Trends in Primary Mental Health Care Service Use and Subsequent Self-Harm in Western Sydney Australia: Policy and Workforce Implications
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Catchment
2.2. Study Participants
2.3. Primary Mental Health Care Services
2.4. Data Sources
2.5. Data Linkage
2.6. Study Factors
2.7. Data Analysis
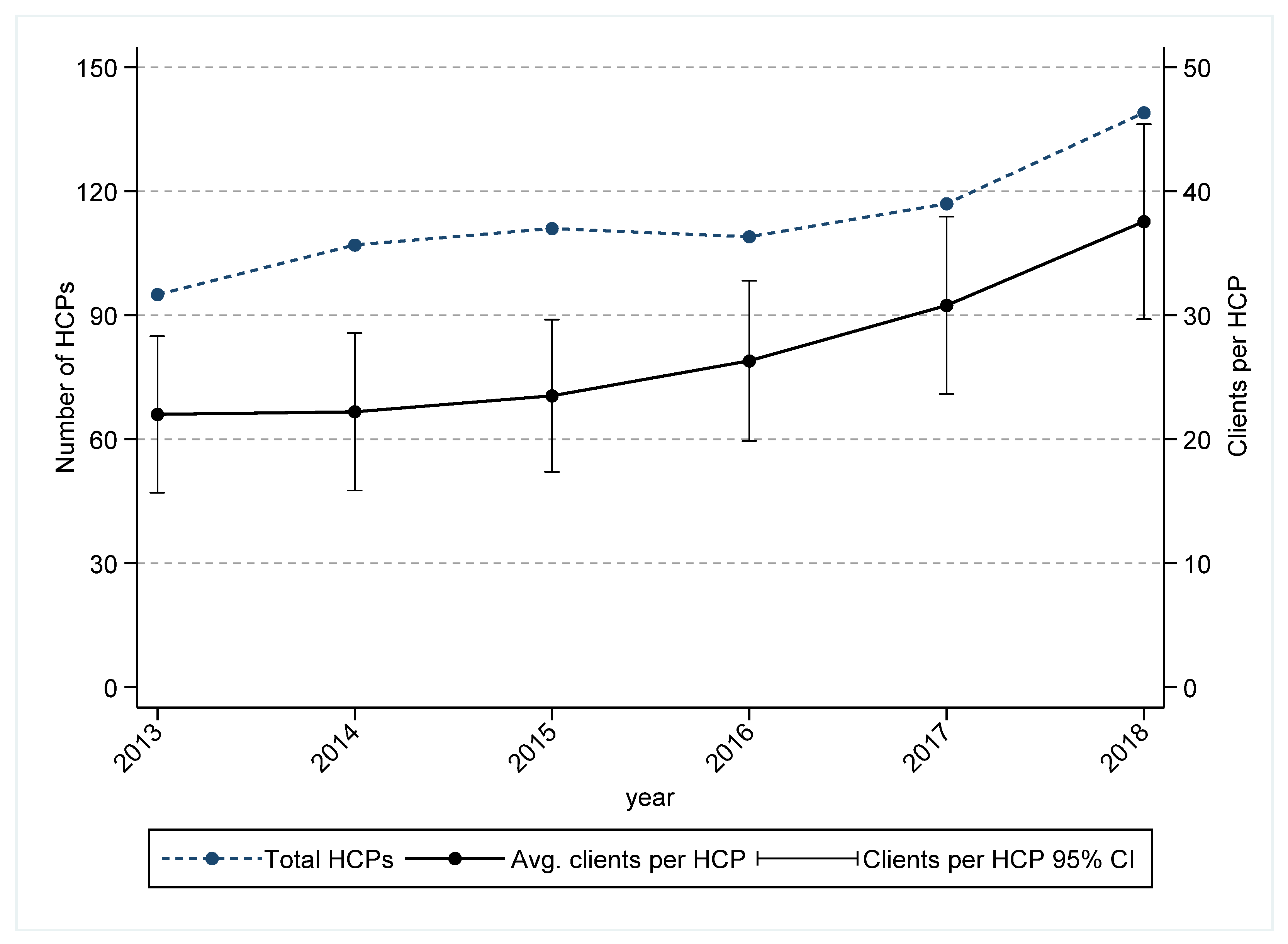
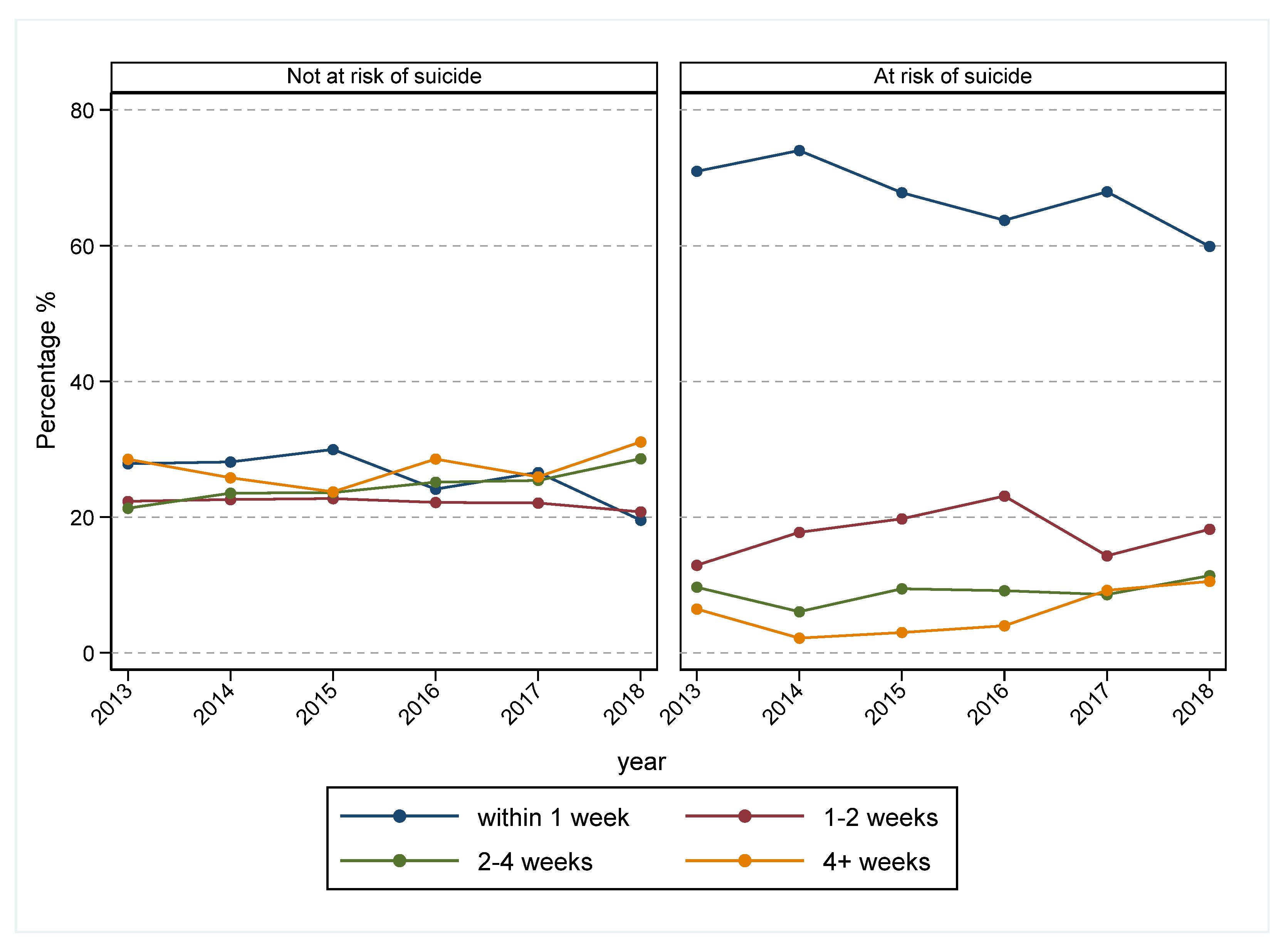
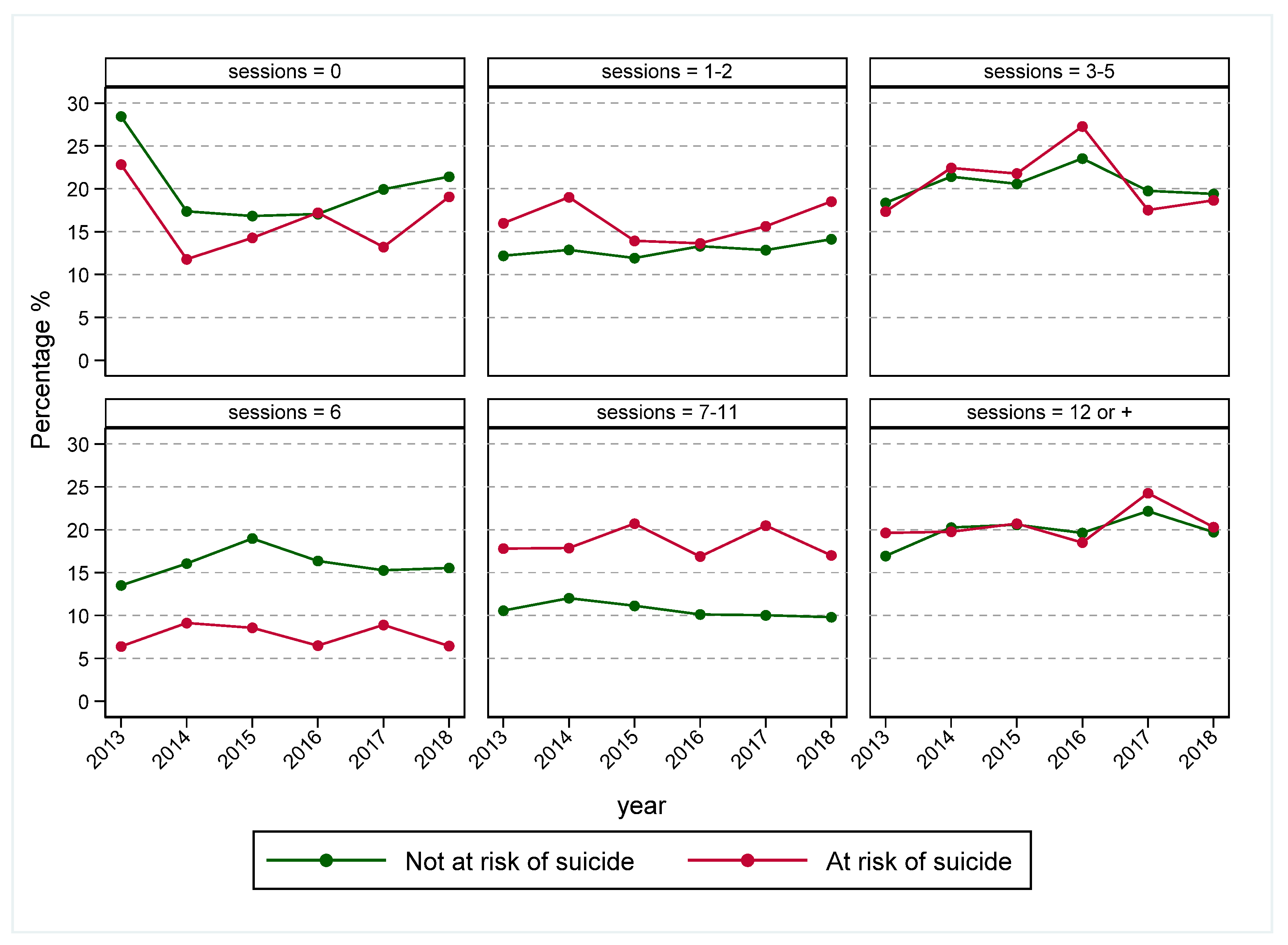
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Hickie, I.; Groom, G. Primary care-led mental health service reform: An outline of the