The Impact of the COVID-19 Pandemic on Hospital Services for Patients with Cardiac Diseases: A Scoping Review
Abstract
:1. Introduction
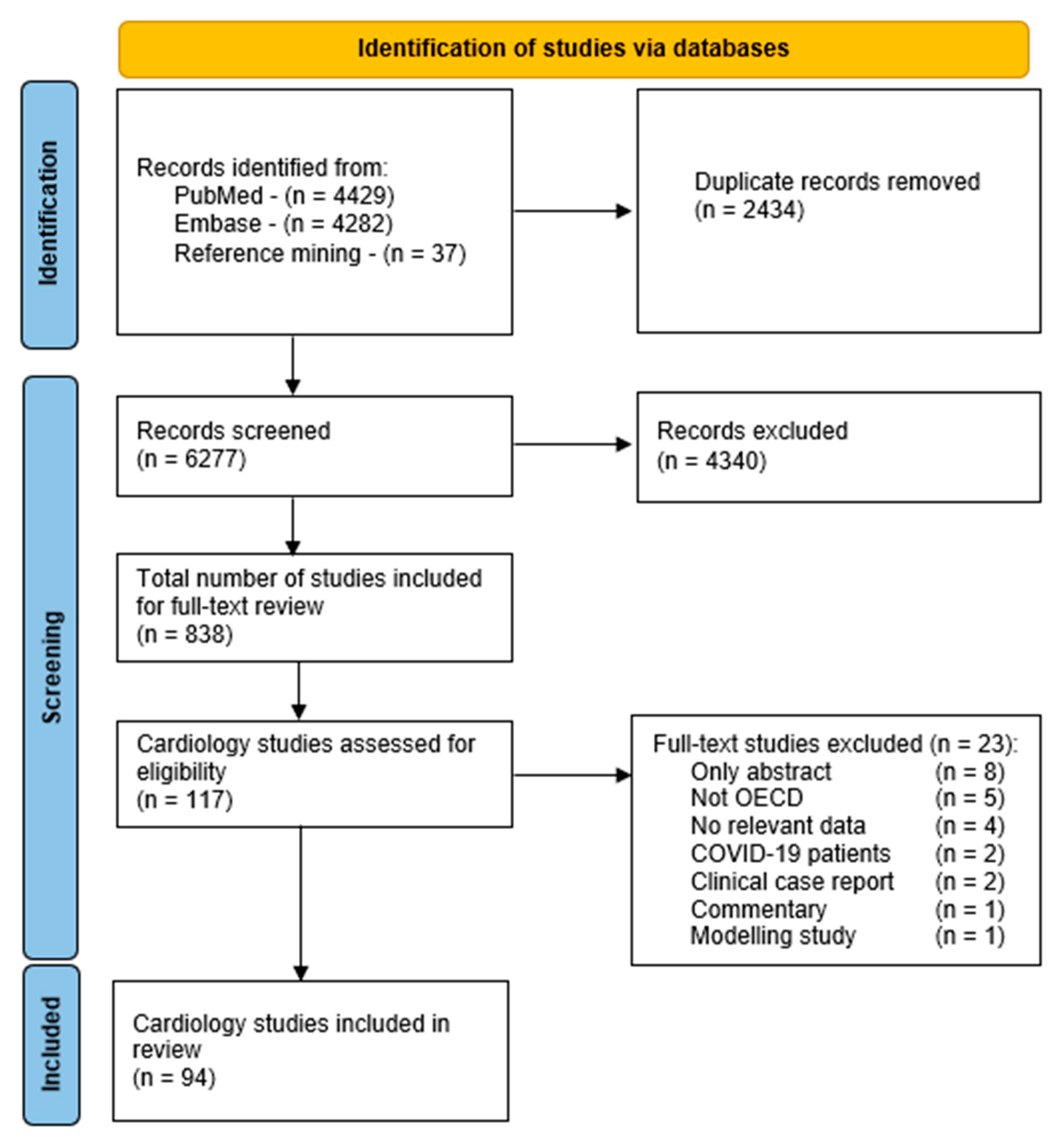
2. Materials and Methods
2.1. Search Strategy
2.2. Study Selection
2.3. Methods of Selection
2.4. Data Extraction and Charting
2.5. Synthesis of the Results
3. Results
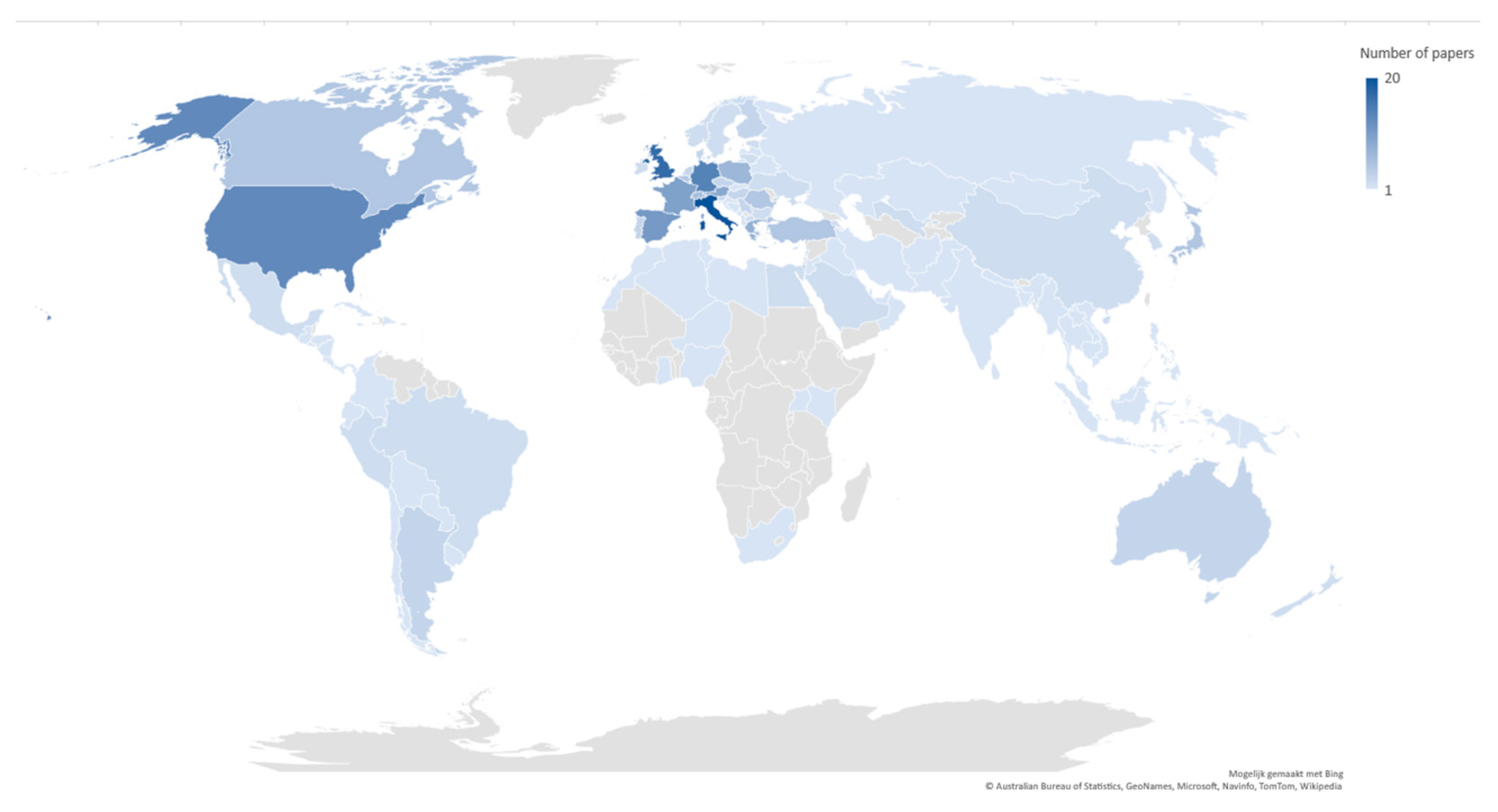
3.1. General Characteristics of the Included Articles
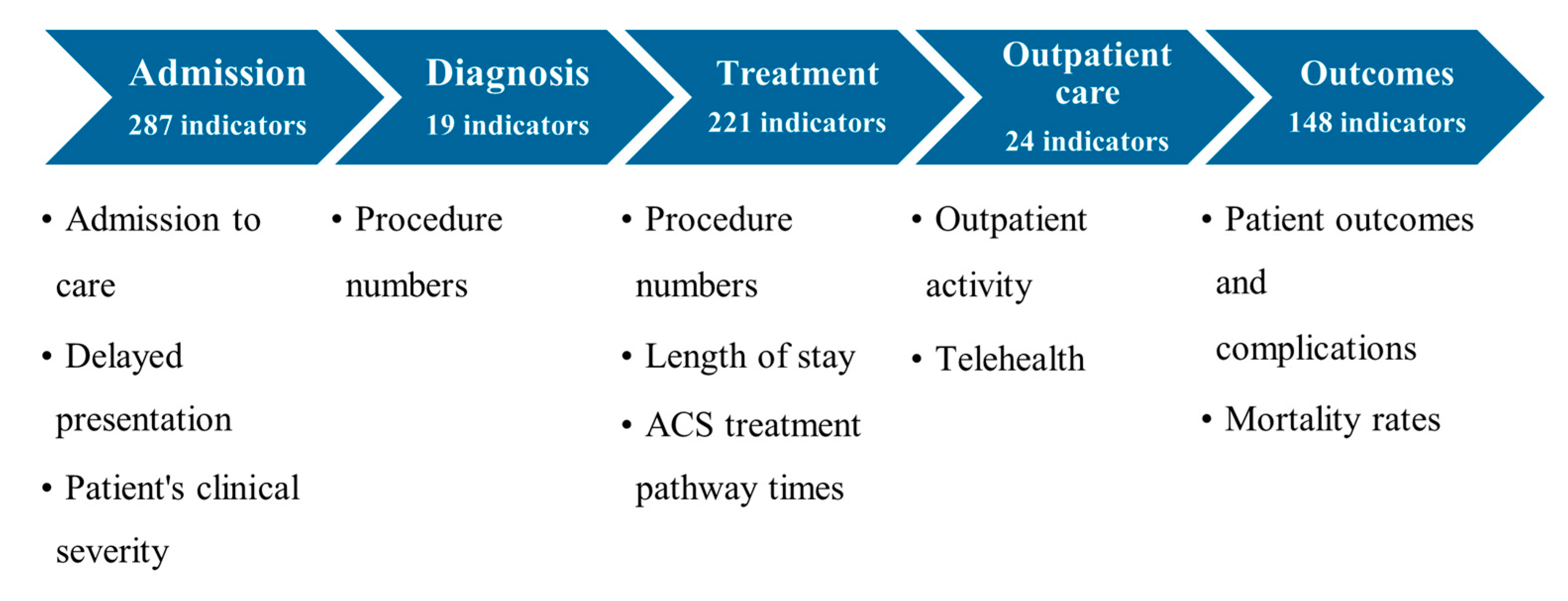
3.2. Impact of COVID-19 on the Hospital Cardiac Care Pathway
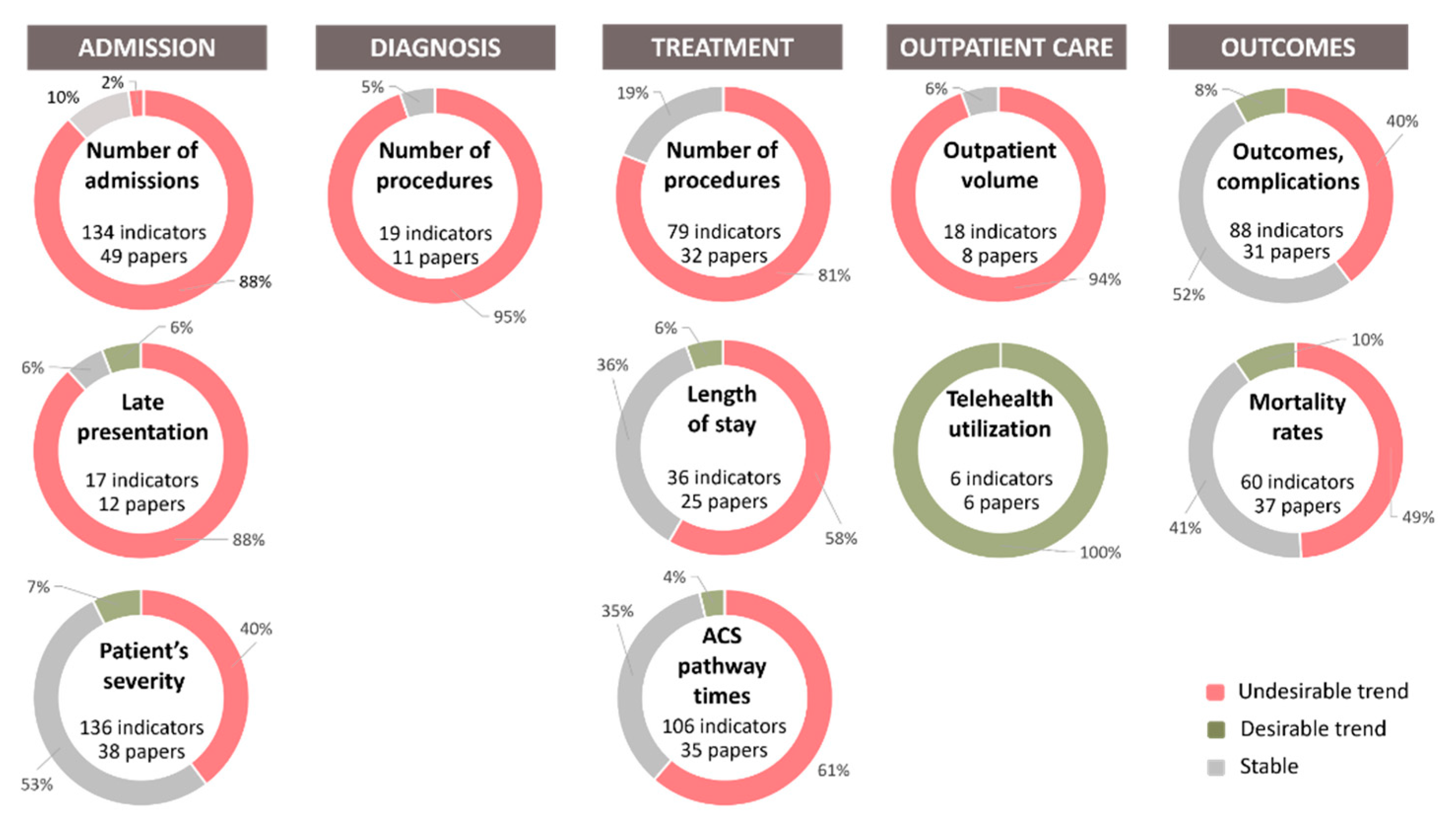
3.2.1. Admission
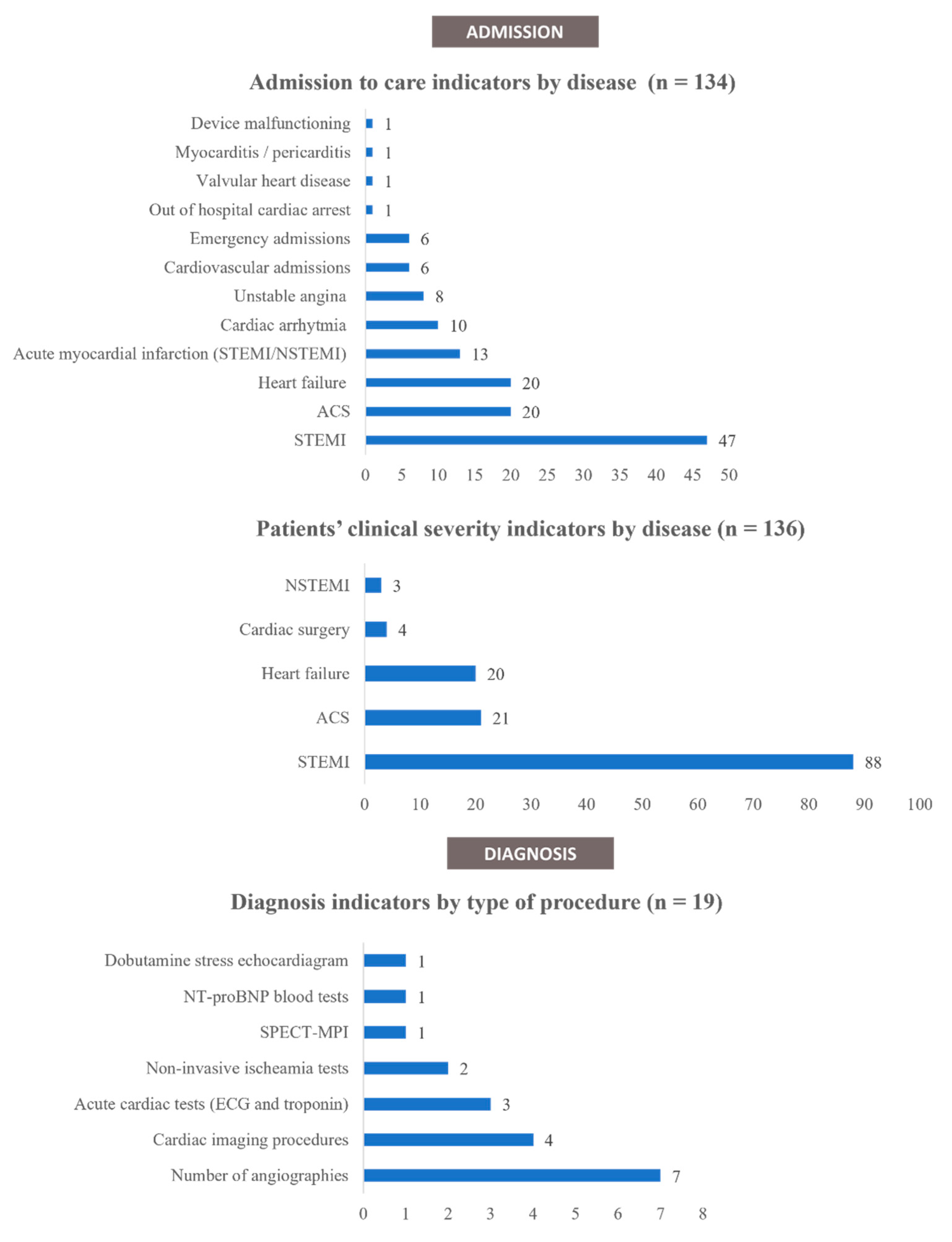
- Admission to care
- Delayed presentation
- Patients’ clinical severity
3.2.2. Diagnosis
3.2.3. Treatment
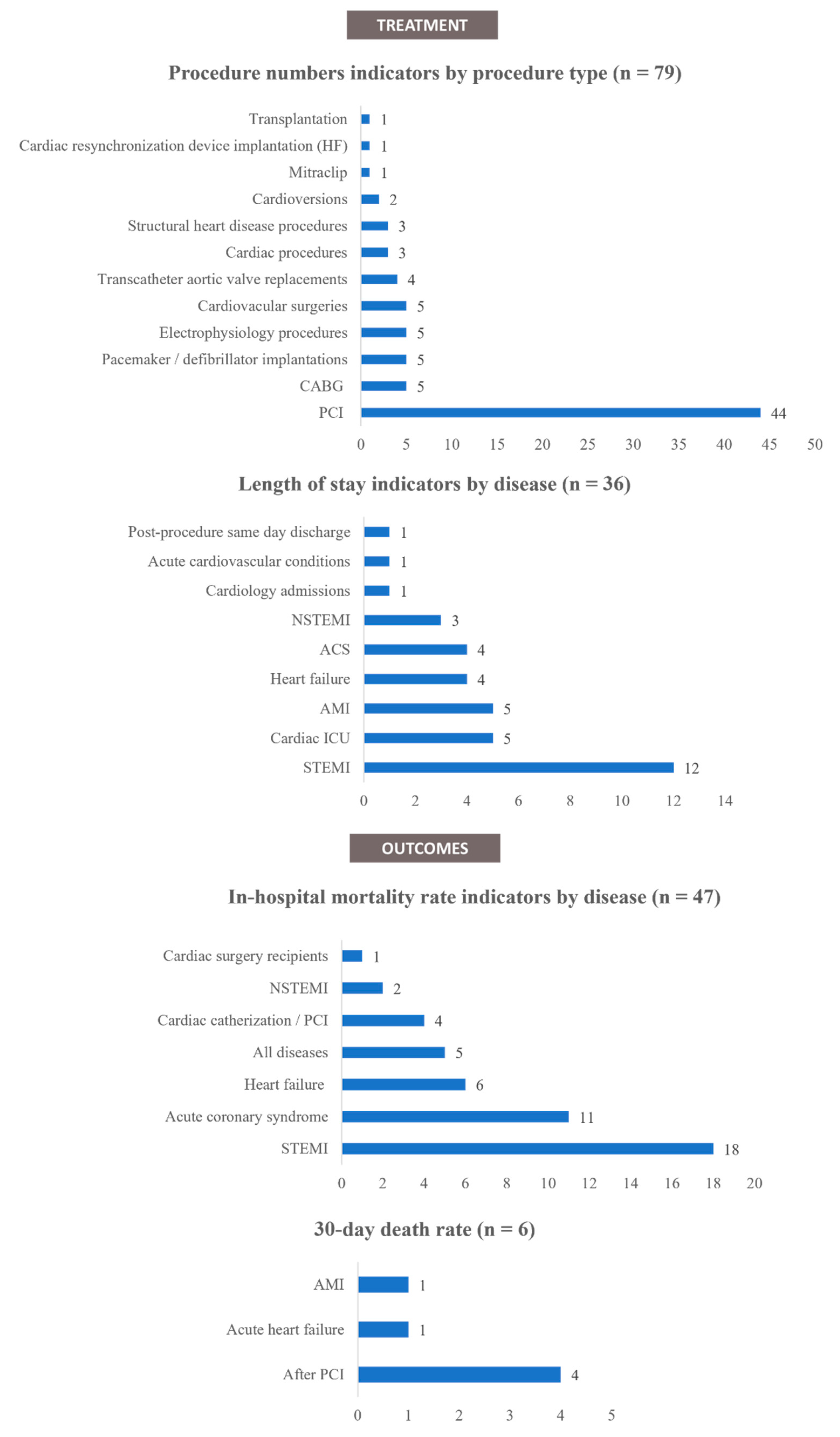
- Procedure numbers
- Length of stay
- Acute Coronary Syndrome treatment pathway times
3.2.4. Outpatient Care
- Outpatient activity volume
- Telehealth
3.2.5. Outcomes
- Outcomes and complications
- Mortality rates
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Wu, F.; Zhao, S.; Yu, B.; Chen, Y.; Wang, W.; Song, Z.; Hu, Y.; Tao, Z.; Tian, J.; Pei, Y.; et al. A new coronavirus associated with human respiratory disease in China. Nature 2020, 579, 265–269. [Google Scholar] [CrossRef] [Green Version]
