 57, 16–22. [Google Scholar] [CrossRef] [Green Version]
- Shields, G.E.; Wells, A.; Doherty, P.; Heagerty, A.; Buck, D.; Davies, L.M. Cost-effectiveness of cardiac rehabilitation: A systematic review. Heart 2018, 104, 1403–1410. [Google Scholar] [CrossRef] [PubMed]
- Pelliccia, A.; Sharma, S.; Gati, S.; Bäck, M.; Börjesson, M.; Caselli, S.; Collet, J.P.; Corrado, D.; Drezner, J.A.; Halle, M.; et al. ESC Guidelines on sports cardiology and exercise in patients with cardiovascular disease. Eur. Heart J. 2021, 42, 17–96. [Google Scholar] [CrossRef]
- Piepoli, M.F.; Hoes, A.W.; Agewall, S.; Albus, C.; Brotons, C.; Catapano, A.L.; Cooney, M.T.; Corrà, U.; Cosyns, B.; Deaton, C.; et al. European Guidelines on cardiovascular disease prevention in clinical practice: The Sixth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of 10 societies and by invited experts) Developed with the special contribution of the European Association for Cardiovascular Prevention & Rehabilitation (EACPR). Eur. Heart J. 2016, 37, 2315–2381. [Google Scholar]
- Candelaria, D.; Randall, S.; Ladak, L.; Gallagher, R. Health-related quality of life and exercise-based cardiac rehabilitation in contemporary acute coronary syndrome patients: A systematic review and meta-analysis. Qual. Life Res. 2020, 29, 579–592. [Google Scholar] [CrossRef] [PubMed]
- Long, L.; Mordi, I.R.; Bridges, C.; Sagar, V.A.; Davies, E.J.; Coats, A.J.; Dalal, H.; Rees, K.; Singh, S.J.; Taylor, R.S. Exercise-based cardiac rehabilitation for adults with heart failure. Cochrane Database Syst. Rev. 2019, 1, Cd003331. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rauch, B.; Davos, C.H.; Doherty, P.; Saure, D.; Metzendorf, M.I.; Salzwedel, A.; Völler, H.; Jensen, K.; Schmid, J.P. The prognostic effect of cardiac rehabilitation in the era of acute revascularisation and statin therapy: A systematic review and meta-analysis of randomized and non-randomized studies—The Cardiac Rehabilitation Outcome Study (CROS). Eur. J. Prev. Cardiol. 2016, 23, 1914–1939. [Google Scholar] [CrossRef] [Green Version]
- Beatty, A.L.; Schiller, N.B.; Whooley, M.A. Six-Minute Walk Test as a Prognostic Tool in Stable Coronary Heart Disease: Data from the Heart and Soul Study. Arch. Int. Med. 2012, 172, 1096–1102. [Google Scholar] [CrossRef] [Green Version]
- Omar, H.R.; Guglin, M. Prognostic value of 6-min walk test and cardiopulmonary exercise test in acute heart failure (from the ESCAPE trial). Am. Heart J. Plus Cardiol. Res. Pract. 2021, 1, 100005. [Google Scholar] [CrossRef]
- Ciani, O.; Piepoli, M.; Smart, N.; Uddin, J.; Walker, S.; Warren, F.C.; Zwisler, A.D.; Davos, C.H.; Taylor, R.S. Validation of Exercise Capacity as a Surrogate Endpoint in Exercise-Based Rehabilitation for Heart Failure: A Meta-Analysis of Randomized Controlled Trials. JACC Heart Fail. 2018, 6, 596–604. [Google Scholar] [CrossRef] [PubMed]
- Giannitsi, S.; Bougiakli, M.; Bechlioulis, A.; Kotsia, A.; Michalis, L.K.; Naka, K.K. 6-min walking test: A useful tool in the management of heart failure patients. Ther. Adv. Cardiovasc. Dis. 2019, 13, 1753944719870084. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ambrosetti, M.; Abreu, A.; Corrà, U.; Davos, C.H.; Hansen, D.; Frederix, I.; Iliou, M.C.; Pedretti, R.F.; Schmid, J.P.; Vigorito, C.; et al. Secondary prevention through comprehensive cardiovascular rehabilitation: From knowledge to implementation. 2020 update. A position paper from the Secondary Prevention and Rehabilitation Section of the European Association of Preventive Cardiology. Eur. J. Prev. Cardiol. 2020, 28, 460–495. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Resurrección, D.M.; Moreno-Peral, P.; Gómez-Herranz, M.; Rubio-Valera, M.; Pastor, L.; Caldas de Almeida, J.M.; Motrico, E. Factors associated with non-participation in and dropout from cardiac rehabilitation programmes: A systematic review of prospective cohort studies. Eur. J. Cardiovasc. Nurs. 2019, 18, 38–47. [Google Scholar] [CrossRef] [PubMed]
