Analysis of the Calls Received during the COVID-19 Lockdown by the Mental Health Crisis Helpline Operated by the Professional College of Psychology of Aragon
Abstract
:1. Introduction
2. Materials and Methods
2.1. Implementation of the Mental Health Crisis Helpline for the Public
2.2. Population
2.3. Intervention
2.4. Winding-Down of the Service
2.5. Data Collection
- Call date
- Caller gender
- Caller age group
- Main reason
- Relevant free text in relation to the call, which was coded as other reasons or other relevant information
- Response given
2.6. Data Analysis
3. Results
3.1. Reasons for the Calls
3.2. Variable Dependency Analysis
3.3. Correlations
4. Discussion
Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- González-Sanguino, C.; Ausín, B.; Castellanos, M.Á.; Saiz, J.; López-Gómez, A.; Ugidos, C.; Muñoz, M. Mental Health Consequences of the Coronavirus 2020 Pandemic (COVID-19) in Spain. A Longitudinal Study. Front. Psychiatry 2020, 11, 565474. [Google Scholar] [CrossRef] [PubMed]
- Health Alert and Centro de Coordinación de Alertas y Emergencias Sanitarias. Actualización no 89. Enfermedad por el COVID-19. 28 April 2020. Madrid. Available online: https://www.mscbs.gob.es/profesionales/saludPublica/ccayes/alertasActual/nCov/documentos/Actualizacion_89_COVID-19.pdf (accessed on 2 May 2020).
- Bo, H.-X.; Li, W.; Yang, Y.; Wang, Y.; Zhang, Q.; Cheung, T.; Wu, X.; Xiang, Y.-T. Posttraumatic Stress Symptoms and Attitude toward Crisis Mental Health Services among Clinically Stable Patients with COVID-19 in China. Psychol. Med. 2021, 51, 1052–1053. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhang, J.; Lu, H.; Zeng, H.; Zhang, S.; Du, Q.; Jiang, T.; Du, B. The differential psychological distress of populations affected by the COVID-19 pandemic. Brain Behav. Immun. 2020, 87, 49–50. [Google Scholar] [CrossRef] [PubMed]
- Fernández-Aranda, F.; Casas, M.; Claes, L.; Bryan, D.C.; Favaro, A.; Granero, R.; Gudiol, C.; Jiménez-Murcia, S.; Karwautz, A.; Le Grange, D.; et al. COVID-19 and implications for eating disorders. Eur. Eat. Disord. Rev. 2020, 28, 239–245. [Google Scholar] [CrossRef]
- Zhou, J.; Liu, L.; Xue, P.; Yang, X.; Tang, X. Mental health response to the COVID-19 outbreak in China. Am. J. Psychiatry 2020, 177, 574–575. [Google Scholar] [CrossRef]
- Cai, W.; Lian, B.; Song, X.; Hou, T.; Deng, G.; Li, H. A cross-sectional study on mental health among health care workers during the outbreak of Corona Virus Disease 2019. Asian J. Psychiatr. 2020, 51, 102111. [Google Scholar] [CrossRef]
- Chen, Y.; Zhou, H.; Zhou, Y.; Zhou, F. Prevalence of self-reported depression and anxiety among pediatric medical staff members during the COVID-19 outbreak in Guiyang, China. Psychiatry Res. 2020, 288, 113005. [Google Scholar] [CrossRef]
- Huang, Y.; Zhao, N. Chinese mental health burden during the COVID-19 pandemic. Asian J. Psychiatr. 2020, 51, 102052. [Google Scholar] [CrossRef]
- Liang, Y.; Chen, M.; Zheng, X.; Liu, J. Screening for Chinese medical staff mental health by SDS and SAS during the outbreak of COVID-19. J. Psychosom. Res. 2020, 133, 110102. [Google Scholar] [CrossRef]
- Lu, W.; Wang, H.; Lin, Y.; Li, L. Psychological status of medical workforce during the COVID-19 pandemic: A cross-sectional study. Psychiatry Res. 2020, 288, 112936. [Google Scholar] [CrossRef]
