Depression before and during-COVID-19 by Gender in the Korean Population
Abstract
:1. Introduction
2. Materials and Methods
2.1. Data
2.2. Participants
2.3. Variables
2.4. Statistical Analysis
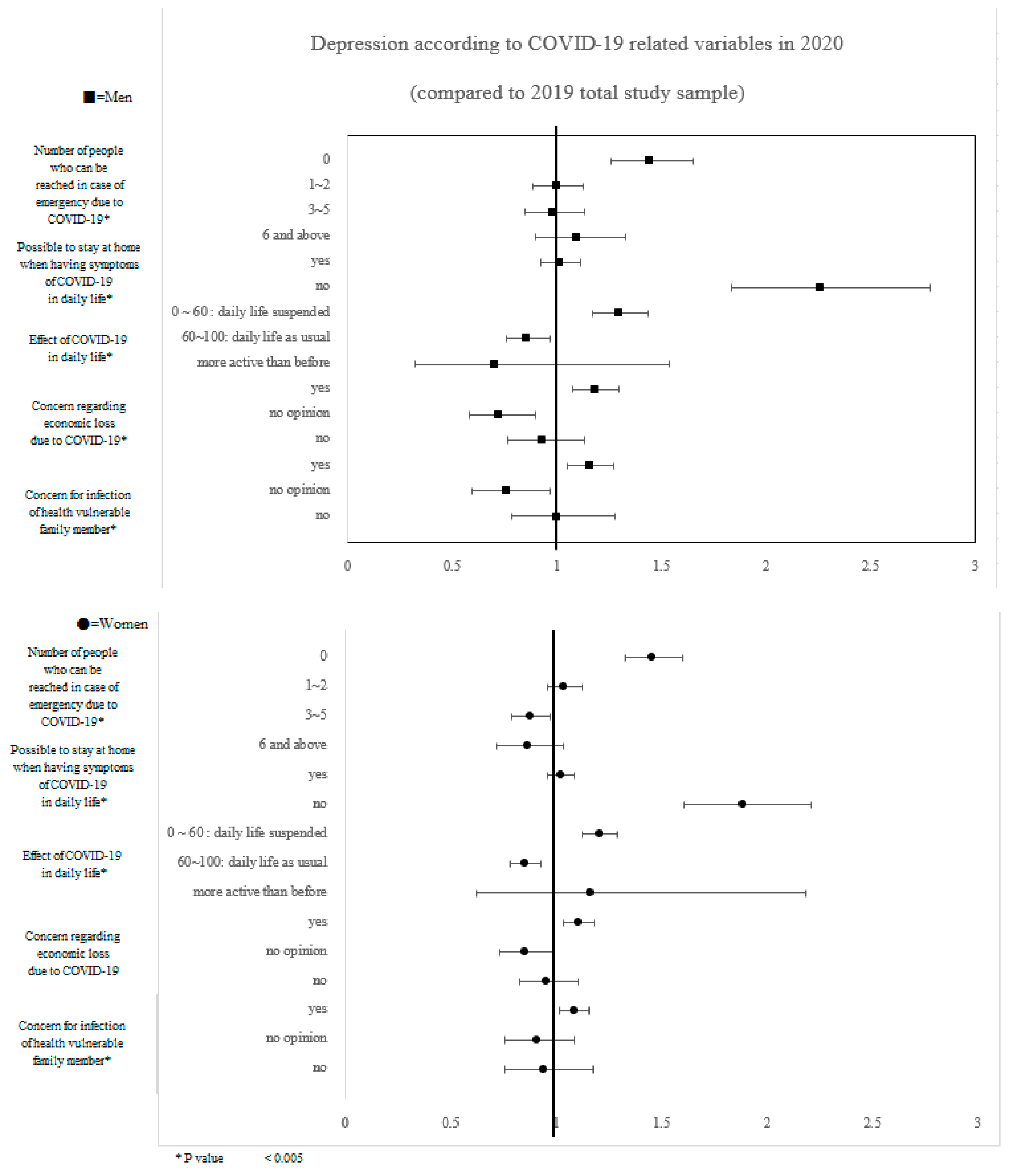
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kim, J.Y.; Choe, P.G.; Oh, Y.; Oh, K.J.; Kim, J.; Park, S.J.; Park, J.H.; Na, H.K.; Oh, M.-D. The First Case of 2019 Novel coronavirus pneumonia imported into Korea from Wuhan, China: Implication for infection prevention and control measures. J. Korean Med. Sci. 2020, 35, e61. [Google Scholar] [CrossRef] [PubMed]
- Pfefferbaum, B.; North, C.S. Mental health and the COVID-19 pandemic. N. Engl. J. Med. 2020, 383, 510–512. [Google Scholar] [CrossRef] [PubMed]
- Cullen, W.; Gulati, G.; Kelly, B.D. Mental health in the COVID-19 pandemic. QJM Int. J. Med. 2020, 113, 311–312. [Google Scholar] [CrossRef] [PubMed]
- Talevi, D.; Socci, V.; Carai, M.; Carnaghi, G.; Faleri, S.; Trebbi, E.; Di Bernardo, A.; Capelli, F.; Pacitti, F. Mental health outcomes of the COVID-19 pandemic. Riv. Psichiatr. 2020, 55, 137–144. [Google Scholar]
- Smith, K.; De Torres, I. A world of depression. Nature 2014, 515, 181. [Google Scholar] [CrossRef]
- Dunn, E.C.; Brown, R.C.; Dai, Y.; Rosand, J.; Nugent, N.R.; Amstadter, A.B.; Smoller, J.W. Genetic determinants of depression: Recent findings and future directions. Harv. Rev. Psychiatry 2015, 23, 1. [Google Scholar] [CrossRef] [Green Version]
- Riso, L.P.; Miyatake, R.K.; Thase, M.E. The search for determinants of chronic depression: A review of six factors. J. Affect. Disord. 2002, 70, 103–115. [Google Scholar] [CrossRef]
- George, L.K.; Blazer, D.G.; Hughes, D.C.; Fowler, N. Social Support and the Outcome of Major Depression. Br. J. Psychiatry 1989, 154, 478–485. [Google Scholar] [CrossRef]
- Tiller, J.W. Depression and anxiety. Med. J. Aust. 2013, 199, S28–S31. [Google Scholar] [CrossRef]
- Choi, E.P.H.; Hui, B.P.H.; Wan, E.Y.F. Depression and anxiety in Hong Kong during COVID-19. Int. J. Environ. Res. Public Health 2020, 17, 3740. [Google Scholar] [CrossRef]
- Hyland, P.; Shevlin, M.; McBride, O.; Murphy, J.; Karatzias, T.; Bentall, R.P.; Martinez, A.; Vallières, F. Anxiety and depression in the Republic of Ireland during the COVID-19 pandemic. Acta Psychiatr. Scand. 2020, 142, 249–256. [Google Scholar] [CrossRef] [PubMed]
- Yoo, J.-H.; Hong, S.-T. The outbreak cases with the novel coronavirus suggest upgraded quarantine and isolation in Korea. J. Korean Med. Sci. 2020, 35, e62. [Google Scholar] [CrossRef] [PubMed]
- Setyawan, F.E.B.; Lestari, R. Challenges of stay-at-home policy implementation during the Coronavirus (COVID-19) pandemic in Indonesia. J. Adm. Kesehat. Indones. 2020, 8, 15–20. [Google Scholar] [CrossRef]
- Kutlu, Ö.; Güneş, R.; Coerdt, K.; Metin, A.; Khachemoune, A. The effect of the “stay-at-home” policy on requests for dermatology outpatient clinic visits after the COVID-19 outbreak. Dermatol. Ther. 2020, 33, e13581. [Google Scholar] [CrossRef]
