Effectiveness of Interventions to Promote Medication Adherence in Schizophrenic Populations in Thailand: A Systematic Review
Abstract
:1. Introduction
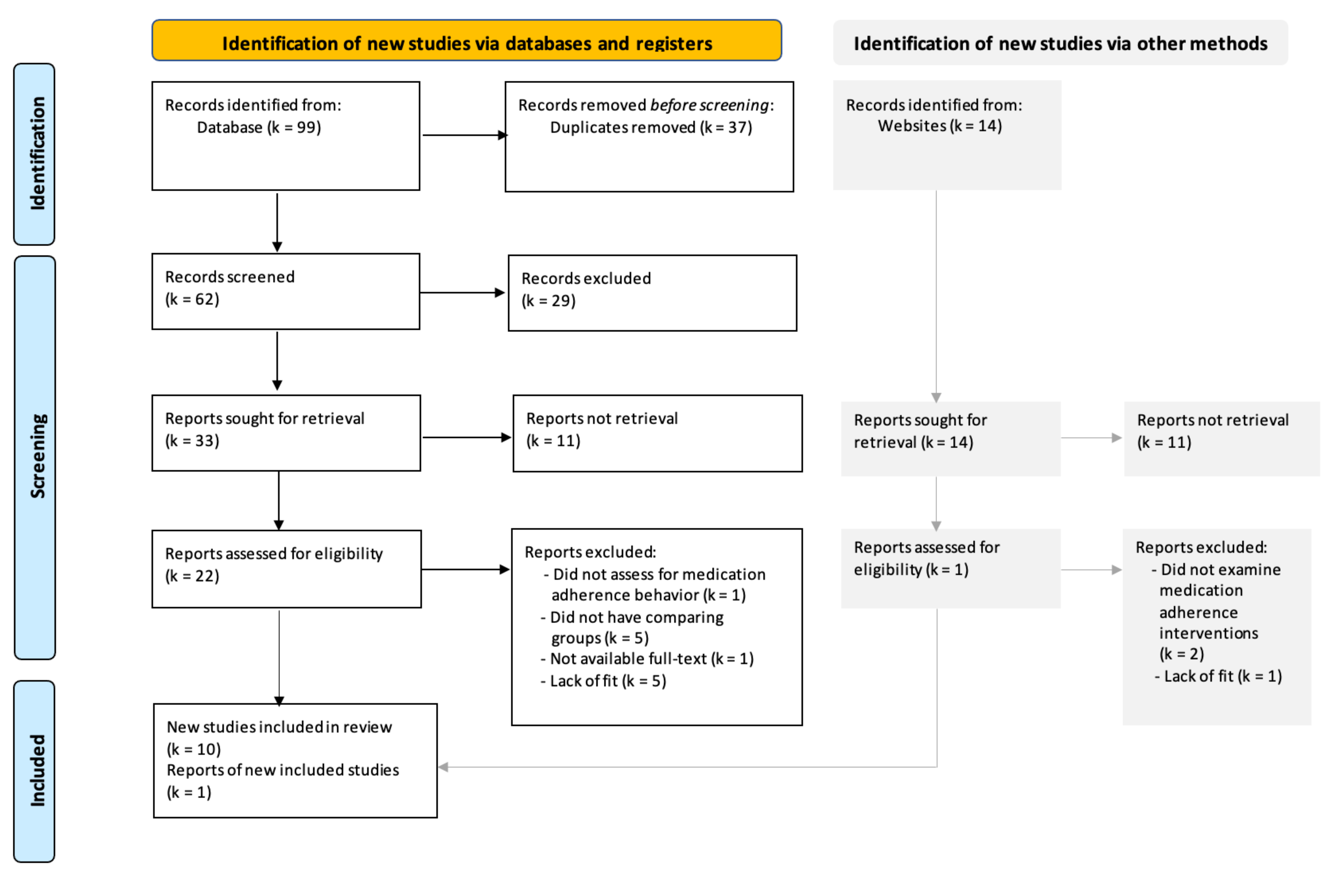
2. Materials and Methods
2.1. Design
2.2. Search Methods for Identification of Studies
2.3. Eligibility Criteria
2.4. Data Analysis
2.5. Quality Appraisal
3. Results
3.1. Quality Appraisal
3.2. Sample Population
3.3. Treatment Settings and Initiation
3.4. Intervention Approaches
3.5. Control Conditions
3.6. Treatment Completion and Retention
3.7. Primary and Secondary Outcomes
3.8. Measurement of Medication or Treatment Adherence
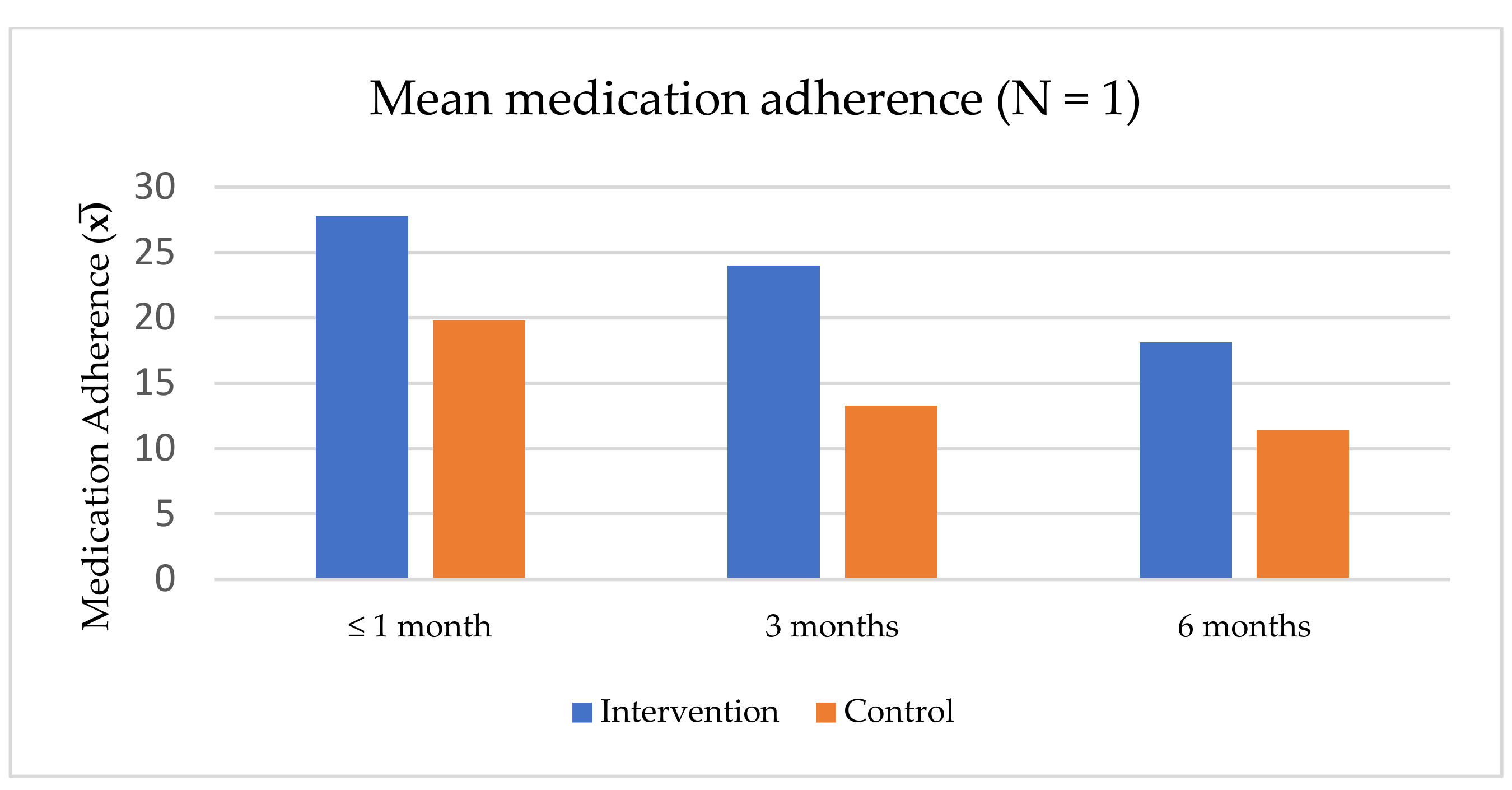
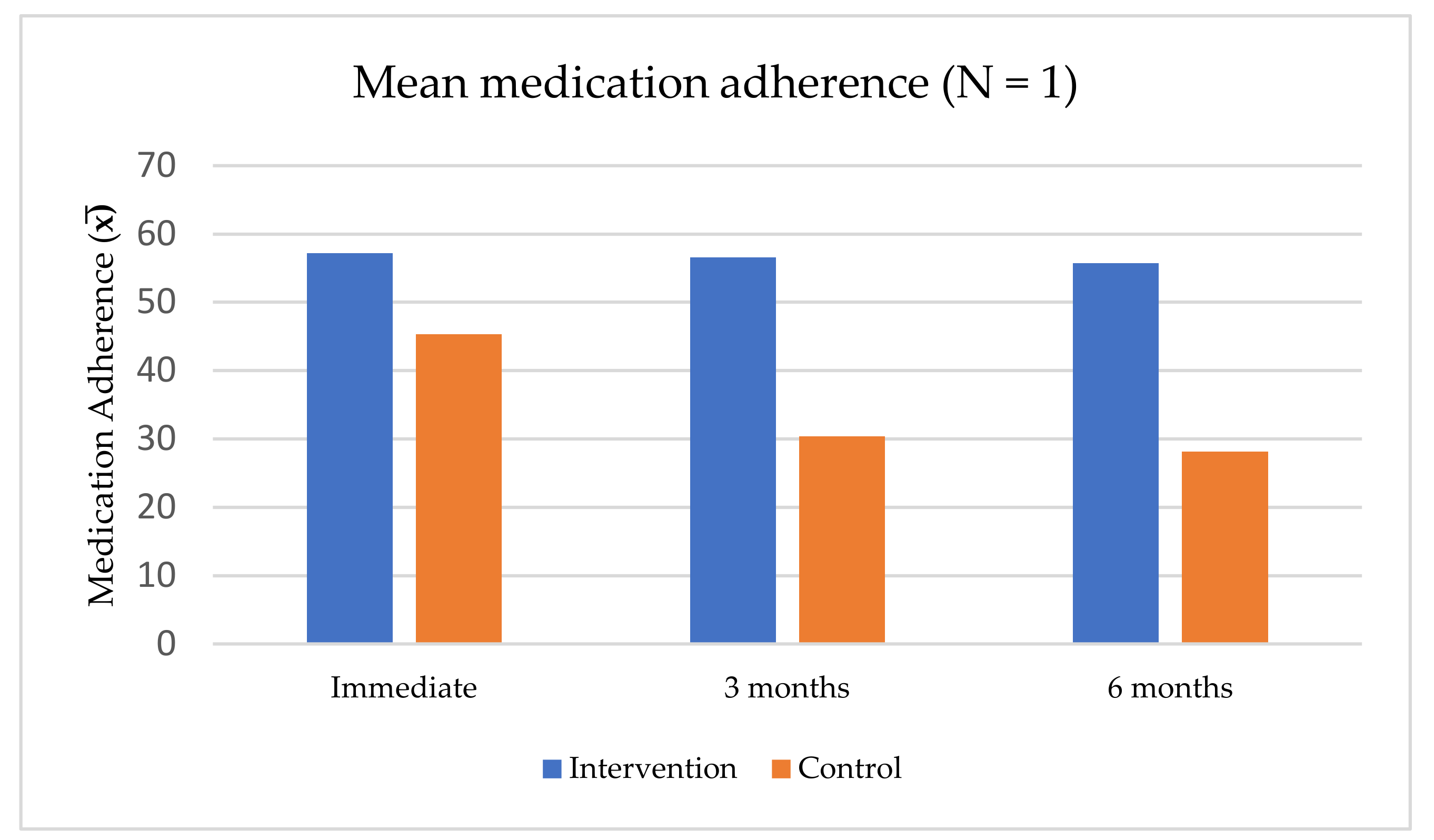
3.9. Effectiveness of Medication Adherence Interventions
4. Discussion
4.1. Implications for Future Research and Nursing Practice
4.2. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Mental Health, Poverty and Development. 2009. Available online: https://www.who.int/nmh/publications/discussion_paper_en.pdf?ua=1 (accessed on 27 June 2021).
- Ritchie, H.; Roser, M.; Mental Health. Published Online at OurWorldInData.org. 2018. Available online: https://ourworldindata.org/mental-health’ (accessed on 27 June 2021).