Better Outcomes in Mental Health Care initiative. Australas. Psychiatry 2002, 10, 376–382. [Google Scholar] [CrossRef]
- McGorry, P.D.; Tanti, C.; Stokes, R.; Hickie, I.B.; Carnell, K.; Littlefield, L.K.; Moran, J. Headspace: Australia’s National Youth Mental Health Foundation—Where young minds come first. Med. J. Aust. 2007, 187, S68–S70. [Google Scholar] [CrossRef] [PubMed]
- Littlefield, L.; Giese, J. The genesis, implementation and impact of the Better Access mental health initiative introducing Medicare-funded psychology services. Clin. Psychol. 2008, 12, 42–49. [Google Scholar] [CrossRef]
- National Mental Health Commission. The National Review of Mental Health Programmes and Services; NMHC: Sydney, Australia, 2014; Volume 67. [Google Scholar]
- Australian Government Department of Health; NATIONAL PHN GUIDANCE. Initial Assessment and Referral for Mental Healthcare—Version 1.05. 2020. Available online: https://www.health.gov.au/sites/default/files/documents/2021/09/primary-health-networks-phn-mental-health-care-guidance-initial-assessment-and-referral-for-mental-health-care-national-phn-guidance-initial-assessment-and-referral-for-mental-health-care.pdf (accessed on 30 November 2021).