- Johns Hopkins Coronavirus Resource Centre. Johns Hopkins University and Medicine, COVID-19 Map. 2022. Available online: https://coronavirus.jhu.edu/map.html (accessed on 12 January 2022).
- Listings of WHO’s Response to COVID-19. 2020. Available online: https://www.who.int/news/item/29-06-2020-covidtimeline (accessed on 28 July 2021).
- Moletta, L.; Pierobon, E.S.; Capovilla, G.; Costantini, M.; Salvador, R.; Merigliano, S.; Valmasoni, M. International guidelines and recommendations for surgery during COVID-19 pandemic: A systematic review. Int. J. Surg. 2020, 79, 180–188. [Google Scholar] [CrossRef]
- AHA/ASA Stroke Council Leadership. Temporary emergency guidance to US stroke centers during the coronavirus disease 2019 (COVID-19) pandemic: On behalf of the American Heart Association/American Stroke Association Stroke Council Leadership. Stroke 2020, 51, 1910–1912. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fisher, L.; Polonsky, W.; Asuni, A.; Jolly, Y.; Hessler, D. The early impact of the COVID-19 pandemic on adults with type 1 or type 2 diabetes: A national cohort study. J. Diabetes Complicat. 2020, 34, 107748. [Google Scholar] [CrossRef] [PubMed]
- Nakayama, A.; Takayama, N.; Kobayashi, M.; Hyodo, K.; Maeshima, N.; Takayuki, F.; Morita, H.; Komuro, I. Remote cardiac rehabilitation is a good alternative of outpatient cardiac rehabilitation in the COVID-19 era. Environ. Health Prev. Med. 2020, 25, 48. [Google Scholar] [CrossRef]