- Kittirattanapaiboon, P.; Kongsuk, T.; Pengjuntr, W.; Leejongpermpoon, J.; Chutha, W.; Kenbubpha, K. Epidemiology of psychiatric comorbidity in Thailand: A national study. J. Ment. Health 2008, 21, 1–14. (In Thai). Available online: https://he01.tci-thaijo.org/index.php/jmht/article/view/10142 (accessed on 15 May 2021).
- Department of Mental Health, Thailand. Report of Patients Receiving Psychiatric Services. 2018. Available online: https://www.dmh.go.th/report/datacenter/hdc/ (accessed on 15 May 2021).
- Phanthunane, P.; Vos, T.; Whiteford, H.; Bertram, M.; Udomratn, P. Schizophrenia in Thailand: Prevalence and burden of disease. Popul. Health Metr. 2010, 8, 24. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chaudhury, P.K.; Deka, K.; Chetia, D. Disability associated with mental disorders. Indian J. Psychiatry 2006, 48, 95–101. [Google Scholar] [CrossRef] [PubMed]
- Mental Disorders. Available online: https://www.who.int/news-room/fact-sheets/detail/mental-disorders (accessed on 18 June 2021).
- El-Mallakh, P.; Findlay, J. Strategies to improve medication adherence in patients with schizophrenia: The role of support services. Neuropsychiatr. Dis. Treat. 2015, 11, 1077–1090. