How Can We Actually Change Help-Seeking Behaviour for Mental Health Problems among the General Public? Development of the ‘PLACES’ Model
Abstract
:1. Introduction
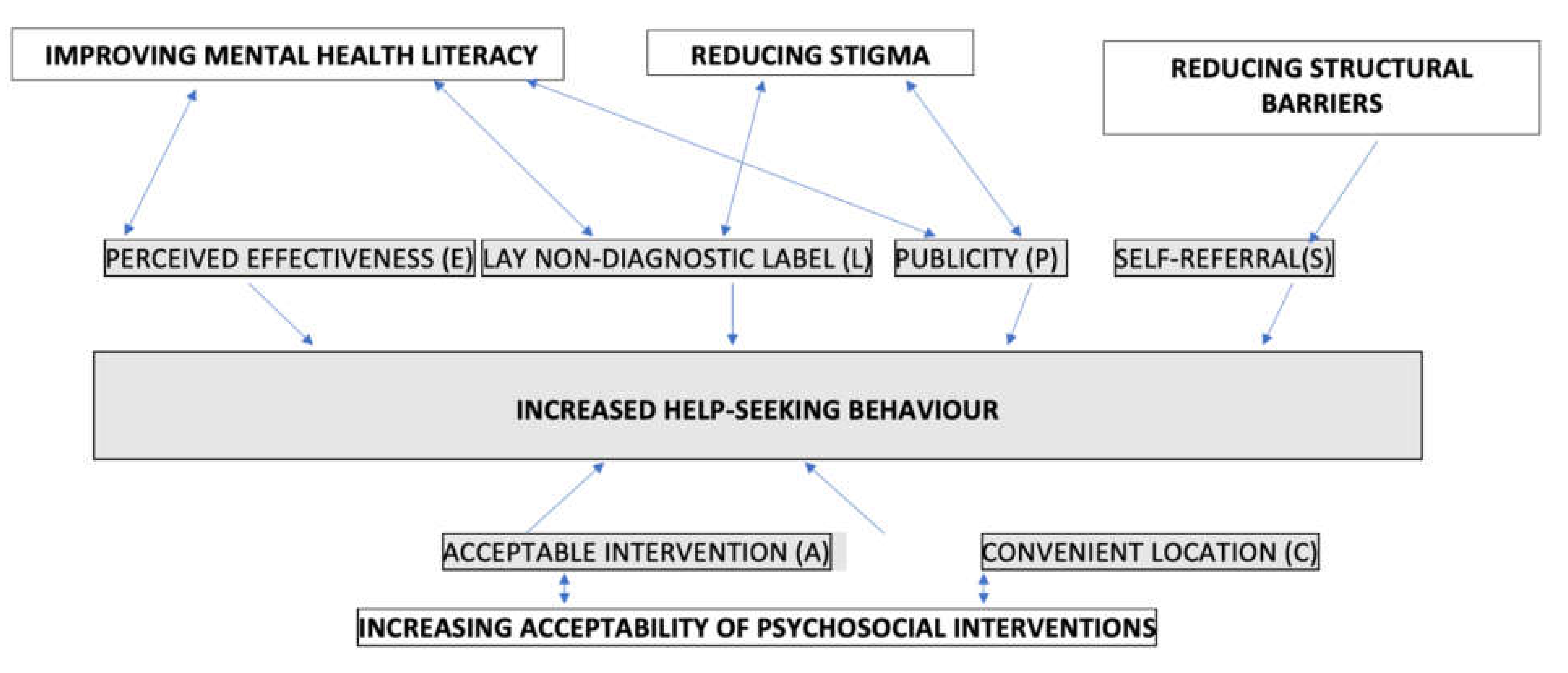
2. The Development and Rationale for Facilitating Factors in ‘PLACES’ Model
2.1. Stress Workshops
- (1)
- To be as accessible as possible, especially to non-consulters.
- (2)
- To offer an acceptable large-scale intervention.
- 1.
- SELF-REFERRAL (S)
- 2.
- PUBLICITY (P)
- 3.
- ACCEPTABLE (AND ENGAGING) INTERVENTION (A)
- 4.
- CONVENIENCE—SETTING AND TIMING (C)
- (1)
- Uptake: 176 attended the information meeting.
