Coping with the COVID-19 Pandemic: Perceived Changes in Psychological Vulnerability, Resilience and Social Cohesion before, during and after Lockdown
Abstract
:1. Introduction
1.1. Psychological Vulnerability
1.2. Resilience
1.3. Social Cohesion
1.4. Psychological Vulnerability, Resilience and Social Cohesion in the Context of the COVID-19 Pandemic
2. Methods
2.1. Sample
2.2. Study Design
2.3. Measures
2.3.1. Vulnerability
2.3.2. Resilience
2.3.3. Social Cohesion
2.4. Data Analysis
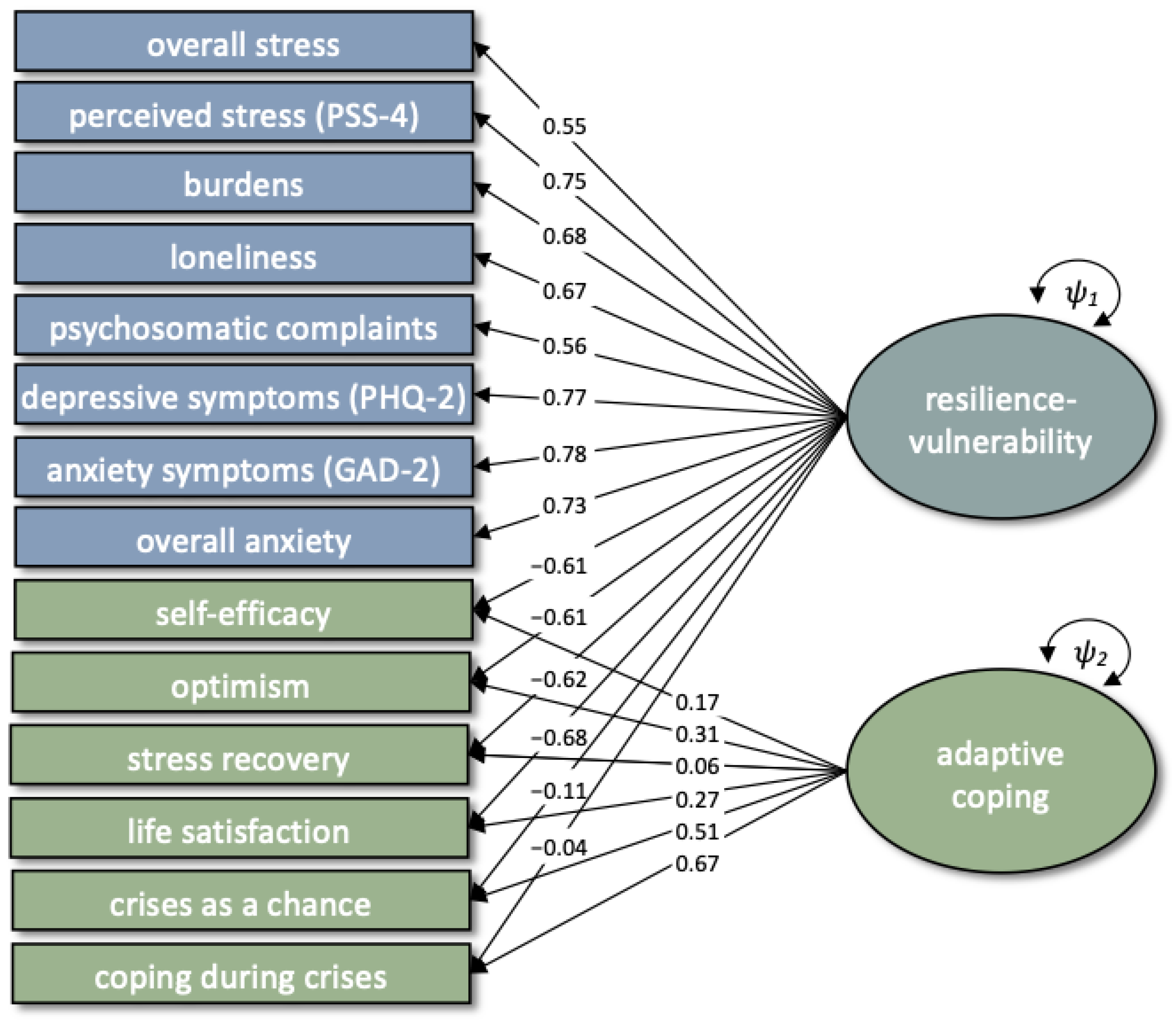
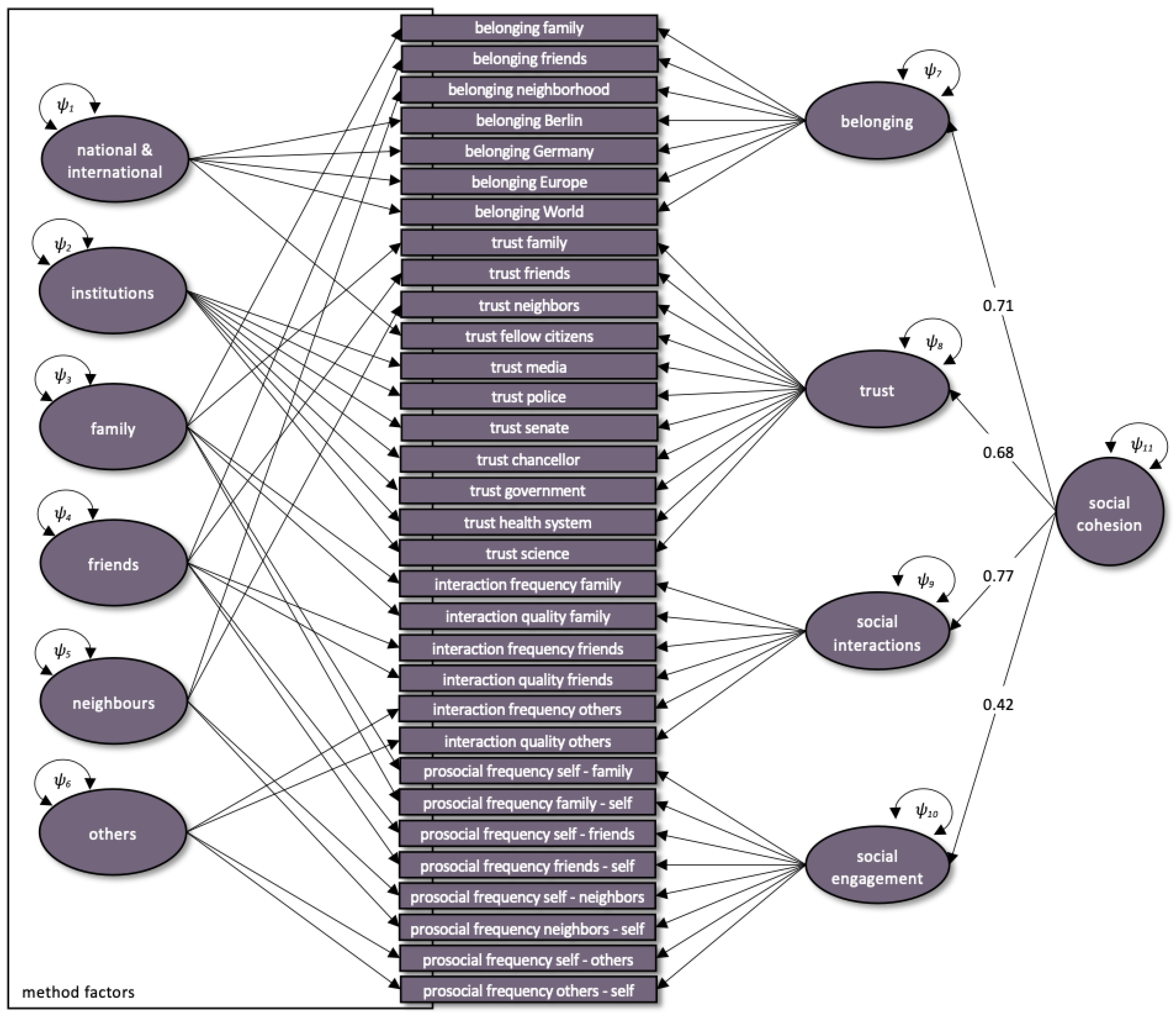
2.4.1. Factor Analyses for Single Constructs
2.4.2. Integrative Measurement Models
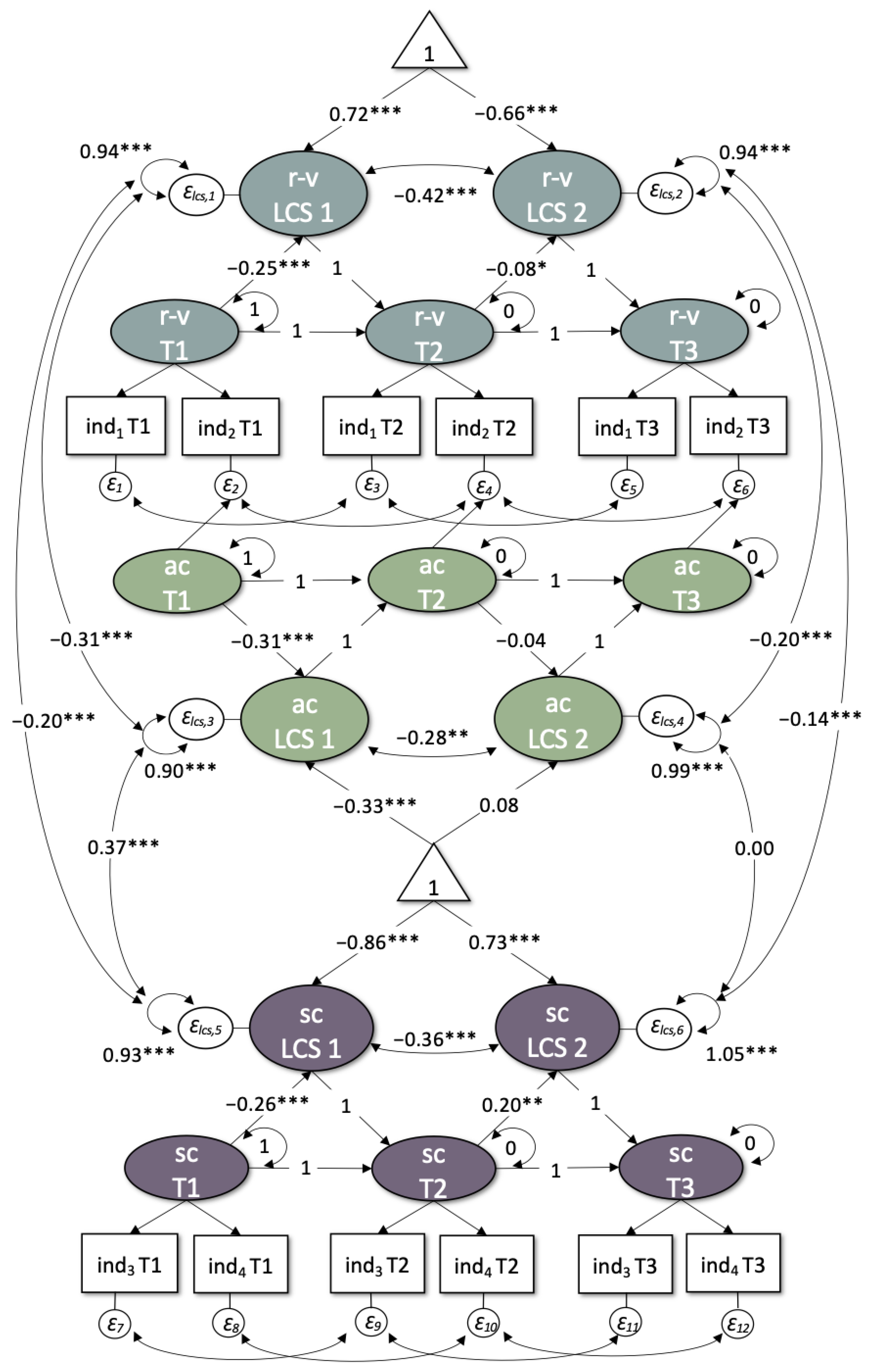
2.4.3. Latent Change Score Modeling
3. Results
3.1. Factor Structure
3.1.1. Vulnerability
3.1.2. Resilience
3.1.3. Social Cohesion
3.1.4. Integrative and Invariant Factor Structure
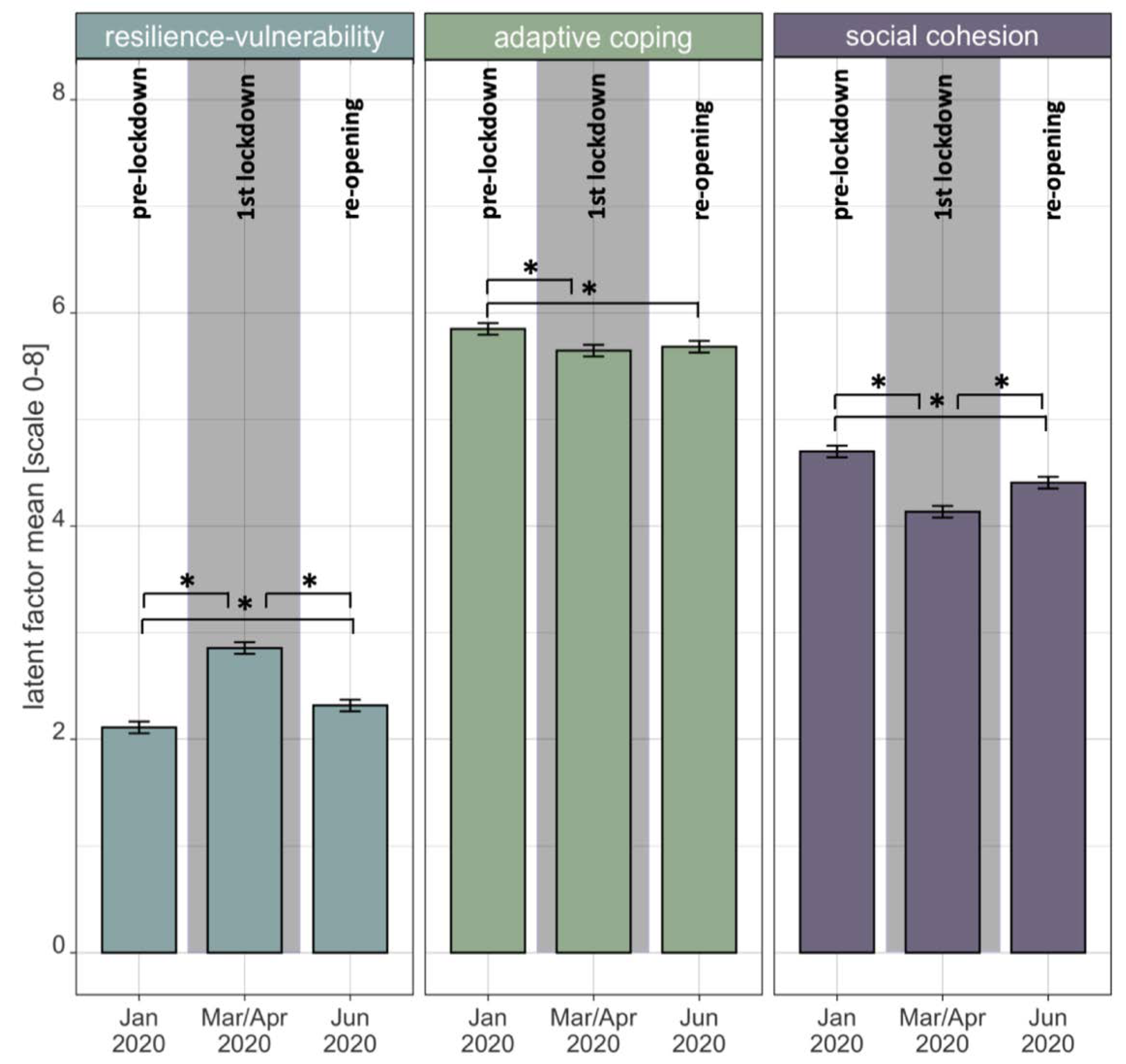
3.2. Within-Construct Changes and Predictions of Change
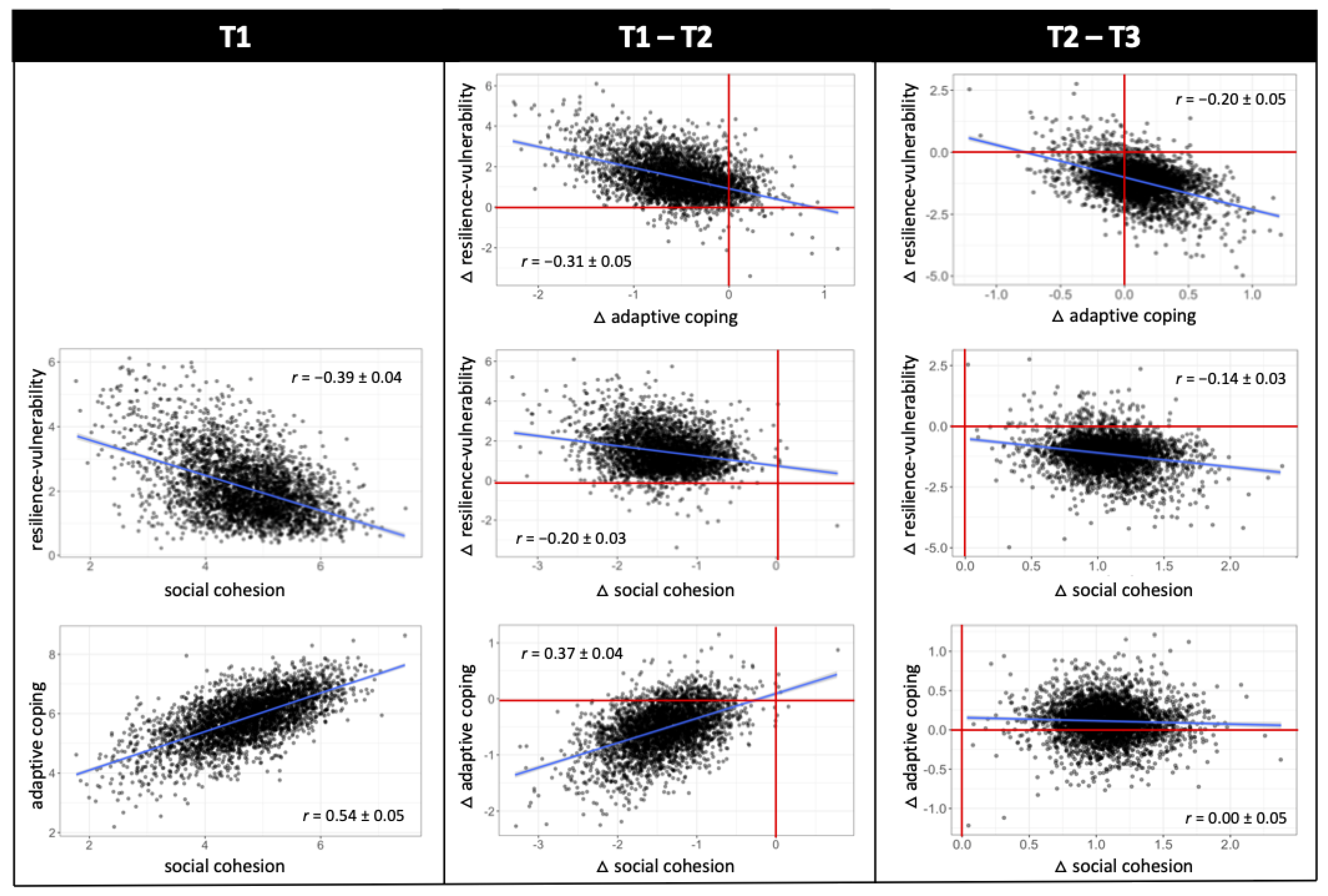
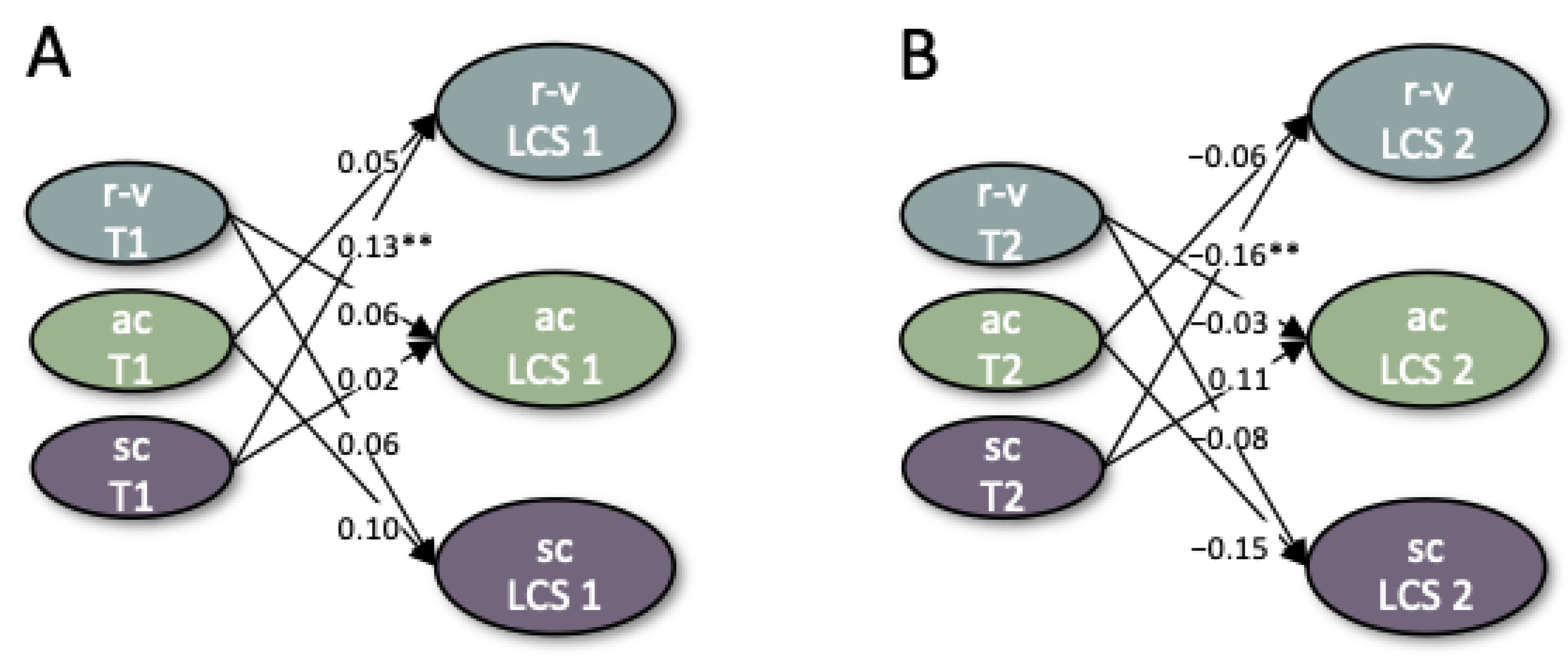
3.3. Between-Construct Interrelations and Predictions of Change
4. Discussion
4.1. Factor Structure
4.2. Within-Construct Changes and Predictions of Change
4.3. Between-Construct Interrelations and Predictions of Change
4.4. Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- O’Connor, R.C.; Wetherall, K.; Cleare, S.; McClelland, H.; Melson, A.J.; Niedzwiedz, C.L.; O’Carroll, R.E.; O’Connor, D.B.; Platt, S.; Scowcroft, E.; et al. Mental health and well-being during the COVID-19 pandemic: Longitudinal analyses of adults in the UK COVID-19 Mental Health & Wellbeing study. Br. J. Psychiatry 2021, 218, 326–333. [Google Scholar] [PubMed]
- Pfefferbaum, B.; North, C.S. Mental health and the COVID-19 pandemic. N. Engl. J. Med. 2020, 383, 510–512. [Google Scholar] [CrossRef] [PubMed]
- Vindegaard, N.; Benros, M.E. COVID-19 pandemic and mental health consequences: Systematic review of the current evidence. Brain. Behav. Immun. 2020, 89, 531–542. [Google Scholar] [CrossRef] [PubMed]
- Xiong, J.; Lipsitz, O.; Nasri, F.; Lui, L.M.W.; Gill, H.; Phan, L.; Chen-Li, D.; Iacobucci, M.; Ho, R.; Majeed, A.; et al. Impact of COVID-19 pandemic on mental health in the general population: A systematic review. J. Affect. Disord. 2020, 277, 55–64. [Google Scholar] [CrossRef]
- Dubey, S.; Biswas, P.; Ghosh, R.; Chatterjee, S.; Dubey, M.J.; Chatterjee, S.; Lahiri, D.; Lavie, C.J. Psychosocial impact of COVID-19. Diabetes Metab. Syndr. Clin. Res. Rev. 2020, 14, 779–788. [Google Scholar] [CrossRef]
- Brooks, S.K.; Webster, R.K.; Smith, L.E.; Woodland, L.; Wessely, S.; Greenberg, N.; Rubin, G.J. The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. Lancet 2020, 395, 912–920. [Google Scholar] [CrossRef] [Green Version]
- Leigh-Hunt, N.; Bagguley, D.; Bash, K.; Turner, V.; Turnbull, S.; Valtorta, N.; Caan, W. An overview of systematic reviews on the public health consequences of social isolation and loneliness. Public Health 2017, 152, 157–171. [Google Scholar] [CrossRef] [Green Version]
