Differences in Body Mass Index Trajectories and Their Classification, Sociodemographic Characteristics, and Health Behaviors between People with and without Disabilities Using Korea Health Panel Survey Data
Abstract
1. Introduction
2. Materials and Methods
2.1. Data
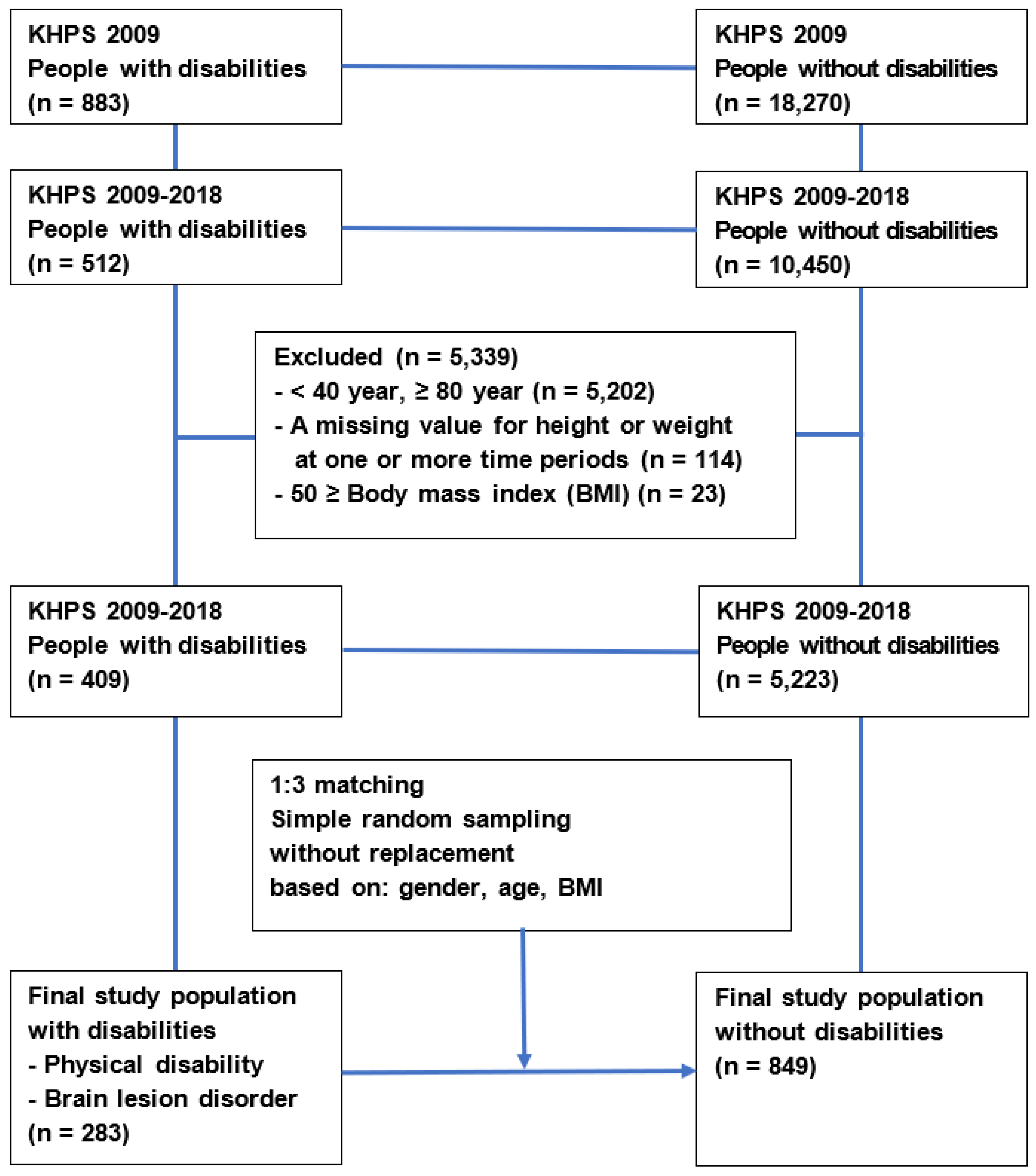
2.2. Study Population
2.3. Measurements
2.4. Analysis
3. Results
3.1. BMI Trajectories for All Study Subjects
3.2. BMI Trajectories by Subgroup According to Disability, Gender, and Age
3.3. BMI Clusters by Sociodemographic Characteristics and Health Behaviors
3.4. According to Sociodemographic Characteristics and Health Behaviors, Trajectories Were Classified into BMI Clusters
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| BMI | Body Mass Index |
| KHPS | Korea Health Panel Survey |
| SD | Standard Deviation |
Appendix A. Measures of Change
Appendix A.1. Elementary Measures of Change (1–10)
Appendix A.2. Measures of the Nonlinearity and Inconsistency of Change (11–18)
Appendix A.3. Measures Sensitive to Nonmonotonicity and Abrupt Short-Term Fluctuations (19–24)
References
- Ministry of Health and Welfare; Korea Institute for Health and Social Affairs. 2017 Survey on Disabled Persons; Ministry of Health and Welfare: Sejong, Korea, 2017.