- Australian Institute of Health and Welfare. Mental Health Services in Australia. 2021. Available online: https://www.aihw.gov.au/reports/mental-health-services/mental-health-services-in-australia (accessed on 31 October 2021).
- Jorm, A.F. Australia’s ‘Better Access’ scheme: Has it had an impact on population mental health? Aust. N. Z. J. Psychiatry 2018, 52, 1057–1062. [Google Scholar] [CrossRef] [PubMed]
- Jorm, A.F.; Patten, S.B.; Brugha, T.S.; Mojtabai, R. Has increased provision of treatment reduced the prevalence of common mental disorders? Review of the evidence from four countries. World Psychiatry 2017, 16, 90–99. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jorm, A.; Mackinnon, A.; Hart, L.; Reavley, N.; Morgan, A. Effect of community members’ willingness to disclose a mental disorder on their psychiatric symptom scores: Analysis of data from two randomised controlled trials of mental health first aid training. Epidemiol. Psychiatr. Sci. 2020, 29, e46. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Appleby, L.; Dennehy, J.A.; Thomas, C.S.; Faragher, E.B.; Lewis, G. Aftercare and clinical characteristics of people with mental illness who commit suicide: A case-control study. Lancet 1999, 353, 1397–1400. [Google Scholar] [CrossRef]
- Harris, M.G.; Diminic, S.; Burgess, P.M.; Carstensen, G.; Stewart, G.; Pirkis, J.; Whiteford, H.A. Understanding service demand for mental health among Australians aged 16 to 64 years according to their possible need for treatment. Aust. N. Z. J. Psychiatry 2014, 48, 838–851. [Google Scholar] [CrossRef] [PubMed]
- Boswell, J.F.; Kraus, D.R.; Miller, S.D.; Lambert, M.J. Implementing routine outcome monitoring in clinical practice: Benefits, challenges, and solutions. Psychother. Res. 2015, 25, 6–19. [Google Scholar] [CrossRef] [PubMed]
- WentWest Primary Health Network. PHN Needs Assessment Western Sydney Primary Health Netork 2019–2022. 2018. Available online: https://wentwest.com.au/wp-content/uploads/planning_resources/Reports_WSPHN_Needs-Assessment_201921.pdf (accessed on 31 July 2021).
- PHIDU. Social Health Atlas of Australia: Primary Health Networks. 2019. Available online: http://phidu.torrens.edu.au/social-health-atlases/data#social-health-atlas-of-australia-primary-health-networks (accessed on 30 November 2019).
- Munasinghe, S.; Page, A.; Mannan, H.; Ferdousi, S.; Peek, B. Referral patterns to primary mental health services in Western Sydney (Australia): An analysis of routinely collected data (2005–2018). Int. J. Ment. Health Syst. 2020, 14, 37. [Google Scholar] [CrossRef] [PubMed]
- Department of Health. About the PMHC-MDS. 2021. Available online: https://pmhc-mds.com/ (accessed on 31 July 2021).
- Australian Bureau of Statistics. Socio-Economic Indexes for Areas. 2018. Available online: https://www.abs.gov.au/websitedbs/censushome.nsf/home/seifa (accessed on 31 August 2019).
- Singhal, A.; Ross, J.; Seminog, O.; Hawton, K.; Goldacre, M.J. Risk of self-harm and suicide in people with specific psychiatric and physical disorders: Comparisons between disorders using English national record linkage. J. R. Soc. Med. 2014, 107, 194–204. [Google Scholar] [CrossRef] [PubMed]
- Gunnell, D.; Hawton, K.; Ho, D.; Evans, J.; O’Connor, S.; Potokar, J.; Donovan, J.; Kapur, N. Hospital admissions for self harm after discharge from psychiatric inpatient care: Cohort study. BMJ 2008, 337, a2278. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Carter, G.; Page, A.; Large, M.; Hetrick, S.; Milner, A.J.; Bendit, N.; Walton, C.; Draper, B.; Hazell, P.; Fortune, S.; et al. Royal Australian and New Zealand College of Psychiatrists clinical practice guideline for the management of deliberate self-harm. Aust. N. Z. J. Psychiatry 2016, 50, 939–1000. [Google Scholar] [CrossRef] [PubMed]
- Centre for Epidemiology and Evidence. Health Statistics New South Wales; NSW Ministry of Health: Sydney, Australia, 2021. Available online: http://www.healthstats.nsw.gov.au/ (accessed on 31 July 2021).