- (2)
- Non-consultation: Just under half (41%) had not previously consulted their GPs [20].
- (3)
- Severity: In this study, participants’ anxiety scores were above average (Spielberger trait scores 51.5), which is higher than the threshold for probable anxiety [34]. A finding from a later study of Stress participants indicated 66% of stress workshop participants scored above the ICD psychiatric threshold [35].
- (4)
- Ethnicity: Data was not collected in the initial study but was collected in a later study in London, where 13.2% reported themselves as Black (9.4%) or Asian (3.8%).
2.2. Depression Workshops
- 1.
- LAY NON-DIAGNOSTIC TITLES (L)
- 2.
- PERCEIVED) EFFECTIVENESS OF INTERVENTION (E)
- 3.
- ACCEPTABILITY OF PROGRAMME (A)
2.3. Stress Workshops for Adolescents
- 1.
- CONVENIENCE—SETTING AND TIMING (C)
- 2.
- ACCEPTABLE (AND ENGAGING) INTERVENTION (A)
- 3.
- LAY NON-DIAGNOSTIC TITLES (L)
- 4.
- SELF-REFERRAL (S)
- 5.
- PUBLICITY (P)
2.4. Postnatal Depression (PND) Workshops
- 1.
- PERCEIVED EFFECTIVENESS (E)
- 2.
- PUBLICITY AND SELF-REFERRAL (P and S)
- 3.
- CONVENIENCE (C)
- 4.
- ACCEPTABILITY (A)
3. Discussion
4. Clinical Implications
Research Implications
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- McManus, S.; Bebbington, P.E.; Jenkins, R.; Brugha, T. Mental Health and Wellbeing in England: Adult Psychiatric Morbidity Survey 2014; NHS Digital: Leeds, UK, 2016. [Google Scholar]
- Andrews, G.; Sanderson, K.; Slade, T.; Issakidis, C. Why does the burden of disease persist? Relating the burden of anxiety and depression to effectiveness of treatment. Bull. World Health Organ. 2000, 78, 446–454. [Google Scholar] [CrossRef] [PubMed]
- Brown, J.S.L.; Murphy, C.; Kelly, J.; Goldsmith, K. How can we successfully recruit depressed people? Lessons learned in recruiting depressed participants to a multi-site trial of a brief depression intervention (the ‘CLASSIC’ trial). Trials 2019, 20, 131. [Google Scholar] [CrossRef] [PubMed]
- Gulliver, A.; Griffiths, K.M.; Christensen, H.; Brewer, J.L. A systematic review of help-seeking interventions for depression, anxiety and general psychological distress. BMC Psychiatry 2012, 12, 81. [Google Scholar] [CrossRef] [Green Version]
- Xu, Z.; Huang, F.; Koesters, M.; Staiger, T.; Becker, T.; Thornicroft, G.; Ruesch, N. Effectiveness of interventions to promote help-seeking for mental health problems: Systematic review and meta-analysis. Psychol. Med. 2018, 48, 2658–2667. [Google Scholar] [CrossRef] [PubMed]
- Kessler, R.C.; Berglund, P.; Demler, O.; Jin, R.; Merikangas, K.R.; Walters, E.E. Lifetime Prevalence and Age-of-Onset Distributions of DSM-IV Disorders in the National Comorbidity Survey Replication. Arch. Gen. Psychiatry 2005, 62, 593–602. [Google Scholar] [CrossRef] [Green Version]
- Colizzi, M.; Lasalvia, A.; Ruggeri, M. Prevention and early intervention in youth mental health: Is it time for a multidisci-plinary and trans-diagnostic model for care? Int. J. Ment. Health Syst. 2020, 14, 23. [Google Scholar] [CrossRef] [Green Version]
- Gask, L.; Bower, P.; Lamb, J.; Burroughs, H.; Chew-Graham, C.; Edwards, S.; Hibbert, D.; Kovandžić, M.; Lovell, K.; Rogers, A.; et al. Improving access to psychosocial interventions for common mental health problems in the United Kingsdom: Narrative review and development of a conceptual model for complex interventions. BMC Health Serv. Res. 2012, 12, 249. [Google Scholar] [CrossRef] [Green Version]
- Clement, S.; Schauman, O.; Graham, T.; Maggioni, F.; Evans-Lacko, S.; Bezborodovs, N.; Morgan, C.; Rüsch, N.; Brown, J.S.; Thornicroft, G. What is the impact of mental health-related stigma on help-seeking? A systematic review of quantitative and qualitative studies. Psychol. Med. 2014, 45, 11–27. [Google Scholar] [CrossRef] [PubMed]