- Brodeur, A.; Grigoryeva, I.; Kattan, L. Stay-at-home orders, social distancing, and trust. J. Popul. Econ. 2021, 34, 1321–1354. [Google Scholar] [CrossRef]
- Jeong, H.; Yim, H.W.; Song, Y.-J.; Ki, M.; Min, J.-A.; Cho, J.; Chae, J.-H. Mental health status of people isolated due to Middle East Respiratory Syndrome. Epidemiol. Health 2016, 38, e2016048. [Google Scholar] [CrossRef]
- Brooks, S.K.; Webster, R.K.; Smith, L.E.; Woodland, L.; Wessely, S.; Greenberg, N.; Rubin, G.J. The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. Lancet 2020, 395, 912–920. [Google Scholar] [CrossRef] [Green Version]
- Chan, S.M.S.; Chiu, F.K.H.; Lam, C.W.L.; Leung, P.Y.V.; Conwell, Y. Elderly suicide and the 2003 SARS epidemic in Hong Kong. Int. J. Geriatr. Psychiatry 2006, 21, 113–118. [Google Scholar] [CrossRef]
- Aum, S.; Lee, S.Y.; Shin, Y. COVID-19 doesn’t need lockdowns to destroy jobs: The effect of local outbreaks in Korea. Labour Econ. 2021, 70, 101993. [Google Scholar] [CrossRef]
- Cajner, T.; Crane, L.D.; Decker, R.A.; Grigsby, J.; Hamins-Puertolas, A.; Hurst, E.; Kurz, C.; Yildirmaz, A. The US Labor Market during the Beginning of the Pandemic Recession; National Bureau of Economic Research: Cambridge, MA, USA, 2020. [Google Scholar]
- Tedeschi, E.; Bui, Q. America’s employment losses might be slowing: Job tracker. The New York Times, 16 June 2020. [Google Scholar]
- Gardiner, L.; Slaughter, H. The effects of the coronavirus crisis on workers. Resolut. Found. 2020, 1–8. [Google Scholar]
- Kim, A.M. The short-term impact of the COVID-19 outbreak on suicides in Korea. Psychiatry Res. 2020, 295, 113632. [Google Scholar] [CrossRef] [PubMed]
- Gunnell, D.; Appleby, L.; Arensman, E.; Hawton, K.; John, A.; Kapur, N.; Khan, M.; O’Connor, R.C.; Pirkis, J.; Caine, E.D. Suicide risk and prevention during the COVID-19 pandemic. Lancet Psychiatry 2020, 7, 468–471. [Google Scholar] [CrossRef]
- Reger, M.A.; Stanley, I.H.; Joiner, T.E. Suicide mortality and coronavirus disease 2019—A perfect storm? JAMA Psychiatry 2020, 77, 1093–1094. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lee, H.-S.; Dean, D.; Baxter, T.; Griffith, T.; Park, S. Deterioration of mental health despite successful control of the COVID-19 pandemic in South Korea. Psychiatry Res. 2021, 295, 113570. [Google Scholar] [CrossRef] [PubMed]
- Zhao, B.; Kong, F.; Aung, M.N.; Yuasa, M.; Nam, E.W. Novel coronavirus (COVID-19) knowledge, precaution practice, and associated depression symptoms among university students in Korea, China, and Japan. Int. J. Environ. Res. Public Health 2020, 17, 6671. [Google Scholar] [CrossRef]
- Choi, S.; Byoun, S.-J.; Kim, E.H. Unwed single mothers in South Korea: Increased vulnerabilities during the COVID-19 pandemic. Int. Soc. Work 2020, 63, 676–680. [Google Scholar] [CrossRef]
- Yoo, H.J.; Shim, J.; Kim, N. Life-changing experiences of mothers with school-age children during the COVID-19 pandemic: Focusing on their health risk perceptions and health-related behaviors. Int. J. Environ. Res. Public Health 2021, 18, 4523. [Google Scholar] [CrossRef]