- Killaspy, H.; Banerjee, S.; King, M.; Lloyd, M. Prospective controlled study of psychiatric out-patient non-attendance: Characteristics and outcome. Br. J. Psychiatry 2000, 176, 160–165. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Harris, M.G.; Hobbs, M.J.; Burgess, P.M.; Pirkis, J.E.; Diminic, S.; Siskind, D.J.; Andrews, G.; Whiteford, H.A. Frequency and quality of mental health treatment for affective and anxiety disorders among Australian adults. Med. J. Aust. 2015, 202, 185–189. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mitchell, A.J.; Selmes, T. Why don’t patients attend their appointments? Maintaining engagement with psychiatric services. Adv. Psychiatr. Treat. 2007, 13, 423–434. [Google Scholar] [CrossRef] [Green Version]
- Munasinghe, S.; Page, A.; Mannan, H.; Ferdousi, S.; Peek, B. Determinants of treatment disengagement among those at risk of suicide referred to primary mental health care services in Western Sydney, Australia. Aust. N. Z. J. Psychiatry 2021, 55, 277–288. [Google Scholar] [CrossRef] [PubMed]
- Clark, D.M.; Canvin, L.; Green, J.; Layard, R.; Pilling, S.; Janecka, M. Transparency about the outcomes of mental health services (IAPT approach): An analysis of public data. Lancet 2018, 391, 679–686. [Google Scholar] [CrossRef] [Green Version]
- Fontanella, C.A.; Warner, L.A.; Steelesmith, D.L.; Brock, G.; Bridge, J.A.; Campo, J. Association of timely outpatient mental health services for youths after psychiatric hospitalization with risk of death by suicide. JAMA Netw. Open 2020, 3, e2012887. [Google Scholar] [CrossRef] [PubMed]

| Characteristics | 2013 | 2014 | 2015 | 2016 | 2017 | 2018 | Total |
|---|---|---|---|---|---|---|---|
