2.2. Presentation of the Study
The study was carried out with the collaboration of 13 family visitation centers (FVCs) that are located in 10 of the 19 Spanish autonomous communities. FVCs were part of the National Federation of Family Visitation Centers (FEDEPE-Federación Nacional de Puntos de Encuentro) which brought together 33 centers at national level. Up to 13 centers chose to participate in the research. The study focused on families with children with high interparental conflict, who attended the FVC by judicial referral. Interparental conflict was measured considering hostility, detachment and escalating distress through the judicial referral report and interviews conducted by the professionals of the FVCs (case history). The inclusion criteria for the study were as follows: the parents were legally separated, did not live in the same household, did not present an active restraining order for gender-based violence, and did not have severe pathological disorders. The FVCs obtained permission from the relevant public administrations to carry out the program. The FVC staff invited the users who met these conditions to participate in the Egokitzen program. The interventions of the study took place between 2016 and 2019.
The research used a quasi-experimental study. Participants were divided into the intervention group (IG) and the wait-list comparison group (CG). Descriptive information was collected from the parents by the FVC staff and data of the main variables of the study through the tests completed by the parents. Both groups of parents (IG and CG) completed the pre- and post-tests, and the IG group completed the questionnaires after 6 months and 12 months.
We used the following instruments to measure the symptomatology of parents and children.
Symptoms Checklist (SCL-90 [
20] in the Spanish version of González de Rivera et al. [
21]) to analyze the dimensions of Interpersonal Sensitivity, Depression, and Anxiety in the parents. Each dimension consists of 9, 13, and 10 items, respectively, which are presented on a 5-point Likert scale ranging from 0 (not at all) to 4 (a lot). The Cronbach alpha was α = 0.96.
The Child Behavior Checklist (CBCL [
22]) was applied to analyze the dimensions of Somatization, Anxiety-Depression, and Aggressiveness in children, as informed by the parents. It consists of 12, 13, and 18 items, respectively, and dimensions are rated on a 3-point Likert scale ranging from 0 (not true), 1 (sometimes true) to 2 (very often or quite often true). Cronbach’s alpha was α = 0.92.