- Lee, H.; Han, B. The impact of school closures on adolescent health-related outcomes during the COVID-19 pandemic: A natural experiment in South Korea. medRxiv 2021. [Google Scholar] [CrossRef]
- Kim, E.S.; Kwon, Y.; Choe, Y.H.; Kim, M.J. COVID-19-related school closing aggravate obesity and glucose intolerance in pediatric patients with obesity. Sci. Rep. 2021, 11, 5494. [Google Scholar] [CrossRef]
- Spanagel, R.; Noori, H.R.; Heilig, M. Stress and alcohol interactions: Animal studies and clinical significance. Trends Neurosci. 2014, 37, 219–227. [Google Scholar] [CrossRef]
- Fidler, J.A.; West, R. Self-perceived smoking motives and their correlates in a general population sample. Nicotine Tob. Res. 2009, 11, 1182–1188. [Google Scholar] [CrossRef] [PubMed]
- An, R.; Xiang, X. Smoking, heavy drinking, and depression among US middle-aged and older adults. Prev. Med. 2015, 81, 295–302. [Google Scholar] [CrossRef] [PubMed]
- Jang, B.N.; Youn, H.M.; Lee, D.W.; Joo, J.H.; Park, E.-C. Association between community deprivation and practising health behaviours among South Korean adults: A survey-based cross-sectional study. BMJ Open 2021, 11, e047244. [Google Scholar] [CrossRef]
- Jang, S.-I.; Bae, H.-C.; Shin, J.; Jang, S.-y.; Hong, S.; Han, K.-T.; Park, E.-C. Depression in the family of patients with dementia in Korea. Am. J. Alzheimer Dis. Dement. 2016, 31, 481–491. [Google Scholar] [CrossRef] [PubMed]
- Park, M.; Nari, F.; Kang, S.H.; Jang, S.-I.; Park, E.-C. Association between living with patients with dementia and family caregivers’ depressive symptoms—Living with dementia patients and family caregivers’ depressive symptoms. Int. J. Environ. Res. Public Health 2021, 18, 4372. [Google Scholar] [CrossRef] [PubMed]
- Kroenke, K.; Spitzer, R.L.; Williams, J.B. The PHQ-9: Validity of a brief depression severity measure. J. Gen. Int. Med. 2001, 16, 606–613. [Google Scholar] [CrossRef] [PubMed]
- Sun, Y.; Fu, Z.; Bo, Q.; Mao, Z.; Ma, X.; Wang, C. The reliability and validity of PHQ-9 in patients with major depressive disorder in psychiatric hospital. BMC Psychiatry 2020, 20, 474. [Google Scholar] [CrossRef]
- Manea, L.; Gilbody, S.; McMillan, D. Optimal cut-off score for diagnosing depression with the Patient Health Questionnaire (PHQ-9): A meta-analysis. Can. Med. Assoc. J. 2012, 184, E191–E196. [Google Scholar] [CrossRef] [Green Version]
- Park, J.; Lee, W.-C.; Jeong, H.; Hong, N.; Bae, B.; Yim, H.W. Characteristic of depressive symptom in middle-aged family members with Dementia patient: 2017 Korea Community Health Survey. Epidemiol. Health 2020, 42, e2020031. [Google Scholar] [CrossRef]
- Kim, E.; Shin, M.-H.; Yang, J.-H.; Ahn, S.-K.; Na, B.-J.; Nam, H.-S. Association of regional-level perceived stress and depression with health related quality-of-life of Korean adults: A multilevel analysis of 2017 Korea Community Health Survey data. Epidemiol. Health 2021, 43, e2021062. [Google Scholar] [CrossRef]
- Choi, S.C.; Ki, M. Estimating the reproductive number and the outbreak size of COVID-19 in Korea. Epidemiol. Health 2020, 42, e2020011. [Google Scholar] [CrossRef] [PubMed]