- Pancani, L.; Marinucci, M.; Aureli, N.; Riva, P. Forced Social Isolation and Mental Health: A Study on 1,006 Italians Under COVID-19 Lockdown. Front. Psychol. 2021, 12, 1540. [Google Scholar] [CrossRef]
- Wang, J.; Lloyd-Evans, B.; Giacco, D.; Forsyth, R.; Nebo, C.; Mann, F.; Johnson, S. Social isolation in mental health: A conceptual and methodological review. Soc. Psychiatry Psychiatr. Epidemiol. 2017, 52, 1451–1461. [Google Scholar] [CrossRef] [Green Version]
- Blanc, J.; Briggs, A.Q.; Seixas, A.A.; Reid, M.; Jean-Louis, G.; Pandi-Perumal, S.R. Addressing psychological resilience during the coronavirus disease 2019 pandemic: A rapid review. Curr. Opin. Psychiatry 2021, 34, 29–35. [Google Scholar] [CrossRef]
- Killgore, W.; Taylor, E.; Cloonan, S.A.; Dailey, N.S. Psychological resilience during the COVID-19 lockdown. Psychiatry Res. 2020, 291, 113216. [Google Scholar] [CrossRef] [PubMed]
- Verdolini, N.; Amoretti, S.; Montejo, L.; García-Rizo, C.; Hogg, B.; Mezquida, G.; Rabelo-da-Ponte, F.D.; Vallespir, C.; Radua, J.; Martinez-Aran, A.; et al. Resilience and mental health during the COVID-19 pandemic. J. Affect. Disord. 2021, 283, 156–164. [Google Scholar] [CrossRef] [PubMed]
- Borkowska, M.; Laurence, J. Coming together or coming apart? Changes in social cohesion during the COVID-19 pandemic in England. Eur. Soc. 2021, 23, S618–S636. [Google Scholar] [CrossRef]
- Jewett, R.L.; Mah, S.M.; Howell, N.; Larsen, M.M. Social Cohesion and Community Resilience During COVID-19 and Pandemics: A Rapid Scoping Review to Inform the United Nations Research Roadmap for COVID-19 Recovery. Int. J. Health Serv. 2021, 51, 325–336. [Google Scholar] [CrossRef]
- Ingram, R.; Luxton, D.D. Vulnerability-stress models. In Development of Psychopathology: A Vulnerability-Stress Perspective; Hankin, B.L., Abela, J.R.Z., Eds.; SAGE Publications: Los Angeles, CA, USA, 2005; pp. 1–510. ISBN 9781452231655. [Google Scholar]
- Rutter, M. Psychosocial resilience and protective mechanisms. Am. J. Orthopsychiatry 1987, 57, 316–331. [Google Scholar] [CrossRef]
- Egeland, B.; Carlson, E.; Sroufe, L.A. Resilience as process. Dev. Psychopathol. 1993, 5, 517–528. [Google Scholar] [CrossRef]
- Masten, A.S.; Garmezy, N. Risk, vulnerability, and protective factors in developmental psychopathology. In Advances in Clinical Child Psychology; Lahey, B.B., Kazdin, A.E., Eds.; Springer: Boston, MA, USA, 1985; pp. 1–52. [Google Scholar]
- Charney, D.S. Psychobiological Mechanism of Resilience and Vulnerability: Implications for Successful Adaptation to Extreme Stress. Am. J. Psychiatry 2004, 161, 195–216. [Google Scholar] [CrossRef] [Green Version]
- Chan, J.; To, H.P.; Chan, E. Reconsidering social cohesion: Developing a definition and analytical framework for empirical research. Soc. Indic. Res. 2006, 75, 273–302. [Google Scholar] [CrossRef]
- Bottoni, G. A Multilevel Measurement Model of Social Cohesion. Soc. Indic. Res. 2018, 136, 835–857. [Google Scholar] [CrossRef]
- Fone, D.; Dunstan, F.; Lloyd, K.; Williams, G.; Watkins, J.; Palmer, S. Does social cohesion modify the association between area income deprivation and mental health? A multilevel analysis. Int. J. Epidemiol. 2007, 36, 338–345. [Google Scholar] [CrossRef] [Green Version]