The final sample of the study included 197 people. Initially, the FVCs contacted 1538 users who met the above-mentioned conditions to participate in the study. After explaining the program, 450 people (29.3%) showed an interest in participating, of whom 382 (84.5%) attended a personal interview.
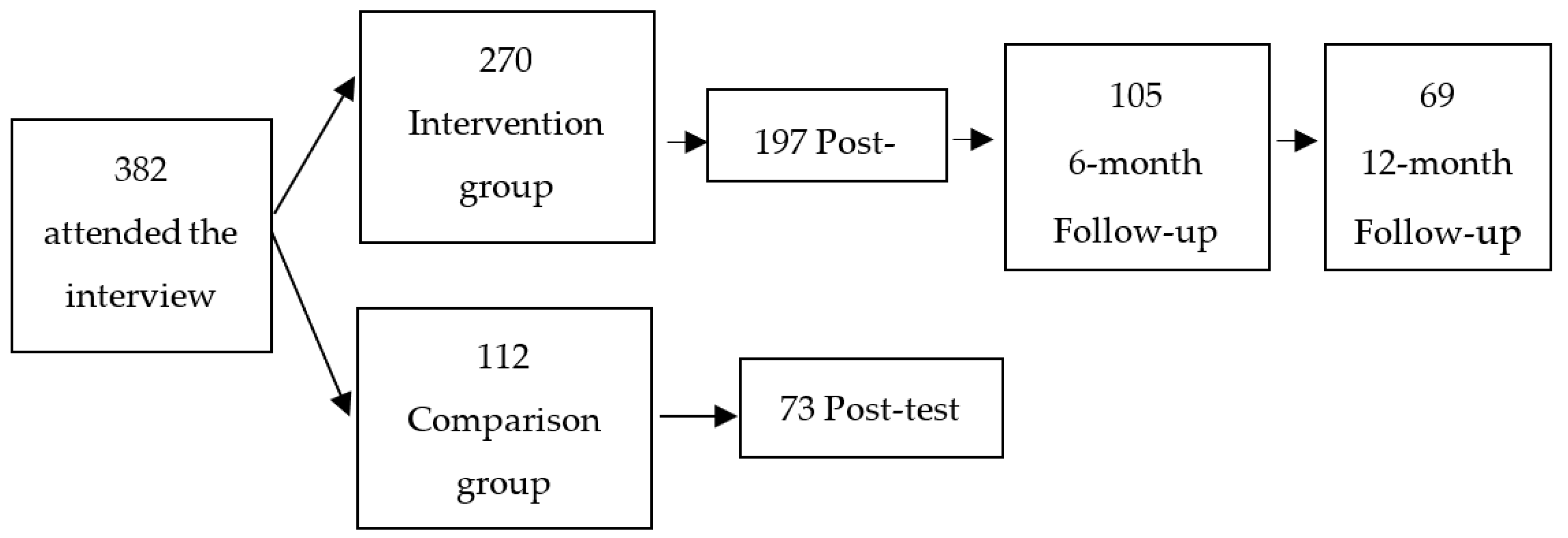
From the initial sample of 382 participants who, after the interview, signed informed consent and completed the evaluation protocol, 112 were part of the CG, and 270 participated in the IG. Of the 112 control participants, 73 people (attrition = 35%) completed the post-treatment questionnaire. Of the 270 intervention participants, 197 (attrition = 24%) responded to the test after the intervention. Of the 197 people, 105 completed the questionnaire at six months and 69 also completed the questionnaire 12 months after the intervention (see
Figure 1). Some of the reasons to arrive to the final sample were practical reasons, such as work schedule, group schedules or children’s difficulties. The number of drop-outs between pretest, posttest, 6-month and 12-month follow-ups was due to the length of the evaluation protocol or the lack of motivation to complete it as there was no economic or other type of compensation. There were no differences between the groups (those who dropped out or who did not) in any of the variables considered.
Of the parents who participated in the study, 61% were mothers (see
Table 1). The time since divorce was more than 3 years in 48% of the cases, 2 to 3 years in 13%, 1 to 2 years in 20% of the cases, and less than one year in 18% of the cases. Participants had an average of 1.5 children, and 22% had joint custody. For the purposes of the study, only one adult and one child per family were included. The average age of parents was 41.18 (SD = 6.49) and the average age of children was 8.40 (SD = 4.30).
The study was approved by the Ethics Committee of the University of Deusto (ETK-7/16-17). Participants were informed of the study from the outset and signed the consent document. None of the people involved in the intervention received an incentive to participate in the study.
2.3. Cost-Benefit Analysis
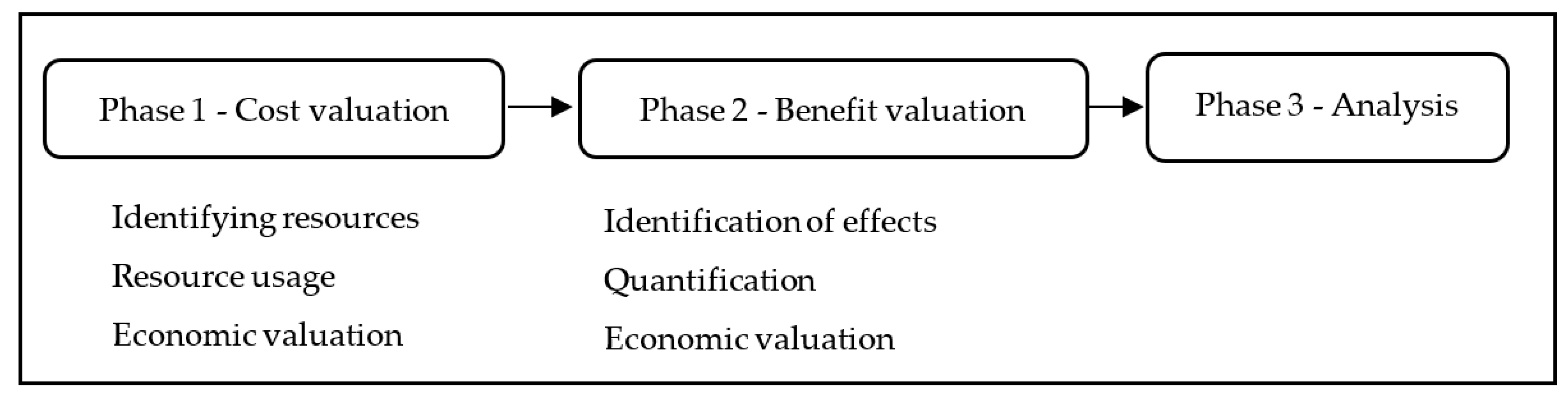
The cost-benefit analysis was carried out in three consecutive phases (see
Figure 2). In the first phase, we assessed the costs of implementing the program, following the methodology recommended by Foster et al. [
19]. Following this method, first, the different types of resources that were required were identified. In the second phase, the usage of those resources was measured. And finally, the usage of resources was valued in monetary units. This program presents two stages, one to train the trainers who will carry out the intervention and a second stage of the implementation of the intervention.