- Korean Society of Infectious Diseases; Korean Society of Pediatric Infectious Diseases; Korean Society of Epidemiology; Korean Society for Antimicrobial Therapy; Korean Society for Healthcare-Associated Infection Control and Prevention; Korea Centers for Disease Control and Prevention. Report on the Epidemiological Features of Coronavirus Disease 2019 (COVID-19) Outbreak in the Republic of Korea from January 19 to March 2, 2020. J. Korean Med. Sci. 2020, 35, e112. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Wang, J.-X.; Yang, G.-S. The psychological impact of COVID-19 on Chinese individuals. Yonsei Med. J. 2020, 61, 438. [Google Scholar] [CrossRef] [PubMed]
- Khan, S.; Siddique, R.; Li, H.; Ali, A.; Shereen, M.A.; Bashir, N.; Xue, M. Impact of coronavirus outbreak on psychological health. J. Glob. Health 2020, 10, 010331. [Google Scholar] [CrossRef]
- Bai, Y.; Lin, C.-C.; Lin, C.-Y.; Chen, J.-Y.; Chue, C.-M.; Chou, P. Survey of stress reactions among health care workers involved with the SARS outbreak. Psychiatr. Serv. 2004, 55, 1055–1057. [Google Scholar] [CrossRef]
- Cava, M.A.; Fay, K.E.; Beanlands, H.J.; McCay, E.A.; Wignall, R. The experience of quarantine for individuals affected by SARS in Toronto. Public Health Nurs. 2005, 22, 398–406. [Google Scholar] [CrossRef]
- Desclaux, A.; Badji, D.; Ndione, A.G.; Sow, K. Accepted monitoring or endured quarantine? Ebola contacts’ perceptions in Senegal. Soc. Sci. Med. 2017, 178, 38–45. [Google Scholar] [CrossRef]
- Braunack-Mayer, A.; Tooher, R.; Collins, J.E.; Street, J.M.; Marshall, H. Understanding the school community’s response to school closures during the H1N1 2009 influenza pandemic. BMC Public Health 2013, 13, 344. [Google Scholar] [CrossRef] [Green Version]
- Narrow, W.; Regier, D.; Roe, D. The de facto mental and addictive disorders service system. Epidemiologic catchment area 1-year prevalence rates of disorders and services. Arch. Gen. Psychiatry 1993, 50, 85–94. [Google Scholar]
- Gold, P.W.; Chrousos, G.P. Organization of the stress system and its dysregulation in melancholic and atypical depression: High vs. low CRH/NE states. Mol. Psychiatry 2002, 7, 254–275. [Google Scholar] [CrossRef] [Green Version]
- Luine, V. Sex Differences in Chronic Stress Effects on Memory in Rats. Stress 2002, 5, 205–216. [Google Scholar] [CrossRef] [PubMed]
- Altemus, M. Sex differences in depression and anxiety disorders: Potential biological determinants. Horm. Behav. 2006, 50, 534–538. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.; Kim, S.L.; Park, E.K.; Yun, S. Social support, work-family conflict, and emotional exhaustion in South Korea. Psychol. Rep. 2013, 113, 619–634. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.; Kwon, H.-Y.; Lee, S.; Kim, C.-B. Depression during COVID-19 quarantine in South Korea: A propensity score-matched analysis. Front. Public Health 2021, 9, 743625. [Google Scholar] [CrossRef]
- Ju, Y.J.; Kim, W.; Lee, S.Y. Perceived social support and depressive symptoms during the COVID-19 pandemic: A nationally-representative study. Int. J. Soc. Psychiatry 2022, 1–9. [Google Scholar] [CrossRef]