- Greene, G.; Paranjothy, S.; Palmer, S.R. Resilience and vulnerability to the psychological harm from flooding: The role of social cohesion. Am. J. Public Health 2015, 105, 1792–1795. [Google Scholar] [CrossRef] [PubMed]
- Gapen, M.; Cross, D.; Ortigo, K.; Graham, A.; Johnson, E.; Evces, M.; Ressler, K.J.; Bradley, B. Perceived neighborhood disorder, community cohesion, and PTSD symptoms among low-income African Americans in an Urban health setting. Am. J. Orthopsychiatry 2011, 81, 31–37. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Friedkin, N.E. Social cohesion. Annu. Rev. Sociol. 2004, 30, 409–425. [Google Scholar] [CrossRef]
- Adger, W.N. Vulnerability. Glob. Environ. Chang. 2006, 16, 268–281. [Google Scholar] [CrossRef]
- Sinclair, V.G.; Wallston, K.A. The development and validation of the psychological vulnerability scale. Cogn. Ther. Res. 1999, 23, 119–129. [Google Scholar] [CrossRef]
- Ingram, R.; Miranda, J.; Segal, Z. Cognitive vulnerability to depression. In Cognitive Vulnerability to Emotional Disorders; Alloy, L.B., Riskind, J.H., Eds.; Routledge: London, UK, 2006; pp. 63–91. ISBN 0805838287. [Google Scholar]
- Fiorenzato, E.; Zabberoni, S.; Costa, A.; Cona, G. Cognitive and mental health changes and their vulnerability factors related to COVID-19 lockdown in Italy. PLoS ONE 2021, 16, e0246204. [Google Scholar] [CrossRef]
- Servidio, R.; Bartolo, M.G.; Palermiti, A.L.; Costabile, A. Fear of COVID-19, depression, anxiety, and their association with Internet addiction disorder in a sample of Italian students. J. Affect. Disord. Reports 2021, 4, 100097. [Google Scholar] [CrossRef]
- Siste, K.; Hanafi, E.; Sen, L.T.; Christian, H.; Adrian; Siswidiani, L.P.; Limawan, A.P.; Murtani, B.J.; Suwartono, C. The Impact of Physical Distancing and Associated Factors Towards Internet Addiction Among Adults in Indonesia During COVID-19 Pandemic: A Nationwide Web-Based Study. Front. Psychiatry 2020, 11, 924. [Google Scholar] [CrossRef]
- Zaami, S.; Marinelli, E.; Varì, M.R. New Trends of Substance Abuse During COVID-19 Pandemic: An International Perspective. Front. Psychiatry 2020, 11, 700. [Google Scholar] [CrossRef]
- Mazza, M.; Marano, G.; Lai, C.; Janiri, L.; Sani, G. Danger in danger: Interpersonal violence during COVID-19 quarantine. Psychiatry Res. 2020, 289, 113046. [Google Scholar] [CrossRef]
- Killgore, W.D.S.; Cloonan, S.A.; Taylor, E.C.; Anlap, I.; Dailey, N.S. Increasing aggression during the COVID-19 lockdowns. J. Affect. Disord. Reports 2021, 5, 100163. [Google Scholar] [CrossRef] [PubMed]
- Yong, J.C.; Choy, B.K.C. Noncompliance With Safety Guidelines as a Free-Riding Strategy: An Evolutionary Game-Theoretic Approach to Cooperation During the COVID-19 Pandemic. Front. Psychol. 2021, 12, 646892. [Google Scholar] [CrossRef] [PubMed]
- Ahrens, K.F.; Neumann, R.J.; Kollmann, B.; Plichta, M.M.; Lieb, K.; Tüscher, O.; Reif, A. Differential impact of COVID-related lockdown on mental health in Germany. World Psychiatry 2021, 20, 140–141. [Google Scholar] [CrossRef] [PubMed]