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gurmu, A.E.; Abdela, E.; Allele, B.; Cheru, E.; Amogne, B. Rate of Nonadherence to Antipsychotic Medications and Factors Leading to Nonadherence among Psychiatric Patients in Gondar University Hospital, Northwest Ethiopia. Adv. Psychiatry 2014, 2014, 1–5. [Google Scholar] [CrossRef] [Green Version]
- Semahegn, A.; Torpey, K.; Manu, A.; Assefa, N.; Tesfaye, G.; Ankomah, A. Psychotropic medication non-adherence and its associated factors among patients with major psychiatric disorders: A systematic review and meta-analysis. Syst. Rev. 2020, 9, 1–18. [Google Scholar] [CrossRef] [Green Version]
- Jaroensan, J. The development of schizophrenia care model in Saunsaranrom psychiatric hospital. J. Psychiatr. Nurs. Ment. Health 2015, 29, 85–98. (in Thai). Available online: https://he02.tci-thaijo.org/index.php/JPNMH/article/view/90480 (accessed on 15 May 2021).
- Inwanna, S.; Sangon, S.; Nintachan, P.; Rungruangsiripan, M. Factors associated with medication non-adherence behavior among persons with bipolar disorder. J. Psychiatr. Nurs. Ment. Health 2020, 34, 33–56. (in Thai). Available online: https://he02.tci-thaijo.org/index.php/JPNMH/article/view/169203 (accessed on 15 May 2021).