- Chang, M.C.; Baek, J.H.; Park, D. Lessons from South Korea regarding the early stage of the COVID-19 outbreak. Healthcare 2020, 8, 229. [Google Scholar] [CrossRef]
- Kang, Y.-J. Lessons learned from cases of COVID-19 infection in South Korea. Disaster Med. Public Health Prep. 2020, 14, 818–825. [Google Scholar] [CrossRef]
- Kim, J.-H.; An, J.A.-R.; Min, P.-K.; Bitton, A.; Gawande, A.A. How South Korea responded to the COVID-19 outbreak in Daegu. NEJM Catal. Innov. Care Deliv. 2020, 1, 4. [Google Scholar] [CrossRef]
| Variables | PHQ-9 Score ≥ 10 (Depression) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Male | Female | |||||||||||
| Total | Yes | No | p-Value | Total | Yes | No | p-Value | |||||
| N | N | % | N | % | N | N | % | N | % | |||
| Total (N = 444,051) | 200,206 | 4131 | 2.1 | 196,075 | 97.9 | 243,845 | 9356 | 3.8 | 234,489 | 96.2 | ||
| Year | 0.0005 | <0.0001 | ||||||||||
| 2019 | 99,396 | 2162 | 2.2 | 97,234 | 97.8 | 122,349 | 5060 | 4.1 | 117,289 | 95.9 | ||
| 2020 | 100,810 | 1969 | 2.0 | 98,841 | 98.0 | 121,496 | 4296 | 3.5 | 117,200 | 96.5 | ||
| Generations residing in one household | <0.0001 | <0.0001 | ||||||||||
| One | 96,149 | 2325 | 2.4 | 93,824 | 97.6 | 118,682 | 5110 | 4.3 | 113,572 | 95.7 | ||
| Two (parents and children) | 91,743 | 1586 | 1.7 | 90,157 | 98.3 | 107,804 | 3607 | 3.3 | 104,197 | 96.7 | ||
| Three (grandparents and grandchildren) | 12,314 | 220 | 1.8 | 12,094 | 98.2 | 17,359 | 639 | 3.7 | 16,720 | 96.3 | ||
| Occupational status | <0.0001 | <0.0001 | ||||||||||
| Employer or self employed | 54,981 | 700 | 1.3 | 54,281 | 98.7 | 27,710 | 751 | 2.7 | 26,959 | 97.3 | ||
| Employee | 87,789 | 1176 | 1.3 | 86,613 | 98.7 | 84,544 | 2234 | 2.6 | 82,310 | 97.4 | ||
| Unoccupied (students, housewives, etc.) | 57,436 | 2255 | 3.9 | 55,181 | 96.1 | 131,591 | 6371 | 4.8 | 125,220 | 95.2 | ||
| Age | <0.0001 | <0.0001 | ||||||||||
| 19–29 | 23,139 | 511 | 2.2 | 22,628 | 97.8 | 24,778 | 1137 | 4.6 | 23,641 | 95.4 | ||
| 30–39 | 24,087 | 504 | 2.1 | 23,583 | 97.9 | 26,529 | 1008 | 3.8 | 25,521 | 96.2 | ||
| 40–49 | 32,841 | 565 | 1.7 | 32,276 | 98.3 | 36,984 | 951 | 2.6 | 36,033 | 97.4 | ||
| 50–59 | 39,285 | 619 | 1.6 | 38,666 | 98.4 | 46,656 | 1225 | 2.6 | 45,431 | 97.4 | ||
| 60–69 | 39,470 | 671 | 1.7 | 38,799 | 98.3 | 47,819 | 1477 | 3.1 | 46,342 | 96.9 | ||
| ≥70 | 41,384 | 1261 | 3.0 | 40,123 | 97.0 | 61,079 | 3558 | 5.8 | 57,521 | 94.2 | ||
| Marital status | <0.0001 | <0.0001 | ||||||||||
| Living with spouse | 138,878 | 2174 | 1.6 | 136,704 | 98.4 | 148,261 | 4163 | 2.8 | 144,098 | 97.2 | ||
| Living without spouse | 61,328 | 1957 | 3.2 | 59,371 | 96.8 | 95,584 | 5193 | 5.4 | 90,391 | 94.6 | ||
| Region | <0.0001 | 0.0001 | ||||||||||
| Daegu, Kyungbuk | 25,594 | 499 | 1.9 | 25,095 | 98.1 | 31,255 | 1175 | 3.8 | 30,080 | 96.2 | ||
| Seoul, Kyunggi | 56,890 | 1309 | 2.3 | 55,581 | 97.7 | 68,148 | 2824 | 4.1 | 65,324 | 95.9 | ||
| Urban (Daejeon, Ulsan, Gwangju, Incheon, Busan) | 32,568 | 684 | 2.1 | 31,884 | 97.9 | 40,308 | 1552 | 3.9 | 38,756 | 96.1 | ||
