Can Teledentistry Replace Conventional Clinical Follow-Up Care for Minor Dental Surgery? A Prospective Randomized Clinical Trial
Abstract
1. Introduction
2. Materials and Methods
2.1. Patients
2.2. Inclusion and Exclusion Criteria
2.3. Study Design
2.4. Questionnaires
2.5. Statistics
3. Results
3.1. Study Population
3.2. Freedom of Symptoms
3.3. Exclusion of Complications
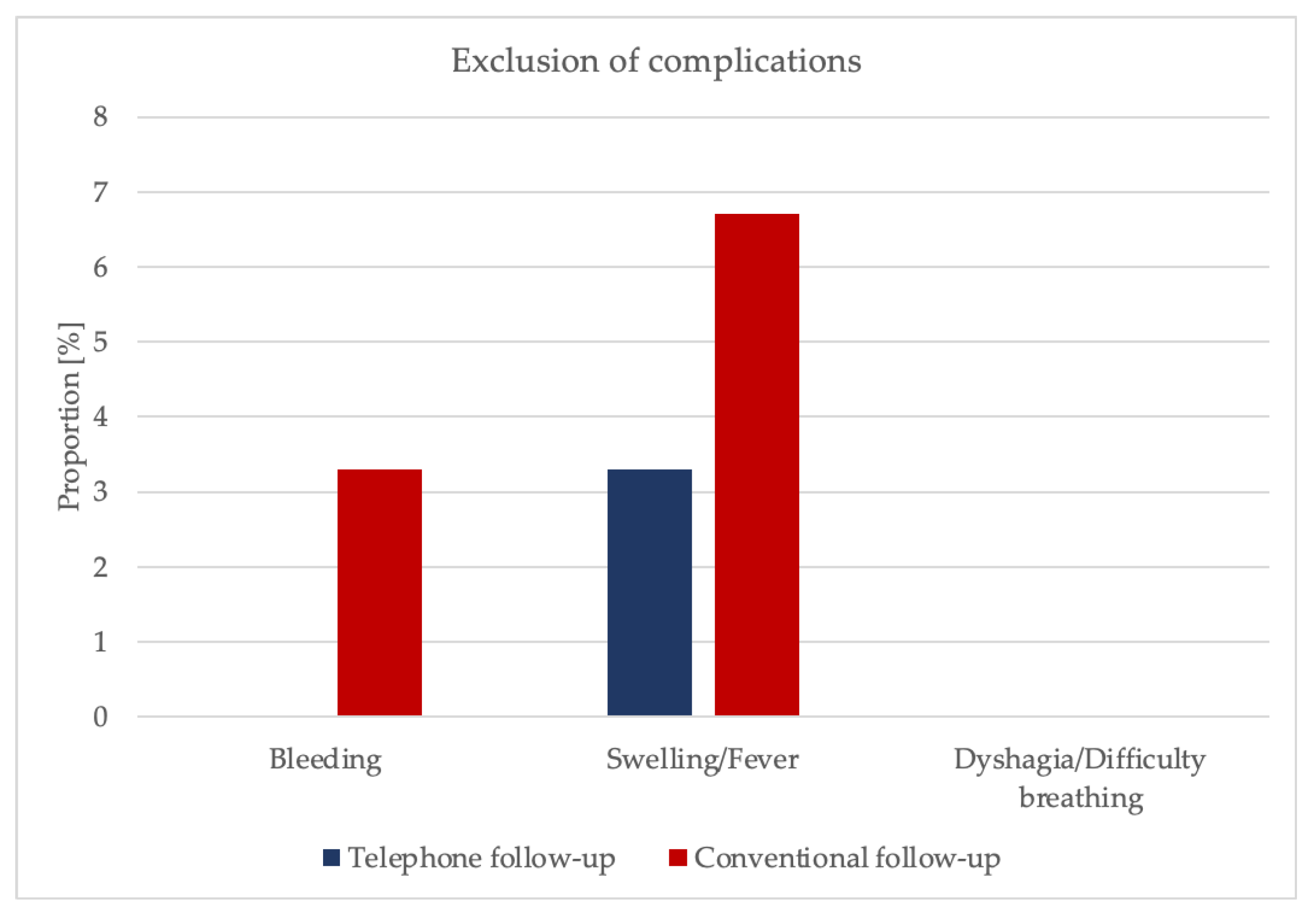
3.4. Evaluation of the Practitioner
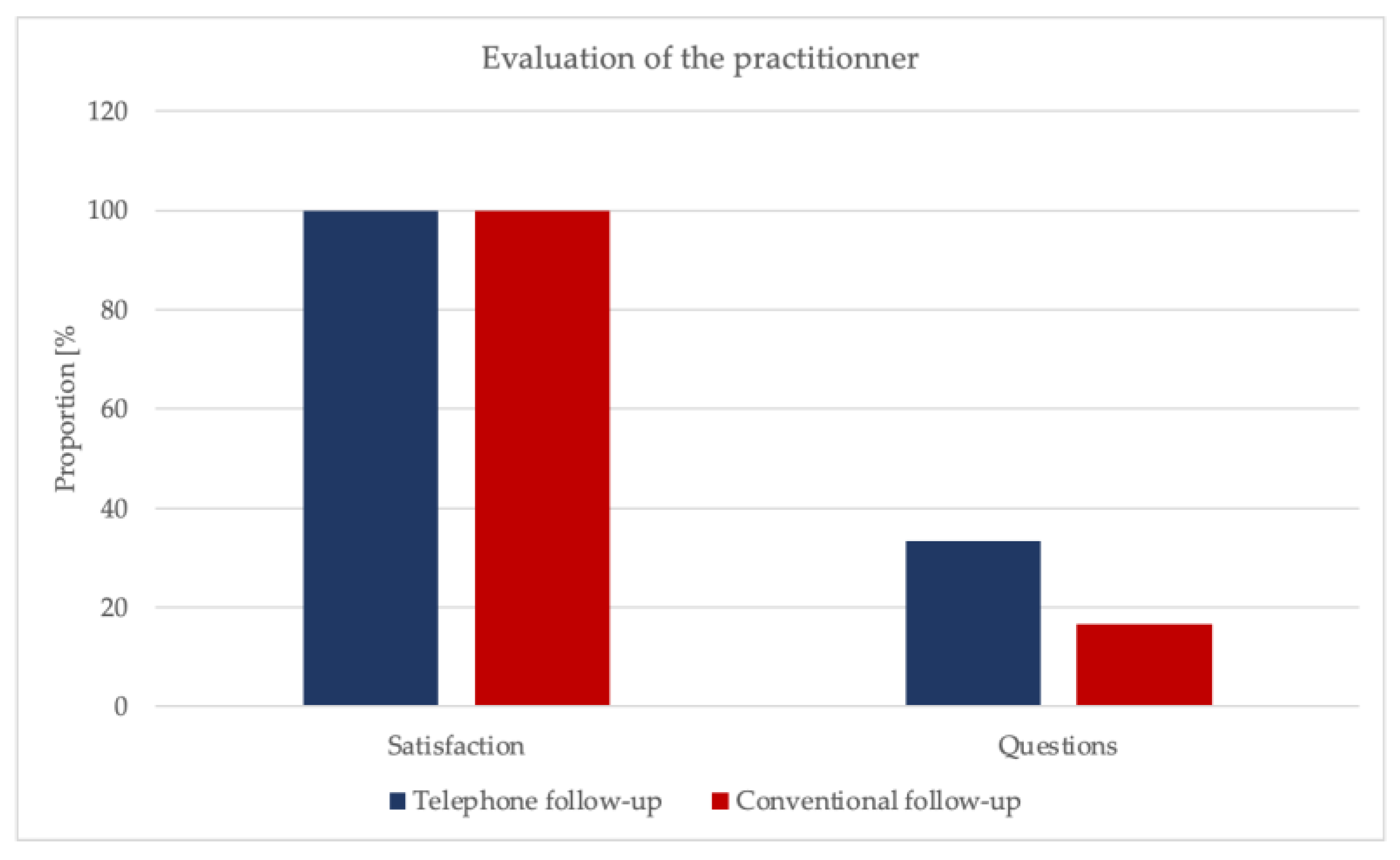
3.5. Evaluation of the Form of Follow-Up Care
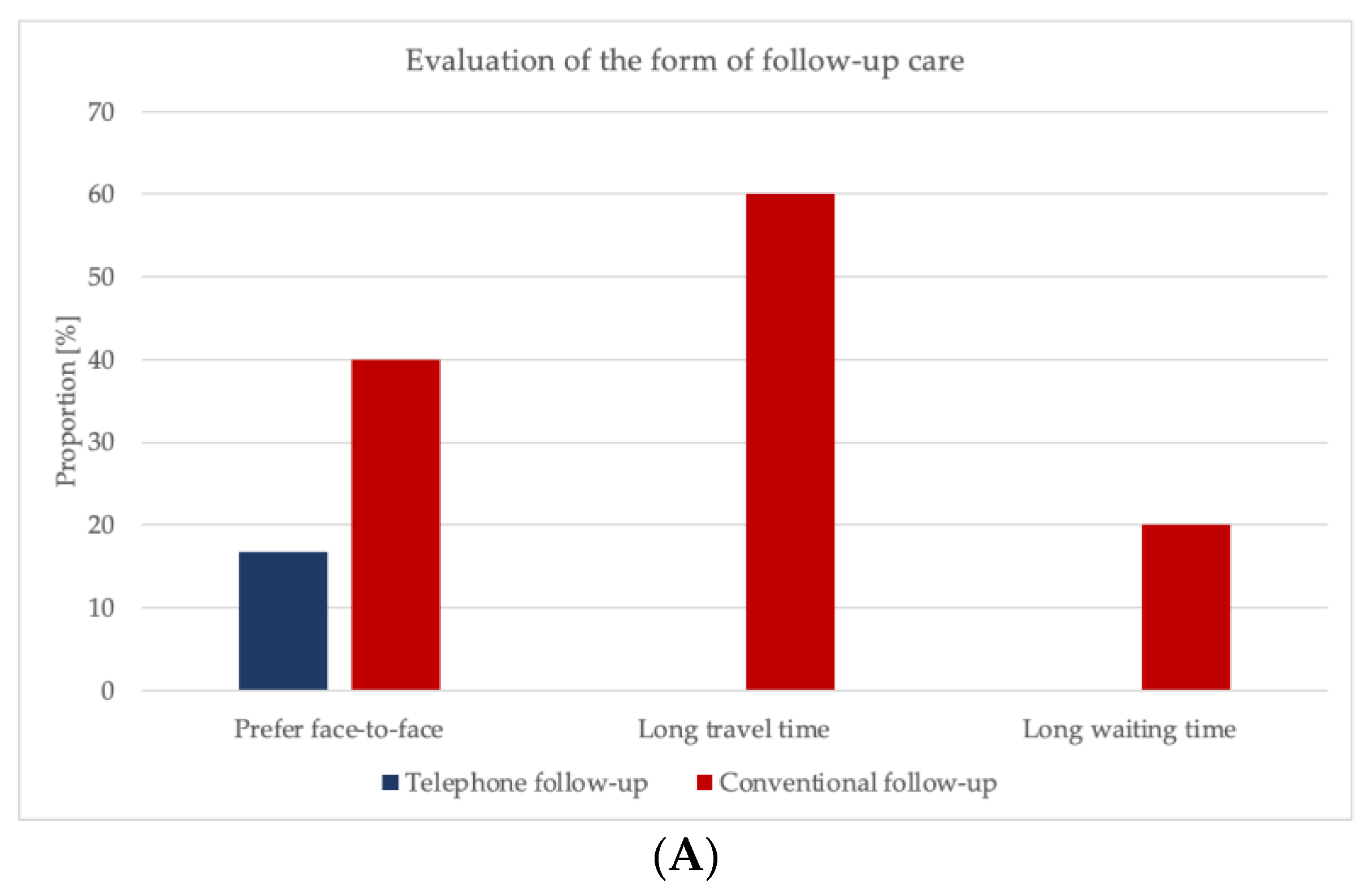
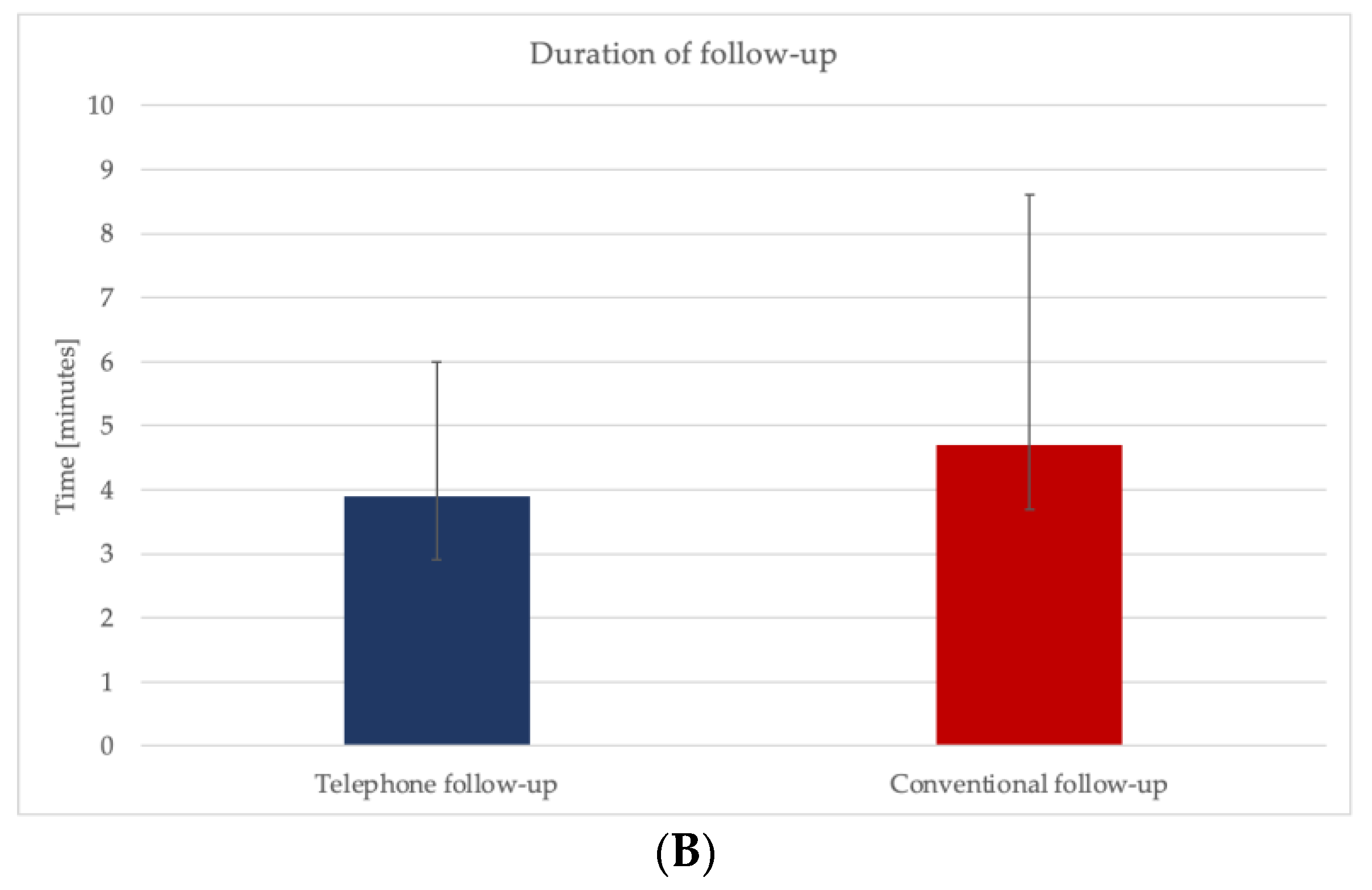
3.6. Quality of the Form of Follow-Up Care