- Schäfer, S.K.; Sopp, M.R.; Schanz, C.G.; Staginnus, M.; Göritz, A.S.; Michael, T. Impact of COVID-19 on Public Mental Health and the Buffering Effect of a Sense of Coherence. Psychother. Psychosom. 2020, 89, 386–392. [Google Scholar] [CrossRef]
- Holmes, E.A.; O’Connor, R.C.; Perry, V.H.; Tracey, I.; Wessely, S.; Arseneault, L.; Ballard, C.; Christensen, H.; Cohen Silver, R.; Everall, I.; et al. Multidisciplinary research priorities for the COVID-19 pandemic: A call for action for mental health science. Lancet Psychiatry 2020, 7, 547–560. [Google Scholar] [CrossRef]
- Killgore, W.D.; Cloonan, S.A.; Taylor, E.C.; Miller, M.A.; Dailey, N.S. Three months of loneliness during the COVID-19 lockdown. Psychiatry Res. 2020, 293, 113392. [Google Scholar] [CrossRef]
- Loades, M.E.; Chatburn, E.; Higson-Sweeney, N.; Reynolds, S.; Shafran, R.; Brigden, A.; Linney, C.; McManus, M.N.; Borwick, C.; Crawley, E. Rapid systematic review: The impact of social isolation on the mental health of children and adolescents in the context of COVID-19. J. Am. Acad. Child Adolesc. Psychiatry 2020, 59, 1218–1239. [Google Scholar] [CrossRef]
- Nekliudov, N.A.; Blyuss, O.; Cheung, K.Y.; Petrou, L.; Genuneit, J.; Sushentsev, N.; Levadnaya, A.; Comberiati, P.; Warner, J.O.; Tudor-Williams, G.; et al. Excessive media consumption about COVID-19 is associated with increased state anxiety: Outcomes of a large online survey in Russia. J. Med. Internet Res. 2020, 22, e20955. [Google Scholar] [CrossRef]
- Stainback, K.; Hearne, B.N.; Trieu, M.M. COVID-19 and the 24/7 News Cycle: Does COVID-19 News Exposure Affect Mental Health? Socius 2020, 6, 2378023120969339. [Google Scholar] [CrossRef]
- Kalisch, R.; Müller, M.B.; Tüscher, O. A conceptual framework for the neurobiological study of resilience. Behav. Brain Sci. 2015, 38, e92. [Google Scholar] [CrossRef]
- Wright, M.O.; Masten, A.S.; Narayan, A.J. Resilience processes in development: Four waves of research on positive adaptation in the context of adversity. In Handbook of Resilience in Children, 2nd ed.; Goldstein, S., Brooks, R.B., Eds.; Kluwer: New York, NY, USA, 2013; pp. 15–37. [Google Scholar]
- Bonanno, G.A. Resilience in the face of potential trauma. Curr. Dir. Psychol. Sci. 2005, 14, 135–138. [Google Scholar] [CrossRef]
- Masten, A.S.; Lucke, C.M.; Nelson, K.M.; Stallworthy, I.C. Resilience in Development and Psychopathology: Multisystem Perspectives. Annu. Rev. Clin. Psychol. 2021, 17, 521–549. [Google Scholar] [CrossRef] [PubMed]
- Ungar, M.; Theron, L. Resilience and mental health: How multisystemic processes contribute to positive outcomes. Lancet Psychiatry 2020, 7, 441–448. [Google Scholar] [CrossRef]
- Masten, A.S.; Cicchetti, D. Resilience in development: Progress and transformation. In Risk, Resilience, and Intervention, 3rd ed.; Cicchetti, D., Ed.; Wiley: New York, NY, USA, 2016; pp. 271–333. [Google Scholar]
- Panter-Brick, C. Culture and resilience: Next steps for theory and practice. In Youth Resilience and Culture: Commonalities and Complexities; Theron, L.C., Liebenberg, L., Ungar, M., Eds.; Springer: Dordrecht, The Netherlands, 2015; pp. 233–244. [Google Scholar]