| Others | 85,154 | 1639 | 1.9 | 83,515 | 98.1 | 104,134 | 3805 | 3.7 | 100,329 | 96.3 | ||
| Educational level | <0.0001 | <0.0001 | ||||||||||
| Middle school or less | 51,295 | 1578 | 3.1 | 49,717 | 96.9 | 101,038 | 4928 | 4.9 | 96,110 | 95.1 | ||
| High school | 63,488 | 1252 | 2.0 | 62,236 | 98.0 | 64,822 | 2213 | 3.4 | 62,609 | 96.6 | ||
| College or over | 85,423 | 1301 | 1.5 | 84,122 | 98.5 | 77,985 | 2215 | 2.8 | 75,770 | 97.2 | ||
| Household income * | <0.0001 | <0.0001 | ||||||||||
| Below 2000 | 49,528 | 1980 | 4.0 | 47,548 | 96.0 | 78,034 | 4709 | 6.0 | 73,325 | 94.0 | ||
| Below 3600 | 37,820 | 685 | 1.8 | 37,135 | 98.2 | 42,460 | 1505 | 3.5 | 40,955 | 96.5 | ||
| Below 6000 | 53,701 | 812 | 1.5 | 52,889 | 98.5 | 57,585 | 1638 | 2.8 | 55,947 | 97.2 | ||
| 6000 and above | 59,157 | 654 | 1.1 | 58,503 | 98.9 | 65,766 | 1504 | 2.3 | 64,262 | 97.7 | ||
| Cigarette use (either conventional or electronic) | <0.0001 | |||||||||||
| Yes | 67,520 | 1744 | 2.6 | 65,776 | 97.4 | 7116 | 857 | 12.0 | 6259 | 88.0 | ||
| No | 132,686 | 2387 | 1.8 | 130,299 | 98.2 | 236,729 | 8499 | 3.6 | 228,230 | 96.4 | ||
| Current alcohol use | <0.0001 | <0.0001 | ||||||||||
| Frequently | 64,194 | 1206 | 1.9 | 62,988 | 98.1 | 119,487 | 5185 | 4.3 | 114,302 | 95.7 | ||
| Occasionally | 81,988 | 1314 | 1.6 | 80,674 | 98.4 | 102,832 | 3160 | 3.1 | 99,672 | 96.9 | ||
| None | 54,024 | 1611 | 3.0 | 52,413 | 97.0 | 21,526 | 1011 | 4.7 | 20,515 | 95.3 | ||
| Perceived condition of health | <0.0001 | <0.0001 | ||||||||||
| Good | 173,058 | 1871 | 1.1 | 171,187 | 98.9 | 194,166 | 3892 | 2.0 | 190,274 | 98.0 | ||
| Bad | 27,148 | 2260 | 8.3 | 24,888 | 91.7 | 49,679 | 5464 | 11.0 | 44,215 | 89.0 | ||
| Variables | PHQ-9 Score ≥ 10 (Depression) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Male | p-Value | Female | p-Value | |||||||
| OR | 95% CI | OR | 95% CI | |||||||
| Year | ||||||||||
| 2019 | 1.000 | 1.000 | ||||||||
| 2020 | 1.092 | 0.998 | - | 1.195 | 0.0559 | 1.066 | 1.002 | - | 1.134 | 0.0418 |
| Generations residing in one household | ||||||||||
| One | 1.000 | 1.000 | ||||||||
| Two (parents and children) | 0.949 | 0.848 | - | 1.062 | 0.6334 | 1.068 | 0.990 | - | 1.152 | 0.6705 |
| Three (grandparents and grandchildren) | 0.955 | 0.780 | - | 1.169 | 0.8348 | 1.180 | 1.040 | - | 1.340 | 0.0276 |
| Occupational status | ||||||||||
| Employer or self employed | 1.000 | 1.000 | ||||||||
| Employee | 0.951 | 0.829 | - | 1.092 | <0.0001 | 0.858 | 0.762 | - | 0.965 | <0.0001 |
| Unoccupied (students, housewives, etc.) | 1.504 | 1.311 | - | 1.726 | <0.0001 | 1.113 | 0.996 | - | 1.245 | <0.0001 |
| Age (years) | ||||||||||
| 19–29 | 2.335 | 1.873 | - | 2.909 | <0.0001 | 2.801 | 2.417 | - | 3.246 | <0.0001 |
| 30–39 | 2.947 | 2.408 | - | 3.606 | <0.0001 | 2.665 | 2.302 | - | 3.084 | <0.0001 |
| 40–49 | 1.910 | 1.583 | - | 2.304 | 0.0016 | 1.910 | 1.583 | - | 2.304 | 0.7575 |
| 50–59 | 1.327 | 1.124 | - | 1.567 | 0.0002 | 1.327 | 1.124 | - | 1.567 | <0.0001 |
| 60–69 | 0.994 | 0.863 | - | 1.144 | <0.0001 | 0.994 | 0.863 | - | 1.144 | <0.0001 |
| ≥70 | 1.000 | 1.000 | ||||||||
| Marital status | ||||||||||