- World Health Organization. Adherence to Long-Term Therapies. Evidence for Action; World Health Organization: Geneva, Switzerland, 2003. [Google Scholar]
- De Geest, S.; Zullig, L.L.; Dunbar-Jacob, J.; Helmy, R.; Hughes, D.; Wilson, I.B.; Vrijens, B. ESPACOMP Medication Adherence Reporting Guideline (EMERGE). Ann. Intern. Med. 2018, 169, 30–35. [Google Scholar] [CrossRef] [Green Version]
- Dilokthornsakul, P.; Thoopputra, T.; Patanaprateep, O.; Kongsakon, R.; Chaiyakunapruk, N. Effects of medication adherence on hospitalizations and healthcare costs in patients with schizophrenia in Thailand. SAGE Open Med. 2016, 4, 2050312116637026. [Google Scholar] [CrossRef]
- Prukkanone, B.; Vos, T.; Burgess, P.; Chaiyakunapruk, N.; Bertram, M. Adherence to antidepressant therapy for major depressive patients in a psychiatric hospital in Thailand. BMC Psychiatry 2010, 10, 64. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chapman, S.C.E.; Horne, R. Medication nonadherence and psychiatry. Curr. Opin. Psychiatry 2013, 26, 446–452. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Depp, C.A.; Moore, D.J.; Patterson, T.L.; Lebowitz, B.D.; Jeste, D.V. Psychosocial interventions and medication adherence in bipolar disorder. Dialog Clin. Neurosci. 2008, 10, 239–250. [Google Scholar] [CrossRef]
- Tang, C.-H.; Hsieh, M.H.; Hung, S.-T.; Lee, I.H.; Lin, Y.-J.; Yang, Y.K. One-year post-hospital medical costs and relapse rates of bipolar disorder patients in Taiwan: A population-based study. Bipolar Disord. 2010, 12, 859–865. [Google Scholar] [CrossRef] [PubMed]
- Fernandez-Lazaro, C.I.; García-González, J.M.; Adams, D.P.; Fernandez-Lazaro, D.; Mielgo-Ayuso, J.; Caballero-Garcia, A.; Racionero, F.M.; Córdova, A.; Miron-Canelo, J.A. Adherence to treatment and related factors among patients with chronic conditions in primary care: A cross-sectional study. BMC Fam. Pr. 2019, 20, 1–12. [Google Scholar] [CrossRef]
- Higashi, K.; Medic, G.; Littlewood, K.J.; Diez, T.; Granström, O.; De Hert, M. Medication adherence in schizophrenia: Factors influencing adherence and consequences of nonadherence, a systematic literature review. Ther. Adv. Psychopharmacol. 2013, 3, 200–218. [Google Scholar] [CrossRef] [Green Version]
- Chakrabarti, S. Medication non-adherence in bipolar disorder: Review of rates, demographic and clinical predictors. World J. Meta-Anal. 2017, 5, 103. [Google Scholar] [CrossRef]
- Ramesh, M.; Parthasarathi, G.; Ram, D.; Lucca, J. Incidence and factors associated with medication nonadherence in patients with mental illness: A cross-sectional study. J. Postgrad. Med. 2015, 61, 251–256. [Google Scholar] [CrossRef]
- Moonchai, K.; Sangon, S.; Ninthachan, P.; Rungrungsiripan, M. Factors associated with adherence to medication in major depressive disorder patients. Thai Red Cross Nurs. J. 2020, 13, 240–260. [Google Scholar]
- Koomala, S.; Sangon, S.; Nintachan, P. Effect of medication adherence promotion program in schizophrenic patients. J. Psychiatr. Nurs. Ment. Health 2020, 34, 132–152. (in Thai). Available online: https://he02.tci-thaijo.org/index.php/JPNMH/article/view/181424 (accessed on 15 May 2021).
- Suwan, I.; Keawkingkeo, S. The effects of psychoeducation program on medication adherence among individuals with Schizophrenia in the community. J. Psychiatr. Nurs. Ment. Health 2020, 34, 152–162. (in Thai). Available online: https://he02.tci-thaijo.org/index.php/JPNMH/article/view/216112 (accessed on 15 May 2021).