- Oosenbrug, E.; Marinho, R.P.; Zhang, J.; Marzolini, S.; Colella, T.J.; Pakosh, M.; Grace, S.L. Sex Differences in Cardiac Rehabilitation Adherence: A Meta-analysis. Can. J. Cardiol. 2016, 32, 1316–1324. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, A.V.; Ong, Y.A.; Luo, C.X.; Thuraisingam, T.; Rubino, M.; Levin, M.F.; Kaizer, F.; Archambault, P.S. Virtual reality exergaming as adjunctive therapy in a sub-acute stroke rehabilitation setting: Facilitators and barriers. Disabil. Rehabil. Assist. Technol. 2018, 14, 317–324. [Google Scholar] [CrossRef] [PubMed]
- Fang, Z.; Wu, T.; Lv, M.; Chen, M.; Zeng, Z.; Qian, J.; Chen, W.; Jiang, S.; Zhang, J. Effect of Traditional plus Virtual Reality Rehabilitation on Prognosis of Stroke Survivors: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Am. J. Phys. Med. Rehabil. 2022, 101, 217–228. [Google Scholar] [CrossRef] [PubMed]
- Laver, K.E.; Lange, B.; George, S.; Deutsch, J.E.; Saposnik, G.; Crotty, M. Virtual reality for stroke rehabilitation. Cochrane Database Syst. Rev. 2017, 11, Cd008349. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zeng, N.; Pope, Z.; Lee, J.E.; Gao, Z. A systematic review of active video games on rehabilitative outcomes among older patients. J. Sport Health Sci. 2017, 6, 33–43. [Google Scholar] [CrossRef]
- Zhang, B.; Li, D.; Liu, Y.; Wang, J.; Xiao, Q. Virtual reality for limb motor function, balance, gait, cognition and daily function of stroke patients: A systematic review and meta-analysis. J. Adv. Nurs. 2021, 77, 3255–3273. [Google Scholar] [CrossRef] [PubMed]
- Verheijden Klompstra, L.; Jaarsma, T.; Strömberg, A. Exergaming in older adults: A scoping review and implementation potential for patients with heart failure. Eur. J. Cardiovasc. Nurs. 2014, 13, 388–398. [Google Scholar] [CrossRef]
- Ruivo, J.; Karim, K.; O’Shea, R.; Oliveira, R.C.S.; Keary, L.; O’Brien, C.; Gormley, J.P. In-class Active Video Game Supplementation and Adherence to Cardiac Rehabilitation. J. Cardiopulm. Rehabil. Prev. 2017, 37, 274–278. [Google Scholar] [CrossRef] [PubMed]
- Radhakrishnan, K.; Baranowski, T.; Julien, C.; Thomaz, E.; Kim, M. Role of Digital Games in Self-Management of Cardiovascular Diseases: A Scoping Review. Games Health J. 2019, 8, 65–73. [Google Scholar] [CrossRef] [PubMed]
- Davis, A.J.; Parker, H.M.; Gallagher, R. Gamified applications for secondary prevention in patients with high cardiovascular disease risk: A systematic review of effectiveness and acceptability. J. Clin. Nurs. 2021, 30, 3001–3010. [Google Scholar] [CrossRef] [PubMed]
- García-Bravo, S.; Cuesta-Gómez, A.; Campuzano-Ruiz, R.; López-Navas, M.J.; Domínguez-Paniagua, J.; Araújo-Narváez, A.; Barreñada-Copete, E.; García-Bravo, C.; Flórez-García, M.T.; Botas-Rodríguez, J.; et al. Virtual reality and video games in cardiac rehabilitation programs. A systematic review. Disabil. Rehabil. 2021, 43, 448–457. [Google Scholar] [CrossRef]
- Gulick, V.; Graves, D.; Ames, S.; Krishnamani, P.P. Effect of a Virtual Reality-Enhanced Exercise and Education Intervention on Patient Engagement and Learning in Cardiac Rehabilitation: Randomized Controlled Trial. J. Med. Int. Res. 2021, 23, e23882. [Google Scholar] [CrossRef]
- Jaarsma, T.; Klompstra, L.; Ben Gal, T.; Ben Avraham, B.; Boyne, J.; Back, M.; Chiala, O.; Dickstein, K.; Evangelista, L.; Hagenow, A.; et al. Effects of exergaming on exercise capacity in patients with heart failure: Results of an international multicentre randomized controlled trial. Eur. J. Heart Fail. 2021, 23, 114–124. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. Int. J. Surg. 2021, 88, 105906. [Google Scholar] [CrossRef] [PubMed]