- Mo, Y.; Deng, L.; Zhang, L.; Lang, Q.; Liao, C.; Wang, N.; Qin, M.; Huang, H. Work stress among Chinese nurses to support Wuhan for fighting against the COVID-19 epidemic. J. Nurs. Manag. 2020, 28, 1002–1009. [Google Scholar] [CrossRef] [Green Version]
- Xiao, H.; Zhang, Y.; Kong, D.; Li, S.; Yang, N. The effects of social support on sleep quality of medical staff treating patients with Coronavirus Disease 2019 (COVID-19) in January and February 2020 in China. Med. Sci. Monit. 2020, 26, e923549. [Google Scholar] [CrossRef]
- Xu, J.; Xu, Q.-H.; Wang, C.-M.; Wang, J. Psychological status of surgical staff during the COVID-19 outbreak. Psychiatry Res. 2020, 288, 112955. [Google Scholar] [CrossRef]
- Zhang, W.R.; Wang, K.; Yin, L.; Zhao, W.F.; Xue, Q.; Peng, M.; Min, B.Q.; Tian, Q.; Leng, H.X.; Du, J.L.; et al. Mental health and psychosocial problems of medical health workers during the COVID-19 epidemic in China. Psychother. Psychosom. 2020, 89, 1–9. [Google Scholar] [CrossRef]
- Li, S.; Wang, Y.; Xue, J.; Zhao, N.; Zhu, T. The impact of COVID-19 epidemic declaration on psychological consequences: A study on active Weibo users. Int. J. Environ. Res. Public Health 2020, 17, 2032. [Google Scholar] [CrossRef] [Green Version]
- Sonderskov, K.M.; Dinesen, P.T.; Santini, Z.I.; Ostergaard, S.D. The depressive state of Denmark during the COVID-19 pandemic. Acta Neuropsychiatr. 2020, 32, 226–228. [Google Scholar] [CrossRef] [Green Version]
- Wang, C.; Pan, R.; Wan, X.; Tan, Y.; Xu, L.; McIntyre, R.S.; Faith, N.C.; Bach, T.; Roger, H.; Vijai, K.S.; et al. A longitudinal study on the mental health of general population during the COVID-19 epidemic in China. Brain. Behav. Immun. 2020, 87, 40–48. [Google Scholar] [CrossRef]
- Yuan, R.; Xu, Q.H.; Xia, C.C.; Lou, C.Y.; Xie, Z.; Ge, Q.M.; Shao, Y. Psychological status of parents of hospitalized children during the COVID-19 epidemic in China. Psychiatry Res. 2020, 288, 112953. [Google Scholar] [CrossRef]
- González-Sanguino, C.; Ausín, B.; ÁngelCastellanos, M.; Saiz, J.; López-Gómez, A.; Ugidos, C.; Muñoz, M. Mental Health Consequences during the Initial Stage of the 2020 Coronavirus Pandemic (COVID-19) in Spain. Brain Behav. Immun. 2020, 87, 172–176. [Google Scholar] [CrossRef]
- Vindegaard, N.; Benros, M.E. COVID-19 pandemic and mental health consequences: Systematic review of the current evidence. Brain Behav. Immun. 2020, 89, 531–542. [Google Scholar] [CrossRef]
- Liu, J.; Zhu, Q.; Fan, W.; Makamure, J.; Zheng, C.; Wang, J. Online Mental Health Survey in a Medical College in China During the COVID-19 Outbreak. Front. Psychiatry 2020, 11, 459. [Google Scholar] [CrossRef] [PubMed]
- Zhu, J.; Sun, L.; Zhang, L.; Wang, H.; Fan, A.; Yang, B.; Li, W.; Xiao, S. Prevalence and Influencing Factors of Anxiety and Depression Symptoms in the First-Line Medical Staff Fighting Against COVID-19 in Gansu. Front. Psychiatry 2020, 11, 386. [Google Scholar] [CrossRef] [PubMed]