- Kaplan, H.B. Toward an understanding of resilience. In Resilience and Development; Glantz, M.D., Johnson, J.L., Eds.; Springer: Boston, MA, USA, 2002; pp. 17–83. [Google Scholar]
- Werner, E.E.; Smith, R.S. Journeys from Childhood to Midlife: Risk, Resilience, and Recovery; Cornell University Press: Ithaca, NY, USA, 2001. [Google Scholar]
- Ingram, R.; Price, J.M. Understanding psychopathology: The role of vulnerability. In Vulnerability to Psychopathology: Risk across the Lifespan; Guilford Press: New York, NY, USA, 2001; pp. 3–17. [Google Scholar]
- Friborg, O.; Hjemdal, O.; Martinussen, M.; Rosenvinge, J.H. Empirical support for resilience as more than the counterpart and absence of vulnerability and symptoms of mental disorder. J. Individ. Differ. 2009, 30, 138–151. [Google Scholar] [CrossRef]
- Huta, V.; Hawley, L. Psychological strengths and cognitive vulnerabilities: Are they two ends of the same continuum or do they have independent relationships with well-being and ill-being? J. Happiness Stud. 2010, 11, 71–93. [Google Scholar] [CrossRef]
- Walker, B.; Holling, C.S.; Carpenter, S.R.; Kinzig, A. Resilience, adaptability and transformability in social-ecological systems. Ecol. Soc. 2004, 9, 5. [Google Scholar] [CrossRef]
- Folke, C. Resilience: The emergence of a perspective for social-ecological systems analyses. Glob. Environ. Chang. 2006, 16, 253–267. [Google Scholar] [CrossRef]
- Carpenter, S.; Walker, B.; Anderies, J.M.; Abel, N. From metaphor to measurement: Resilience of what to what? Ecosystems 2001, 4, 765–781. [Google Scholar] [CrossRef]
- Ong, A.D.; Bergeman, C.S.; Bisconti, T.L.; Wallace, K.A. Psychological resilience, positive emotions, and successful adaptation to stress in later life. J. Pers. Soc. Psychol. 2006, 91, 730–749. [Google Scholar] [CrossRef] [Green Version]
- Vella, S.-L.; Pai, N.B. A theoretical review of psychological resilience: Defining resilience and resilience research over the decades. Arch. Med. Health Sci. 2019, 7, 233. [Google Scholar] [CrossRef]
- Scherer, K.R. Appraisal considered as a process of multilevel sequential checking. Apprais. Processes Emot. Theory Methods Res. 2001, 92, 57. [Google Scholar]
- Scheier, M.F.; Weintraub, J.K.; Carver, C.S. Coping with stress: Divergent strategies of optimists and pessimists. J. Pers. Soc. Psychol. 1986, 51, 1257–1264. [Google Scholar] [CrossRef] [PubMed]
- Russo, S.J.; Murrough, J.W.; Han, M.H.; Charney, D.S.; Nestler, E.J. Neurobiology of resilience. Nat. Neurosci. 2012, 15, 1475–1484. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Linley, P.A.; Joseph, S. Positive Change Following Trauma and Adversity: A Review. J. Trauma. Stress 2004, 17, 11–21. [Google Scholar] [CrossRef]
- Polizzi, C.; Lynn, S.J.; Perry, A. Stress and coping in the time of COVID-19: Pathways to resilience and recovery. Clin. Neuropsychiatry 2020, 17, 59–62. [Google Scholar]
- Petzold, M.B.; Bendau, A.; Plag, J.; Pyrkosch, L.; Mascarell Maricic, L.; Betzler, F.; Rogoll, J.; Große, J.; Ströhle, A. Risk, resilience, psychological distress, and anxiety at the beginning of the COVID-19 pandemic in Germany. Brain Behav. 2020, 10, e01745. [Google Scholar] [CrossRef]