- Mojtabai, R.; Olfson, M.; Sampson, N.A.; Jin, R.; Druss, B.; Wang, P.S.; Wells, K.B.; Pincus, H.A.; Kessler, R.C. Barriers to mental health treatment: Results from the National Comorbidity Survey Replication. Psychol. Med. 2010, 41, 1751–1761. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bonabi, H.; Müller, M.; Ajdacic-Gross, V.; Eisele, J.; Rodgers, S.; Seifritz, E.; Rössler, W.; Rüsch, N. Mental Health Literacy, Attitudes to Help Seeking, and Perceived Need as Predictors of Mental Health Service Use: A Longitudinal Study. J. Nerv. Ment. Dis. 2016, 204, 321–324. [Google Scholar] [CrossRef] [Green Version]
- Codony, M.; Alonso, J.; Almansa, J.; Bernert, S.; De Girolamo, G.; De Graaf, R.; Haro, J.M.; Kovess, V.; Vilagut, G.; Kessler, R.C. Perceived Need for Mental Health Care and Service Use Among Adults in Western Europe: Results of the ESEMeD Project. Psychiatr. Serv. 2009, 60, 1051–1058. [Google Scholar] [CrossRef] [PubMed]
- Rafferty, L.A.; Wessely, S.; Stevelink, S.A.; Greenberg, N. The journey to professional mental health sup-port: A qualitative exploration of the barriers and facilitators impacting military veterans’ engagement with mental health treatment. Eur. J. Psychotraumatol. 2019, 10, 1700613. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gulliver, A.; Griffiths, K.M.; Christensen, H. Perceived barriers and facilitators to mental health help-seeking in young people: A systematic review. BMC Psychiatry 2010, 10, 113. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jorm, A.F. Mental health literacy—Public knowledge and beliefs about mental disorders. Br. J. Psychiatry 2000, 177, 396–401. [Google Scholar] [CrossRef] [Green Version]
- Bhui, K.; Stansfeld, S.; Hull, S.; Priebe, S.; Mole, F.; Feder, G. Ethnic variations in pathways to and use of specialist mental health services in the UK—Systematic review. Br. J. Psychiatry 2003, 182, 105–116. [Google Scholar] [CrossRef]
- Sekhon, M.; Cartwright, M.; Francis, J.J. Acceptability of healthcare interventions: An overview of reviews and development of a theoretical framework. BMC Health Serv. Res. 2017, 17, 88. [Google Scholar] [CrossRef] [Green Version]
- Musiat, P.; Goldstone, P.; Tarrier, N. Understanding the acceptability of e-mental health—Attitudes and expectations towards computerised self-help treatments for mental health problems. BMC Psychiatry 2014, 14, 109. [Google Scholar] [CrossRef] [Green Version]
- Anderson, J.; Howarth, E.; Vainre, M.; Jones, P.B.; Humphrey, A. A scoping literature review of service-level barriers for access and engagement with mental health services for children and young people. Child. Youth Serv. Rev. 2017, 77, 164–176. [Google Scholar] [CrossRef]
- Brown, J.; Cochrane, R.; Cardon, D. Running large-scale stress workshops for the general public: Promotion methods, pro-gramme content, clients’ satisfaction and drop-out rates. J. Ment. Health 1999, 8, 391–402. [Google Scholar]
- Brown, J.S.; Elliott, S.A.; Boardman, J.; Ferns, J.; Morrison, J. Meeting the unmet need for depression services with psy-cho-educational self-confidence workshops: Preliminary report. Br. J. Psychiatry 2004, 185, 511–515. [Google Scholar] [CrossRef] [Green Version]
- Sclare, I.; Michelson, D.; Malpass, L.; Coster, F.; Brown, J. Innovations in Practice: DISCOVER CBT workshops for 16-18-year-olds: Development of an open-access intervention for anxiety and depression in inner-city youth. Child Adolesc. Ment. Health 2014, 20, 102–106. [Google Scholar] [CrossRef]