- Cumpston, M.; Li, T.; Page, M.J.; Chandler, J.; Welch, V.A.; Higgins, J.P.; Thomas, J. Updated guidance for trusted systematic reviews: A new edition of the Cochrane Handbook for Systematic Reviews of Interventions. Cochrane Database Syst. Rev. 2019, 10, Ed000142. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences; Academic Press: Cambridge, MA, USA, 2013. [Google Scholar]
- Higgins, J.P.; Thomas, J.; Chandler, J.; Cumpston, M.; Li, T.; Page, M.J.; Welch, V.A. Cochrane Handbook for Systematic Reviews of Interventions; John Wiley & Sons: Hoboken, NJ, USA, 2019. [Google Scholar]
- Hedges, L.V.; Tipton, E.; Johnson, M.C. Robust variance estimation in meta-regression with dependent effect size estimates. Res. Synth. Methods 2010, 1, 39–65. [Google Scholar] [CrossRef] [PubMed]
- Tipton, E. Small sample adjustments for robust variance estimation with meta-regression. Psychol. Methods 2015, 20, 375–393. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.P.; Thompson, S.G. Quantifying heterogeneity in a meta-analysis. Stat. Med. 2002, 21, 1539–1558. [Google Scholar] [CrossRef] [PubMed]
- Melsen, W.G.; Bootsma, M.C.; Rovers, M.M.; Bonten, M.J. The effects of clinical and statistical heterogeneity on the predictive values of results from meta-analyses. Clin. Microbiol. Infect. 2014, 20, 123–129. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cacau, L.A.; Oliveira, G.U.; Maynard, L.G.; Araújo Filho, A.A.; Silva, W.M.; Cerqueria Neto, M.L.; Antoniolli, A.R.; Santana-Filho, V.J. The use of the virtual reality as intervention tool in the postoperative of cardiac surgery. Braz. J. Cardiovasc. Surg. 2013, 28, 281–289. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chuang, T.Y.; Sung, W.H.; Chang, H.A.; Wang, R.Y. Effect of a virtual reality-enhanced exercise protocol after coronary artery bypass grafting. Phys. Ther. 2006, 86, 1369–1377. [Google Scholar] [CrossRef]
- Klompstra, L.; Jaarsma, T.; Strömberg, A. Exergaming to increase the exercise capacity and daily physical activity in heart failure patients: A pilot study. BMC Geriatr. 2014, 14, 119. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vieira, A.; Melo, C.; Machado, J.; Gabriel, J. Virtual reality exercise on a home-based phase III cardiac rehabilitation program, effect on executive function, quality of life and depression, anxiety and stress: A randomized controlled trial. Disabil. Rehabil. Assist. Technol. 2018, 13, 112–123. [Google Scholar] [CrossRef]
- Garcia-Bravo, S.; Cano-de-la-Cuerda, R.; Dominguez-Paniagua, J.; Campuzano-Ruiz, R.; Barrenada-Copete, E.; Lopez-Navas, M.J.; Araujo-Narvaez, A.; Garcia-Bravo, C.; Florez-Garcia, M.; Botas-Rodriguez, J.; et al. Effects of Virtual Reality on Cardiac Rehabilitation Programs for Ischemic Heart Disease: A Randomized Pilot Clinical Trial. Int. J. Environ. Res. Public Health 2020, 17, 8472. [Google Scholar] [CrossRef]
- Brewer, L.C.; Kaihoi, B.; Schaepe, K.; Zarling, K.; Squires, R.W.; Thomas, R.J.; Kopecky, S. Patient-perceived acceptability of a virtual world-based cardiac rehabilitation program. Digit. Health 2017, 3, 2055207617705548. [Google Scholar] [CrossRef]
- Chatzitofis, A.; Monaghan, D.; Mitchell, E.; Honohan, F.; Zarpalas, D.; O’Connor, N.E.; Daras, P. HeartHealth: A cardiovascular disease home-based rehabilitation system. Procedia Comput. Sci. 2015, 63, 340–347. [Google Scholar] [CrossRef] [Green Version]