- Sirthemanun, P.; Seeherunwong, A.; Au-Yeong, A.P. Cognitive behavior therapy for reducing positive symptoms in patients with Schizophrenia: Reviews for evidence-based practice. J. Psychiatr. Assoc. Thai. 2012, 57, 235–248. [Google Scholar]
- Francey, S.M.; O’Donoghue, B.; Nelson, B.; Graham, J.; Baldwin, L.; Yuen, H.P.; Kerr, M.J.; Ratheesh, A.; Allott, K.; Alvarez-Jimenez, M.; et al. Psychosocial Intervention with or Without Antipsychotic Medication for First-Episode Psychosis: A Randomized Noninferiority Clinical Trial. Schizophr. Bull. Open 2020, 1, 015. [Google Scholar] [CrossRef]
- Guo, X.; Zhai, J.; Liu, Z.; Fang, M.; Wang, B.; Wang, C.; Hu, B.; Sun, X.; Lv, L.; Lu, Z.; et al. Effect of Antipsychotic Medication Alone vs Combined with Psychosocial Intervention on Outcomes of Early-Stage Schizophrenia. Arch. Gen. Psychiatry 2010, 67, 895–904. [Google Scholar] [CrossRef]
- Jones, S. Psychotherapy of bipolar disorder: A review. J. Affect. Disord. 2004, 80, 101–114. [Google Scholar] [CrossRef]
- Miklowitz, D.J. Adjunctive Psychotherapy for Bipolar Disorder: State of the Evidence. Am. J. Psychiatry 2008, 165, 1408–1419. [Google Scholar] [CrossRef] [Green Version]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Haddaway, N.R.; Collins, A.; Coughlin, D.; A Kirk, S. The Role of Google Scholar in Evidence Reviews and Its Applicability to Grey Literature Searching. PLoS ONE 2015, 10, e0138237. [Google Scholar] [CrossRef] [Green Version]
- Garrard, J. Health Sciences Literature Review Made Easy: The Matrix Method, 5th ed.; Jones & Bartlett Learning: Burlington, MA, USA, 2017. [Google Scholar]
- Higgins, J.P.T.; Green, S. Cochrane Handbook for Systematic Reviews of Interventions: Cochrane Book Series; John Wiley & Sons: Chichester, UK, 2008. [Google Scholar]
- Suntarowit, N.; Wijitphanya, A.; Inkunthum, P. Effects of health promotion program on health behaviors for medication adherence of persons with Schizophrenia. J. Psychiatr. Nurs. Ment. Health 2020, 34, 153–168. (in Thai). Available online: https://he02.tci-thaijo.org/index.php/JPNMH/article/view/178331 (accessed on 15 May 2021).
- Tanabodee-tummajaree, P.; Themrasi, B. The development of the program to promote illness awareness and belief in taking medications on medication adherence in patients with Schizophrenia. J. Psychiatr. Nurs. Ment. Health 2018, 32, 133–153. (in Thai). Available online: https://he02.tci-thaijo.org/index.php/JPNMH/article/view/163112 (accessed on 15 May 2021).
- Luangmongkhonchai, N.; Lueboonthavatchai, O. The effect of perceived self-efficacy promoting group on medication adherence and follow-up intention of schizophrenia patients. J. Psychiatr. Nurs. Ment. Health 2011, 25, 69–81. (in Thai). Available online: https://he02.tci-thaijo.org/index.php/JPNMH/article/view/18171 (accessed on 15 May 2021).
- Phuengnam, K.; Uthis, P. The effect of family-centered empowerment program on drug adherence of people with Schizophrenia in the community. J. Baromarajonani Coll. Nurs. 2017, 23, 47–67. [Google Scholar]
- Uthaiphan, R.; Dangdomyouth, P. The effect of group motivational interviewing on medication compliance of schizophrenic patients in the community. J. Psychiatr. Nurs. Ment. Health 2013, 27, 136–148. (in Thai). Available online: https://he02.tci-thaijo.org/index.php/JPNMH/article/view/18126 (accessed on 15 May 2021).
- Wachiradilok, P.; Rungreangkulkit, R. Effectiveness of individual counseling program based on motivational interviewing and cognitive-behavioral technique for treatment compliance schizophrenia. J. Ment. Health Thail. 2008, 16, 41–51. (in Thai). Available online: https://he01.tci-thaijo.org/index.php/jmht/article/view/1467 (accessed on 15 May 2021).
- Eungsanran, J.; Napontan, P.; Hatthapanom, W. Effect of adherence group therapy compared with treatment as usual on schizophrenia patients in Khon Kaen Rajanagarindra Psychiatric Hospital. J. Nurses Assoc. Thail. N.East. Div. 2012, 30, 48–58. (in Thai). Available online: https://he01.tci-thaijo.org/index.php/jnat-ned/article/view/9240 (accessed on 15 May 2021).
