Prevalence of Obesity and Associated Risk Factors among Children and Adolescents in the Eastern Cape Province
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Setting
2.3. Population
2.4. Sampling Procedure
2.5. Data Collection
2.6. Data Analysis
2.7. Ethical and Legal Considerations
2.8. Validity and Reliability
3. Results
3.1. Demographic Charecteristics
3.2. Anthropometric Measurements
3.3. Physical Activity
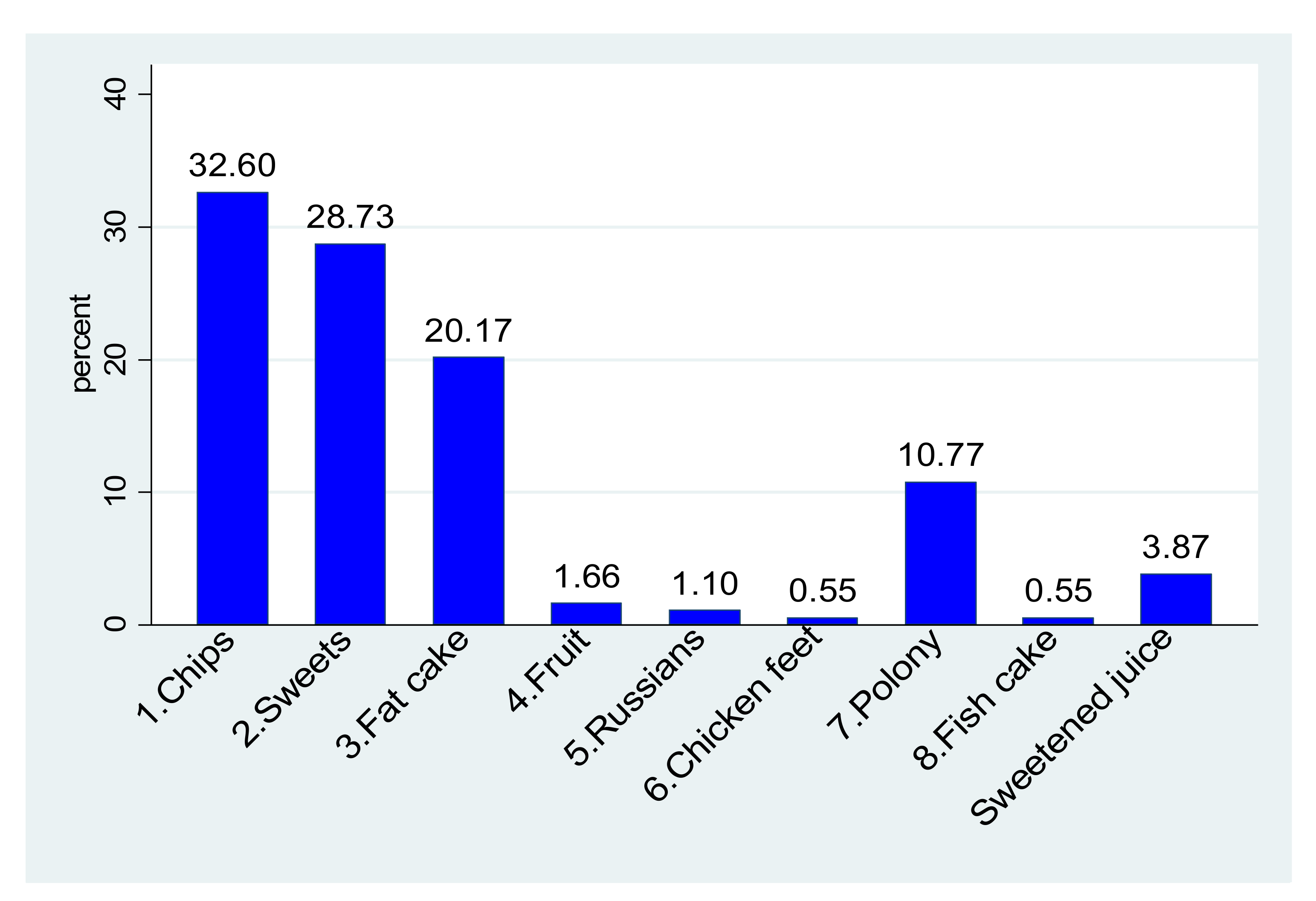
3.4. Dietary Habits of South African Rural Children
3.4.1. School Meals
3.4.2. After School Meal and Dinner
4. Discussion
5. Limitations
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Correction Statement
References
- Sahoo, K.; Sahoo, B.; Choudhury, A.K.; Sofi, N.Y.; Kumar, R.; Bhadoria, A.S. Childhood obesity: Causes and consequences. J. Fam. Med. Prim. Care 2015, 4, 187–192. [Google Scholar] [CrossRef]
- WHO. Obesity and Overweight. Available online: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight (accessed on 3 January 2022).