- Pappa, S.; Ntella, V.; Giannakas, T.; Giannakoulis, V.G.; Papoutsi, E.; Katsaounou, P. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: A systematic review and meta-analysis. Brain Behav. Immun. 2020, 88, 901–907. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.; Pan, R.; Wan, X.; Tan, Y.; Xu, L.; Ho, C.S.; Ho, R.C. Immediate Psychological Responses and Associated Factors during the Initial Stage of the 2019 Coronavirus Disease (COVID-19) Epidemic among the General Population in China. Int. J. Environ. Res. Public Health 2020, 17, 1729. [Google Scholar] [CrossRef] [Green Version]
- Zhang, C.; Yang, L.; Liu, S.; Ma, S.; Wang, Y.; Cai, Z.; Du, H.; Li, R.; Kang, L.; Su, M.; et al. Survey of Insomnia and Related Social Psychological Factors Among Medical Staff Involved in the 2019 Novel Coronavirus Disease Outbreak. Front. Psychiatry 2020, 11, 306. [Google Scholar] [CrossRef] [Green Version]
- Defensor del Pueblo. El defensor del Pueblo Recomienda al Gobierno y las CCAA Incrementar la Asistencia Psicológica en el Sistema Nacional de Salud. 2020. Available online: https://www.defensordelpueblo.es/noticias/salud-mental/ (accessed on 25 September 2020).
- Zhou, X.; Snoswell, C.L.; Harding, L.E.; Bambling, M.; Edirippulige, S.; Bai, X.; Smith, A.C. The role of telehealth in reducing the mental health burden from COVID-19. Telemed. J. E-Health 2020, 26, 377–379. [Google Scholar] [CrossRef] [Green Version]
- Wang, J.; Wei, H.; Zhou, L. Hotline services in China during COVID-19 pandemic. J. Affect. Disord. 2020, 275, 125–126. [Google Scholar] [CrossRef]
- Combs, D.C. Mental health interventions by telephone with Katrina survivors. J. Health Care Poor Underserved 2007, 18, 271–276. [Google Scholar] [CrossRef]
- Leung, T.; Wong, H. Community reactions to the SARS crisis in Hong Kong: Analysis of a time-limited counseling hotline. J. Hum. Behav. Soc. Environ. 2005, 12, 1–22. [Google Scholar] [CrossRef]
- Ussery, W.; Waters, J. COP2COP hotlines: Programs to address the needs of first responders and their families. Brief Treat. Crisis Interv. 2020, 6, 66–78. [Google Scholar] [CrossRef]
- Wunsch-Hitzig, R.; Plapinger, J.; Draper, J.; del Campo, E. Calls for help after September 11: A community mental health hot line. J. Urban Health 2002, 79, 417–428. [Google Scholar] [CrossRef] [Green Version]
- National Health Commission of China. Guidelines for Psychological Assistance Hotlines during 2019-nCoV Pneumonia Epidemic. Available online: http://www.nhc.gov.cn/jkj/s3577/202002/f389f20cc1174b21b981ea2919beb8b0.shtml (accessed on 16 September 2020).
- Ribeiro, E.; Sampaio, A.; Gonçalves, M.; Taveira, M.; Cunha, J.; Maia, A.; Matos, M.; Gonçalves, S.; Figueiredo, B.; Freire, T.; et al. Telephone-based psychological crisis intervention: The Portuguese experience with COVID-19. Couns. Psychol. Q. 2020, 34, 432–446. [Google Scholar] [CrossRef]
- Berdullas Saunders, S.; Gesteira Santos, C.; Morán Rodríguez, C.; Fernández Hermida, J.R.; Santolaya, F.; Sanz Fernández, J.; García-Vera, M.P. El teléfono de asistencia psicológica por la COVID-19 del Ministerio de Sanidad y del Consejo General de la Psicología de España: Características y demanda. Rev. Esp. Salud Pública 2020, 94, e202010138. [Google Scholar]
- Grupo de Intervención Psicológica en Situaciones de Emergencias, Desastres y Catástrofes -GIPEC- NAVARRA. Atención Psicológica Telefónica COVID-19. 2020. Available online: http://www.colpsinavarra.org/sites/default/files/imagenes/atencion-psicologica-covid.pdf (accessed on 3 April 2020).