- Veer, I.M.; Riepenhausen, A.; Zerban, M.; Wackerhagen, C.; Puhlmann, L.M.C.; Engen, H.; Köber, G.; Bögemann, S.A.; Weermeijer, J.; Uściłko, A.; et al. Psycho-social factors associated with mental resilience in the Corona lockdown. Transl. Psychiatry 2021, 11, 67. [Google Scholar] [CrossRef]
- Arslan, G.; Yıldırım, M.; Tanhan, A.; Buluş, M.; Allen, K.A. Coronavirus Stress, Optimism-Pessimism, Psychological Inflexibility, and Psychological Health: Psychometric Properties of the Coronavirus Stress Measure. Int. J. Ment. Health Addict. 2020, 2, 2423–2439. [Google Scholar] [CrossRef]
- Trzebiński, J.; Cabański, M.; Czarnecka, J.Z. Reaction to the COVID-19 Pandemic: The Influence of Meaning in Life, Life Satisfaction, and Assumptions on World Orderliness and Positivity. J. Loss Trauma 2020, 25, 544–557. [Google Scholar] [CrossRef]
- Silveira, S.; Hecht, M.; Adli, M.; Voelkle, M.; Singer, T. Exploring the sturcture and interrelations of time-stable psychological resilience, psychological vulnerability and social cohesion. Front. Psychiatry, 2022; in press. [Google Scholar]
- Durkheim, E. Le Suicide: Étude de Sociologie; Alcan: New York, NY, USA, 1897. [Google Scholar]
- McDougall, W. The Group Mind: A Sketch of the Principles of Collective Psychology; Prabhat Prakashan: New Delhi, India, 1921. [Google Scholar]
- Freud, S. Massenpsychologie und Ich-Analyse; Internationaler Psychoanalytischer Verlag: Wien, Austria, 1921. [Google Scholar]
- Festinger, L.; Schachter, S.; Back, K. Social Pressures in Informal Groups: A Study of Human Factors in Housing; Stanford University Press: Redwood City, CA, USA, 1950. [Google Scholar]
- Schiefer, D.; van der Noll, J. The essentials of social cohesion: A literature review. Soc. Indic. Res. 2017, 132, 579–603. [Google Scholar] [CrossRef]
- Fonseca, X.; Lukosch, S.; Brazier, F. Social cohesion revisited: A new definition and how to characterize it. Innov. Eur. J. Soc. Sci. Res. 2019, 32, 231–253. [Google Scholar] [CrossRef]
- Hagerty, B.; Williams, R.A.; Coyne, J.C.; Early, M.R. Sense of belonging and indicators of social and psychological functioning. Arch. Psychiatr. Nurs. 1996, 10, 235–244. [Google Scholar] [CrossRef]
- Dickes, P.; Valentova, M.; Borsenberger, M. Construct Validation and Application of a Common Measure of Social Cohesion in 33 European Countries. Soc. Indic. Res. 2010, 98, 451–473. [Google Scholar] [CrossRef]
- Glaeser, E.L.; Laibson, D.I.; Scheinkman, J.A.; Soutter, C.L. Measuring trust. Q. J. Econ. 2000, 115, 811–846. [Google Scholar] [CrossRef] [Green Version]
- Larsen, C.A. The Rise and Fall of Social Cohesion: The Construction and De-Construction of Social Trust in the US, UK, Sweden and Denmark; Oxford University Press: Oxford, UK, 2013. [Google Scholar]
- Putnam, R. The prosperous community: Social capital and public life. Am. Prospect 1993, 4, 35–42. [Google Scholar]
- Cheong, H.P.; Edwards, R.; Goulbourne, H.; Solomos, J. Immigration, social cohesion and social capital: A critical review. Crit. Soc. Policy 2007, 27, 24–49. [Google Scholar] [CrossRef]
- OECD Perspectives on global development 2012. In Perspectives on Global Development; OECD Publishing: Paris, France, 2011.