- NCD-RisC. Trends in adult body-mass index in 200 countries from 1975 to 2014: A pooled analysis of 1698 population-based measurement studies with 19·2 million participants. Lancet 2016, 387, 1377–1396. [Google Scholar] [CrossRef]
- Hernández-Cordero, S.; Cuevas-Nasu, L.; Morales-Ruán, M.d.C.; Humarán, I.M.-G.; Ávila-Arcos, M.A.; Rivera-Dommarco, J. Overweight and obesity in Mexican children and adolescents during the last 25 years. Nutr. Diabetes 2017, 7, e247. [Google Scholar] [CrossRef] [PubMed]
- Kovac, M.; Jurak, G.; Kragelj, L.Z.; Leskosek, B. The secular trend in the prevalence of overweight and obesity in the population of primary school children from Ljubljana (Slovenia). Zdr. Varst. 2014, 53, 188–198. [Google Scholar] [CrossRef]
- Xing, K.; Zhang, X.; Jiao, M.; Cui, Y.; Lu, Y.; Liu, J.; Zhang, J.; Zhao, Y.; Zhao, Y.; Li, Y. Concern about workplace violence and its risk factors in Chinese township hospitals: A cross-sectional study. Int. J. Environ. Res. Public Health 2016, 13, 811. [Google Scholar] [CrossRef]
- Liu, W.; Li, Q.; Li, H.; Li, J.; Wang, H.-J.; Li, B. 20-year trends in prevalence of overweight and obesity among children aged 0–6 in Harbin, China: A multiple cross-sectional study. PLoS ONE 2018, 13, e0198032. [Google Scholar] [CrossRef] [PubMed]
- Black, R.E.; Victora, C.G.; Walker, S.P.; Bhutta, Z.A.; Christian, P.; de Onis, M.; Ezzati, M.; Grantham-McGregor, S.; Katz, J.; Martorell, R.; et al. Maternal and child undernutrition and overweight in low-income and middle-income countries. Lancet 2013, 382, 427–451. [Google Scholar] [CrossRef]
- Pienaar, A.E. Prevalence of overweight and obesity among primary school children in a developing country: NW-CHILD longitudinal data of 6–9-yr-old children in South Africa. BMC Obes. 2015, 2, 2. [Google Scholar] [CrossRef] [PubMed]
- WHO. Preventing Chronic Diseases: A Vital Investment: WHO Global Report. Available online: https://apps.who.int/iris/handle/10665/43314 (accessed on 3 January 2022).
- Reddy, S.P.; Resnicow, K.; James, S.; Funani, I.N.; Kambaran, N.S.; Omardien, R.G.; Masuka, P.; Sewpaul, R.; Vaughan, R.D.; Mbewu, A. Rapid increases in overweight and obesity among South African adolescents: Comparison of data from the South African National Youth Risk Behaviour Survey in 2002 and 2008. Am. J. Public Health 2012, 102, 262–268. [Google Scholar] [CrossRef] [PubMed]
- Muthuri, S.K.; Francis, C.E.; Wachira, L.J.; Leblanc, A.G.; Sampson, M.; Onywera, V.O.; Tremblay, M.S. Evidence of an overweight/obesity transition among school-aged children and youth in Sub-Saharan Africa: A systematic review. PLoS ONE 2014, 9, e92846. [Google Scholar] [CrossRef]
- Bhurosy, T.; Jeewon, R. Overweight and obesity epidemic in developing countries: A problem with diet, physical activity, or socioeconomic status? Sci. World J. 2014, 2014, 964236. [Google Scholar] [CrossRef] [PubMed]
- Monsivais, P.; Drewnowski, A. Lower-energy-density diets are associated with higher monetary costs per kilocalorie and are consumed by women of higher socioeconomic status. J. Am. Diet. Assoc. 2009, 109, 814–822. [Google Scholar] [CrossRef]
- Hercberg, S.; Chat-Yung, S.; Chaulia, M. The French National Nutrition and Health Program: 2001–2006–2010. Int. J. Public Health 2008, 53, 68–77. [Google Scholar] [CrossRef] [PubMed]
- Girardet, J.P.; Rieu, D.; Bocquet, A.; Bresson, J.L.; Chouraqui, J.P.; Darmaun, D.; Dupont, C.; Frelut, M.L.; Ghisolfi, J.; Goulet, O.; et al. Childhood diet and cardiovascular risk factors. Arch. Pediatr 2010, 17, 51–59. [Google Scholar] [CrossRef]