- Nyante, S.J.; Benefield, T.S.; Kuzmiak, C.M.; Earnhardt, K.; Pritchard, M.; Henderson, L.M. Population-level impact of coronavirus disease 2019 on breast cancer screening and diagnostic procedures. Cancer 2021, 127, 2111–2121. [Google Scholar] [CrossRef]
- Oba, A.; Stoop, T.F.; Löhr, M.; Hackert, T.; Zyromski, N.; Nealon, W.H.; Unno, M.; Schulick, R.D.; Al-Musawi, M.H.; Wu, W.; et al. Global survey on pancreatic surgery during the COVID-19 pandemic. Ann. Surg. 2020, 272, e87–e93. [Google Scholar] [CrossRef]
- Sokolski, M.; Gajewski, P.; Zymliński, R.; Biegus, J.; Berg, J.M.T.; Bor, W.; Braunschweig, F.; Caldeira, D.; Cuculi, F.; D’Elia, E.; et al. Impact of coronavirus disease 2019 (COVID-19) outbreak on acute admissions at the emergency and cardiology departments across Europe. Am. J. Med. 2021, 134, 482–489. [Google Scholar] [CrossRef]
- Weber, T.; Januszewicz, A.; Rosei, E.; Tsioufis, K.; Okorie, M.; Stergiou, G.; Volpe, M.; Kreutz, R.; Abraham, G.; Azizi, M.; et al. The coronavirus disease 2019 pandemic compromised routine care for hypertension: A survey conducted among excellence centers of the European Society of Hypertension. J. Hypertens. 2021, 39, 190–195. [Google Scholar]
- World Health Organization. NCDs and COVID-19. 2021. Available online: https://www.who.int/teams/noncommunicable-diseases/covid-19 (accessed on 29 July 2021).