| Living with spouse | 1.000 | 1.000 | ||||||||
| Living without spouse | 1.456 | 1.311 | - | 1.618 | <0.0001 | 1.367 | 1.278 | - | 1.464 | <0.0001 |
| Region | ||||||||||
| Daegu, Kyungbuk | 0.981 | 0.841 | - | 1.143 | 0.0115 | 1.049 | 0.947 | - | 1.161 | 0.1222 |
| Seoul, Kyunggi | 1.530 | 1.370 | - | 1.710 | <0.0001 | 1.329 | 1.230 | - | 1.435 | <0.0001 |
| Urban (Daejeon, Ulsan, Gwangju, Incheon, Busan) | 1.051 | 0.926 | 1.192 | 0.1254 | 1.074 | 0.983 | 1.174 | 0.317 | ||
| Others | 1.000 | 1.000 | ||||||||
| Educational level | ||||||||||
| Middle school or less | 1.484 | 1.263 | - | 1.745 | <0.0001 | 1.307 | 1.157 | - | 1.476 | 0.0256 |
| High school | 1.242 | 1.104 | - | 1.398 | 0.6948 | 1.355 | 1.236 | - | 1.484 | <0.0001 |
| College or over | 1.000 | 1.000 | ||||||||
| Household income * | ||||||||||
| Below 2000 | 2.262 | 1.944 | - | 2.632 | <0.0001 | 2.114 | 1.901 | - | 2.351 | <0.0001 |
| Below 3600 | 1.494 | 1.276 | - | 1.749 | 0.5937 | 1.507 | 1.358 | - | 1.672 | 0.0384 |
| Below 6000 | 1.333 | 1.165 | 1.526 | 0.0386 | 1.254 | 1.143 | - | 1.376 | <0.0001 | |
| 6000 and above | 1.000 | 1.000 | ||||||||
| Current cigarette use (either conventional or electronic) | ||||||||||
| Yes | 1.587 | 1.446 | - | 1.741 | <0.0001 | 2.518 | 2.246 | - | 2.822 | <0.0001 |
| No | 1.000 | 1.000 | ||||||||
| Current alcohol Use | ||||||||||
| Frequently | 1.032 | 0.919 | - | 1.158 | 0.0120 | 1.555 | 1.400 | - | 1.727 | <0.0001 |
| Occasionally | 0.826 | 0.740 | - | 0.921 | <0.0001 | 1.097 | 1.024 | - | 1.175 | 0.000 |
| None | 1.000 | 1.000 | ||||||||
| Perceived condition of health | ||||||||||
| Good | 1.000 | 1.000 | ||||||||
| Bad | 7.606 | 6.905 | - | 8.379 | <0.0001 | 6.501 | 6.073 | - | 6.959 | <0.0001 |
| Variables | PHQ-9 Score of 10 or Above | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Year | ||||||||||
| Male | Female | |||||||||
| 2020 | 2019 | 2020 | 2019 | |||||||
| OR | 95% CI | OR | OR | 95% CI | OR | |||||
| Generations residing in one household | ||||||||||
| One | 1.00 | 0.88 | - | 1.13 | 1.00 | 1.06 | 0.98 | - | 1.16 | 1.00 |
| Two (parents and children) | 1.16 | 1.01 | - | 1.33 | 1.00 | 1.06 | 0.97 | - | 1.16 | 1.00 |
| Three (grandparents and grandchildren) | 1.21 | 0.82 | - | 1.77 | 1.00 | 1.11 | 0.88 | - | 1.39 | 1.00 |
| Occupational status | ||||||||||
| Employer or self employed | 1.13 | 0.91 | - | 1.42 | 1.00 | 1.10 | 0.89 | - | 1.35 | 1.00 |
| Employee | 1.14 | 0.98 | - | 1.32 | 1.00 | 1.08 | 0.96 | - | 1.21 | 1.00 |
| Unemployed (students, homemakers, etc.) | 1.03 | 0.91 | - | 1.16 | 1.00 | 1.05 | 0.97 | - | 1.13 | 1.00 |
| Age (years) | ||||||||||
| 19–29 | 1.08 | (0.87 | - | 1.34) | 1.00 | 1.01 | (0.87 | - | 1.17) | 1.00 |
| 30–39 | 1.40 | (1.12 | - | 1.75) | 1.00 | 1.07 | (0.91 | - | 1.26) | 1.00 |
| 40–49 | 0.94 | (0.75 | - | 1.17) | 1.00 | 1.23 | (1.03 | - | 1.45) | 1.00 |
| 50–59 | 1.12 | 0.90 | - | 1.41 | 1.00 | 1.21 | (1.02 | - | 1.42) | 1.00 |
| 60–69 | 1.07 | (0.86 | - | 1.34) | 1.00 | 0.97 | (0.84 | - | 1.13) | 1.00 |
| ≥70 | 0.93 | (0.79 | - | 1.10) | 1.00 | 0.98 | (0.88 | - | 1.09) | 1.00 |