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Susarla, S.M.; Black, R.; Dodson, T.B. After dentoalveolar surgery, most patients are satisfied with telephone follow-up. J. Oral Maxillofac. Surg. 2011, 69, 2099–2105. [Google Scholar] [CrossRef] [PubMed]
- WHO. A Health Telematics Policy in Support of WHO’S Health-For-All Strategy for Global Development: Report of the WHO Group Consultation on Health Telematics 11–16 December, Geneva, 1997; World Health Organization: Geneva, Switzerland, 1998. [Google Scholar]
- WHO. Telemedicine: Opportunities and Developments in Member States: Report on the Second Global Survey on eHealth 2009. Healthc. Inform. Res. 2012, 18, 153–155. [Google Scholar] [CrossRef]
- Thompson, J.C.; Cichowski, S.B.; Rogers, R.G.; Qeadan, F.; Zambrano, J.; Wenzl, C.; Jeppson, P.C.; Dunivan, G.C.; Komesu, Y.M. Outpatient visits versus telephone interviews for postoperative care: A randomized controlled trial. Int. Urogynecol. J. 2019, 30, 1639–1646. [Google Scholar] [CrossRef] [PubMed]
- Woods, C.E.; Jones, R.; O’Shea, E.; Grist, E.; Wiggers, J.; Usher, K. Nurse-led postdischarge telephone follow-up calls: A mixed study systematic review. J. Clin. Nurs. 2019, 28, 3386–3399. [Google Scholar] [CrossRef] [PubMed]
- Mistiaen, P.; Poot, E. Telephone follow-up, initiated by a hospital-based health professional, for postdischarge problems in patients discharged from hospital to home. Cochrane Database Syst. Rev. 2006, 2006, Cd004510. [Google Scholar] [CrossRef] [PubMed]
- Balas, E.A.; Jaffrey, F.; Kuperman, G.J.; Boren, S.A.; Brown, G.D.; Pinciroli, F.; Mitchell, J.A. Electronic communication with patients. Evaluation of distance medicine technology. JAMA 1997, 278, 152–159. [Google Scholar] [CrossRef] [PubMed]
- Wells, J.P.; Roked, Z.; Moore, S.C.; Sivarajasingam, V. Telephone review after minor oral surgery. Br. J. Oral Maxillofac. Surg. 2016, 54, 526–530. [Google Scholar] [CrossRef]
- Martenstein, I.; Wienke, A. Das neue E-Health-Gesetz. HNO 2016, 64, 515–516. [Google Scholar] [CrossRef]
- Müller-Mielitz, S.; Lux, T. E-Health-Gesetz. In E-Health-Ökonomie; Müller-Mielitz, S., Lux, T., Eds.; Springer Fachmedien Wiesbaden: Wiesbaden, Germany, 2017; pp. 125–136. [Google Scholar]
- Available online: https://www.bundesaerztekammer.de/fileadmin/user_upload/downloads/pdf-Ordner/MBO/Synopse_MBO-AE_zu_AEnderungen____7_Abs._4.pdf (accessed on 22 February 2022).