- IBM Corp. IBM SPSS Statistics for Windows; IBM Corp: Armonk, NY, USA, 2017; Available online: https://hadoop.apache.org (accessed on 13 September 2020).
- Colegio Oficial de la Psicología de Castilla-La Mancha. COPCLM: Escuchando a las Personas en la COVID-19. Atención Psicológica Inmediata, Prevención para el Futuro. 2020. Available online: http://www.cop.es/uploads/PDF/CASTILLA-LA-MANCHA-MEMORIA-TELEFONO-COVID19.pdf (accessed on 13 September 2020).
- Geoffroy, P.A.; Le Goanvic, V.; Sabbagh, O.; Richoux, C.; Weinstein, A.; Dufayet, G.; Lejoyeux, M. Psychological Support System for Hospital Workers during the Covid-19 Outbreak: Rapid Design and Implementation of the Covid-Psy Hotline. Front. Psychiatry 2020, 11, 511. [Google Scholar] [CrossRef]
- Rodríguez-Rey, R.; Garrido-Hernansaiz, H.; Collado, S. Psychological impact of COVID-19 in Spain: Early data report. Psychol. Trauma Theory Res. Pract. Policy 2020, 12, 550–552. [Google Scholar] [CrossRef]
- Usman, M.; Fahy, S. Coping with the COVID-19 crisis: An overview of service adaptation and challenges encountered by a rural Psychiatry of Later Life (POLL) team. Ir. J. Psychol Med. 2020, 38, 1–5. [Google Scholar] [CrossRef]
- Li, W.T.; Yang, G.Y.; Tong, J.; Li, Y.; Liu, L.Z.; Liu, C.L. Trend Analysis of Calls of Wuhan “Xinxinyu” Psychological Hotline from February 4 to February 24 in 2020. Psychol. Commun. 2020, 3, 24–27. [Google Scholar]
- Brülhart, M.; Klotzbücher, V.; Lalive, R.; Reich, S.K. Mental health concerns during the COVID-19 pandemic as revealed by helpline calls. Nature 2021, 600, 121–126. [Google Scholar] [CrossRef]
- Mahase, E. COVID-19: EU states report 60% rise in emergency calls about domestic violence. BMJ 2020, 369, m1872. [Google Scholar] [CrossRef]
- Lebel, U.; Dana, M. Life Scripts, Counter Scripts and Online Videos: The Struggle of Religious-Nationalist Community Epistemic Authorities against Military Service for Women. Religions 2021, 12, 750. [Google Scholar] [CrossRef]