- Hughes, A.R.; Sherriff, A.; Ness, A.R.; Reilly, J.J. Timing of adiposity rebound and adiposity in adolescence. Pediatrics 2014, 134, e1354–e1361. [Google Scholar] [CrossRef]
- Li, X.H.; Lin, S.; Guo, H.; Huang, Y.; Wu, L.; Zhang, Z.; Ma, J.; Wang, H.J. Effectiveness of a school-based physical activity intervention on obesity in school children: A nonrandomized controlled trial. BMC Public Health 2014, 14, 1282. [Google Scholar] [CrossRef]
- Ghesmaty Sangachin, M.; Cavuoto, L.A.; Wang, Y. Use of various obesity measurement and classification methods in occupational safety and health research: A systematic review of the literature. BMC Obes. 2018, 5, 28. [Google Scholar] [CrossRef] [PubMed]
- Yusuf, S.; Joseph, P.; Rangarajan, S.; Islam, S.; Mente, A.; Hystad, P.; Brauer, M.; Kutty, V.R.; Gupta, R.; Wielgosz, A.; et al. Modifiable risk factors, cardiovascular disease, and mortality in 155 722 individuals from 21 high-income, middle-income, and low-income countries (PURE): A prospective cohort study. Lancet 2020, 395, 795–808. [Google Scholar] [CrossRef]
- Stats, S. Statistics South Africa. Form. Census 2011, 78, 1–77. [Google Scholar]
- WHO. WHO Child Growth Standards: Length/Height-for-Age, Weight-for-Age, Weight-for-Length, Weight-for-Height and Body Mass Index-for-Age: Methods and Development. Available online: https://www.who.int/publications/i/item/924154693X (accessed on 3 January 2022).
- SAFOODS. SAMRC Food Quantitative Management South Africa. 2018. Available online: http://safoods.mrc.ac.za/database.html (accessed on 18 November 2017).
- Yusuf, S.; Hawken, S.; Ounpuu, S.; Bautista, L.; Franzosi, M.G.; Commerford, P.; Lang, C.C.; Rumboldt, Z.; Onen, C.L.; Lisheng, L.; et al. Obesity and the risk of myocardial infarction in 27,000 participants from 52 countries: A case-control study. Lancet 2005, 366, 1640–1649. [Google Scholar] [CrossRef]
- Shisana, O.; Labadarios, D.; Rehle, T.; Simbayi, L.; Zuma, K.; Dhansay, A.; Reddy, P.; Parker, W.; Hoosain, E.; Naidoo, P. The South African National Health and Nutrition Examination Survey, 2012: SANHANES-1: The Health and Nutritional Status of the Nation; HSRC Press: Cape Town, South Africa, 2014. [Google Scholar]
- Rockett, H.R.; Wolf, A.M.; Colditz, G.A. Development and reproducibility of a food frequency questionnaire to assess diets of older children and adolescents. J. Am. Diet. Assoc. 1995, 95, 336–340. [Google Scholar] [CrossRef]
- Galai, T.; Moran-Lev, H.; Cohen, S.; Ben-Tov, A.; Levy, D.; Weintraub, Y.; Amir, A.; Segev, O.; Yerushalmy-Feler, A. Higher prevalence of obesity among children with functional abdominal pain disorders. BMC Pediatr. 2020, 20, 193. [Google Scholar] [CrossRef] [PubMed]
- Manandhar, S.; Suksaroj, T.T.; Rattanapan, C. The Association between Green Space and the Prevalence of Overweight/Obesity among Primary School Children. Int. J. Occup. Environ. Med. 2019, 10, 1–10. [Google Scholar] [CrossRef]
- Sommer, I.; Teufer, B.; Szelag, M.; Nussbaumer-Streit, B.; Titscher, V.; Klerings, I.; Gartlehner, G. The performance of anthropometric tools to determine obesity: A systematic review and meta-analysis. Sci. Rep. 2020, 10, 12699. [Google Scholar] [CrossRef]
- Gažarová, M.; Galšneiderová, M.; Mečiarová, L. Obesity diagnosis and mortality risk based on a body shape index (ABSI) and other indices and anthropometric parameters in university students. Rocz Panstw Zakl Hig 2019, 70, 267–275. [Google Scholar] [CrossRef] [PubMed]