- Maneesakorn, S.; Robson, D.; Gournay, K.; Gray, R. An RCT of adherence therapy for people with schizophrenia in Chiang Mai, Thailand. J. Clin. Nurs. 2007, 16, 1302–1312. [Google Scholar] [CrossRef]
- von Bormann, S.; Robson, D.; Gray, R. Adherence therapy following acute exacerbation of schizophrenia: A randomised controlled trial in Thailand. Int. J. Soc. Psychiatry 2015, 61, 3–9. [Google Scholar] [CrossRef]
- Chaiyajan, W.; Sitthimongkol, Y.; Yuttatri, P.; Kiainin, P. Effects of a psychoeducational program on attitude toward medication and compliance with the first appointment after discharge in schizophrenic patients. J. Nurs. Sci. 2009, 27, 73–81. [Google Scholar]
- Tufanaru, C.; Munn, Z.; Aromataris, E.; Campbell, J.; Hopp, L. Chapter 3: Systematic reviews of effectiveness. In Aromataris; JBI Manual for Evidence Synthesis; Munn, E.Z., Ed.; Joanna Briggs Institute (JBI): Adelaide, Australia, 2020; Available online: https://jbi-global-wiki.refined.site/space/MANUAL/3283910685/Chapter+3%3A+Systematic+reviews+of+effectiveness (accessed on 15 May 2021). [CrossRef]
- Lee, H.; Min, H.; Oh, S.-M.; Shim, K. Mobile Technology in Undergraduate Nursing Education: A Systematic Review. Health Inform. Res. 2018, 24, 97–108. [Google Scholar] [CrossRef] [Green Version]
- Gray, R.; Leese, M.; Bindman, J.; Becker, T.; Burti, L.; David, A.; Gournay, K.; Kikkert, M.; Koeter, M.; Puschner, B.; et al. Adherence therapy for people with schizophrenia: European multicentre randomized controlled trial. Br. J. Psychiatry 2006, 189, 508–514. [Google Scholar] [CrossRef]
- Spoelstra, S.L.; Schueller, M.; Hilton, M.; Ridenour, K. Interventions combining motivational interviewing and cognitive behaviour to promote medication adherence: A literature review. J. Clin. Nurs. 2014, 24, 1163–1173. [Google Scholar] [CrossRef]
- Sajatovic, M.; Velligan, D.I.; Weiden, P.J.; Valenstein, M.A.; Ogedegbe, G. Measurement of psychiatric treatment adherence. J. Psychosom. Res. 2010, 69, 591–599. [Google Scholar] [CrossRef] [Green Version]
- Lam, W.Y.; Fresco, P. Medication Adherence Measures: An Overview. BioMed Res. Int. 2015, 2015, 1–12. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Probst, P.; Grummich, K.; Heger, P.; Zaschke, S.; Knebel, P.; Ulrich, A.; Büchler, M.W.; Diener, M.K. Blinding in randomized controlled trials in general and abdominal surgery: Protocol for a systematic review and empirical study. Syst. Rev. 2016, 5, 48. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- World Health Organization. The ICD-10 Classification of Mental and Behavioural Disorders. Diagnostic Criteria for Research; World Health Organization: Geneva, Switzerland, 1993. [Google Scholar]
- Center for Behavioral Health Statistics and Quality. Impact of the DSM-IV to DSM-5 Changes on the National Survey on Drug Use and Health; Substance Abuse and Mental Health Services Administration: Rockville, MD, USA, 2016. [Google Scholar]
- Gaebel, W. Status of Psychotic Disorders in ICD-11. Schizophr. Bull. 2012, 38, 895–898. [Google Scholar] [CrossRef] [PubMed]
- Stirratt, M.J.; Dunbar-Jacob, J.; Crane, H.M.; Simoni, J.; Czajkowski, S.; Hilliard, M.; Aikens, J.E.; Hunter, C.M.; Velligan, D.I.; Huntley, K.; et al. Self-report measures of medication adherence behavior: Recommendations on optimal use. Transl. Behav. Med. 2015, 5, 470–482. [Google Scholar] [CrossRef] [PubMed] [Green Version]

| Authors Year | Aim | Design | Sample | Setting | Theory-Based | Intervention for Experimental Group | Regular Nursing Care for Control Group | Measurement | Findings | Quality Score |
|---|---|---|---|---|---|---|---|---|---|---|
| 1. Koomala et al., 2020 [25] | To Investigate the effect of medication adherence promotion program in patients with Schizophrenia. | Quasi-experiment | 24 patients with schizophrenia | Inpatient | 1. Psychoeducation 2. Family involvement | No. of sessions: 5 (1 session/day) 1. Therapeutic relationship 2. Individual psychoeducation 3. Individual psychoeducation 4. Family psychoeducation 5. Skill practice Duration: 60–90 min/session Initiation: 1 week before discharge | N/A | 1. Medication Adherence Behaviors Scale | - The program was effective in improving medication adherence. - At 2-week follow-up, the experimental group had a significantly different mean score on medication adherence (p < 0.001). - The experimental group had a significantly different mean score of medication adherence from the control group (p < 0.001). | High risk |
| 2. Suntarowit et al. 2020 [36] | Compare medication adherence behavior before and after receiving a health promotion program and compare the program with a control group. | Quasi-experiment | 68 patients with schizophrenia | Inpatient | 1. Pender’s health promotion theory | No. of sessions: 6 (in 1 week) 1. Identifying patient’s characteristics 2. Identifying prior behavior 3. Identifying medication adherence & non-adherence 4. Problem-solving 5. Intention to medication adherence 6. Follow-up Duration: 60 min/session Initiation: N/A | 1. Routine daily activity 2. Psychoeducation 3. Group therapy | 1. Health Behavior for Medication Adherence Assessment Form | The program was effective in increasing health behavior for medication adherence. Immediately after the program completion and 1-month follow-up, the experimental group had significantly higher mean medication adherence scores than before (p < 0.001). - The experimental group had a significantly higher mean medication adherence score than the control group (p < 0.001). | High risk |