- An, R.; Andrade, F.; Chiu, C.Y. Overweight and obesity among U.S. adults with and without disability, 1999–2012. Prev. Med. Rep. 2015, 2, 419–422. [Google Scholar] [CrossRef][Green Version]
- Froehlich-Grobe, K.; Lee, J.; Washburn, R.A. Disparities in obesity and related conditions among Americans with disabilities. Am. J. Prev. Med. 2013, 45, 83–90. [Google Scholar] [CrossRef]
- Weil, E.; Wachterman, M.; McCarthy, E.P.; Davis, R.B.; O’Day, L.I.; Iezzoni, L.I.; Wee, C.C. Obesity among adults with disabling conditions. JAMA 2002, 288, 1265–1268. [Google Scholar] [CrossRef] [PubMed]
- Peterson, M.D.; Mahmoudi, E. Healthcare utilization associated with obesity and physical disabilities. Am. J. Prev. Med. 2015, 48, 426–435. [Google Scholar] [CrossRef]
- Doshi, J.A.; Poisky, D.; Chang, V.W. Prevalence and trends in obesity among aged and disabled U.S. medicare beneficiaries, 1997–2002. Health Aff. 2007, 26, 1111–1117. [Google Scholar] [CrossRef][Green Version]
- Dahl, A.K.; Reynolds, C.A.; Fall, T.; Magnusson, P.K.; Pedersen, N.L. Multifactorial analysis of changes in body mass index across the adult life course: A study with 65 years of follow-up. Int. J. Obes. 2014, 38, 1133–1141. [Google Scholar] [CrossRef]
- Korea Health Panel Survey. Available online: https://www.khp.re.kr:444/eng/main.do (accessed on 10 August 2021).
- Statistics Korea. Available online: https://www.census.go.kr/mainView.do (accessed on 12 September 2021).
- Ministry of Health and Welfare. Available online: http://www.mohw.go.kr/react/gm/sgm0701ls.jsp?PAR_MENU_ID=13&MENU_ID=1304080902 (accessed on 20 March 2021).
- Park, J.H.; Park, J.H.; Lee, S.Y.; Kim, S.Y.; Shin, Y.; Kim, S.Y. Disparities in antihypertensive medication adherence in persons with disabilities and without disabilities: Results of a Korean population-based study. Arch. Phys. Med. Rehabil. 2008, 89, 1460–1467. [Google Scholar] [CrossRef]
- Kuchibhatla, M.N.; Fillenbaum, G.G.; Kraus, W.E.; Cohen, H.J.; Blazer, D.G. Trajectory classes of body mass index in a representative elderly community sample. J. Gerontol. A Biol. Sci. Med. Sci. 2013, 68, 699–704. [Google Scholar] [CrossRef] [PubMed]
- Salmela, J.; Lallukka, T.; Mauramo, E.; Rahkonen, O.; Kanerva, N. Body mass index trajectory–specific changes in economic circumstances: A person-oriented approach among midlife and ageing Finns. Int. J. Environ. Res. Public Health 2020, 17, 3668. [Google Scholar] [CrossRef]
- Leffondre´, K.; Abrahamowicza, M.; Regeassec, A.; Hawkerd, G.A.; Badleye, E.M.; McCuskera, J.; Belzile, E. Statistical measures were proposed for identifying longitudinal patterns of change in quantitative health indicators. J. Clin. Epidemiol. 2004, 57, 1049–1062. [Google Scholar] [CrossRef]
- Liou, T.H.; Pi-Sunyer, X.; Laferrere, B. Physical disability and obesity. Nutr. Rev. 2005, 63, 321–331. [Google Scholar] [CrossRef]
- Sun, W.; Watanabe, M.; Tanimoto, Y.; Shibutani, T.; Kono, R.; Saito, M.; Usuda, K.; Kono, K. Factors associated with good self-rated health of non-disabled elderly living alone in Japan: A cross-sectional study. BMC Public Health 2007, 7, 297. [Google Scholar] [CrossRef]
- Schwartz, N.; Buliungb, R.; Wilson, K. Disability and food access and insecurity: A scoping review of the literature. Health Place 2019, 57, 107–121. [Google Scholar] [CrossRef] [PubMed]
- Holmgren, M.; Sandberg, M.; Ahlström, G. The complexity of reaching and maintaining a healthy body weight—The experience from adults with a mobility disability. BMC Obes. 2018, 5, 33. [Google Scholar] [CrossRef]