- Bundesärztekammer. (Muster-)Berufsordnung für Die in Deutschland Tätigen Ärztinnen und Ärzte. Available online: https://www.bundesaerztekammer.de/fileadmin/user_upload/downloads/pdf-Ordner/MBO/MBO-AE.pdf (accessed on 22 February 2022).
- Preshaw, P.M.; Fisher, S.E. Routine review of patients after extraction of third molars: Is it justified? Br. J. Oral Maxillofac. Surg. 1997, 35, 393–395. [Google Scholar] [CrossRef]
- Thompson-Coon, J.; Abdul-Rahman, A.K.; Whear, R.; Bethel, A.; Vaidya, B.; Gericke, C.A.; Stein, K. Telephone consultations in place of face to face out-patient consultations for patients discharged from hospital following surgery: A systematic review. BMC Health Serv. Res. 2013, 13, 128. [Google Scholar] [CrossRef]
- Hannis, M.D.; Hazard, R.L.; Rothschild, M.; Elnicki, D.M.; Keyserling, T.C.; DeVellis, R.F. Physician attitudes regarding telephone medicine. J. Gen. Intern. Med. 1996, 11, 678–683. [Google Scholar] [CrossRef] [PubMed]
- Gray, R.T.; Sut, M.K.; Badger, S.A.; Harvey, C.F. Post-operative telephone review is cost-effective and acceptable to patients. Ulst. Med. J. 2010, 79, 76–79. [Google Scholar]
- McVay, M.R.; Kelley, K.R.; Mathews, D.L.; Jackson, R.J.; Kokoska, E.R.; Smith, S.D. Postoperative follow-up: Is a phone call enough? J. Pediatr. Surg. 2008, 43, 83–86. [Google Scholar] [CrossRef]
- Molfenter, T.; Boyle, M.; Holloway, D.; Zwick, J. Trends in telemedicine use in addiction treatment. Addict. Sci. Clin. Pract. 2015, 10, 14. [Google Scholar] [CrossRef]
- Craig, J.; Patterson, V. Introduction to the practice of telemedicine. J. Telemed. Telecare 2005, 11, 3–9. [Google Scholar] [CrossRef]
- Wood, E.W.; Strauss, R.A.; Janus, C.; Carrico, C.K. Telemedicine Consultations in Oral and Maxillofacial Surgery: A Follow-Up Study. J. Oral Maxillofac. Surg. 2016, 74, 262–268. [Google Scholar] [CrossRef]
- Car, J.; Sheikh, A. Telephone consultations. BMJ 2003, 326, 966–969. [Google Scholar] [CrossRef] [PubMed]
- Kassmann, B.P.; Docherty, S.L.; Rice, H.E.; Bailey, D.E., Jr.; Schweitzer, M. Telephone follow-up for pediatric ambulatory surgery: Parent and provider satisfaction. J. Pediatr. Nurs. 2012, 27, 715–724. [Google Scholar] [CrossRef] [PubMed]
- Pathni, R.K.; Satpathy, S.; Kailash, S. Need for tele follow-up—A study at a public sector quaternary referral hospital in India. J. Telemed. Telecare 2009, 15, 255–259. [Google Scholar] [CrossRef] [PubMed]
- Ainsworth, G. Routine follow-up visits not necessary after third molar removal under sedation. Evid. Based Dent. 2006, 7, 92. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Goedeke, J.; Ertl, A.; Zöller, D.; Rohleder, S.; Muensterer, O.J. Telemedicine for pediatric surgical outpatient follow-up: A prospective, randomized single-center trial. J. Pediatr. Surg. 2019, 54, 200–207. [Google Scholar] [CrossRef] [PubMed]
- Foster, J.; Jessopp, L.; Dale, J. Concerns and confidence of general practitioners in providing telephone consultations. Br. J. Gen. Pract. 1999, 49, 111–113. [Google Scholar] [PubMed]
- Rosbe, K.W.; Jones, D.; Jalisi, S.; Bray, M.A. Efficacy of postoperative follow-up telephone calls for patients who underwent adenotonsillectomy. Arch. Otolaryngol. Head Neck Surg. 2000, 126, 718–721. [Google Scholar] [CrossRef] [PubMed]
- Wootton, R. Telemedicine in the National Health Service. J. R. Soc. Med. 1998, 91, 614–621. [Google Scholar] [CrossRef] [PubMed]
- Bruining, N. The post-pandemic legacy: The breakthrough of digital health and telemedicine. Cardiovasc. Res. 2021, 117, e118–e119. [Google Scholar] [CrossRef] [PubMed]