- Hickman, R.L.; Clochesy, J.M.; Pinto, M.D.; Burant, C.; Pignatiello, G. Impact of serious game for health on chronic disease self-management: Preliminary efficacy among community dwelling adults with hypertension. J. Health Hum. Serv. Adm. 2015, 38, 253–275. [Google Scholar]
- Jóźwik, S.; Cieślik, B.; Gajda, R.; Szczepańska-Gieracha, J. Evaluation of the Impact of Virtual Reality-Enhanced Cardiac Rehabilitation on Depressive and Anxiety Symptoms in Patients with Coronary Artery Disease: A Randomised Controlled Trial. J. Clin. Med. 2021, 10, 2148. [Google Scholar] [CrossRef]
- Maciołek, J.; Wąsek, W.; Kamiński, B.; Piotrowicz, K.; Krzesiński, P. The impact of mobile virtual reality-enhanced relaxation training on anxiety levels in patients undergoing cardiac rehabilitation. Kardiol. Pol. (Pol. Heart J.) 2020, 78, 1032–1034. [Google Scholar] [CrossRef]
- Radhakrishnan, K.; Julien, C.; O’Hair, M.; Baranowski, T.; Lee, G.; Allen, C.; Sagna, A.; Thomaz, E.; Kim, M. Usability Testing of a Sensor-Controlled Digital Game to Engage Older Adults with Heart Failure in Physical Activity and Weight Monitoring. Appl. Clin. Inform. 2020, 11, 873–881. [Google Scholar] [CrossRef] [PubMed]
- Radhakrishnan, K.; Toprac, P.; O’Hair, M.; Bias, R.; Kim, M.T.; Bradley, P.; Mackert, M. Interactive Digital e-Health Game for Heart Failure Self-Management: A Feasibility Study. Games Health J. 2016, 5, 366–374. [Google Scholar] [CrossRef]
- Szczepańska-Gieracha, J.; Jóźwik, S.; Cieślik, B.; Mazurek, J.; Gajda, R. Immersive Virtual Reality Therapy as a Support for Cardiac Rehabilitation: A Pilot Randomized-Controlled Trial. Cyberpsychol. Behav. Soc. Netw. 2021, 24, 543–549. [Google Scholar] [CrossRef] [PubMed]
- da Cruz, M.M.A.; Ricci-Vitor, A.L.; Borges, G.L.B.; da Silva, P.F.; Turri-Silva, N.; Takahashi, C.; Grace, S.L.; Vanderlei, L.C.M. A Randomized, Controlled, Crossover Trial of Virtual Reality in Maintenance Cardiovascular Rehabilitation in a Low-Resource Setting: Impact on Adherence, Motivation, and Engagement. Phys. Ther. 2021, 101, pzab071. [Google Scholar] [CrossRef]
- Vieira, A.; Gabriel, J.; Melo, C.; Machado, J. Kinect system in home-based cardiovascular rehabilitation. Proc. Inst. Mech. Eng. Part H J. Eng. Med. 2017, 231, 40–47. [Google Scholar] [CrossRef]
- Klochkov, A.; Khizhnikova, A.E.; Kotov-Smolenskiy, A.M.; Suponeva, N.A.; Chernikova, L. In Efficacy of training in virtual environment in patients with balance disturbances. Eur. J. Neurol. 2018, 25, 207. [Google Scholar]
- Gremeaux, V.; Troisgros, O.; Benaïm, S.; Hannequin, A.; Laurent, Y.; Casillas, J.M.; Benaïm, C. Determining the minimal clinically important difference for the six-minute walk test and the 200-m fast-walk test during cardiac rehabilitation program in coronary artery disease patients after acute coronary syndrome. Arch. Phys. Med. Rehabil. 2011, 92, 611–619. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Täger, T.; Hanholz, W.; Cebola, R.; Fröhlich, H.; Franke, J.; Doesch, A.; Katus, H.A.; Wians, F.H., Jr.; Frankenstein, L. Minimal important difference for 6-min walk test distances among patients with chronic heart failure. Int. J. Cardiol. 2014, 176, 94–98. [Google Scholar] [CrossRef] [PubMed]
- Candelaria, D.; Zecchin, R.; Ferry, C.; Ladak, L.; Randall, S.; Gallagher, R. Shorter Wait Times to Cardiac Rehabilitation Associated with Greater Exercise Capacity Improvements: A Multisite study. J. Cardiopulm. Rehabil. Prev. 2021, 41, 243–248. [Google Scholar] [CrossRef] [PubMed]
- Collins, Z.C.; Suskin, N.; Aggarwal, S.; Grace, S.L. Cardiac rehabilitation wait times and relation to patient outcomes. Eur. J. Phys. Rehabil. Med. 2015, 51, 301–309. [Google Scholar]