- Amirabdollahian, F.; Haghighatdoost, F. Anthropometric Indicators of Adiposity Related to Body Weight and Body Shape as Cardiometabolic Risk Predictors in British Young Adults: Superiority of Waist-to-Height Ratio. J. Obes. 2018, 2018, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Miyawaki, A.; Evans, C.E.L.; Lucas, P.J.; Kobayashi, Y. Relationships between social spending and childhood obesity in OECD countries: An ecological study. BMJ Open 2021, 11, e044205. [Google Scholar] [CrossRef]
- Liu, D.; Mason, A.; Marks, L.; Davis, H.; Hunter, D.J.; Jehu, L.M.; Smithson, J.; Visram, S. Effects of local authority expenditure on childhood obesity. Eur. J. Public Health 2018, 29, 785–790. [Google Scholar] [CrossRef]
- Li, M.; Xue, H.; Jia, P.; Zhao, Y.; Wang, Z.; Xu, F.; Wang, Y. Pocket money, eating behaviors, and weight status among Chinese children: The Childhood Obesity Study in China mega-cities. Prev. Med. 2017, 100, 208–215. [Google Scholar] [CrossRef] [PubMed]
- Grammatikopoulou, M.; Galli-Tsinopoulou, A.; Daskalou, E.; Tsigga, M.; Stylianou, C.; Kokka, P.; Emmanouilidou, E. IS POCKET-MONEY AN INDICANT OF DIETARY INTAKE AND OBESITY? Arch. Dis. Child. 2008, 93, 2. [Google Scholar]
- Ma, L.; Fang, Z.; Gao, L.; Zhao, Y.; Xue, H.; Li, K.; Wang, Y. A 3-year Longitudinal Study of Pocket Money, Eating Behavior, Weight Status: The Childhood Obesity Study in China Mega-Cities. Int. J. Environ. Res. Public Health 2020, 17, 9139. [Google Scholar] [CrossRef] [PubMed]
- Arluk, S.L.; Branch, J.D.; Swain, D.P.; Dowling, E.A. Childhood obesity’s relationship to time spent in sedentary behavior. Mil. Med. 2003, 168, 583–586. [Google Scholar] [CrossRef] [PubMed]
- Robinson, T.N.; Banda, J.A.; Hale, L.; Lu, A.S.; Fleming-Milici, F.; Calvert, S.L.; Wartella, E. Screen Media Exposure and Obesity in Children and Adolescents. Pediatrics 2017, 140 (Suppl. S2), S97–S101. [Google Scholar] [CrossRef] [PubMed]
- Pacific, R.; Kulwa, K.; Martin, H.D.; Petrucka, P. Physical activity and sedentary behaviors associated with overweight and obesity among primary school children in Tanzania: A case-control study. Nutr. Food Sci. 2021. [Google Scholar] [CrossRef]
- Sheldrick, M.P.R.; Tyler, R.; Mackintosh, K.A.; Stratton, G. Relationship between Sedentary Time, Physical Activity and Multiple Lifestyle Factors in Children. J. Funct. Morphol. Kinesiol. 2018, 3, 15. [Google Scholar] [CrossRef]
- Lubbad, T. Food consumption patterns and dietary habits associated with weight status in healthy young adult students. Masters’ Thesis, Al Azhar University Gaza, Gaza, Palestinian, 2011. [Google Scholar]
- Kesztyüs, D.; Traub, M.; Lauer, R.; Kesztyüs, T.; Steinacker, J.M. Skipping breakfast is detrimental for primary school children: Cross-sectional analysis of determinants for targeted prevention. BMC Public Health 2017, 17, 258. [Google Scholar] [CrossRef]
- Fiuza, R.F.D.P.; Muraro, A.P.; Rodrigues, P.R.M.; Sena, E.d.M.S.; Ferreira, M.G. Skipping breakfast and associated factors among Brazilian adolescents. Rev. De Nutr. 2017, 30, 615–626. [Google Scholar] [CrossRef]
- Cook, S.; Kavey, R.E. Dyslipidemia and pediatric obesity. Pediatr. Clin. North Am. 2011, 58, 1363–1373, ix. [Google Scholar] [CrossRef] [PubMed]
- Papoutsou, S.; Briassoulis, G.; Wolters, M.; Peplies, J.; Iacoviello, L.; Eiben, G.; Veidebaum, T.; Molnar, D.; Russo, P.; Michels, N.; et al. No breakfast at home: Association with cardiovascular disease risk factors in childhood. Eur. J. Clin. Nutr 2014, 68, 829–834. [Google Scholar] [CrossRef] [PubMed]