- Grossman, Z.; Chodick, G.; Reingold, S.M.; Chapnick, G.; Ashkenazi, S. The future of telemedicine visits after COVID-19: Perceptions of primary care pediatricians. Isr. J. Health Policy Res. 2020, 9, 53. [Google Scholar] [CrossRef]
- Hagge, D.; Knopf, A.; Hofauer, B. Chancen und Einsatzmöglichkeiten von Telemedizin in der Hals-, Nasen- und Ohrenheilkunde bei der Bekämpfung von SARS-CoV-2. HNO 2020, 68, 433–439. [Google Scholar] [CrossRef]
- Bestsennyy, O.; Gilbert, G.; Rost, J. Telehealth: A Quarter-Trillion-Dollar Post-COVID-19 Reality? McKinsey & Company: New York, NY, USA, 2021. [Google Scholar]
- Beule, A.G. Telemedical Methods in Otorhinolaryngology. Laryngorhinootologie 2019, 98, S129–S172. [Google Scholar] [CrossRef]
- Chanussot-Deprez, C.; Contreras-Ruiz, J. Telemedicine in wound care: A review. Adv. Skin Wound Care 2013, 26, 78–82. [Google Scholar] [CrossRef]
- Knox, L.; Rahman, R.J.; Beedie, C. Quality of life in patients receiving telemedicine enhanced chronic heart failure disease management: A meta-analysis. J. Telemed. Telecare 2017, 23, 639–649. [Google Scholar] [CrossRef] [PubMed]
- Tupper, O.D.; Gregersen, T.L.; Ringbaek, T.; Brøndum, E.; Frausing, E.; Green, A.; Ulrik, C.S. Effect of tele-health care on quality of life in patients with severe COPD: A randomized clinical trial. Int. J. Chron. Obstruct. Pulmon. Dis. 2018, 13, 2657–2662. [Google Scholar] [CrossRef] [PubMed]
- Sanders, C.; Rogers, A.; Bowen, R.; Bower, P.; Hirani, S.; Cartwright, M.; Fitzpatrick, R.; Knapp, M.; Barlow, J.; Hendy, J.; et al. Exploring barriers to participation and adoption of telehealth and telecare within the Whole System Demonstrator trial: A qualitative study. BMC Health Serv. Res. 2012, 12, 220. [Google Scholar] [CrossRef]
- Pippi, R.; Pietrantoni, A.; Patini, R.; Santoro, M. Is telephone follow-up really effective in early diagnosis of inflammatory complications after tooth extraction? Med. Oral Patol. Oral Cir. Bucal. 2018, 23, e707–e715. [Google Scholar] [CrossRef] [PubMed]
- Adeyemo, W.L.; Ladeinde, A.L.; Ogunlewe, M.O. Clinical evaluation of post-extraction site wound healing. J. Contemp. Dent. Pract. 2006, 7, 40–49. [Google Scholar] [CrossRef] [PubMed]
- Miclotte, I.; Agbaje, J.O.; Spaey, Y.; Legrand, P.; Politis, C. Incidence and treatment of complications in patients who had third molars or other teeth extracted. Br. J. Oral Maxillofac. Surg. 2018, 56, 388–393. [Google Scholar] [CrossRef] [PubMed]
- Al-Khateeb, T.H.; Alnahar, A. Pain experience after simple tooth extraction. J. Oral Maxillofac. Surg. 2008, 66, 911–917. [Google Scholar] [CrossRef] [PubMed]
- Akinbami, B.O.; Godspower, T. Dry socket: Incidence, clinical features, and predisposing factors. Int. J. Dent. 2014, 2014, 796102. [Google Scholar] [CrossRef] [PubMed]
- Pierse, J.E.; Dym, H.; Clarkson, E. Diagnosis and management of common postextraction complications. Dent. Clin. N. Am. 2012, 56, 75–93. [Google Scholar] [CrossRef] [PubMed]
- Siddiqi, A.; Morkel, J.A.; Zafar, S. Antibiotic prophylaxis in third molar surgery: A randomized double-blind placebo-controlled clinical trial using split-mouth technique. Int. J. Oral Maxillofac. Surg. 2010, 39, 107–114. [Google Scholar] [CrossRef] [PubMed]
- Bouloux, G.F.; Steed, M.B.; Perciaccante, V.J. Complications of third molar surgery. Oral Maxillofac. Surg. Clin. N. Am. 2007, 19, 117–128. [Google Scholar] [CrossRef]