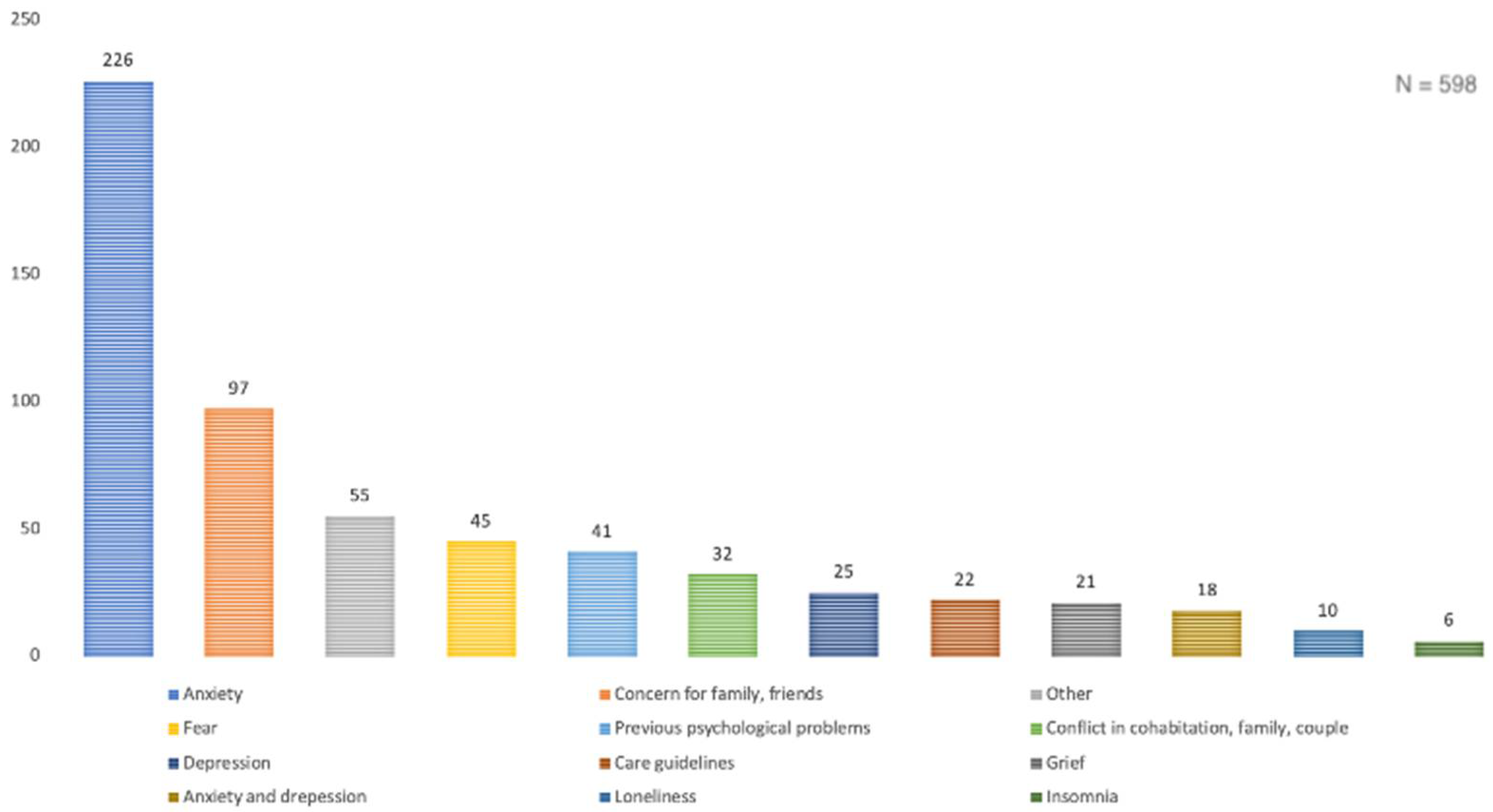
| Main Reasons (%) | General Reasons (%) | |
|---|---|---|
| Anxiety symptomatology | 38% | 52.4% |
| Concern for family, friends | 16% | 20.1% |
| Other | 9% | - |
| Fear | 8% | 16.4% |
| Prior condition | 7% | 11.7% |
| Conflicts in cohabitation, family, relationship | 5% | 18.5% |
| Depressive symptomatology | 4% | 23.1% |
| Bereavement | 4% | 5.1% |
| Care guidelines | 4% | 4.7% |
| Anxiety and depression symptomatology | 3% | - |
| Loneliness | 2% | 6.6% |
| Insomnia | 1% | 5.6% |
| Chronic physical condition | - | 2.7% |
| Correlation between Variables | Females | Males | p-Value | Chi-Squared |
|---|---|---|---|---|
| Bereavement | 6.2% | 2% | 0.039 | 4.25 |
| Conflicts | 20.3% | 13.7% | 0.071 | 3.25 |
| Prior psychological conditions | 12% | 11.1% | 0.767 | 0.09 |
| Chronic physical condition | 3.5% | 0.7% | 0.049 | 3.36 |
| Anxiety symptomatology | 49.5% | 60.8% | 0.017 | 5.74 |
| Depression symptomatology | 22.4% | 24.8% | 0.530 | 0.40 |
| Concern for a family member/friend | 22.7% | 12.4% | 0.006 | 7.48 |
| Care-giving guidelines | 6% | 1.3% | 0.020 | 5.42 |
| Loneliness | 6.4% | 7.2% | 0.743 | 0.11 |
| Fear | 14.7% | 20.9% | 0.072 | 3.23 |
| Insomnia | 4.8% | 7.2% | 0.265 | 1.24 |
| Correlation between Variables | Children and Youths | Adults | Older People | p-Value | Chi-Squared |
|---|---|---|---|---|---|
| Anxiety symptomatology | 50% | 54.9% | 42.9% | 0.071 | 5.25 |
| Insomnia | 16.7% | 4.6% | 7.1% | 0.069 | 5.26 |
| Correlation between Variables | p-Value | r |
|---|---|---|
| Gender | 0.574 | −0.023 |
| Age | p < 0.001 | 0.155 |
| Bereavement | 0.242 | 0.049 |
| Conflicts | p < 0.001 | 0.147 |
| Prior psychological conditions | 0.035 | −0.087 |
| Physical illness | 0.183 | −0.055 |
| Anxiety symptomatology | 0.005 | −0.117 |