- World Health Organization. Factsheet on Cardiovascular Diseases (CVDs). 2021. Available online: https://www.who.int/news-room/fact-sheets/detail/cardiovascular-diseases-(cvds) (accessed on 16 August 2021).
- OECD; The King’s Fund. Is Cardiovascular Disease Slowing Improvements in Life Expectancy? OECD Publishing: Paris, France, 2020. [Google Scholar]
- Bhatia, R.T.; Gati, S.; Papadakis, M.; Sharma, S. The impact of COVID-19 on the continuity of cardiovascular care. Eur. Heart J. 2021, 42, 215–217. [Google Scholar] [CrossRef] [PubMed]
- Kiss, P.; Carcel, C.; Hockham, C.; Peters, S.A.E. The impact of the COVID-19 pandemic on the care and management of patients with acute cardiovascular disease: A systematic review. Eur. Heart J. Qual. Care Clin. Outcomes 2021, 7, 18–27. [Google Scholar] [CrossRef] [PubMed]
- Gadella, A.; Sastre, M.Á.; Maicas, C.; Rodríguez-Padial, L.; Arias, M.Á. ST-segment elevation myocardial infarction in times of COVID-19: Back to the last century? A call for attention. Rev. Esp. Cardiol. 2020, 73, 582–583. [Google Scholar] [CrossRef] [PubMed]
- Moroni, F.; Gramegna, M.; Ajello, S.; Beneduce, A.; Baldetti, L.; Vilca, L.M.; Cappelletti, A.; Scandroglio, A.M.; Azzalini, L. Collateral damage: Medical care avoidance behavior among patients with myocardial infarction during the COVID-19 pandemic. JACC Case Rep. 2020, 2, 1620–1624. [Google Scholar] [CrossRef] [PubMed]
- De Rosa, S.; Spaccarotella, C.; Basso, C.; Calabrò, M.P.; Curcio, A.; Filardi, P.P.; Mancone, M.; Mercuro, G.; Muscoli, S.; Nodari, S.; et al. Reduction of hospitalizations for myocardial infarction in Italy in the COVID-19 era. Eur. Heart J. 2020, 41, 2083–2088. [Google Scholar] [CrossRef] [PubMed]
- Cho, K.H.; Han, X.; Ahn, J.H.; Hyun, D.Y.; Kim, M.C.; Sim, D.S.; Hong, Y.J.; Kim, J.H.; Ahn, Y.; Hwang, J.Y.; et al. Long-term outcomes of patients with late presentation of ST-segment elevation myocardial infarction. J. Am. Coll. Cardiol. 2021, 77, 1859–1870. [Google Scholar] [CrossRef]
- Munn, Z.; Peters, M.D.J.; Stern, C.; Tufanaru, C.; McArthur, A.; Aromataris, E. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med. Res. Methodol. 2018, 18, 143. [Google Scholar] [CrossRef]
- Arksey, H.; O’Malley, L. Scoping studies: Towards a methodological framework. Int. J. Soc. Res. Methodol. 2005, 8, 19–32. [Google Scholar] [CrossRef] [Green Version]
- Levac, D.; Colquhoun, H.; O’Brien, K.K. Scoping studies: Advancing the methodology. Implement. Sci. 2010, 5, 69. [Google Scholar] [CrossRef] [Green Version]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L.; et al. PRISMA extension for scoping reviews (PRISMA-ScR): Checklist and explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef] [Green Version]
- Ouzzani, M.; Hammady, H.; Fedorowicz, Z.; Elmagarmid, A. Rayyan—A web and mobile app for systematic reviews. Syst. Rev. 2016, 5, 210. [Google Scholar] [CrossRef] [Green Version]
- Alba, A.; Frankfurter, C.; Buchan, T.; Kobulnik, J.; Luk, A.; McDonald, M.; Ross, H.; Lee, D. Reduced rate of hospital presentations for heart failure during the COVID-19 pandemic in Toronto, Canada. Can. J. Cardiol. 2020, 36, S74. [Google Scholar] [CrossRef]
- Araiza-Garaygordobil, D.; Montalto, C.; Martinez-Amezcua, P.; Cabello-Lopez, A.; Gopar-Nieto, R.; Alabrese, R.; Almaghraby, A.; Catoya-Villa, S.; Chacon-Diaz, M.; Kaufmann, C.C.; et al. Impact of the COVID-19 pandemic on hospitalizations for acute coronary syndromes: A multinational study. QJM 2021, 114, 642–647. [Google Scholar] [CrossRef]
- Ball, S.; Banerjee, A.; Berry, C.; Boyle, J.R.; Bray, B.; Bradlow, W.; Chaudhry, A.; Crawley, R.; Danesh, J.; Denniston, A.; et al. Monitoring indirect impact of COVID-19 pandemic on services for cardiovascular diseases in the UK. Heart 2020, 106, 1890–1897. [Google Scholar] [CrossRef]
- Bhatt, A.S.; Moscone, A.; McElrath, E.E.; Varshney, A.S.; Claggett, B.L.; Bhatt, D.L.; Januzzi, J.L.; Butler, J.; Adler, D.S.; Solomon, S.D.; et al. Fewer hospitalizations for acute cardiovascular conditions during the COVID-19 pandemic. J. Am. Coll. Cardiol. 2020, 76, 280–288. [Google Scholar] [CrossRef]
- Boeddinghaus, J.; Nestelberger, T.; Kaiser, C.; Twerenbold, R.; Fahrni, G.; Bingisser, R.; Khanna, N.; Tschudin-Sutter, S.; Widmer, A.; Jeger, R.; et al. Effect of COVID-19 on acute treatment of ST-segment elevation and non-ST-segment elevation acute coronary syndrome in Northwestern Switzerland. Int. J. Cardiol. Heart Vasc. 2021, 32, 100686. [Google Scholar] [CrossRef]
- Bollmann, A.; Hohenstein, S.; König, S.; Meier-Hellmann, A.; Kuhlen, R.; Hindricks, G. In-hospital mortality in heart failure in germany during the COVID-19 pandemic. ESC Heart Fail. 2020, 7, 4416–4419. [Google Scholar] [CrossRef]
- Bromage, D.I.; Cannatà, A.; Rind, I.A.; Gregorio, C.; Piper, S.; Shah, A.M.; McDonagh, T.A. The impact of COVID-19 on heart failure hospitalization and management: Report from a Heart Failure Unit in London during the peak of the pandemic. Eur. J. Heart Fail. 2020, 22, 978–984. [Google Scholar] [CrossRef]
- Bruoha, S.; Yosefy, C.; Gallego-Colon, E.; Rieck, J.; Orlov, Y.; Osherov, A.; Jihad, A.H.; Sherer, Y.; Viki, N.; Jafari, J. Impact in total ischemic time and ST-segment elevation myocardial infarction admissions during COVID-19. Am. J. Emerg. Med. 2021, 45, 7–10. [Google Scholar] [CrossRef]
- Bugger, H.; Gollmer, J.; Pregartner, G.; Wünsch, G.; Berghold, A.; Zirlik, A.; Von Lewinski, D. Complications and mortality of cardiovascular emergency admissions during COVID-19 associated restrictive measures. PLoS ONE 2020, 15, e0239801. [Google Scholar] [CrossRef]
- Butt, J.H.; Fosbøl, E.L.; Gerds, T.A.; Andersson, C.; Kragholm, K.; Biering-Sørensen, T.; Andersen, J.; Phelps, M.; Andersen, M.P.; Gislason, G.; et al. All-cause mortality and location of death in patients with established cardiovascular disease before, during, and after the COVID-19 lockdown: A Danish Nationwide Cohort Study. Eur. Heart J. 2021, 42, 1516–1523. [Google Scholar] [CrossRef]
- Claeys, M.J.; Argacha, J.; Collart, P.; Carlier, M.; Van Caenegem, O.; Sinnaeve, P.R.; Desmet, W.; Dubois, P.; Stammen, F.; Gevaert, S.; et al. Impact of COVID-19-related public containment measures on the ST elevation myocardial infarction epidemic in Belgium: A nationwide, serial, cross-sectional study. Acta Cardiol. 2020, 76, 863–869. [Google Scholar] [CrossRef]
- Colivicchi, F.; Di Fusco, S.A.; Magnanti, M.; Cipriani, M.; Imperoli, G. The impact of the coronavirus disease-2019 pandemic and Italian lockdown measures on clinical presentation and management of acute heart failure. J. Card. Fail. 2020, 26, 464–465. [Google Scholar] [CrossRef]