- Chuang, S.K.; Perrott, D.H.; Susarla, S.M.; Dodson, T.B. Risk factors for inflammatory complications following third molar surgery in adults. J. Oral Maxillofac. Surg. 2008, 66, 2213–2218. [Google Scholar] [CrossRef] [PubMed]
- Lieblich, S.E.; Kleiman, M.A.; Zak, M.J. Dentoalveolar surgery. J. Oral Maxillofac. Surg. 2012, 70, e50–e71. [Google Scholar] [CrossRef] [PubMed]
- Eisenberg, D.; Hwa, K.; Wren, S.M. Telephone follow-up by a midlevel provider after laparoscopic inguinal hernia repair instead of face-to-face clinic visit. JSLS J. Soc. Laparoendosc. Surg. 2015, 19, e2014.00205. [Google Scholar] [CrossRef] [PubMed]
- Capuzzi, P.; Montebugnoli, L.; Vaccaro, M.A. Extraction of impacted third molars. A longitudinal prospective study on factors that affect postoperative recovery. Oral Surg. Oral Med. Oral Pathol. 1994, 77, 341–343. [Google Scholar] [CrossRef]
- Kim, J.C.; Choi, S.S.; Wang, S.J.; Kim, S.G. Minor complications after mandibular third molar surgery: Type, incidence, and possible prevention. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2006, 102, e4–e11. [Google Scholar] [CrossRef]
- Pathak, S.; Vashisth, S.; Mishra, S.; Singh, S.P.; Sharma, S. Grading of Extraction and Its Relationship with Post-operative Pain and Trismus, along with Proposed Grading for Trismus. J. Clin. Diagn. Res. 2014, 8, ZC09–ZC11. [Google Scholar] [CrossRef] [PubMed]
- Sukegawa, S.; Yokota, K.; Kanno, T.; Manabe, Y.; Sukegawa-Takahashi, Y.; Masui, M.; Furuki, Y. What are the risk factors for postoperative infections of third molar extraction surgery: A retrospective clinical study? Med. Oral Patol. Oral Cir. Bucal 2019, 24, e123–e129. [Google Scholar] [CrossRef]
- Shigeishi, H.; Ohta, K.; Takechi, M. Risk factors for postoperative complications following oral surgery. J. Appl. Oral Sci. 2015, 23, 419–423. [Google Scholar] [CrossRef] [PubMed]
- Kumbargere Nagraj, S.; Prashanti, E.; Aggarwal, H.; Lingappa, A.; Muthu, M.S.; Kiran Kumar Krishanappa, S.; Hassan, H. Interventions for treating post-extraction bleeding. Cochrane Database Syst. Rev. 2018, 3, Cd011930. [Google Scholar] [CrossRef]
- Louis, P.J. Complications of Dentoalveolar Surgery. Oral Maxillofac. Surg. Clin. N. Am. 2020, 32, 649–674. [Google Scholar] [CrossRef] [PubMed]
- Bortoluzzi, M.C.; Capella, D.L.; Barbieri, T.; Marchetti, S.; Dresch, C.P.; Tirello, C. Does smoking increase the incidence of postoperative complications in simple exodontia? Int. Dent. J. 2012, 62, 106–108. [Google Scholar] [CrossRef]
- Forbes, B.; Secrest, A.M.; Hand, M.Q.; Eliason, M.J. Process of Post-operative Telephone Follow-up Implementation for Mohs Micrographic Surgery: A Pilot Study. J. Clin. Aesthet. Dermatol. 2018, 11, 36–39. [Google Scholar] [PubMed]
- Bui, C.H.; Seldin, E.B.; Dodson, T.B. Types, frequencies, and risk factors for complications after third molar extraction. J. Oral Maxillofac. Surg. 2003, 61, 1379–1389. [Google Scholar] [CrossRef] [PubMed]
- da Mata, L.R.; da Silva, A.C.; Pereira Mda, G.; de Carvalho, E.C. Telephone follow-up of patients after radical prostatectomy: A systematic review. Rev. Lat. Am. Enferm. 2014, 22, 337–345. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Eaton, J.; Rasgon, B.; Derbin, L.W.; Hilsinger, R.L., Jr.; Buenavista, T. Telephone appointment visits for head and neck surgery follow-up care. Laryngoscope 2002, 112, 1060–1064. [Google Scholar] [CrossRef]
- Jones, D.T.; Yoon, M.J.; Licameli, G. Effectiveness of postoperative follow-up telephone interviews for patients who underwent adenotonsillectomy: A retrospective study. Arch. Otolaryngol. Head Neck Surg. 2007, 133, 1091–1095. [Google Scholar] [CrossRef][Green Version]