- Cattell, R.B. Theory of fluid and crystallized intelligence: A critical experiment. J. Educ. Psychol. 1963, 54, 1–22. [Google Scholar] [CrossRef]
- Baumeister, R.F.; Leary, M.R. The Need to Belong: Desire for Interpersonal Attachments as a Fundamental Human Motivation. Psychol. Bull. 1995, 117, 497–529. [Google Scholar] [CrossRef]
- Taylor, S.E. Tend and befriend: Biobehavioral bases of affiliation under stress. Curr. Dir. Psychol. Sci. 2006, 15, 273–277. [Google Scholar] [CrossRef]
- von Dawans, B.; Fischbacher, U.; Kirschbaum, C.; Fehr, E.; Heinrichs, M. The Social Dimension of Stress Reactivity: Acute Stress Increases Prosocial Behavior in Humans. Psychol. Sci. 2012, 23, 651–660. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Uchida, Y.; Takahashi, Y.; Kawahara, K. Changes in hedonic and eudaimonic well-being after a severe nationwide disaster: The case of the Great East Japan Earthquake. J. Happiness Stud. 2014, 15, 207–221. [Google Scholar] [CrossRef] [Green Version]
- Holt-Lunstad, J.; Smith, T.B.; Baker, M.; Harris, T.; Stephenson, D. Loneliness and Social Isolation as Risk Factors for Mortality: A Meta-Analytic Review. Perspect. Psychol. Sci. 2015, 10, 227–237. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rollston, R.; Galea, S. COVID-19 and the Social Determinants of Health. Am. J. Health Promot. 2020, 34, 687–689. [Google Scholar] [CrossRef] [PubMed]
- Galea, S.; Abdalla, S.M. COVID-19 pandemic, unemployment, and civil unrest: Underlying deep racial and socioeconomic divides. JAMA 2020, 324, 227–228. [Google Scholar] [CrossRef] [PubMed]
- Van Dorn, A.; Cooney, R.E.; Sabin, M.L. COVID-19 exacerbating inequalities in the US. Lancet 2020, 395, 1243–1244. [Google Scholar] [CrossRef]
- Dorn, F.; Fuest, C.; Göttert, M.; Krolage, C.; Lautenbacher, S.; Lehmann, R.; Link, S.; Möhrle, S.; Peichl, A.; Reif, M.; et al. The Economic Costs of the Coronavirus Shutdown for Selected European Countries: A Scenario Calculation; EconPol Policy Brief No. 25; IFO Institute—Leibniz Institute for Economic Research at the University of Munich: Munich, Germany, 2020. [Google Scholar]
- Fletcher, D.; Sarkar, M. Psychological resilience: A review and critique of definitions, concepts and theory. Eur. Psychol. 2013, 18, 12–23. [Google Scholar] [CrossRef] [Green Version]
- Ungar, M.; Brown, M.; Liebenberg, L.; Othman, R. Unique pathways to resilience across cultures. Adolescence 2007, 42, 287. [Google Scholar]
- Snyder-Mackler, N.; Burger, J.R.; Gaydosh, L.; Daniel, W.; Noppert, G.A.; Campos, F.A.; Yang, Y.C.; Aiello, A.E.; O’Rand, A.; Harris, K.M.; et al. Social determinants of health and survival in humans and other animals. Science 2020, 368, 6493. [Google Scholar] [CrossRef]
- Nitschke, J.P.; Forbes, P.A.G.; Ali, N.; Cutler, J.; Apps, M.A.J.; Lockwood, P.L.; Lamm, C. Resilience during uncertainty? Greater social connectedness during COVID-19 lockdown is associated with reduced distress and fatigue. Br. J. Health Psychol. 2021, 26, 553–569. [Google Scholar] [CrossRef]
- Lowe, S.R.; Chan, C.S.; Rhodes, J.E. Pre-hurricane perceived social support protects against psychological distress: A longitudinal analysis of low-income mothers. J. Consult. Clin. Psychol. 2010, 78, 551–560. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rodriguez-llanes, J.M.; Vos, F.; Guha-Sapir, D. Measuring psychological resilience to disasters: Are evidence-based indicators an achievable goal? Environ. Health 2013, 12, 115. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Townshend, I.; Awosoga, O.; Kulig, J.; Fan, H. Social cohesion and resilience across communities that have experienced a disaster. Nat. Hazards 2015, 76, 913–938. [Google Scholar] [CrossRef]
- Magis, K. Community resilience: An indicator of social sustainability. Soc. Nat. Resour. 2010, 23, 401–416. [Google Scholar] [CrossRef]
- Carroll, M.S.; Cohn, P.J.; Seesholtz, D.N.; Higgins, L.L. Fire as a galvanizing and fragmenting influence on communities: The case of the Rodeo-Chediski fire. Soc. Nat. Resour. 2005, 18, 301–320. [Google Scholar] [CrossRef]
- Vollhardt, J.R. Altruism born of suffering and prosocial behavior following adverse life events: A review and conceptualization. Soc. Justice Res. 2009, 22, 53–97. [Google Scholar] [CrossRef]
- Tedeschi, R.G.; Park, C.L.; Calhoun, L.G. Posttraumatic Growth; Routledge: London, UK, 1998. [Google Scholar]
- Bush, K.; Kivlahan, D.R.; McDonell, M.B.; Fihn, S.D.; Bradley, K.A. The AUDIT alcohol consumption questions (AUDIT-C): An effective brief screening test for problem drinking. Arch. Intern. Med. 1998, 158, 1789–1795. [Google Scholar] [CrossRef] [Green Version]
- Besser, B.; Rumpf, H.J.; Bischof, A.; Meerkerk, G.J.; Higuchi, S.; Bischof, G. Internet-Related Disorders: Development of the Short Compulsive Internet Use Scale. Cyberpsychol. Behav. Soc. Netw. 2017, 20, 709–717. [Google Scholar] [CrossRef]
- Cohen, S.; Kamarck, T.; Mermelstein, R. A global measure of perceived stress. J. Health Soc. Behav. 1983, 24, 385–396. [Google Scholar] [CrossRef]
- Löwe, B.; Kroenke, K.; Gräfe, K. Detecting and monitoring depression with a two-item questionnaire (PHQ-2). J. Psychosom. Res. 2005, 58, 163–171. [Google Scholar] [CrossRef]