- De Filippo, O.; D’Ascenzo, F.; Angelini, F.; Bocchino, P.P.; Conrotto, F.; Saglietto, A.; Secco, G.G.; Campo, G.; Gallone, G.; Verardi, R.; et al. Reduced rate of hospital admissions for ACS during COVID-19 outbreak in Northern Italy. N. Engl. J. Med. 2020, 383, 88–89. [Google Scholar] [CrossRef]
- Doolub, G.; Wong, C.; Hewitson, L.; Mohamed, A.; Todd, F.; Gogola, L.; Skyrme-Jones, A.; Aziz, S.; Sammut, E.; Dastidar, A. Impact of COVID-19 on inpatient referral of acute heart failure: A single-centre experience from the South-West of the UK. ESC Heart Fail. 2021, 8, 1691–1695. [Google Scholar] [CrossRef]
- Erol, M.K.; Kayıkçıoğlu, M.; Kılıçkap, M.; Güler, A.; Yıldırım, A.; Kahraman, F.; Can, V.; Inci, S.; Baysal, S.S.; Er, O.; et al. Treatment delays and in-hospital outcomes in acute myocardial infarction during the COVID-19 pandemic: A nationwide study. Anatol. J. Cardiol. 2020, 24, 334–342. [Google Scholar]
- Fabris, E.; Bessi, R.; De Bellis, A.; Gregorio, C.; Peratoner, A.; Lardieri, G.; Cominotto, F.; Vitrella, G.; Rakar, S.; Perkan, A.; et al. COVID-19 impact on ST-elevation myocardial infarction incidence rate in a Italian STEMI network: A U-shaped curve phenomenon. J. Cardiovasc. Med. 2021, 22, 344–349. [Google Scholar] [CrossRef]
- Fersia, O.; Bryant, S.; Nicholson, R.; McMeeken, K.; Brown, C.; Donaldson, B.; Jardine, A.; Grierson, V.; Whalen, V.; Mackay, A. The impact of the COVID-19 pandemic on cardiology services. Open Heart 2020, 7, e001359. [Google Scholar] [CrossRef]
- Fileti, L.; Vecchio, S.; Moretti, C.; Reggi, A.; Aquilina, M.; Balducelli, M.; Santarelli, A.; Grosseto, D.; Piovaccari, G.; Rubboli, A. Impact of the COVID-19 pandemic on coronary invasive procedures at two Italian high-volume referral centers. J. Cardiovasc. Med. 2020, 21, 869–873. [Google Scholar] [CrossRef]
- Folino, A.F.; Zorzi, A.; Cernetti, C.; Marchese, D.; Pasquetto, G.; Roncon, L.; Saccà, S.; Themistoclakis, S.; Turiano, G.; Verlato, R.; et al. Impact of COVID-19 epidemic on coronary care unit accesses for acute coronary syndrome in Veneto region, Italy. Am. Heart J. 2020, 226, 26–28. [Google Scholar] [CrossRef]
- Gąsior, M.; Gierlotka, M.; Tycińska, A.; Wojtaszczyk, A.; Skrzypek, M.; Nadolny, K.; Ładny, J.R.; Dobrzycki, S.; Hausner, A.; Wita, K.; et al. Effects of the coronavirus disease 2019 pandemic on the number of hospitalizations for myocardial infarction: Regional differences. Population analysis of 7 million people. Kardiol. Pol. 2020, 78, 1039–1042. [Google Scholar] [CrossRef]
- Gitt, A.K.; Karcher, A.K.; Zahn, R.; Zeymer, U. Collateral damage of COVID-19-lockdown in Germany: Decline of NSTE-ACS admissions. Clin. Res. Cardiol. 2020, 109, 1585–1587. [Google Scholar] [CrossRef]
- Gluckman, T.J.; Wilson, M.A.; Chiu, S.; Penny, B.W.; Chepuri, V.B.; Waggoner, J.W.; Spinelli, K.J. Case rates, treatment approaches, and outcomes in acute myocardial infarction during the coronavirus disease 2019 pandemic. JAMA Cardiol. 2020, 5, 1419–1424. [Google Scholar] [CrossRef]
- Gramegna, M.; Baldetti, L.; Beneduce, A.; Pannone, L.; Falasconi, G.; Calvo, F.; Pazzanese, V.; Sacchi, S.; Pagnesi, M.; Moroni, F.; et al. ST-Segment–Elevation myocardial infarction during COVID-19 pandemic: Insights from a regional public service healthcare hub. Circ. Cardiovasc. Interv. 2020, 13, e009413. [Google Scholar] [CrossRef]
- Holy, E.W.; Jakob, P.; Manka, R.; Stähli, B.E.; Siegrist, P.T.; Ruschitzka, F.; Templin, C. Impact of a nationwide COVID-19 lockdown on acute coronary syndrome referrals. Cardiol. J. 2020, 27, 633–635. [Google Scholar] [CrossRef]
- Kapelios, C.J.; Siafarikas, C.; Bonou, M.; Liatis, S.; Barbetseas, J. The effect of the COVID-19 pandemic on acute coronary syndrome hospitalizations and out-of-hospital cardiac arrest in Greece. Public Health 2021, 191, 17–19. [Google Scholar] [CrossRef]
- Khalil, E.; Ozcan, S. Comparison of the number of cardiovascular admissions before and after COVID-19: Experience from Turkey. Acta Med. Mediterr. 2020, 36, 2433–2437. [Google Scholar]
- König, S.; Hohenstein, S.; Meier-Hellmann, A.; Kuhlen, R.; Hindricks, G.; Bollmann, A. In-hospital care in acute heart failure during the COVID-19 pandemic: Insights from the German-wide helios hospital network. Eur. J. Heart Fail. 2020, 22, 2190–2201. [Google Scholar] [CrossRef]
- König, S.; Ueberham, L.; Pellissier, V.; Hohenstein, S.; Meier-Hellmann, A.; Thiele, H.; Ahmadli, V.; Borger, M.A.; Kuhlen, R.; Hindricks, G.; et al. Hospitalization deficit of in-and outpatient cases with cardiovascular diseases and utilization of cardiological interventions during the COVID-19 pandemic: Insights from the German-wide helios hospital network. Clin. Cardiol. 2021, 44, 392–400. [Google Scholar] [CrossRef]
- Mafham, M.M.; Spata, E.; Goldacre, R.; Gair, D.; Curnow, P.; Bray, M.; Hollings, S.; Roebuck, C.; Gale, C.P.; Mamas, M.A.; et al. COVID-19 pandemic and admission rates for and management of acute coronary syndromes in England. Lancet 2020, 396, 381–389. [Google Scholar] [CrossRef]
- Mcilvennan, C.K.; Allen, L.A.; Devore, A.D.; Granger, C.B.; Kaltenbach, L.A.; Granger, B.B. Changes in care delivery for patients with heart failure during the COVID-19 pandemic: Results of a multicenter survey. J. Card. Fail. 2020, 26, 635–636. [Google Scholar] [CrossRef]
- Moreno, R.; Alonso, J.J.; Caballero, R.; del Corral, E.; Elízaga, J.; Asenjo, R.M.; Mena, M.J.; Alfonso, F.; Fernández-Ortiz, A.; Goicolea, F.J.; et al. Age and gender influence on time of arrival for STEMI patients during COVID-19 pandemic. Am. J. Emerg. Med. 2021, 42, 244–245. [Google Scholar] [CrossRef]
- Nef, H.M.; Elsässer, A.; Möllmann, H.; Abdel-Hadi, M.; Bauer, T.; Brück, M.; Eggebrecht, H.; Ehrlich, J.R.; Ferrari, M.W.; Fichtlscherer, S.; et al. Impact of the COVID-19 pandemic on cardiovascular mortality and catherization activity during the lockdown in central Germany: An observational study. Clin. Res. Cardiol. 2021, 110, 292–301. [Google Scholar] [CrossRef]
- Negreira Caamaño, M.; Piqueras Flores, J.; Mateo Gómez, C. Impact of COVID-19 pandemic in cardiology admissions. Med. Clin. 2020, 155, 179–180. [Google Scholar] [CrossRef]
- Papafaklis, M.I.; Katsouras, C.S.; Tsigkas, G.; Toutouzas, K.; Davlouros, P.; Hahalis, G.N.; Kousta, M.S.; Styliadis, I.G.; Triantafyllou, K.; Pappas, L.; et al. “Missing” acute coronary syndrome hospitalizations during the COVID-19 era in Greece: Medical care avoidance combined with a true reduction in incidence? Clin. Cardiol. 2020, 43, 1142–1149. [Google Scholar] [CrossRef]