- Ward, Z.J.; Long, M.W.; Resch, S.C.; Giles, C.M.; Cradock, A.L.; Gortmaker, S.L. Simulation of Growth Trajectories of Childhood Obesity into Adulthood. N. Engl. J. Med. 2017, 377, 2145–2153. [Google Scholar] [CrossRef]
- O’Neil, C.E.; Byrd-Bredbenner, C.; Hayes, D.; Jana, L.; Klinger, S.E.; Stephenson-Martin, S. The role of breakfast in health: Definition and criteria for a quality breakfast. J. Acad. Nutr. Diet. 2014, 114, S8–S26. [Google Scholar] [CrossRef] [PubMed]
- Hong, I.; Coker-Bolt, P.; Anderson, K.R.; Lee, D.; Velozo, C.A. Relationship Between Physical Activity and Overweight and Obesity in Children: Findings From the 2012 National Health and Nutrition Examination Survey National Youth Fitness Survey. Am. J. Occup. Ther. Cup 2016, 70, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Wyszyńska, J.; Ring-Dimitriou, S.; Thivel, D.; Weghuber, D.; Hadjipanayis, A.; Grossman, Z.; Ross-Russell, R.; Dereń, K.; Mazur, A. Physical Activity in the Prevention of Childhood Obesity: The Position of the European Childhood Obesity Group and the European Academy of Pediatrics. Front. Pediatrics 2020, 8, 662. [Google Scholar] [CrossRef] [PubMed]
- Al-Nuaim, A.A.; Al-Nakeeb, Y.; Lyons, M.; Al-Hazzaa, H.M.; Nevill, A.; Collins, P.; Duncan, M.J. The Prevalence of Physical Activity and Sedentary Behaviours Relative to Obesity among Adolescents from Al-Ahsa, Saudi Arabia: Rural versus Urban Variations. J. Nutr. Metab. 2012, 2012, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Liu, M.; Cao, B.; Liu, M.; Liang, X.; Wu, D.; Li, W.; Su, C.; Chen, J.; Gong, C. High Prevalence of Obesity but Low Physical Activity in Children Aged 9-11 Years in Beijing. Diabetes, Metab. Syndr. Obesity: Targets Ther. 2021, 14, 3323–3335. [Google Scholar] [CrossRef]
- Vandewater, E.A.; Park, S.E.; Hébert, E.T.; Cummings, H.M. g.gs, H.M. Time with friends and physical activity as mechanisms linking obesity and television viewing among youth. Int. J. Behav. Nutr. Phys. Act. 2015, 12 (Suppl. S1), S6. [Google Scholar] [CrossRef]
- Bell, S.K.; Morgan, S.B. Children’s attitudes and behavioral intentions toward a peer presented as obese: Does a medical explanation for the obesity make a difference? J. Pediatr. Psychol. 2000, 25, 137–145. [Google Scholar] [CrossRef]
- Sigelman, C.K. The effect of causal information on peer perceptions of children with physical problems. J. Appl. Dev. Psychol. 1991, 12, 237–253. [Google Scholar] [CrossRef]
- Zeller, M.H.; Reiter-Purtill, J.; Ramey, C. Negative peer perceptions of obese children in the classroom environment. Obesity 2008, 16, 755–762. [Google Scholar] [CrossRef] [PubMed]
- Altman, M.; Wilfley, D.E. Evidence update on the treatment of overweight and obesity in children and adolescents. J. Clin. Child Adolesc. Psychol 2015, 44, 521–537. [Google Scholar] [CrossRef] [PubMed]
- Sampasa-Kanyinga, H.; Hamilton, H.A. Eating breakfast regularly is related to higher school connectedness and academic performance in Canadian middle- and high-school students. Public Health 2017, 145, 120–123. [Google Scholar] [CrossRef] [PubMed]
- Van den Berg, V.L.; Seheri, L.; Raubenheimer, J. Body mass index of 16-year olds in urban Maseru, Lesotho. Afr. J. Prim. Health Care Fam. Med. 2014, 6, E1–E14. [Google Scholar] [CrossRef] [PubMed]
- Nortje, N.; Faber, M.; de Villiers, A. School tuck shops in South Africa—an ethical appraisal. South. Afr. J. Clin. Nutr. 2017, 30, 74–79. [Google Scholar] [CrossRef]
- Govender, P. Ban Junk Food and Fizzy Drinks from Schools. Available online: https://www.timeslive.co.za/news/south-africa/2019-12-20-ban-junk-food-and-fizzy-drinks-from-schools/ (accessed on 4 January 2022).