- Van Lieshout, R.J.; Layton, H.; Rangan, M.; Ferro, M.A.; Brown, J.S.; Bieling, P.J. Treating Postpartum Depression With 1-Day Cognitive Behavioural Therapy-Based Workshops. J. Obstet. Gynaecol. Can. 2019, 41, 591–592. [Google Scholar] [CrossRef] [PubMed]
- Brown, J.; Cochrane, R.; Hancox, T. Large scale stress management workshops for the general public: A controlled evaluation. Behav. Cogn. Psychother. 2000, 28, 139–151. [Google Scholar] [CrossRef]
- Horrell, L.; Goldsmith, K.; Tylee, A.; Schmidt, U.; Murphy, C.; Bonin, E.M.; Beecham, J.K.; Kelly, J.; Raikundalia, S.; Brown, J. Brown One-day CBT self-confidence workshops for people with depression: Randomised controlled trial to assess clinical outcomes and investigate access by difficult to engage groups. Br. J. Psychiatry 2014, 204, 222–233. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brown, J.S.; Blackshaw, E.; Stahl, D.; Fennelly, L.; McKeague, L.; Sclare, I.; Michelson, D. School-based early intervention for anxiety and depression in older adolescents: A feasibility randomised controlled trial of a self-referral stress management workshop programme (“DISCOVER”). J. Adolesc. 2019, 71, 150–161. [Google Scholar] [CrossRef]
- Van Lieshout, R.J.; Layton, H.; Savoy, C.D.; Brown, J.S.; Ferro, M.A.; Streiner, D.L.; Bieling, P.J.; Feller, A.; Hanna, S. Effect of Online 1-Day Cognitive Behavioral Therapy–Based Workshops Plus Usual Care vs Usual Care Alone for Postpartum Depression: A Ran-domized Clinical Trial. JAMA Psychiatry 2021, 78, 1200–1207. [Google Scholar] [CrossRef] [PubMed]
- Brown, J.S.; Boardman, J.; Whittinger, N.; Ashworth, M. Can a self-referral system help improve access to psychological treatments? Br. J. Gen. Pract. 2010, 60, 365–371. [Google Scholar] [CrossRef] [Green Version]
- Sisley, E.; Hutton, J.; Goodbody, L.; Brown, J.S.L. ‘You swim or you sink...I’m still swimming’: An interpretative phenome-nonological analysis of African Caribbean women’s experiences and managment of emotional distress. Health Soc. Care Community 2011, 19, 392–402. [Google Scholar] [CrossRef]
- Apolinário-Hagen, J.; Kemper, J.; Stürmer, C. Public Acceptability of E-Mental Health Treatment Services for Psychological Problems: A Scoping Review. JMIR Ment. Health 2017, 4, e10. [Google Scholar] [CrossRef]
- Middendorf, J.; Kalish, A. The ‘Change-up” in lectures. Natl. Teach. Learn. Forum 1996, 5, 1–5. [Google Scholar]
- Bisson, J.I.; Ehlers, A.; Matthews, R.; Pilling, S.; Richards, D.; Turner, S. Psychological treatments for chronic post-traumatic stress disorder: Systematic review and meta-analysis. Br. J. Psychiatry 2007, 190, 97–104. [Google Scholar] [PubMed] [Green Version]
- Moreno, C.; Wykes, T.; Galderisi, S.; Nordentoft, M.; Crossley, N.; Jones, N.; Cannon, M.; Correll, C.U.; Byrne, L.; Carr, S.; et al. How mental health care should change as a consequence of the COVID-19 pandemic. Lancet Psychiatry 2020, 7, 813–824. [Google Scholar] [CrossRef]
- Van Dam, N.T.; Gros, D.F.; Earleywine, M.; Antony, M.M. Establishing a trait anxiety threshold that signals likelihood of anxiety disorders. Anxiety Stress Coping 2013, 26, 70–86. [Google Scholar] [CrossRef]
- Brown, J.S.; Boardman, J.; Elliott, S.A.; Howay, E.; Morrison, J. Are self-referrers just the worried well? Soc. Psychiatry Psy-Chiatr. Epidemiol. 2005, 40, 396–401. [Google Scholar] [CrossRef]
- Watkins, E.; Elliott, S.; Stanhope, N.; Button, J.; Williams, R.; Brown, J.S.L. Meeting the needs for psychological treatment of people with common mental disorders: An exploratory study. J. Ment. Health 2000, 9, 445–456. [Google Scholar]