The resources required to carry out the training of the FVC workers are the trainers who taught the training course, trainers’ transportation, course materials, and course participants (FVC workers), considering this as an opportunity cost because while receiving the formation, they were not carrying out other normal activities of their position. The resources required to carry out the interventions are: FVC professionals, materials (reflection documents, theoretical reading content, cases with different situations to discuss in class, the evaluation protocol, pens or photocopies), and administration services for program management.
Table 2 presents the resources, the variables used to measure them, and the monetizing measures used, at both stages.
In the second phase, the effects achieved through the implementation of the Egokitzen program were valued. First, the main benefits of the program were identified, and then, quantified and, thirdly, valued in monetary units. In the case of the Egokitzen program, the identified benefits were a statistically significant improvement in the parents’ depressive symptomatology and the children’s anxiety when the parents’ global symptomatology improved, as can be seen in Martínez-Pampliega et al. [
17]. Situations not statistically significant were not considered in this phase.
The effects were then quantified. Based on the parents’ depressive symptomatology, a prevalence analysis was performed to observe how many IG parents’ depressive symptomatology improved or worsened compared to the control group. Based on the Spanish population standards of the SCL-90 [
21], we established cut-off points such that people whose personal score (
p) exceeded the standardized score (T) of 18.2 in mothers and 14.04 in the fathers were considered to have high levels of depression. This coincides with the 85th centile of those standards. Concerning child anxiety, we observed how many IG parents’ global symptomatology improved. Based on weighted data from the global symptomatology subscales included [
21], we established cut-off points such that people whose personal score exceeded the standardized score (mean plus one standard deviation) of 31.04 in mothers and 23.68 in fathers were considered to have high levels of global symptomatology. Next, a prevalence analysis was performed to determine how many children improved or worsened their anxiety when their parents had improved their global symptomatology, comparing the pre-test and post-test results.
Third, the effects were valued in monetary units. Several studies have calculated the costs of depression in different countries, through the savings both of direct (primary care, specialist, pharmacological) and indirect (loss of productivity) costs produced by a reduction in symptomatology [
23,
24]. In this case, we used the cost savings calculated by Salvador-Carulla et al. [
25], who carried out a study in a Spanish region with a health system similar to that of the regions that participated in this research. Concerning children’s anxiety, we used the cost savings calculated by Gustavsson et al. [
26]. Their study of direct and indirect costs was carried out for 30 European countries, including Spain. Direct costs include components such as visits to a general practitioner, hospital stays in mental health units (general hospital) and in acute care units (psychiatric hospital), visits to psychiatrists and psychologists, nurse and social work visits, or pharmacological treatment (dispensed prescriptions of anti-depressants, antipsychotics, anxiolytics and antiepileptic). While indirect costs include items such as, temporary disability for depression diagnosis in terms of working days lost and permanent disability for depression (early retirement). Although there are more recent cost-of-illness studies, such as Pella et al. [
27], the studies conducted by Salvador-Carulla et al. [
25] and Gustavsson et al. [
26] are closer to the cost structure of the Spanish health institutional framework and, therefore, this work follows them. All figures were converted to monetary units at the time of this study to be comparable, using variations in the Consumer Price Index (CPI) [
28].
The final impact of the program was determined in the third phase taking into account the benefits achieved and the costs required. This shows whether the funds invested in the Egokitzen program had a positive economic impact on society.
Finally, a sensitivity analysis was carried out to analyze the effects of the global outcome of the project, changes both in the costs and in the estimation of benefits.