- Haykowsky, M.; Scott, J.; Esch, B.; Schopflocher, D.; Myers, J.; Paterson, I.; Warburton, D.; Jones, L.; Clark, A.M. A meta-analysis of the effects of exercise training on left ventricular remodeling following myocardial infarction: Start early and go longer for greatest exercise benefits on remodeling. Trials 2011, 12, 92. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Manresa-Rocamora, A.; Ribeiro, F.; Sarabia, J.M.; Íbias, J.; Oliveira, N.L.; Vera-García, F.J.; Moya-Ramón, M. Exercise-based cardiac rehabilitation and parasympathetic function in patients with coronary artery disease: A systematic review and meta-analysis. Clin. Auton. Res. 2021, 31, 187–203. [Google Scholar] [CrossRef]
- Manresa-Rocamora, A.; Sarabia, J.M.; Sánchez-Meca, J.; Oliveira, J.; Vera-Garcia, F.J.; Moya-Ramón, M. Are the Current Cardiac Rehabilitation Programs Optimized to Improve Cardiorespiratory Fitness in Patients? A Meta-Analysis. J. Aging Phys. Act. 2020, 29, 327–342. [Google Scholar] [CrossRef] [PubMed]
- Johnson, D.A.; Sacrinty, M.T.; Gomadam, P.S.; Mehta, H.J.; Brady, M.M.; Douglas, C.J.; Paladenech, C.C.; Robinson, K.C. Effect of early enrollment on outcomes in cardiac rehabilitation. Am. J. Cardiol. 2014, 114, 1908–1911. [Google Scholar] [CrossRef]
- McPhee, P.G.; Winegard, K.J.; MacDonald, M.J.; McKelvie, R.S.; Millar, P.J. Importance of early cardiac rehabilitation on changes in exercise capacity: A retrospective pilot study. Appl. Physiol. Nutr. Metab. 2015, 40, 1314–1317. [Google Scholar] [CrossRef] [PubMed]
- MacInnis, M.J.; Gibala, M.J. Physiological adaptations to interval training and the role of exercise intensity. J. Physiol. 2017, 595, 2915–2930. [Google Scholar] [CrossRef] [Green Version]
- Peng, W.; Lin, J.H.; Crouse, J. Is playing exergames really exercising? A meta-analysis of energy expenditure in active video games. Cyberpsychol. Behav. Soc. Netw. 2011, 14, 681–688. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Balady, G.J.; Williams, M.A.; Ades, P.A.; Bittner, V.; Comoss, P.; Foody, J.M.; Franklin, B.; Sanderson, B.; Southard, D. Core components of cardiac rehabilitation/secondary prevention programs: 2007 update: A scientific statement from the American Heart Association Exercise, Cardiac Rehabilitation, and Prevention Committee, the Council on Clinical Cardiology; the Councils on Cardiovascular Nursing, Epidemiology and Prevention, and Nutrition, Physical Activity, and Metabolism; and the American Association of Cardiovascular and Pulmonary Rehabilitation. Circulation 2007, 115, 2675–2682. [Google Scholar]
- Domínguez-Téllez, P.; Moral-Muñoz, J.A.; Salazar, A.; Casado-Fernández, E.; Lucena-Antón, D. Game-Based Virtual Reality Interventions to Improve Upper Limb Motor Function and Quality of Life After Stroke: Systematic Review and Meta-analysis. Games Health J. 2020, 9, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Sever, S.; Doherty, P.; Golder, S.; Harrison, A.S. Is improvement in depression in patients attending cardiac rehabilitation with new-onset depressive symptoms determined by patient characteristics? Open Heart 2020, 7, e001264. [Google Scholar] [CrossRef] [PubMed]
- Jolliffe, J.A.; Rees, K.; Taylor, R.S.; Thompson, D.; Oldridge, N.; Ebrahim, S. Exercise-based rehabilitation for coronary heart disease. Cochrane Database Syst. Rev. 2001, 6, Cd001800. [Google Scholar]
- Martin, B.J.; Hauer, T.; Arena, R.; Austford, L.D.; Galbraith, P.D.; Lewin, A.M.; Knudtson, M.L.; Ghali, W.A.; Stone, J.A.; Aggarwal, S.G. Cardiac rehabilitation attendance and outcomes in coronary artery disease patients. Circulation 2012, 126, 677–687. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Benjamin, E.J.; Virani, S.S.; Callaway, C.W.; Chamberlain, A.M.; Chang, A.R.; Cheng, S.; Chiuve, S.E.; Cushman, M.; Delling, F.N.; Deo, R.; et al. Heart Disease and Stroke Statistics-2018 Update: A Report From the American Heart Association. Circulation 2018, 137, e67–e492. [Google Scholar] [CrossRef]