| 3. Tanabo-deetumma-jaree & Themrasi, 2018 [37] | To develop and examine the program’s effectiveness to promote illness awareness and belief in taking medication on medication adherence. | Quasi-experiment | 60 patients with schizophrenia | Inpatient | 1. Necessary-concern framework | No. of sessions: 4 (in 2 weeks) 1. Illness awareness promotion 2. Belief in antipsychotic drugs 3. Common concerns and beliefs with antipsychotic drugs 4. Strategies to deal with barriers and individuals that affect medication adherence behavior Duration: 60 min/session Initiation: N/A | 1. Psychoeducation (disease, medication, and self-care) | 1. Brief Illness Perception Questionnaire 2. Beliefs in Taking Medication Questionnaire 3. Self-Medication Intake Record Form | The program was effective in increasing medication adherence behavior. - After program completion, the experiment group had a higher mean score of illness perception than the control group (p < 0.05). - After program completion, the experiment group had a lower belief score in taking medication than the control group (p < 0.05). - At 1,3, 6 months follow-up, the experiment group had a higher average day of medication adherence than the control group (p < 0.05). | High risk |
| 4. Luangmongkhonchai & Lueboon thavatchai, 2011 [38] | To examine the effects of perceived self-efficacy promotion on medication adherence and follow-up an intention. | Quasi-experiment | 40 patients with schizophrenia | Out-patient | 1. Bandura’s self-efficacy theory | No. of sessions: 5 (in 4 weeks) 1. Emotional & physiological state stimulation 2. Role model 3. Foremost mastery experience 4. Verbal persuasion 5. Previous success experiences and being confident to take medicines and follow-up Duration: 60 min/session Initiation: N/A | 1. Group psychoeducation | 1. Medication Adherence Scale 2. Follow-up Intention Scale | The program effectively increased medication adherence behavior and intention to follow up. - After program completion (week 5), the experimental group had significantly higher mean scores of medication adherence and follow-up intention than that before (p < 0.05). - Experiment group had significantly higher mean scores of medication adherence and follow-up intention than the control group (p < 0.05). | High risk |
| 5. Phuengnam & Uthis, 2017 [39] | To examine the effect of the family-centered empowerment program on medication adherence. | Quasi-experiment | 40 patients with schizophrenia | Out-patient | 1. Family-centered empowerment model 2. Empowerment 3. Families and family therapy | No. of sessions: 6 (in 4 weeks) 1. Building family’s awareness to medication adherence behavior 2. Developing family’s knowledge and skills 3. Recalling previous experiences on problem-solving 4. Practicing problem-solving skills 5. Exchanging experiences 6. Evaluation Duration: 90 min/session Initiation: N/A | 1. Physical and mental assessment 2. Counseling 3. Advising | 1. Drug Adherence Questionnaire | The program was effective in increasing medication adherence behavior. After program completion, the experimental group had significantly higher mean medication adherence scores than before (p < 0.05). - Experiment group had significantly higher mean scores of medication adherence than the control group (p < 0.05) | High risk |
| 6. Uthaiphan & Dangdomyouth, 2013 [40] | To examine the effect of group motivational interviewing on medication adherence. | Quasi-experiment | 40 patients with schizophrenia | Out-patient | 1. Motivation interviewing 2. Stage of change | No. of sessions: 5 (in 4 weeks) 1. Behavior change motivation 2. Strengthen commitment to a target behavior change 3. Strengthen commitment to a target behavior change 4. Strengthen commitment to a target behavior change 5. Follow-up Duration: 60–90 min/session Initiation: N/A | 1 Physical and mental assessment 2. Counseling 3. Advising 4. Group psychoeducation | 1. Compliance Behaviors Assessment Scale | The program was effective in increasing medication adherence behavior. After program completion, the experimental group had significantly higher mean medication adherence scores than before (p < 0.05). - Experiment group had significantly higher mean scores of medication adherence than the control group (p < 0.05). | High risk |
| 7. Wachiradilok & Rungreangkulkit, 2008 [41] | To examine the effect of individual counseling programs on treatment compliance. | Quasi-experiment | 100 patients with schizophrenia | Out-patient | 1. Motivational interviewing 2. Cognitive-behavioral technique | No. of sessions: 5 (1 session/week) 1. Therapeutic relationship 2. Seeking for beliefs and hesitation of treatment 3. Cognitive restructuring 4. Practicing medication administration skills 5. Family’s appropriate emotional expression Duration: 60 min/session Initiation: N/A | N/A | 1. Compliance Behaviors Assessment Scale 2. Knowledge of Self Management Scale 3. Brief Psychotic Rating Scale | The program was effective in increasing treatment adherence behavior and self-management. - At program completion, 3-month, and 6- month follow-up, the experiment group had significantly higher mean scores of compliance behaviors and self-management knowledge than the control group (p < 0.01). | High risk |
| 8. Eungsanran et al., 2012 [42] | To examine the effect of adherence group therapy program on treatment adherence, drug attitude, psychotic symptoms, and hospital readmission. | Quasi-experiment | 60 patients with schizophrenia | Inpatient | 1. Compliance therapy model 2. Motivational interviewing 3. Cognitive approaches | No. of sessions: 5 1. Engagement 2. Adherence Assessment 3. Eliminating barriers and hesitation on treatment adherence 4. Motivational interviewing and problem-solving 5. Improving self-confidence and practicing medication administration skills Duration: 60 min/session Initiation: N/A | N/A | 1. Medication Adherence Scale 2. Brief Psychotic Rating Scale 3. Drug Attitude Inventory | The program was effective in increasing treatment adherence behavior and positive drug attitude. - At 1-month and 3- month follow-up, the experiment group had significantly higher mean scores of medication adherence (p < 0.05) and drug attitude (p < 0.05), but lower mean scores of psychotic symptoms (p < 0.001) than the control group. - No hospital readmission within three months. | High risk |