| Depression symptomatology | 0.936 | 0.003 |
| Concern for a family member/friend | 0.084 | −0.071 |
| Care-giving guidelines | 0.113 | 0.066 |
| Loneliness | 0.349 | −0.039 |
| Fear | 0.169 | 0.057 |
| Insomnia | 0.972 | 0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Monreal-Bartolomé, A.; López-Del-Hoyo, Y.; Cabrera-Gil, I.; Aguilar-Latorre, A.; Puebla-Guedea, M.; Boira, S.; Lanero, J. Analysis of the Calls Received during the COVID-19 Lockdown by the Mental Health Crisis Helpline Operated by the Professional College of Psychology of Aragon. Int. J. Environ. Res. Public Health 2022, 19, 2901. https://doi.org/10.3390/ijerph19052901
Monreal-Bartolomé A, López-Del-Hoyo Y, Cabrera-Gil I, Aguilar-Latorre A, Puebla-Guedea M, Boira S, Lanero J. Analysis of the Calls Received during the COVID-19 Lockdown by the Mental Health Crisis Helpline Operated by the Professional College of Psychology of Aragon. International Journal of Environmental Research and Public Health. 2022; 19(5):2901. https://doi.org/10.3390/ijerph19052901
Chicago/Turabian StyleMonreal-Bartolomé, Alicia, Yolanda López-Del-Hoyo, Itxaso Cabrera-Gil, Alejandra Aguilar-Latorre, Marta Puebla-Guedea, Santiago Boira, and Jesús Lanero. 2022. "Analysis of the Calls Received during the COVID-19 Lockdown by the Mental Health Crisis Helpline Operated by the Professional College of Psychology of Aragon" International Journal of Environmental Research and Public Health 19, no. 5: 2901. https://doi.org/10.3390/ijerph19052901
APA StyleMonreal-Bartolomé, A., López-Del-Hoyo, Y., Cabrera-Gil, I., Aguilar-Latorre, A., Puebla-Guedea, M., Boira, S., & Lanero, J. (2022). Analysis of the Calls Received during the COVID-19 Lockdown by the Mental Health Crisis Helpline Operated by the Professional College of Psychology of Aragon. International Journal of Environmental Research and Public Health, 19(5), 2901. https://doi.org/10.3390/ijerph19052901