- van Riet, E.E.; Hoes, A.W.; Wagenaar, K.P.; Limburg, A.; Landman, M.A.; Rutten, F.H. Epidemiology of heart failure: The prevalence of heart failure and ventricular dysfunction in older adults over time. A systematic review. Eur. J. Heart Fail. 2016, 18, 242–252. [Google Scholar] [CrossRef]
- Puymirat, E.; Simon, T.; Cayla, G.; Cottin, Y.; Elbaz, M.; Coste, P.; Lemesle, G.; Motreff, P.; Popovic, B.; Khalife, K.; et al. Acute Myocardial Infarction: Changes in Patient Characteristics, Management, and 6-Month Outcomes Over a Period of 20 Years in the FAST-MI Program (French Registry of Acute ST-Elevation or Non-ST-Elevation Myocardial Infarction) 1995 to 2015. Circulation 2017, 136, 1908–1919. [Google Scholar] [CrossRef] [PubMed]
- Agmon, M.; Perry, C.K.; Phelan, E.; Demiris, G.; Nguyen, H.Q. A pilot study of Wii Fit exergames to improve balance in older adults. J. Geriatr. Phys. 2011, 34, 161–167. [Google Scholar] [CrossRef] [Green Version]
- Bhakta, M.D.; Mookadam, F.; Wilansky, S. Cardiovascular disease in women. Future Cardiol. 2011, 7, 613–627. [Google Scholar] [CrossRef] [PubMed]
- Samayoa, L.; Grace, S.L.; Gravely, S.; Scott, L.B.; Marzolini, S.; Colella, T.J. Sex differences in cardiac rehabilitation enrollment: A meta-analysis. Can. J. Cardiol. 2014, 30, 793–800. [Google Scholar] [CrossRef] [PubMed] [Green Version]


| Study (Author, Year) | Group | Study Characteristics | Participant Characteristics | |
|---|---|---|---|---|
| Country; Study Design; Journal | Sample Size; Male Percentage; Age | CVD Diagnosis; Risk Factors or Comorbidities | ||
| Cacau et al. [38] (2013) | EG | Brazil; RCT; Rev Bras Cir Cardiovasc | 30; 43.0%; 49.2 ± 2.6 years | CAD; NR |
| CG | 30; 53.0%; 52.0 ± 2.4 years | |||
| Chuang et al. [39] (2006) | EG | Taiwan; RCT; Phys Ther | 10; 100%; 65.7 ± 14.5 years | CAD; AHT, DM2, DLP, SM |
| CG | 10; 100%; 63.7 ± 10.3 years | |||
| Garcia-Bravo et al. [42] (2020) | EG | Spain; RCT; Int J Environ Res Public Health | 10; 70.0%; 48.7 ± 6.7 years | CAD; NR |
| CG | 10; 100%; 53.7 ± 10.3 years | |||
| Gulick et al. [28] (2021) | EG | USA; RCT; J Med Internet Res | 41; 72.0% *; 61 ± 9.9 years * | MS; COPD |
| CG | 31; 72.0% *; 61 ± 9.9 years * | |||
| Jaarsma et al. [29] (2021) | EG | Sweden, Italy, Israel, Netherlands, Germany, USA; RCT; Eur J Heart Fail | 234; 72.0% ^; 66 ± 12.0 years | CHF; AHT, AF, CVA, COPD, DM2, MI |
| CG | 230; 70.0% ^; 67 ± 11.0 years | |||
| Klompstra et al. [40] (2014) | EG | Sweden; Single Intervention; BMC Geriatrics | 32; 68.8%; 63.0 ± 14.0 years | CHF; SM |
| Ruivo et al. [24] (2017) | EG | Ireland; RCT; J Cardiopulm Rehabil Prev | 16; 87.5%; 59.4 ± 11.8 years | MS; AHT, DLP; DM2, OB, SM |
| CG | 16; 75.0%; 60.4 ± 8.5 years | |||
| Vieira et al. [41] (2018) | EG | Portugal; RCT; Disabil Rehabil: Assist Technol | 11; 100%; 55.0 ± 9.0 years | CAD; AHT, DLP; DM2, OB, SM |
| CG1 | 11; 100%; 59.0 ± 11.3 years | |||
| CG2 | 11; 100%; 59.0 ± 5.8 years | |||
| Study | Intervention Characteristics | Intervention and Technology Description | Main Findings |
|---|---|---|---|
| Cacau et al. [38] | Supervised training; phase I; intervention length (NR); 2 sessions a day until hospital discharge; intensity (NR) | EG: Physiotherapeutic protocols: breathing exercises, airways clearance techniques, metabolic exercise, and motor exercise using VR CG (active): Physiotherapeutic protocols: breathing exercises, airways clearance techniques, metabolic exercise, and motor exercise | The EG had lower hospitalization length (EG: 9.5 ± 0.5 days; CG: 12.2 ± 0.9 days), as well as higher exercise capacity (6MWT) at post-intervention The EG had higher functional independence, better energy levels, and less pain, while no between-group differences were found in emotional reactions, physical ability, and social interaction (measured with the Nottingham Health Profile) |