| Total referrals | 2262 (11.6) | 2243 (11.5) | 2420 (12.5) | 2637 (13.6) | 3544 (18.2) | 6331 (32.6) | 19,437 (100) |
| Gender (gender is missing for 47 (0.24) referrals) | |||||||
| Male | 849 (37.5) | 940 (41.9) | 993 (41.0) | 1086 (41.2) | 1372 (38.8) | 2342 (37.2) | 7582 (39.1) |
| Female | 1412 (62.5) | 1302 (58.1) | 1427 (59.0) | 1550 (58.8) | 2165 (61.2) | 3952 (62.8) | 11,808 (60.9) |
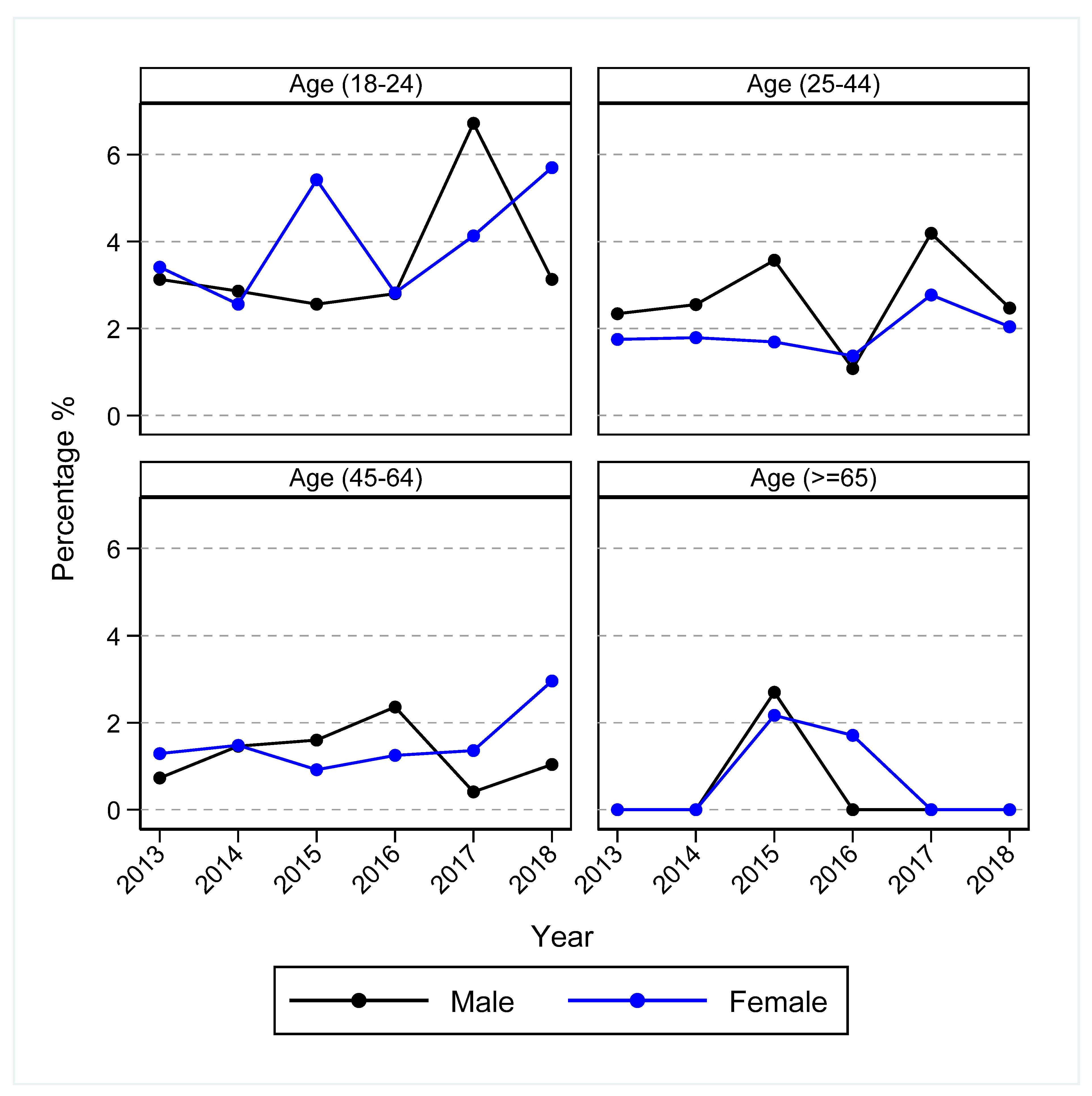
| Age (age is missing for 923 (4.75) referrals) | |||||||
| 5–17 | 570 (25.3) | 933 (41.6) | 808 (33.4) | 783 (29.7) | 947 (27.5) | 1122 (20.3) | 5163 (27.9) |
| 18–24 | 276 (12.3) | 187 (8.3) | 244 (10.1) | 284 (10.8) | 363 (10.5) | 691 (12.5) | 2045 (11.0) |
| 25–44 | 827 (36.7) | 595 (26.5) | 726 (30.0) | 789 (29.9) | 1171 (34.0) | 1881 (34.1) | 5989 (32.3) |
| 45–64 | 492 (21.8) | 408 (18.2) | 513 (21.2) | 613 (23.3) | 742 (21.6) | 1452 (26.3) | 4220 (22.8) |
| ≥65 | 87 (3.9) | 120 (5.3) | 129 (5.3) | 167 (6.3) | 218 (6.3) | 376 (6.8) | 1097 (5.9) |
| Socioeconomic status (socioeconomic status is missing for 1403 (7.22) referrals) | |||||||
| 5 (Least disadvantaged) | 197 (16.4) | 396 (17.7) | 430 (17.8) | 395 (15.0) | 550 (15.7) | 952 (15.8) | 2920 (16.2) |
| 4 | 166 (13.8) | 292 (13.0) | 339 (14.0) | 464 (17.6) | 684 (19.5) | 1154 (19.1) | 3099 (17.2) |
| 3 | 316 (26.3) | 525 (23.4) | 591 (24.4) | 509 (19.3) | 703 (20.0) | 1491 (24.7) | 4135 (22.9) |
| 2 | 192 (16.0) | 311 (13.9) | 340 (14.1) | 381 (14.5) | 478 (13.6) | 863 (14.3) | 2565 (14.2) |
| 1 (Most disadvantaged) | 329 (27.4) | 715 (31.9) | 718 (29.7) | 884 (33.6) | 1092 (31.1) | 1577 (26.1) | 5315 (29.5) |
| Diagnosis (diagnosis is missing for 1888 (9.71) referrals) | |||||||