- Pinto, R.D.; Ferri, C.; Mammarella, L.; Abballe, S.; Dell’Anna, S.; Cicogna, S.; Grassi, D.; Sacco, S.; Desideri, G. Increased cardiovascular death rates in a COVID-19 low prevalence area. J. Clin. Hypertens. 2020, 22, 1932–1935. [Google Scholar] [CrossRef]
- Primessnig, U.; Pieske, B.M.; Sherif, M. Increased mortality and worse cardiac outcome of acute myocardial infarction during the early COVID-19 pandemic. ESC Heart Fail. 2021, 8, 333–343. [Google Scholar] [CrossRef]
- Rattka, M.; Baumhardt, M.; Dreyhaupt, J.; Rothenbacher, D.; Thiessen, K.; Markovic, S.; Rottbauer, W.; Imhof, A. 31 days of COVID-19-cardiac events during restriction of public life-a comparative study. Clin. Res. Cardiol. 2020, 109, 1476–1482. [Google Scholar] [CrossRef]
- Reinstadler, S.J.; Reindl, M.; Lechner, I.; Holzknecht, M.; Tiller, C.; Roithinger, F.X.; Frick, M.; Hoppe, U.C.; Jirak, P.; Berger, R.; et al. Effect of the COVID-19 pandemic on treatment delays in patients with ST-segment elevation myocardial infarction. J. Clin. Med. 2020, 9, 2183. [Google Scholar] [CrossRef]
- Roffi, M.; Capodanno, D.; Windecker, S.; Baumbach, A.; Dudek, D. Impact of the COVID-19 pandemic on interventional cardiology practice: Results of the EAPCI survey. EuroIntervention 2020, 16, 247–250. [Google Scholar] [CrossRef]
- Schnaubelt, S.; Domanovits, H.; Niederdoeckl, J.; Schuetz, N.; Cacioppo, F.; Oppenauer, J.; Spiel, A.O.; Laggner, A.N. The impact of the COVID-19 pandemic on incidences of atrial fibrillation and electrical cardioversion at a tertiary care emergency department: An inter- and intra-year analysis. Front. Med. 2020, 7, 595881. [Google Scholar] [CrossRef]
- Secco, G.G.; Zocchi, C.; Parisi, R.; Roveta, A.; Mirabella, F.; Vercellino, M.; Pistis, G.; Reale, M.; Maggio, S.; Audo, A.; et al. Decrease and delay in hospitalization for acute coronary syndromes during the 2020 SARS-CoV-2 pandemic. Can. J. Cardiol. 2020, 36, 1152–1155. [Google Scholar] [CrossRef] [PubMed]
- Singh, S.; Fong, H.K.; Desai, R.; Zwinderman, A.H. Impact of COVID-19 on acute coronary syndrome-related hospitalizations: A pooled analysis. Int. J. Cardiol. Heart Vasc. 2021, 32, 100718. [Google Scholar] [CrossRef]
- Solomon, M.D.; McNulty, E.J.; Rana, J.S.; Leong, T.K.; Lee, C.; Sung, S.; Ambrosy, A.P.; Sidney, S.; Go, A.S. The COVID-19 pandemic and the incidence of acute myocardial infarction. N. Engl. J. Med. 2020, 383, 691–693. [Google Scholar] [CrossRef] [PubMed]
- Tomasoni, D.; Adamo, M.; Italia, L.; Branca, L.; Chizzola, G.; Fiorina, C.; Lupi, L.; Inciardi, R.M.; Cani, D.S.; Lombardi, C.M.; et al. Impact of COVID-2019 outbreak on prevalence, clinical presentation and outcomes of ST-elevation myocardial infarction. J. Cardiovasc. Med. 2020, 21, 874–881. [Google Scholar] [CrossRef] [PubMed]
- Vassilikos, V.P.; Pagourelias, E.D.; Katsos, K.; Zaggelidou, E.; Raikos, N.; Tzikas, S.; Tsavousoglou, C.; Kouparanis, A.; Anastasakis, A.; Papatheodorou, E.; et al. Impact of social containment measures on cardiovascular admissions and sudden cardiac death rates during Coronavirus Disease (COVID-19) outbreak in Greece. Hell. J. Cardiol. 2020, 62, 318–319. [Google Scholar] [CrossRef]
- Vecchio, S.; Fileti, L.; Reggi, A.; Moschini, C.; Lorenzetti, S.; Rubboli, A. Impact of the COVID-19 pandemic on admissions for acute coronary syndrome: Review of the literature and single-center experience. G Ital. Cardiol. 2020, 21, 502–508. [Google Scholar]
- Vest, A.R.; Upshaw, J.N.; Dean, K.; Donovan, E.; Diakos, N.; Hong, C.; Conway, L.; Kiernan, M.S.; DeNofrio, D.; Konstam, M.A. The Decrease in Hospitalizations for Heart Failure during the COVID-19 Pandemic: A Community and Academic Hospital Comparison Study. J. Card. Fail. 2020, 26, S71. [Google Scholar] [CrossRef]
- Wu, J.; Mamas, M.; Rashid, M.; Weston, C.; Hains, J.; Luescher, T.; de Belder, M.A.; Deanfield, J.E.; Gale, C.P. Patient response, treatments, and mortality for acute myocardial infarction during the COVID-19 pandemic. Eur. Heart J. Qual. Care Clin. Outcomes 2021, 7, 238–246. [Google Scholar] [CrossRef]
- Aldujeli, A.; Hamadeh, A.; Briedis, K.; Tecson, K.M.; Rutland, J.; Krivickas, Z.; Stiklioraitis, S.; Briede, K.; Aldujeili, M.; Unikas, R.; et al. Delays in presentation in patients with acute myocardial infarction during the COVID-19 pandemic. Cardiol. Res. 2020, 11, 386–391. [Google Scholar] [CrossRef]
- Hammad, T.A.; Parikh, M.; Tashtish, N.; Lowry, C.M.; Gorbey, D.; Forouzandeh, F.; Filby, S.J.; Wolf, W.M.; Costa, M.A.; Simon, D.I.; et al. Impact of COVID-19 pandemic on ST-elevation myocardial infarction in a non-COVID-19 epicenter. Catheter. Cardiovasc. Interv. 2021, 97, 208–214. [Google Scholar] [CrossRef]
- Kitahara, S.; Fujino, M.; Honda, S.; Asaumi, Y.; Kataoka, Y.; Otsuka, F.; Nakanishi, M.; Tahara, Y.; Ogata, S.; Onozuka, D.; et al. COVID-19 pandemic is associated with mechanical complications in patients with ST-elevation myocardial infarction. Open Heart 2021, 8, e001497. [Google Scholar] [CrossRef] [PubMed]
- Perrin, N.; Iglesias, J.F.; Rey, F.; Benzakour, L.; Cimci, M.; Noble, S.; Degrauwe, S.; Tessitore, E.; Mach, F.; Roffi, M. Impact of the COVID-19 pandemic on acute coronary syndromes. Swiss. Med. Wkly. 2020, 150, w20448. [Google Scholar] [CrossRef] [PubMed]
- Toner, L.; Koshy, A.N.; Hamilton, G.W.; Clark, D.; Farouque, O.; Yudi, M.B. Acute coronary syndromes undergoing percutaneous coronary intervention in the COVID-19 era: Comparable case volumes but delayed symptom onset to hospital presentation. Eur. Heart J. Qual. Care Clin. Outcomes 2020, 6, 225–226. [Google Scholar] [CrossRef] [PubMed]
- Wilson, S.J.; Connolly, M.J.; Elghamry, Z.; Cosgrove, C.; Firoozi, S.; Lim, P.; Sharma, R.; Spratt, J.C. Effect of the COVID-19 pandemic on ST-segment-elevation myocardial infarction presentations and in-hospital outcomes. Circ. Cardiovasc. Interv. 2020, 13, e009438. [Google Scholar] [CrossRef]
- Yong, C.M.; Ang, L.; Welt, F.G.P.; Gummidipundi, S.; Henry, T.D.; Pinto, D.S.; Cox, D.; Wang, P.; Asch, S.; Mahmud, E.; et al. Cardiac procedural deferral during the coronavirus (COVID-19) pandemic. Catheter. Cardiovasc. Interv. 2020, 96, 1080–1086. [Google Scholar] [CrossRef]
- Barbieri, L.; Tumminello, G.; Lucreziotti, S.; Gentile, D.; Centola, M.; Conconi, B.; Carlà, M.; Mafrici, A.; Carugo, S. Mortality in STEMI Patients during the COVID era: Has the pandemic changed our clinical practice? Cardiovasc. Revasc. Med. 2021, 22, 120–121. [Google Scholar] [CrossRef]