| Chuang et al. [39] | Supervised training; phase II; 12 weeks; 2 sessions a week; <30 min or >30 min depending on the subject’s condition; 3 min of low intensity with progressive increase until they reach a score of 16 in Borg scale or target HR or V02 | EG: Treadmill with speed alteration and incline adjustments using Microsoft Direct 3D-constructed “virtual runner” model with “wraparound” screens CG (active): Treadmill with speed alteration and incline adjustments | The number of sessions needed to reach the target of 85% heart rate max and the target of 75% VO2 peak was lower in the EG than in the CG. Moreover, the maximum work rate achieved in the endurance training sessions was higher in the EG |
| Garcia-Bravo et al. [42] | Supervised training; phase II; 8 weeks; 2 sessions a week; 60 min a session; intensity adapted according to the limits of HR and sensation of effort | EG: warm-up (10 min), VR-based training (20 min), resistance exercise (endless belt) for 10 min and limb strength exercises with weight of 0.5–3.0 kg (10 min) and cool-down (10 min) CG (active): warm-up (10 min), aerobic exercise (treadmill for 30 min) and limb strength 0.5–3.0 kg (10 min) and cool-down (10 min) | No between-group differences in exercise capacity (metabolic equivalent of task and 6MWT), functional independence measure, recovery of heart rate after 6MWT, quality of life (Short Form Health Survey-36 Questionnaire), depression (Beck-II Depression Inventory), and satisfaction (Client Satisfaction Questionnaire). Moreover, no differences were found in adherence and adverse events during the intervention |
| Gulick et al. [28] | Supervised training; phase II; intervention length (NR); training frequency (NR); intensity (NR) | EG: Standard of care CR: 4 types of exercise equipment, including bionautica trail system (VR), stationary bikes, ellipticals, and hand rowing machines CG (active): Standard of care CR: 4 types of exercise equipment, including treadmills, stationary bikes, ellipticals, and hand rowing machines | Patient attendance was lower in the EG (58%) than in the CG (81%), with no correlation between the group and reasons for ending No between-group differences in education (5-question test), satisfaction (6-question examination), engagement (3-question test), and exercise capacity (6MWT) |
| Jaarsma et al. [29] | Home based; phase III; 48 weeks; 5 sessions a week; 30 min per session; intensity (NR) | EG: Standard practice at their referring center (usual care) and Nintendo Wii Sports with baseball, bowling, boxing, golf, and tennis CG (passive): Standard practice at their referring center (usual care): protocol-based physical activity advice from a heart failure team member | No between-group differences in exercise capacity (6MWT) at 3, 6, and 12 months, as well as in exercise motivation (15-question exercise motivation index), exercise self-efficacy (6-question exercise self-efficacy questionnaire), and self-reported physical activity (single item question) |
| Klompstra et al. [40] | Home based; phase III; 12 weeks; 7 sessions a week; 20 min per session; intensity (NR) | EG: Nintendo Wii sports. Advice 20 min everyday: bowling, tennis, baseball, golf, and boxing games | Exercise capacity (6MWT) increased from 501 ± 95 m to 521 ± 101 m. Fifty-three percent of the patients increased the distance more than 30 m, which was considered clinically relevant Lower New York Heart Association scale and shorter time since diagnosis (less than one year) were related to the increase in exercise capacity |