| Anxiety disorders | 324 (15.9) | 434 (21.3) | 434 (18.8) | 425 (17.6) | 854 (26.1) | 1405 (25.6) | 3876 (22.1) |
| Affective (mood) disorders | 477 (23.4) | 387 (19.0) | 478 (20.7) | 420 (17.4) | 582 (17.8) | 1075 (19.6) | 3419 (19.5) |
| Anxiety and affective disorders | 701 (34.4) | 677 (33.2) | 872 (37.7) | 1034 (42.9) | 1322 (40.5) | 1933 (35.3) | 6539 (37.3) |
| Substance use disorders | 73 (3.6) | 81 (4.0) | 112 (4.8) | 160 (6.6) | 133 (4.1) | 150 (2.7) | 709 (4.0) |
| Other | 465 (22.8) | 462 (22.6) | 415 (18.0) | 369 (15.3) | 377 (11.5) | 918 (16.7) | 3006 (17.1) |
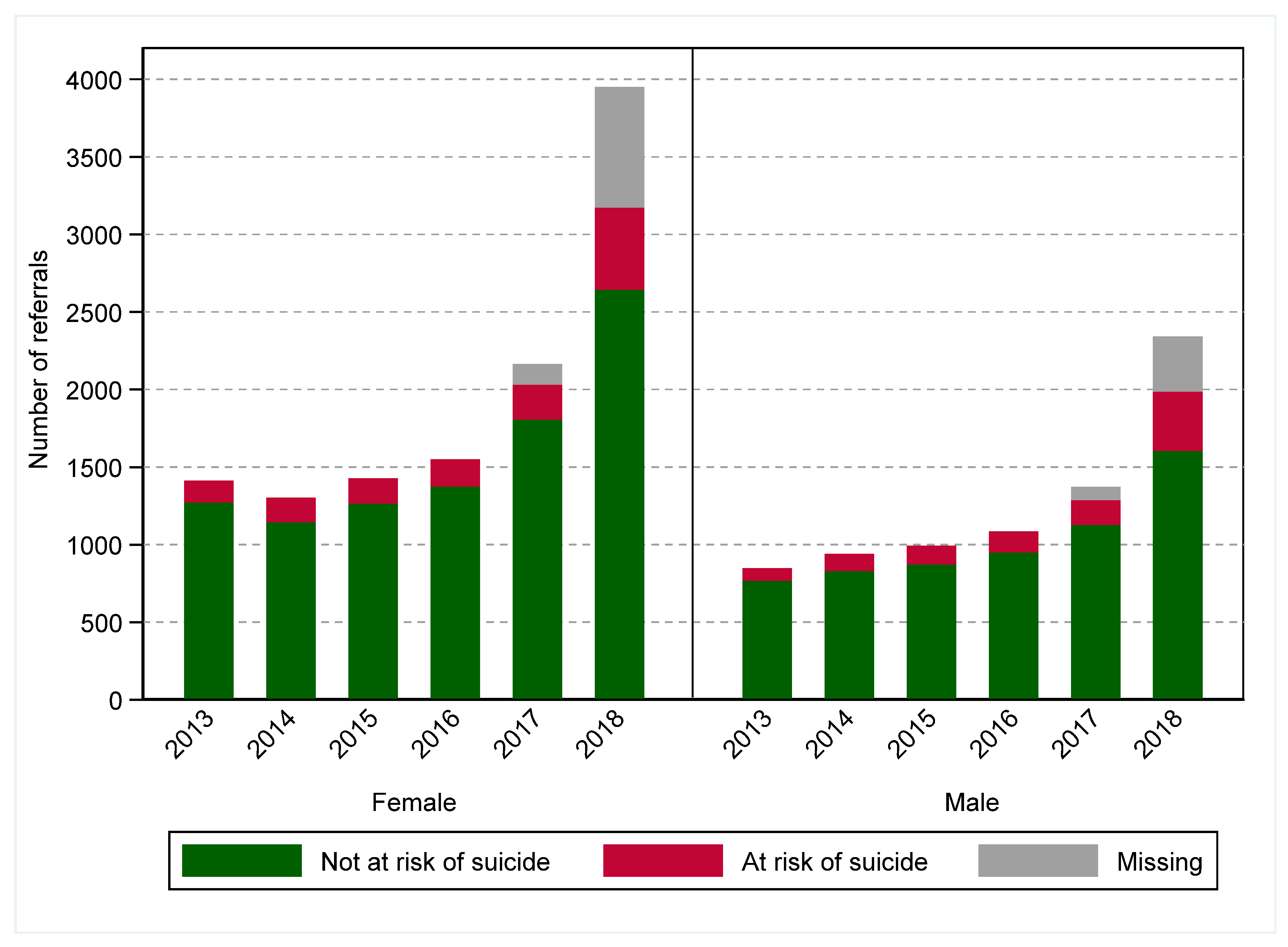
| Risk of suicide (risk of suicide is missing for 1373 (7.06) referrals) | |||||||
| No | 2043 (90.3) | 1980 (88.3) | 2140 (88.4) | 2329 (88.3) | 2939 (88.4) | 4258 (82.2) | 15,689 (86.9) |
| Yes | 219 (9.7) | 263 (11.7) | 280 (11.6) | 308 (11.7) | 385 (11.6) | 920 (17.8) | 2375 (13.1) |
| Any medication use (any medication use is missing for 3108 (15.99) referrals) | |||||||
| No | 1592 (70.4) | 1590 (70.9) | 1628 (67.3) | 1730 (65.6) | 1714 (59.2) | 1961 (50.6) | 10,215 (62.6) |
| Yes | 670 (29.6) | 653 (29.1) | 790 (32.7) | 906 (34.4) | 1180 (40.8) | 1915 (49.4) | 6114 (37.4) |
| Total referrals (linked data) a | 1535 (12.7) | 1302 (10.8) | 1611 (13.3) | 1852 (15.3) | 2331 (19.3) | 3440 (28.5) | 12,071 (100) |
| Intentional self-harm (undetermined included) b | |||||||
| Within 365 days after LSD # | 28 (1.8) | 23 (1.8) | 37 (2.3) | 30 (1.6) | 60 (2.6) | 86 (2.5) | 264 (2.2) |
| Within 365 days after LSD $ | 24 (2.1) | 17 (1.6) | 29 (2.1) | 22 (1.4) | 49 (2.6) | 66 (2.4) | 207 (2.1) |
| Intentional self-harm (undetermined excluded) c | |||||||