- Melmer, A.; Kempf, P.; Laimer, M. The Role of Physical Exercise in Obesity and Diabetes. Praxis 2018, 107, 971–976. [Google Scholar] [CrossRef] [PubMed]
- Metcalf, B.S.; Hosking, J.; Jeffery, A.N.; Voss, L.D.; Henley, W.; Wilkin, T.J. Fatness leads to inactivity, but inactivity does not lead to fatness: A longitudinal study in children (EarlyBird 45). Arch. Dis. Child. 2011, 96, 942–947. [Google Scholar] [CrossRef] [PubMed]
| Demographic Characteristics (n = 209) | Overweight or Obese | Normal | Underweight | p-Value | |||
|---|---|---|---|---|---|---|---|
| Weight status; n (%) | 28 | (13.4) | 148 | (70.8) | 33 | (15.8) | - |
| Age, years; med (IQR **) | 13.95 | (4.1) | 12.2 | (4.4) | 13.0 | (3) | 0.081 ♣ |
| Sex; n (%) | |||||||
| Males | 9 | (32.1) | 65 | (43.9) | 19 | (57.6) | 0.138 |
| Females | 19 | (67.9) | 83 | (56.1) | 14 | (42.4) | |
| Age, years; n (%) | |||||||
| ≤11 | 7 | (25.0) | 64 | (43.2) | 10 | (30.3) | 0.089 |
| 12–15 | 13 | (46.4) | 53 | (35.8) | 19 | (57.6) | |
| >15 | 8 | (28.6) | 31 | (21.0) | 4 | (12.1) | |
| Current grade at school; n (%) | |||||||
| None | 0 | (0.0) | 3 | (2.0) | 0 | (0.0) | 0.085 * |
| Primary school | 15 | (53.6) | 102 | (68.9) | 28 | (84.9) | |
| High school | 13 | (46.4) | 43 | (29.1) | 5 | (15.2) | |
| ~ Mode used to get to school; n (%) | |||||||
| Walk | 21 | (75.0) | 118 | (80.8) | 30 | (90.9) | 0.216 |
| Public, private or school transport | 7 | (25.0) | 28 | (19.2) | 3 | (9.1) | |
| Average walking time to school, minutes; med (IQR) | 20 | (15) | 20 | (20) | 15 | (20) | 0.171 ♣ |
| ^ Participation in sports; n (%) | |||||||
| Yes | 22 | (78.6) | 134 | (91.1) | 30 | (90.9) | 0.153 |
| No | 6 | (21.4) | 13 | (8.8) | 3 | (9.1) | |
| $ Where most sport takes place; n (%) | |||||||
| School | 9 | (40.9) | 69 | (52.3) | 11 | (35.5) | 0.171 |
| Home | 5 | (22.7) | 15 | (11.4) | 8 | (25.8) | |
| School and home | 8 | (36.4) | 48 | (36.4) | 12 | (38.7) | |
| $ Specific sport; n (%) | |||||||
| Soccer | 7 | (33.3) | 72 | (43.9) | 17 | (54.8) | 0.074 ** |
| Netball | 7 | (33.3) | 27 | (16.5) | 5 | (16.1) | |
| Cricket | 0 | (0.0) | 12 | (9.0) | 1 | (3.2) | |
| Rugby | 1 | (4.8) | 0 | (0.00) | 0 | (0.0) | |
| Hoopla hoops | 0 | (0.0) | 0 | (0.0) | 1 | (3.2) | |
| Other | 6 | (28.6) | 44 | (33.1) | 7 | (22.6) | |
| # Frequency of sport; n (%) | |||||||
| Daily | 7 | (31.8) | 60 | (46.9) | 17 | (60.7) | 0.092 * |
| Weekly | 11 | (50.0) | 34 | (26.6) | 4 | (14.3) | |
| Occasionally | 4 | (18.2) | 34 | (26.6) | 7 | (25.0) | |
| Play sport after school; n (%) | |||||||
| Yes | 17 | (60.7) | 98 | (66.2) | 22 | (66.7) | 0.563 |
| No | 11 | (39.3) | 50 | (33.8) | 11 | (33.3) | |
| Watch TV after school; n (%) | |||||||
| Yes | 21 | (75.0) | 75 | (50.7) | 15 | (45.5) | 0.013 |
| No | 7 | (25.0) | 73 | (49.3) | 18 | (54.5) | |
| Play TV or Video games; n (%) | |||||||
| Yes | 2 | (7.1) | 4 | (2.7) | 0 | (0.0) | 0.185 * |
| No | 26 | (92.9) | 144 | (97.3) | 33 | (100.0) | |
| Sleep; n (%) | |||||||
| Yes | 0 | (0.0) | 2 | (1.4) | 1 | (3.0) | 1.00 * |
| No | 28 | (100.0) | 146 | (98.6) | 32 | (97.0) | |
| House chores; n (%) | |||||||
| Yes | 23 | (82.1) | 114 | (75.7) | 23 | (69.7) | 0.453 |
| No | 5 | (17.9) | 34 | (24.3) | 10 | (30.3) | |
| Traditional games; n (%) | |||||||
| Yes | 9 | (32.1) | 40 | (27.0) | 11 | (33.3) | 0.666 |
| No | 19 | (67.9) | 108 | (73.0) | 22 | (66.7) | |