- Kummerow Broman, K.; Roumie, C.L.; Stewart, M.K.; Castellanos, J.A.; Tarpley, J.L.; Dittus, R.S.; Pierce, R.A. Implementation of a Telephone Postoperative Clinic in an Integrated Health System. J. Am. Coll. Surg. 2016, 223, 644–651. [Google Scholar] [CrossRef] [PubMed]
- Hwa, K.; Wren, S.M. Telehealth follow-up in lieu of postoperative clinic visit for ambulatory surgery: Results of a pilot program. JAMA Surg. 2013, 148, 823–827. [Google Scholar] [CrossRef] [PubMed]
- Fischer, K.; Hogan, V.; Jager, A.; von Allmen, D. Efficacy and utility of phone call follow-up after pediatric general surgery versus traditional clinic follow-up. Perm. J. 2015, 19, 11–14. [Google Scholar] [CrossRef] [PubMed]
- Lesher, A.P.; Shah, S.R. Telemedicine in the perioperative experience. Semin. Pediatr. Surg. 2018, 27, 102–106. [Google Scholar] [CrossRef] [PubMed]


| Inclusion Criteria | Exclusion Criteria |
|---|---|
|
|
| Class | Questions |
|---|---|
| Freedom of symptoms | Do you feel bad after surgery? Are you currently taking pain medication? Can you perform normal daily activities? Do you have any concerns? Do you continue to eat a liquid-soft diet? |
| Exclusion of complications | Do you have a taste of blood in your mouth or is there active bleeding? Do you suffer from swelling, fever, or chills with sweat? Is there any difficulty swallowing or breathing? |
| Practitioner | Are you satisfied with your surgeon? Are there any questions concerning the discharge consultation or the postoperative check-up? |
| Follow-up care | Would you either prefer telephone follow-up or personal follow-up |
| Travel and waiting time | Did you have a long travel time? Did you have a long waiting time? |
| Telephone Follow-Up | Clinical Follow-Up | Total | |||||
|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | p | |
| Age (y) | 53.9 | 20.8 | 49.4 | 16.2 | 51.6 | 18.6 | 0.208 |
| Travel distance (km) | 23.1 | 25.2 | 20.3 | 22.4 | 21.7 | 23.7 | 0.598 |
| Travel time (min) | 26.4 | 17.5 | 25.1 | 16.0 | 25.7 | 16.6 | 0.864 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Heimes, D.; Luhrenberg, P.; Langguth, N.; Kaya, S.; Obst, C.; Kämmerer, P.W. Can Teledentistry Replace Conventional Clinical Follow-Up Care for Minor Dental Surgery? A Prospective Randomized Clinical Trial. Int. J. Environ. Res. Public Health 2022, 19, 3444. https://doi.org/10.3390/ijerph19063444
Heimes D, Luhrenberg P, Langguth N, Kaya S, Obst C, Kämmerer PW. Can Teledentistry Replace Conventional Clinical Follow-Up Care for Minor Dental Surgery? A Prospective Randomized Clinical Trial. International Journal of Environmental Research and Public Health. 2022; 19(6):3444. https://doi.org/10.3390/ijerph19063444
Chicago/Turabian StyleHeimes, Diana, Philipp Luhrenberg, Nils Langguth, Sebahat Kaya, Christine Obst, and Peer W. Kämmerer. 2022. "Can Teledentistry Replace Conventional Clinical Follow-Up Care for Minor Dental Surgery? A Prospective Randomized Clinical Trial" International Journal of Environmental Research and Public Health 19, no. 6: 3444. https://doi.org/10.3390/ijerph19063444
APA StyleHeimes, D., Luhrenberg, P., Langguth, N., Kaya, S., Obst, C., & Kämmerer, P. W. (2022). Can Teledentistry Replace Conventional Clinical Follow-Up Care for Minor Dental Surgery? A Prospective Randomized Clinical Trial. International Journal of Environmental Research and Public Health, 19(6), 3444. https://doi.org/10.3390/ijerph19063444