- Chen, Y.; Rathod, K.S.; Hamshere, S.; Choudry, F.; Akhtar, M.M.; Curtis, M.; Amersey, R.; Guttmann, O.; O’Mahony, C.; Jain, A.; et al. COVID-19 and changes in activity and treatment of ST elevation MI from a UK cardiac centre. Int. J. Cardiol. Heart Vasc. 2021, 33, 100736. [Google Scholar] [CrossRef]
- De Luca, G.; Cercek, M.; Jensen, L.O.; Vavlukis, M.; Calmac, L.; Johnson, T.; Ferrer, G.R.; Ganyukov, V.; Wojakowski, W.; Von Birgelen, C.; et al. Impact of COVID-19 pandemic and diabetes on mechanical reperfusion in patients with STEMI: Insights from the ISACS STEMI COVID 19 Registry. Cardiovasc. Diabetol. 2020, 19, 215. [Google Scholar] [CrossRef]
- Haddad, K.; Potter, B.J.; Matteau, A.; Gobeil, F.; Mansour, S. Implications of COVID-19 on Time-Sensitive STEMI Care: A Report from a North American epicenter. Cardiovasc. Revasc. Med. 2021, 30, 33–37. [Google Scholar] [CrossRef]
- Hannan, E.L.; Wu, Y.; Cozzens, K.; Friedrich, M.; Tamis-Holland, J.; Jacobs, A.K.; Ling, F.S.K.; King, S.B.; Venditti, F.J.; Walford, G.; et al. Percutaneous coronary intervention for ST-elevation myocardial infarction before and during COVID in New York. Am. J. Cardiol. 2021, 142, 25–34. [Google Scholar] [CrossRef]
- Hauguel-Moreau, M.; Pillière, R.; Prati, G.; Beaune, S.; Loeb, T.; Lannou, S.; Mallet, S.; Mustafic, H.; Bégué, C.; Dubourg, O.; et al. Impact of coronavirus disease 2019 outbreak on acute coronary syndrome admissions: Four weeks to reverse the trend. J. Thromb. Thrombolysis 2020, 51, 31–32. [Google Scholar] [CrossRef] [PubMed]
- Kobo, O.; Efraim, R.; Saada, M.; Kofman, N.; Abu Dogosh, A.; Abramowitz, Y.; Aronson, D.; Minha, S.; Roguin, A.; Meisel, S.R. The impact of lockdown enforcement during the SARSCoV-2 pandemic on the timing of presentation and early outcomes of patients with ST-elevation myocardial infarction. PLoS ONE 2020, 15, e0241149. [Google Scholar] [CrossRef] [PubMed]
- Kwok, C.S.; Gale, C.P.; Kinnaird, T.; Curzen, N.; Ludman, P.; Kontopantelis, E.; Wu, J.; Denwood, T.; Fazal, N.; Deanfield, J.; et al. Impact of COVID-19 on percutaneous coronary intervention for ST-elevation myocardial infarction. Heart 2020, 106, 1805–1811. [Google Scholar] [CrossRef] [PubMed]
- Little, C.D.; Kotecha, T.; Candilio, L.; Jabbour, R.J.; Collins, G.B.; Ahmed, A.; Connolly, M.; Kanyal, R.; Demir, O.M.; Lawson, L.O.; et al. COVID-19 pandemic and STEMI: Pathway activation and outcomes from the pan-London heart attack group. Open Heart 2020, 7, e001432. [Google Scholar] [CrossRef]
- Nader, J.; Anselmi, A.; Tomasi, J.; Martin, A.; Aymami, M.; Rouze, S.; Corbineau, H.; Langanay, T.; Flecher, E.; Nesseler, N.; et al. Adult cardiac surgery during COVID-19 lockdown: Impact on activity and outcomes in a high-volume centre. Arch. Cardiovasc. Dis. 2021, 114, 364–370. [Google Scholar] [CrossRef]
- Pascual Calleja, I.; Álvarez Velasco, R.; Almendarez Lacayo, M.; Arboine Aguirre, L.; Avanzas Fernández, P.; Moris de la Tassa, C. Impact of the COVID-19 pandemic on acute myocardial infarction care times. Emergencias 2020, 32, 440–442. [Google Scholar]
- Popovic, B.; Varlot, J.; Metzdorf, P.A.; Jeulin, H.; Goehringer, F.; Camenzind, E. Changes in characteristics and management among patients with ST-elevation myocardial infarction due to COVID-19 infection. Catheter. Cardiovasc. Interv. 2021, 97, E319–E326. [Google Scholar] [CrossRef]
- Rodríguez-Leor, O.; Cid-Álvarez, B.; De Prado, A.P.; Rossello, X.; Ojeda, S.; Serrador, A.; López-Palop, R.; Martín-Moreiras, J.; Rumoroso, J.R.; Cequier, Á.; et al. Impact of COVID-19 on ST-segment elevation myocardial infarction care. The Spanish experience. Rev. Esp. Cardiol. 2020, 73, 994–1002. [Google Scholar] [CrossRef]
- Scholz, K.H.; Lengenfelder, B.; Thilo, C.; Jeron, A.; Stefanow, S.; Janssens, U.; Bauersachs, J.; Schulze, P.C.; Winter, K.D.; Schröder, J.; et al. Impact of COVID-19 outbreak on regional STEMI care in Germany. Clin. Res. Cardiol. 2020, 109, 1511–1521. [Google Scholar] [CrossRef]
- Garcia, S.; Stanberry, L.; Schmidt, C.; Sharkey, S.; Megaly, M.; Albaghdadi, M.S.; Meraj, P.M.; Garberich, R.; Jaffer, F.A.; Stefanescu Schmidt, A.C.; et al. Impact of COVID-19 pandemic on STEMI care: An expanded analysis from the United States. Catheter. Cardiovasc. Interv. 2021, 98, 217–222. [Google Scholar] [CrossRef]
- Nappi, C.; Megna, R.; Acampa, W.; Assante, R.; Zampella, E.; Gaudieri, V.; Mannarino, T.; Green, R.; Cantoni, V.; Petretta, M.; et al. Effects of the COVID-19 pandemic on myocardial perfusion imaging for ischemic heart disease. Eur. J. Nucl. Med. Mol. Imaging 2020, 48, 421–427. [Google Scholar] [CrossRef] [PubMed]
- Quadri, G.; Rognoni, A.; Cerrato, E.; Baralis, G.; Boccuzzi, G.; Brscic, E.; Conrotto, F.; De Benedictis, M.; De Martino, L.; Di Leo, A.; et al. Catheterization laboratory activity before and during COVID-19 spread: A comparative analysis in Piedmont, Italy, by the Italian Society of Interventional Cardiology (GISE). Int. J. Cardiol. 2021, 323, 288–291. [Google Scholar] [CrossRef] [PubMed]
- Casey, L.; Khan, N.; Healy, D.G. The Impact of the COVID-19 pandemic on cardiac surgery and transplant services in Ireland’s National Centre. Ir. J. Med. Sci. 2020, 190, 13–17. [Google Scholar] [CrossRef] [PubMed]
- Elliott, J.M.; Crozier, I.G. Decreases in cardiac catheter laboratory workload during the COVID-19 level 4 lockdown in New Zealand. Intern. Med. J. 2020, 50, 1000–1003. [Google Scholar] [CrossRef]
- Iafrancesco, M.; Farina, P.; Bruno, P.; Pavone, N.; Mazza, A.; Cammertoni, F.; Nesta, M.; Chiariello, G.A.; Grandinetti, M.; Comerci, G.; et al. Impact of COVID-19 pandemia on provision of surgical treatment for patients with cardiovascular disease. Circulation 2020, 142, A15347. [Google Scholar] [CrossRef]
- Ishii, H.; Amano, T.; Yamaji, K.; Kohsaka, S.; Yokoi, H.; Ikari, Y. Implementation of Percutaneous coronary intervention during the COVID-19 pandemic in Japan—Nationwide survey report of the Japanese Association of Cardiovascular Intervention and Therapeutics for Cardiovascular Disease. Circ. J. 2020, 84, 2185–2189. [Google Scholar] [CrossRef]
- Kwok, C.S.; Gale, C.P.; Curzen, N.; de Belder, M.A.; Ludman, P.; Lüscher, T.F.; Kontopantelis, E.; Roebuck, C.; Denwood, T.; Burton, T.; et al. Impact of the COVID-19 pandemic on percutaneous coronary intervention in England: Insights from the British cardiovascular intervention society PCI database cohort. Circ. Cardiovasc. Interv. 2020, 13, e009654. [Google Scholar] [CrossRef]
- Mohamed, M.O.; Kinnaird, T.; Curzen, N.; Ludman, P.; Wu, J.; Rashid, M.; Shoaib, A.; De Belder, M.; Deanfield, J.; Gale, C.P.; et al. In-hospital and 30-day mortality after percutaneous coronary intervention in England in the pre-COVID and COVID eras. J. Invasive Cardiol. 2021, 33, E206–E219. [Google Scholar]