| ~ Taking breakfast; n (%) | 0.299 | ||||||
| Yes | 18 | (66.7) | 111 | (75.5) | 25 | (78.1) | |
| No | 9 | (33.3) | 36 | (24.5) | 7 | (21.9) | |
| ~ Breakfast; n (%) | |||||||
| Cornflakes | 6 | (22.2) | 28 | (19.1) | 3 | (9.4) | 0.698 |
| Weet-bix/wheat-base | 2 | (7.4) | 11 | (7.5) | 1 | (3.1) | |
| Sifted maize | 9 | (33.3) | 65 | (44.2) | 17 | (53.1) | |
| Previous day’s food | 1 | (3.7) | 7 | (4.8) | 4 | (12.5) | |
| None | 9 | (33.3) | 36 | (24.5) | 7 | (21.9) | |
| ¥ Bring own lunch to school; n (%) | |||||||
| Yes | 6 | (21.4) | 33 | (22.6) | 6 | (18.2) | 1.000 |
| No | 22 | (78.6) | 113 | (77.4) | 27 | (81.8) | |
| ^ Lunch core starch; n (%) | |||||||
| Maize based | 26 | (92.9) | 129 | (87.8) | 30 | (90.9) | 0.342 |
| None | 1 | (3.6) | 15 | (10.2) | 3 | (9.1) | |
| Both | 1 | (3.6) | 3 | (2.0) | 0 | (0.0) | |
| Starch dinner; n (%) | |||||||
| Maize based | 21 | (75.0) | 108 | (73.0) | 23 | (69.7) | 0.142 * |
| Rice | 6 | (21.4) | 40 | (27.0) | 10 | (30.3) | |
| None | 1 | (3.6) | 0 | (0.0) | 0 | (0.0) | |
| Caregiver employment status; n (%) | |||||||
| Yes | 2 | (7.1) | 11 | (7.4) | 2 | (6.1) | 1.000 * |
| No | 26 | (92.9) | 137 | (92.6) | 31 | (93.9) | |
| Caregiver income source; n (%) | |||||||
| None | 4 | (14.23) | 22 | (14.9) | 3 | (9.1) | 0.979 * |
| Disability grant | 3 | (10.7) | 5 | (4.4) | 3 | (9.1) | |
| Old age grant | 8 | (28.6) | 43 | (29.1) | 11 | (33.3) | |
| Child support grant | 8 | (28.6) | 45 | (30.4) | 8 | (24.2) | |
| Support from spouse | 2 | (7.1) | 12 | (6.8) | 2 | (6.1) | |
| Support from parent | 0 | (0.0) | 3 | (2.0) | 0 | (0.0) | |
| Support from other children | 1 | (3.6) | 5 | (3.4) | 2 | (6.1) | |
| Vending | 0 | (0.0) | 0 | (0.0) | 1 | (3.0) | |
| Pension or retirement | 0 | (0.0) | 3 | (2.0) | 0 | (0.0) | |
| Foster care grant | 0 | (0.0) | 1 | (0.7) | 1 | (3.0) | |
| Employment | 2 | (7.1) | 11 | (7.4) | 2 | (6.1) | |
| ^ Pocket money to school; n (%) | |||||||
| Yes | 26 | (92.9) | 122 | (83.0) | 30 | (90.9) | 0.560 |
| No | 2 | (7.1) | 25 | (17.0) | 3 | (9.1) | |
| Characteristics (n = 209) | Male | Female | p-Value | ||
|---|---|---|---|---|---|
| n = 93 | n = 116 | ||||
| MUAC; n (%) | |||||
| Obese | 0 | (0.0) | 3 | (2.6) | 0.256 * |
| Not obese | 93 | (100.0) | 113 | (97.4) | |
| Waist circumference, cm #; med (IQR **) | 62 | (10) | 63 | (13) | 0.677 |
| ~ Waist circumference; n (%) | |||||
| Obese | 0 | (0.0) | 3 | (2.7) | 0.253 |
| Not obese | 93 | (100.0) | 110 | (97.4) | |
| Triceps skinfold, cm #; med (IQR **) | 8 | (4) | 11 | (7) | <0.0001 |
| Triceps skinfold; n (%) | |||||
| Obese | 3 | (3.2) | 8 | (6.9) | 0.352 |
| Not obese | 90 | (96.8) | 108 | (93.1) | |
| BMI, kg/m2; med (IQR **) | 17.42 | (3.9) | 18.41 | (4.6) | 0.088 |
| BMI; n (%) | |||||
| Obese | 1 | (1.1) | 4 | (3.5) | 0.221 |
| Overweight | 8 | (8.6) | 15 | (12.9) | |
| Not obese | 65 | (69.9) | 83 | (71.6) | |
| Malnourished | 19 | (20.4) | 14 | (12.1) | |
| Anthropometric Measure | Agreement (%) | Kappa | p-Value |
|---|---|---|---|
| BMI | 100 | 1 | 1 |
| Waist Circumference | 87.9 | 0.1718 | <0.0001 |
| Triceps Skinfold | 90.0 | 0.4175 | <0.0001 |
| MUAC | 88.0 | 0.1720 | <0.0001 |
| Type of Food | n (%) | |
|---|---|---|
| Carbohydrates | Maize | 186 (88.6) |
| Maize and rice | 4 (1.9) | |
| Bread | Brown bread | 22 (10.5) |
| White bread | 22 (10.5) | |
| Vegetables | Beans/legumes | 176 (83.8) |