| Marital status | ||||||||||
| Living with spouse | 1.11 | (0.98 | - | 1.25) | 1.00 | 1.07 | (0.97 | - | 1.17) | 1.00 |
| Living without spouse | 1.06 | (0.93 | - | 1.20) | 1.00 | 1.07 | (0.98 | - | 1.16) | 1.00 |
| Region | ||||||||||
| Daegu, Kyungbuk | 0.86 | (0.66 | - | 1.11) | 1.00 | 1.08 | (0.91 | - | 1.28) | 1.00 |
| Seoul, Kyunggi | 1.12 | (0.97 | - | 1.29) | 1.00 | 1.13 | (1.02 | - | 1.24) | 1.00 |
| Urban (Daejeon, Ulsan, Gwangju, Incheon, Busan) | 1.15 | (0.95 | - | 1.41) | 1.00 | 1.10 | (0.96 | - | 1.27) | 1.00 |
| Others | 1.10 | (0.93 | - | 1.30) | 1.00 | 0.94 | (0.84 | - | 1.06) | 1.00 |
| Educational level | ||||||||||
| Middle school or less | 1.04 | (0.88 | - | 1.22) | 1.00 | 1.01 | (0.93 | - | 1.10) | 1.00 |
| High school | 1.07 | (0.91 | - | 1.26) | 1.00 | 1.07 | (0.95 | - | 1.21) | 1.00 |
| College or over | 1.14 | (0.99 | - | 1.31) | 1.00 | 1.11 | (0.99 | - | 1.23) | 1.00 |
| Household income * | ||||||||||
| Below 2000 | 1.00 | (0.88 | - | 1.15) | 1.00 | 1.02 | (0.93 | - | 1.11) | 1.00 |
| Below 3600 | 1.14 | (0.91 | - | 1.42) | 1.00 | 1.03 | (0.89 | - | 1.20) | 1.00 |
| Below 6000 | 1.15 | (0.96 | - | 1.39) | 1.00 | 1.19 | (1.04 | - | 1.37) | 1.00 |
| 6000 and above | 1.12 | (0.91 | - | 1.36) | 1.00 | 1.04 | (0.91 | - | 1.19) | 1.00 |
| Current cigarette use (either conventional or electronic) | ||||||||||
| Yes | 1.12 | (0.98 | - | 1.27) | 1.00 | 1.35 | (1.11 | - | 1.65) | 1.00 |
| No | 1.07 | (0.95 | - | 1.21) | 1.00 | 1.04 | (0.98 | - | 1.11) | 1.00 |
| Current alcohol use | ||||||||||
| Frequently | 1.27 | (1.08 | - | 1.48) | 1.00 | 1.11 | (0.93 | - | 1.31) | 1.00 |
| Occasionally | 1.02 | (0.87 | - | 1.18) | 1.00 | 1.18 | (1.07 | - | 1.31) | 1.00 |
| None | 1.02 | (0.88 | - | 1.18) | 1.00 | 0.96 | (0.88 | - | 1.04) | 1.00 |
| Perceived condition of health | ||||||||||
| Good | 1.05 | (0.93 | - | 1.18) | 1.00 | 1.04 | (0.96 | - | 1.14) | 1.00 |
| Bad | 1.15 | (1.02 | - | 1.31) | 1.00 | 1.10 | (1.01 | - | 1.20) | 1.00 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cha, W.-T.; Joo, H.-J.; Park, Y.-S.; Park, E.-C.; Kim, S.-Y. Depression before and during-COVID-19 by Gender in the Korean Population. Int. J. Environ. Res. Public Health 2022, 19, 3477. https://doi.org/10.3390/ijerph19063477
Cha W-T, Joo H-J, Park Y-S, Park E-C, Kim S-Y. Depression before and during-COVID-19 by Gender in the Korean Population. International Journal of Environmental Research and Public Health. 2022; 19(6):3477. https://doi.org/10.3390/ijerph19063477
Chicago/Turabian StyleCha, Won-Tae, Hye-Jin Joo, Yu-Shin Park, Eun-Cheol Park, and Soo-Young Kim. 2022. "Depression before and during-COVID-19 by Gender in the Korean Population" International Journal of Environmental Research and Public Health 19, no. 6: 3477. https://doi.org/10.3390/ijerph19063477
APA StyleCha, W.-T., Joo, H.-J., Park, Y.-S., Park, E.-C., & Kim, S.-Y. (2022). Depression before and during-COVID-19 by Gender in the Korean Population. International Journal of Environmental Research and Public Health, 19(6), 3477. https://doi.org/10.3390/ijerph19063477