- Woodall, A.; Morgan, C.; Sloan, C.; Howard, L. Barriers to participation in mental health research: Are there specific gender, ethnicity and age related barriers? BMC Psychiatry 2010, 10, 103. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gronholm, P.C.; Nye, E.; Michelson, D. Stigma related to targeted school-based mental health interventions: A systematic review of qualitative evidence. J. Affect. Disord. 2018, 240, 17–26. [Google Scholar] [CrossRef] [Green Version]
- Pill, R.; Prior, L.; Wood, F. Lay attitudes to professional consultations for common mental disorder: A sociological perspective. Br. Med. Bull. 2001, 57, 207–219. [Google Scholar] [CrossRef] [Green Version]
- Beck, A.T.; Rush, A.J.; Shaw, B.F.; Emery, G. Cognitive Therapy of Depression; Guilford Press: New York, NY, USA, 1979. [Google Scholar]
- Brown, J.S.L. Increasing access to psychological treatments for adults by improving uptake and equity: Rationale and lessons from the UK. Int. J. Ment. Health Syst. 2018, 12, 67. [Google Scholar] [CrossRef]
- O’connor, P.J.; Martin, B.; Weeks, C.S.; Ong, L. Factors that influence young people’s mental health help-seeking be-haviour: A study based on the Health Belief Model. J. Adv. Nurs. 2014, 70, 2577–2587. [Google Scholar] [CrossRef]
- House, J.; Marasli, P.; Lister, M.; Brown, J.S.L. Male views on help-seeking for depression: A Q methodology study. Psychol. Psychother. Theory Res. Pr. 2017, 91, 117–140. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fennell, M. Overcoming Low Self-Esteem: A Self-Help Guide; Robinson: London, UK, 2006. [Google Scholar]
- Rickwood, D.; Deane, F.P.; Wilson, C.J.; Ciarrochi, J. Young people’s help-seeking for mental health problems. Aust. E-J. Adv. Ment. Health 2005, 4, 218–251. [Google Scholar] [CrossRef] [Green Version]
- McKeague, L.; Morant, N.; Blackshaw, E.; Brown, J.S.L. Exploring the feasibility and acceptability of a school-based self-referral intervention for emotional difficulties in older adolescents: Qualitative perspectives from students and school staff. Child Adolesc. Ment. Health 2017, 23, 198–205. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bowen, A.; Bowen, R.; Butt, P.; Rahman, K.; Muhajarine, N. Patterns of Depression and Treatment in Pregnant and Post-partum Women. Can. J. Psychiatry 2012, 57, 161–167. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- O’Mahen, H.A.; Flynn, H.A. Preferences and Perceived Barriers to Treatment for Depression during the Perinatal Period. J. Women’s Health 2008, 17, 1301–1309. [Google Scholar] [CrossRef] [PubMed]
- Chabrol, H.; Teissedre, F.; Armitage, J.; Danel, M.; Walburg, V. Acceptability of psychotherapy and antidepressants for postnatal depression among newly delivered mothers. J. Reprod. Infant Psychol. 2004, 22, 5–12. [Google Scholar] [CrossRef]
- Arundell, L.L.; Barnett, P.; Buckman, J.E.; Saunders, R.; Pilling, S. The effectiveness of adapted psychological interven-tions for people from ethnic minority groups: A systematic review and conceptual typology. Clin. Psychol. Rev. 2021, 88, 102063. [Google Scholar] [CrossRef]
- Clark, D.M.; Layard, R.; Smithies, R.; Richards, D.A.; Suckling, R.; Wright, B. Improving access to psychological therapy: Initial evaluation of two UK demonstration sites. Behav. Res. Ther. 2009, 47, 910–920. [Google Scholar] [CrossRef] [Green Version]
- Brown, J.S.L.; Ferner, H.; Wingrove, J.; Aschan, L.; Hatch, S.L.; Hotopf, M. How equitable are psychological therapy services in South East London now? A comparison of referrals to a new psychological therapy services with participants in a psychiatric morbidity survey in the same London borough. Soc. Psychiatry Psychiatr. Epidemiol. 2014, 49, 1893–1902. [Google Scholar] [CrossRef] [Green Version]