| Ruivo et al. [24] | Supervised training; phase II; 6 weeks; 2 sessions a week; 60 min per session; intensity monitored with individual target HR zones | EG: Aerobic, resistance, and flexibility training using 9 circuit stations Nintendo Wii sports (boxing and canoeing) CG (active): Aerobic, resistance, and flexibility training using 9 circuit stations and music video | Lower tendency for dropping out in the EG (6%) than in the CG (19%). Higher improvement in energy expenditure in the EG compared to the CG No between-group differences in the median individual attendance and the number of patients experiencing adverse events during the intervention. Moreover, no differences in changes in exercise capacity (metabolic equivalent of task), affect toward exercise (Positive and Negative Affect Scale), anxiety and depression (Hospital Anxiety and Depression Scale), and quality of life (MacNew) |
| Vieira et al. [41] | Mixed; phase III; 24 weeks; 3 sessions a week; 60 min per session approx.; two progressive levels of intensity: level 1 (65% of HR reserve) and after three months, level 2 (70% of HR reserve); intensity monitored with the Borg scale | EG: Education on cardiovascular risk factors and 10 exercises: a warm-up exercise, 7 exercises of conditioning workout aimed at enhancing muscular endurance and/or strength, and 2 exercises to increase limb flexibility using a computer and Kinect-rehab play CG1 (active): Education on cardiovascular risk factors and 10 exercises: a warm-up exercise, 7 exercises of conditioning workout aimed at enhancing muscular endurance and/or strength, and 2 exercises to increase limb flexibility using a paper booklet CG2 (passive): Usual care: Education on cardiovascular risk factors and daily walks encouraged | The EG showed an enhanced selective attention and conflict resolution ability (Stroop Test) in comparison with the two CGs In contrast, no between-group differences were found in the quality of life (MacNew), depression, anxiety, and stress (Depression, Anxiety, and Stress Scale 21) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Blasco-Peris, C.; Fuertes-Kenneally, L.; Vetrovsky, T.; Sarabia, J.M.; Climent-Paya, V.; Manresa-Rocamora, A. Effects of Exergaming in Patients with Cardiovascular Disease Compared to Conventional Cardiac Rehabilitation: A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2022, 19, 3492. https://doi.org/10.3390/ijerph19063492
Blasco-Peris C, Fuertes-Kenneally L, Vetrovsky T, Sarabia JM, Climent-Paya V, Manresa-Rocamora A. Effects of Exergaming in Patients with Cardiovascular Disease Compared to Conventional Cardiac Rehabilitation: A Systematic Review and Meta-Analysis. International Journal of Environmental Research and Public Health. 2022; 19(6):3492. https://doi.org/10.3390/ijerph19063492
Chicago/Turabian StyleBlasco-Peris, Carles, Laura Fuertes-Kenneally, Tomas Vetrovsky, José Manuel Sarabia, Vicente Climent-Paya, and Agustín Manresa-Rocamora. 2022. "Effects of Exergaming in Patients with Cardiovascular Disease Compared to Conventional Cardiac Rehabilitation: A Systematic Review and Meta-Analysis" International Journal of Environmental Research and Public Health 19, no. 6: 3492. https://doi.org/10.3390/ijerph19063492
APA StyleBlasco-Peris, C., Fuertes-Kenneally, L., Vetrovsky, T., Sarabia, J. M., Climent-Paya, V., & Manresa-Rocamora, A. (2022). Effects of Exergaming in Patients with Cardiovascular Disease Compared to Conventional Cardiac Rehabilitation: A Systematic Review and Meta-Analysis. International Journal of Environmental Research and Public Health, 19(6), 3492. https://doi.org/10.3390/ijerph19063492