| Potatoes | 44 (21.0) | |
| Cabbage | 147 (70) | |
| Carrots | 102 (48.6) | |
| Beetroot | 64 (30.5) | |
| Spinach | 8 (3.8) | |
| Mixed vegetables | 2 (1.0) | |
| None | 23 (11.0) | |
| Fruit | Apple | 112 (53.3) |
| Orange | 3 (1.4) | |
| Plum | 1 (0.5) | |
| None | 93 (44.3) | |
| Meat | Red meat | 5 (2.4) |
| Chicken/pork | 49 (23.3) | |
| Processed meat (sausage/vienna/polony) | 16 (7.6) | |
| Eggs/Fish | 45 (21.4) | |
| Soup | 72 (34.3) | |
| Dairy products | Fermented milk (Amasi) | 11 (5.2) |
| Usual drink at school | Water | 172 (81.9) |
| Fruit juice | 11 (5.2) | |
| Sweetened juice | 20 (9.5) | |
| Fizzy drink | 1 (0.5) | |
| Other forms of beverages | 1 (0.48; 0.07–3.4) | |
| None | 5 (2.38; 0.99–5.6) |
| Type of Food | n (%) | |
|---|---|---|
| Carbohydrates | Maize | 89 (42.4) |
| Rice | 73 (34.8) | |
| Maize and rice | 1 (0.5) | |
| Bread | Brown bread | 83 (39.5) |
| White bread | 43 (20.5) | |
| Vegetables | Beans/legumes | 38 (18.1) |
| Potatoes | 48 (22.9) | |
| Cabbage | 51 (24.3) | |
| Carrots | 14 (6.7) | |
| Beetroot | 2 (1.0) | |
| Spinach | 17 (8.1) | |
| Mixed vegetables | 3 (1.4) | |
| None | 96 (45.7) | |
| Fruit | Apple | 1 (0.5) |
| Banana | 1 (0.5) | |
| None | 208 (99.1) | |
| Meat | Red meat | 3 (1.4) |
| Chicken/pork | 62 (29.5) | |
| Processed meat (sausage/vienna/polony) | 17 (8.1) | |
| Eggs/Fish | 21 (10) | |
| Soup | 67 (31.9) | |
| Dairy products | Fermented milk (Amasi) | 4 (1.9) |
| Types of Food | n (%) | |
|---|---|---|
| Carbohydrates | Maize | 153 (72.9) |
| Rice | 56 (26.7) | |
| Bread | Brown bread | 8 (3.9) |
| White bread | 39 (18.6) | |
| Vegetables | Beans/legumes | 87 (41.4) |
| Potatoes | 81 (38.6) | |
| Cabbage | 111 (52.9) | |
| Carrots | 33 (15.7) | |
| Beetroot | 3 (1.4) | |
| Spinach | 22 (10.5) | |
| Mixed vegetables | 13 (6.2) | |
| None | 26 (12.4) | |
| Fruit | Apple | 1 (0.5) |
| Banana | 1 (0.5) | |
| None | 208 (99.1) | |
| Meat | Red meat | 13 (6.2) |
| Chicken/pork | 133 (63.3) | |
| Eggs/Fish | 12 (5.7) | |
| Soup | 35 (16.7) | |
| Dairy products | Fermented milk (Amasi) | 15 (7.1) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nomatshila, S.C.; Mabunda, S.A.; Puoane, T.; Apalata, T.R. Prevalence of Obesity and Associated Risk Factors among Children and Adolescents in the Eastern Cape Province. Int. J. Environ. Res. Public Health 2022, 19, 2946. https://doi.org/10.3390/ijerph19052946
Nomatshila SC, Mabunda SA, Puoane T, Apalata TR. Prevalence of Obesity and Associated Risk Factors among Children and Adolescents in the Eastern Cape Province. International Journal of Environmental Research and Public Health. 2022; 19(5):2946. https://doi.org/10.3390/ijerph19052946
Chicago/Turabian StyleNomatshila, Sibusiso Cyprian, Sikhumbuzo A. Mabunda, Thandi Puoane, and Teke R. Apalata. 2022. "Prevalence of Obesity and Associated Risk Factors among Children and Adolescents in the Eastern Cape Province" International Journal of Environmental Research and Public Health 19, no. 5: 2946. https://doi.org/10.3390/ijerph19052946
APA StyleNomatshila, S. C., Mabunda, S. A., Puoane, T., & Apalata, T. R. (2022). Prevalence of Obesity and Associated Risk Factors among Children and Adolescents in the Eastern Cape Province. International Journal of Environmental Research and Public Health, 19(5), 2946. https://doi.org/10.3390/ijerph19052946