- Spitzer, R.L.; Kroenke, K.; Williams, J.B.W.; Loewe, B. A Brief Measure for Assessing Generalized Anxiety Disorder: The GAD-7. Arch. Intern. Med. 2006, 166, 1092–1097. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Beierlein, C.; Kemper, C.; Kovaleva, A.; Rammstedt, B. Short scale for measuring general self-efficacy (ASKU). Kurzskala zur Erfassung allgemeiner Selbstwirksamkeitserwartungen (ASKU). Methoden Daten Anal. 2013, 7, 251–278. [Google Scholar]
- Aron, A.; Aron, E.N.; Smollan, D. Inclusion of other in the self scale and the structure of interpersonal closeness. J. Pers. Soc. Psychol. 1992, 63, 596–612. [Google Scholar] [CrossRef]
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2020. [Google Scholar]
- Rosseel, Y. lavaan: An R package for structural equation modeling and more. J. Stat. Softw. 2012, 48, 1–36. [Google Scholar] [CrossRef] [Green Version]
- Enders, C.K. The impact of nonnormality on full information maximum-likelihood estimation for structural equation models with missing data. Psychol. Methods 2001, 6, 352–370. [Google Scholar] [CrossRef] [PubMed]
- Enders, C.K.; Bandalos, D.L. The relative performance of full information maximum likelihood estimation for missing data in structural equation models. Struct. Equ. Model. 2001, 8, 430–457. [Google Scholar] [CrossRef]
- Lai, K. Estimating standardized SEM parameters given nonnormal data and incorrect model: Methods and comparison. Struct. Equ. Model. 2018, 25, 600–620. [Google Scholar] [CrossRef]
- Sass, D.A.; Schmitt, T.A. A comparative investigation of rotation criteria within exploratory factor analysis. Multivar. Behav. Res. 2010, 45, 73–103. [Google Scholar] [CrossRef]
- Chen, F.F.; Sousa, K.H.; West, S.G. Testing measurement invariance of second-order factor models. Struct. Equ. Model. 2005, 12, 471–492. [Google Scholar] [CrossRef]
- Liu, Y.; Millsap, R.E.; West, S.G.; Tein, J.Y.; Tanaka, R.; Grimm, K.J. Testing measurement invariance in longitudinal data with ordered-categorical measures. Psychol. Methods 2017, 22, 486–506. [Google Scholar] [CrossRef]
- Kievit, R.A.; Brandmaier, A.M.; Ziegler, G.; van Harmelen, A.L.; de Mooij, S.M.M.; Moutoussis, M.; Goodyer, I.M.; Bullmore, E.; Jones, P.B.; Fonagy, P.; et al. Developmental cognitive neuroscience using latent change score models: A tutorial and applications. Dev. Cogn. Neurosci. 2018, 33, 99–117. [Google Scholar] [CrossRef] [PubMed]
- McArdle, J.J. Latent variable modeling of differences and changes with longitudinal data. Annu. Rev. Psychol. 2009, 60, 577–605. [Google Scholar] [CrossRef] [PubMed]
- Gallopín, G.C. Linkages between vulnerability, resilience, and adaptive capacity. Glob. Environ. Chang. 2006, 16, 293–303. [Google Scholar] [CrossRef]
- Little, T.D.; Siegers, D.W.; Card, N.A. A non-arbitrary method of identifying and scaling latent variables in SEM and MACS models. Struct. Equ. Model. 2006, 13, 59–72. [Google Scholar] [CrossRef]
- Smit, B.; Wandel, J. Adaptation, adaptive capacity and vulnerability. Glob. Environ. Chang. 2006, 16, 282–292. [Google Scholar] [CrossRef]
- Jacobi, F.; Höfler, M.; Strehle, J.; Mack, S.; Gerschler, A.; Scholl, L.; Wittchen, H.U. Mental disorders in the general population: Study on the health of adults in Germany and the additional module mental health (DEGS1-MH). Nervenarzt 2014, 85, 77–87. [Google Scholar] [CrossRef]
- Harrison, J.L.; Montgomery, C.A.; Bliss, J.C. Beyond the monolith: The role of bonding, bridging, and linking social capital in the cycle of adaptive capacity. Soc. Nat. Resour. 2016, 29, 525–539. [Google Scholar] [CrossRef]
- Pelling, M.; High, C. Understanding adaptation: What can social capital offer assessments of adaptive capacity? Glob. Environ. Chang. 2005, 15, 308–319. [Google Scholar] [CrossRef]
- Cummins, R.A.; Wooden, M. Personal Resilience in Times of Crisis: The Implications of SWB Homeostasis and Set-Points. J. Happiness Stud. 2014, 15, 223–235. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Silveira, S.; Hecht, M.; Matthaeus, H.; Adli, M.; Voelkle, M.C.; Singer, T. Coping with the COVID-19 Pandemic: Perceived Changes in Psychological Vulnerability, Resilience and Social Cohesion before, during and after Lockdown. Int. J. Environ. Res. Public Health 2022, 19, 3290. https://doi.org/10.3390/ijerph19063290
Silveira S, Hecht M, Matthaeus H, Adli M, Voelkle MC, Singer T. Coping with the COVID-19 Pandemic: Perceived Changes in Psychological Vulnerability, Resilience and Social Cohesion before, during and after Lockdown. International Journal of Environmental Research and Public Health. 2022; 19(6):3290. https://doi.org/10.3390/ijerph19063290
Chicago/Turabian StyleSilveira, Sarita, Martin Hecht, Hannah Matthaeus, Mazda Adli, Manuel C. Voelkle, and Tania Singer. 2022. "Coping with the COVID-19 Pandemic: Perceived Changes in Psychological Vulnerability, Resilience and Social Cohesion before, during and after Lockdown" International Journal of Environmental Research and Public Health 19, no. 6: 3290. https://doi.org/10.3390/ijerph19063290
APA StyleSilveira, S., Hecht, M., Matthaeus, H., Adli, M., Voelkle, M. C., & Singer, T. (2022). Coping with the COVID-19 Pandemic: Perceived Changes in Psychological Vulnerability, Resilience and Social Cohesion before, during and after Lockdown. International Journal of Environmental Research and Public Health, 19(6), 3290. https://doi.org/10.3390/ijerph19063290