- Rodríguez-Caulo, E.A.; Carnero Alcázar, M.; Garrido Jiménez, J.M.; Barquero Aroca, J.M. National survey: Impact of COVID-19 on cardiovascular surgery services in Spain (SECCE-COVID19 Study). Cirugía Cardiovasc. 2021, 28, 67–70. [Google Scholar] [CrossRef]
- Soylu, K.; Coksevim, M.; Yanık, A.; Bugra Cerik, I.; Aksan, G. Effect of COVID-19 pandemic process on STEMI patients timeline. Int. J. Clin. Pract. 2021, 75, e14005. [Google Scholar] [CrossRef]
- Rebollal-Leal, F.; Aldama-López, G.; Flores-Ríos, X.; Piñón-Esteban, P.; Salgado-Fernández, J.; Calviño-Santos, R.; Vázquez-González, N.; Vázquez-Rodríguez, J.M. Impact of COVID-19 outbreak and public lockdown on ST-segment elevation myocardial infarction care in Spain. Cardiol. J. 2020, 27, 425–426. [Google Scholar] [CrossRef] [PubMed]
- Einstein, A.J.; Shaw, L.J.; Hirschfeld, C.; Williams, M.C.; Villines, T.C.; Better, N.; Vitola, J.V.; Cerci, R.; Dorbala, S.; Raggi, P.; et al. International impact of COVID-19 on the diagnosis of heart disease. J. Am. Coll. Cardiol. 2021, 77, 173–185. [Google Scholar] [CrossRef] [PubMed]
- Sankaranarayanan, R.; Hartshorne-Evans, N.; Redmond-Lyon, S.; Wilson, J.; Essa, H.; Gray, A.; Clayton, L.; Barton, C.; Ahmed, F.Z.; Cunnington, C.; et al. The Impact of COVID-19 on the management of heart failure: A United Kingdom patient questionnaire study. ESC Heart Fail. 2021, 8, 1324–1332. [Google Scholar] [CrossRef] [PubMed]
- Wosik, J.; Clowse, M.E.B.; Overton, R.; Adagarla, B.; Economou-Zavlanos, N.; Cavalier, J.; Henao, R.; Piccini, J.P.; Thomas, L.; Pencina, M.J.; et al. Impact of the COVID-19 pandemic on patterns of outpatient cardiovascular care. Am. Heart J. 2021, 231, 1–5. [Google Scholar] [CrossRef]
- Chagué, F.; Boulin, M.; Eicher, J.; Bichat, F.; Saint Jalmes, M.; Cransac-Miet, A.; Soudry-Faure, A.; Danchin, N.; Cottin, Y.; Zeller, M. Impact of lockdown on patients with congestive heart failure during the coronavirus disease 2019 pandemic. ESC Heart Fail. 2020, 7, 4420–4423. [Google Scholar] [CrossRef]
- Wadhera, R.K.; Shen, C.; Gondi, S.; Chen, S.; Kazi, D.S.; Yeh, R.W. Cardiovascular deaths during the COVID-19 pandemic in the United States. J. Am. Coll. Cardiol. 2021, 77, 159–169. [Google Scholar] [CrossRef]
- Czeisler, M.É. Delay or avoidance of medical care because of COVID-19–Related concerns–United States, June 2020. MMWR Morb. Mortal. Wkly. Rep. 2020, 69, 1250. [Google Scholar] [CrossRef]
- Al-Kindi, S.G.; Brook, R.D.; Biswal, S.; Rajagopalan, S. Environmental determinants of cardiovascular disease: Lessons learned from air pollution. Nat. Rev. Cardiol. 2020, 17, 656–672. [Google Scholar] [CrossRef]
- Venter, Z.S.; Aunan, K.; Chowdhury, S.; Lelieveld, J. COVID-19 lockdowns cause global air pollution declines. Proc. Natl. Acad. Sci. USA 2020, 117, 18984–18990. [Google Scholar] [CrossRef]
- Krumholz, H.M. Where Have All the Heart Attacks Gone? The New York Times. 6 April 2020. Available online: https://www.nytimes.com/2020/04/06/well/live/coronavirus-doctors-hospitals-emergency-care-heart-attack-stroke.html (accessed on 12 October 2021).
- Coronavirus Doctor’s Diary: Is Lockdown Good for Your Heart? BBC News. 5 May 2020. Available online: https://www.bbc.com/news/health-52535044 (accessed on 12 October 2021).
- Harky, A.; Harrington, D.; Nawaytou, O.; Othman, A.; Fowler, C.; Owens, G.; Torella, F.; Kuduvalli, M.; Field, M. COVID-19 and cardiac surgery: The perspective from United Kingdom. J. Card. Surg. 2020, 36, 1649–1658. [Google Scholar] [CrossRef]
- The European Society for Cardiology. ESC Guidance for the Diagnosis and Management of CV Disease during the COVID-19 Pandemic. 2020. Available online: https://academic.oup.com/eurheartj/advance-article/doi/10.1093/eurheartj/ehab697/6429145?login=false (accessed on 13 October 2021).
- Sofi, F.; Dinu, M.; Reboldi, G.; Stracci, F.; Pedretti, R.F.E.; Valente, S.; Gensini, G.; Gibson, C.M.; Ambrosio, G. Worldwide differences of hospitalization for ST-segment elevation myocardial infarction during COVID-19: A systematic review and meta-analysis. Int. J. Cardiol. 2022, 347, 89–96. [Google Scholar] [CrossRef] [PubMed]
- Chew, N.W.; Sia, C.H.; Wee, H.L.; Benedict, L.J.; Rastogi, S.; Kojodjojo, P.; Chor, W.P.D.; Leong, B.S.; Koh, B.C.; Tam, H.; et al. Impact of the COVID-19 pandemic on door-to-balloon time for primary percutaneous coronary intervention—Results from the Singapore Western STEMI network. Circ. J. 2021, 85, 139–149. [Google Scholar] [CrossRef] [PubMed]
- Cannatà, A.; Bromage, D.I.; McDonagh, T.A. The collateral cardiovascular damage of COVID-19: Only history will reveal the depth of the iceberg. Eur. Heart J. 2021, 42, 1524–1527. [Google Scholar] [CrossRef] [PubMed]
- HealthPros Network. 2021. Available online: https://www.healthpros-h2020.eu/index.php (accessed on 23 August 2021).
- Kringos, D.; Carinci, F.; Barbazza, E.; Bos, V.; Gilmore, K.; Groene, O.; Gulácsi, L.; Ivankovic, D.; Jansen, T.; Johnsen, S.P.; et al. Managing COVID-19 within and across health systems: Why we need performance intelligence to coordinate a global response. Health Res. Policy Syst. 2020, 18, 80. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
de Lange, M.; Carvalho, A.S.; Brito Fernandes, Ó.; Lingsma, H.; Klazinga, N.; Kringos, D. The Impact of the COVID-19 Pandemic on Hospital Services for Patients with Cardiac Diseases: A Scoping Review. Int. J. Environ. Res. Public Health 2022, 19, 3172. https://doi.org/10.3390/ijerph19063172
de Lange M, Carvalho AS, Brito Fernandes Ó, Lingsma H, Klazinga N, Kringos D. The Impact of the COVID-19 Pandemic on Hospital Services for Patients with Cardiac Diseases: A Scoping Review. International Journal of Environmental Research and Public Health. 2022; 19(6):3172. https://doi.org/10.3390/ijerph19063172
Chicago/Turabian Stylede Lange, Mats, Ana Sofia Carvalho, Óscar Brito Fernandes, Hester Lingsma, Niek Klazinga, and Dionne Kringos. 2022. "The Impact of the COVID-19 Pandemic on Hospital Services for Patients with Cardiac Diseases: A Scoping Review" International Journal of Environmental Research and Public Health 19, no. 6: 3172. https://doi.org/10.3390/ijerph19063172
APA Stylede Lange, M., Carvalho, A. S., Brito Fernandes, Ó., Lingsma, H., Klazinga, N., & Kringos, D. (2022). The Impact of the COVID-19 Pandemic on Hospital Services for Patients with Cardiac Diseases: A Scoping Review. International Journal of Environmental Research and Public Health, 19(6), 3172. https://doi.org/10.3390/ijerph19063172