- Kennedy, I.; Whybrow, D.; Jones, N.; Sharpley, J.; Greenberg, N. A service evaluation of self-referral to military mental health teams. Occup. Med. 2016, 66, 394–398. [Google Scholar] [CrossRef] [Green Version]
- Andersen, R.M. Revisiting the behavioral model and access to medical care: Does it matter? J. Health Soc. Behav. 1995, 30–36. [Google Scholar] [CrossRef]
- Tomczyk, S.; Schomerus, G.; Stolzenburg, S.; Muehlan, H.; Schmidt, S. Ready, Willing and Able? An Investigation of the Theory of Planned Behaviour in Help-Seeking for a Community Sample with Current Untreated Depressive Symptoms. Prev. Sci. 2020, 21, 749–760. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- National Collaborating Centre for Mental Health. Depression: The Treatment and Management of Depression in Adults (Updated Edition); British Psychological Society: Leicester, UK, 2010. [Google Scholar]
- The British Psychological Society & The Royal College of Psychiatrists; Stanley Hunt: Leicester, UK, 2010.
- Iorfino, F.; Cheng, V.W.S.; Cross, S.P.; Yee, H.F.; Davenport, T.A.; Scott, E.M.; Hickie, I.B. Right Care, First Time: De-veloping a Theory-Based Automated Protocol to Help Clinically Stage Young People Based on Severity and Persistence of Mental Illness. Front. Public Health 2021, 9, 1230–1239. [Google Scholar] [CrossRef]
- Sagar-Ouriaghli, I.; Brown, J.S.L.; Tailor, V.; Godfrey, E. Engaging male students with mental health support: A qualitative focus group study. BMC Public Heal. 2020, 20, 1159. [Google Scholar] [CrossRef]
- Aggarwal, N.K.; Pieh, M.C.; Dixon, L.; Guarnaccia, P.; Alegria, M.; Lewis-Fernandez, R. Clinician descriptions of commu-nication strategies to improve treatment engagement by racial/ethnic minorities in mental health services: A systematic review. Patient Educ. Couns. 2016, 99, 198–209. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Barello, S.; Castiglioni, C.; Bonanomi, A.; Graffigna, G. The Caregiving Health Engagement Scale (CHE-s): Development and initial validation of a new questionnaire for measuring family caregiver engagement in healthcare. BMC Public Heal. 2019, 19, 1562. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Brown, J.S.L.; Lisk, S.; Carter, B.; Stevelink, S.A.M.; Van Lieshout, R.; Michelson, D. How Can We Actually Change Help-Seeking Behaviour for Mental Health Problems among the General Public? Development of the ‘PLACES’ Model. Int. J. Environ. Res. Public Health 2022, 19, 2831. https://doi.org/10.3390/ijerph19052831
Brown JSL, Lisk S, Carter B, Stevelink SAM, Van Lieshout R, Michelson D. How Can We Actually Change Help-Seeking Behaviour for Mental Health Problems among the General Public? Development of the ‘PLACES’ Model. International Journal of Environmental Research and Public Health. 2022; 19(5):2831. https://doi.org/10.3390/ijerph19052831
Chicago/Turabian StyleBrown, June S. L., Stephen Lisk, Ben Carter, Sharon A. M. Stevelink, Ryan Van Lieshout, and Daniel Michelson. 2022. "How Can We Actually Change Help-Seeking Behaviour for Mental Health Problems among the General Public? Development of the ‘PLACES’ Model" International Journal of Environmental Research and Public Health 19, no. 5: 2831. https://doi.org/10.3390/ijerph19052831
APA StyleBrown, J. S. L., Lisk, S., Carter, B., Stevelink, S. A. M., Van Lieshout, R., & Michelson, D. (2022). How Can We Actually Change Help-Seeking Behaviour for Mental Health Problems among the General Public? Development of the ‘PLACES’ Model. International Journal of Environmental Research and Public Health, 19(5), 2831. https://doi.org/10.3390/ijerph19052831