| Within 365 days after LSD # | 21 (1.4) | 18 (1.4) | 31 (1.9) | 24 (1.3) | 49 (2.1) | 70 (2.0) | 213 (1.8) |
| Within 365 days after LSD $ | 18 (1.6) | 13 (1.2) | 25 (1.8) | 19 (1.2) | 40 (2.1) | 54 (2.0) | 169 (1.7) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Munasinghe, S.; Page, A.; Sperandei, S.; Gaur, P.; Ferdousi, S.; Mannan, H.; Brakoulias, V. Trends in Primary Mental Health Care Service Use and Subsequent Self-Harm in Western Sydney Australia: Policy and Workforce Implications. Int. J. Environ. Res. Public Health 2022, 19, 3382. https://doi.org/10.3390/ijerph19063382
Munasinghe S, Page A, Sperandei S, Gaur P, Ferdousi S, Mannan H, Brakoulias V. Trends in Primary Mental Health Care Service Use and Subsequent Self-Harm in Western Sydney Australia: Policy and Workforce Implications. International Journal of Environmental Research and Public Health. 2022; 19(6):3382. https://doi.org/10.3390/ijerph19063382
Chicago/Turabian StyleMunasinghe, Sithum, Andrew Page, Sandro Sperandei, Pankaj Gaur, Shahana Ferdousi, Haider Mannan, and Vlasios Brakoulias. 2022. "Trends in Primary Mental Health Care Service Use and Subsequent Self-Harm in Western Sydney Australia: Policy and Workforce Implications" International Journal of Environmental Research and Public Health 19, no. 6: 3382. https://doi.org/10.3390/ijerph19063382
APA StyleMunasinghe, S., Page, A., Sperandei, S., Gaur, P., Ferdousi, S., Mannan, H., & Brakoulias, V. (2022). Trends in Primary Mental Health Care Service Use and Subsequent Self-Harm in Western Sydney Australia: Policy and Workforce Implications. International Journal of Environmental Research and Public Health, 19(6), 3382. https://doi.org/10.3390/ijerph19063382