| 9. Maneesakorn et al., 2007 [43] | To evaluate the effectiveness of adherence therapy on psychotic symptoms, general functioning, attitude towards and satisfaction with medication, and medication side effects. | Randomized Controlled Trial | 32 patients with schizophrenia | Inpatient | 1. Compliance therapy 2. Motivational interviewing 3. Cognitive approaches | No. of sessions: 8 (5 phases) (1 session/week) 1. Engagement 2. Assessment: problem, self-confidence, side effects experiences, beliefs, and attitudes 3. Rate readiness to take medicines 4. Intervention: problem-solving, timeline, exploring ambivalence, discussing beliefs and concerns, using medication in the future 5. Evaluation Duration: 15–60 min/session Initiation: N/A | 1. Medication treatment 2. Occupational therapy 3. Group therapy 4. Recreation therapy | Primary: 1. Positive and Negative Syndrome Scale Secondary: 2. Global Assessment of Functioning Scale 3. Drug Attitude Inventory 4. Satisfaction with Antipsychotic Medication Scale 5. Liverpool University Neuroleptic Side Effect Rating Scale | The program effectively increased treatment adherence, attitude toward, and satisfaction with medication. - At nine-week follow-up, the experiment group had significantly more significant improvement on psychotic symptoms (p = 0.001), attitude towards (p = 0.001), and satisfaction with medication (p = 0.019) than the control group. - No significant difference was found in general functioning or side effects. | Moderate risk |
| 10. von Borman et al., 2015 [44] | To examine the efficacy of adherence therapy on clinical outcomes. | Randomized Controlled Trial | 70 patients with schizophrenia | Inpatient | 1. Compliance therapy 2. Motivational interviewing 3. Cognitive approaches | No. of sessions: 8 sessions (6 exercises) (1 session/week) 1. Assessment: beliefs, problems, medication reconciliation 2. Problem-solving 3. Reviewing previous illness and treatment experiences 4. Seeking ambivalence to take medications 5. Examining beliefs about medication 6. Supporting life goals. Duration: 15–60 min/session Initiation: N/A | 1. Medication, vocational, and recreation therapy 2. Outreach community psychiatric support | Primary: 1. Positive and Negative Syndrome Scale Secondary: 2. Global Assessment of Functioning Scale 3. Drug Attitude Inventory 4. Liverpool University Neuroleptic Side Effect Rating Scale | The program was effective in improving psychotic symptoms - At 26-week follow-up, the experiment group had significantly more significant improvement on psychotic symptoms than the control group (p < 0.05). - No statistically significant differences were found in attitude toward treatment, functioning, or side effects. | High risk |
| 11. Chaiya-jan et al., 2009 [45] | To examine the effects of a psychoeducation program on attitude toward medication and compliance with a first follow-up appointment. | Quasi-experiment | 55 patients with schizophrenia | Inpatient | 1. Psychoeducation | No. of sessions: 10 sessions (1 session/day for the first six sessions, one session/week for the other four sessions) 1. Therapeutic relationship 2. Illness knowledge 3. Medication knowledge 4. Side effects management 5. Stress management 6. Symptom management 7–10. Assess health conditions, discuss the problem, and problem-solving Duration: -30 min/session (the first 6 sessions)-15–20 min/session (the other 4 sessions) Initiation: Last week of hospital stay | 1. Psychoeducation 2. Reminding of regimens adherence and a follow up visit 3. Home visit | 1. Drug Attitude Inventory | The program was effective in increasing positive attitudes toward medication. - After program completion, the experiment group had a significantly higher positive attitude toward medication (p < 0.05) and proportion of attendance for the first follow-up appointment than the control group (p < 0.05). | High risk |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Inwanna, S.; Duangchan, C.; Matthews, A.K. Effectiveness of Interventions to Promote Medication Adherence in Schizophrenic Populations in Thailand: A Systematic Review. Int. J. Environ. Res. Public Health 2022, 19, 2887. https://doi.org/10.3390/ijerph19052887
Inwanna S, Duangchan C, Matthews AK. Effectiveness of Interventions to Promote Medication Adherence in Schizophrenic Populations in Thailand: A Systematic Review. International Journal of Environmental Research and Public Health. 2022; 19(5):2887. https://doi.org/10.3390/ijerph19052887
Chicago/Turabian StyleInwanna, Suchanart, Cherdsak Duangchan, and Alicia K. Matthews. 2022. "Effectiveness of Interventions to Promote Medication Adherence in Schizophrenic Populations in Thailand: A Systematic Review" International Journal of Environmental Research and Public Health 19, no. 5: 2887. https://doi.org/10.3390/ijerph19052887
APA StyleInwanna, S., Duangchan, C., & Matthews, A. K. (2022). Effectiveness of Interventions to Promote Medication Adherence in Schizophrenic Populations in Thailand: A Systematic Review. International Journal of Environmental Research and Public Health, 19(5), 2887. https://doi.org/10.3390/ijerph19052887