- Story, M.F.; Schwier, E.; Kailes, J.I. Perspectives of patients with disabilities on the accessibility of medical equipment: Examination tables, imaging equipment, medical chairs, and weight scales. Disabil. Health J. 2009, 2, 169–179. [Google Scholar] [CrossRef]
- Fox, M.H.; Witten, M.H.; Lullo, C. Reducing obesity among people with disabilities. J. Disabil. Policy Stud. 2014, 25, 175–185. [Google Scholar] [CrossRef]
- Feng, X.; Wilson, A. Getting bigger, quicker? Gendered socioeconomic trajectories in body mass index across the adult lifecourse: A longitudinal study of 21,403 Australians. PLoS ONE 2015, 10, e0141499. [Google Scholar] [CrossRef] [PubMed]
- Kanter, R.; Caballero, B. Global gender disparities in obesity: A review. ASN 2012, 3, 491–498. [Google Scholar] [CrossRef] [PubMed]
- Gretebeck, K.A.; Sabatini, L.M.; Black, D.R.; Gretebeck, R.J. Physical activity, functional ability, and obesity in older adults: A gender difference. J. Gerontol. Nurs. 2017, 43, 38–46. [Google Scholar] [CrossRef] [PubMed]
- Lagarrigue, A.; Ajana, S.; Capuron, L.; Feart, C.; Moisan, M.P. Obesity in French inmates: Gender differences and relationship with mood, eating behavior and physical activity. PLoS ONE 2017, 12, e0170413. [Google Scholar] [CrossRef] [PubMed]
- Coen, S.E.; Rosenberg, M.W.; Davidson, J. “It’s gym, like g-y-m not J-i-m”: Exploring the role of place in the gendering of physical activity. Soc. Sci. Med. 2018, 196, 29–36. [Google Scholar] [CrossRef] [PubMed]
- Brooks, R.; Maklakov, A. Sex differences in obesity associated with total fertility rate. PLoS ONE 2010, 5, e10587. [Google Scholar] [CrossRef] [PubMed]
- Acevedo, P.; Mora-Urda, A.I.; Montero, P. Social inequalities in health: Duration of unemployment unevenly effects on the health of men and women. Eur. J. Public Health 2020, 30, 305–310. [Google Scholar] [CrossRef]
- Laitinen, J.; Power, C.; Ek, E.; Sovio, U.; Järvelin, M.R. Unemployment and obesity among young adults in a northern Finland 1966 birth cohort. Int. J. Obes. 2002, 26, 1329–1338. [Google Scholar] [CrossRef]
- Loman, T.; Lallukka, T.; Laaksonen, M.; Rahkonen, O.; Lahelma, E. Multiple socioeconomic determinants of weight gain: The Helsinki Health Study. BMC Public Health 2013, 13, 259. [Google Scholar] [CrossRef]
- Yamamoto, R.; Shinzawa, M.; Yoshimura, R.; Taneike, M.; Nakanishi, K.; Nishida, M.; Yamauchi-Takihara, K.; Kudo, T.; Moriyama, T. Living alone and prediction of weight gain and overweight/obesity in university students: A retrospective cohort study. J. Am. Coll. Health. 2021, 29, 1–10. [Google Scholar] [CrossRef]
- Lund, R.; Due, P.; Modvig, J.; Holsetin, B.E.; Damsgaard, M.T.; Andersen, P.K. Cohabitation and marital status as predictors of mortality—An eight year follow-up study. Soc. Sci. Med. 2002, 55, 673–679. [Google Scholar] [CrossRef]
- Kilpi, F.; Konttinen, H.; Silventoinen, K.; Martikainen, P. Living arrangements as determinants of myocardial infarction incidence and survival: A prospective register study of over 300,000 Finnish men and women. Soc. Sci. Med. 2015, 133, 93–100. [Google Scholar] [CrossRef]
- Schuler, B.; Daundasekara, S.; Hernandez, D.; Dumenci, L.; Clark, M.; Fisher, J.; Miller, A. Economic hardship and child intake of foods high in saturated fats and added sugars: The mediating role of parenting stress among high-risk families. Public Health Nutr. 2020, 23, 2781–2792. [Google Scholar] [CrossRef] [PubMed]
- Smed, S.; Tetens, I.; Bøker Lund, T.; Holm, L.; Ljungdalh Nielsen, A. The consequences of unemployment on diet composition and purchase behaviour: A longitudinal study from Denmark. Public Health Nutr. 2018, 21, 580–592. [Google Scholar] [CrossRef]
- Van Domelen, D.R.; Koster, A.; Caserotti, P.; Brychta, R.J.; Chen, K.Y.; McClain, J.J.; Troiano, R.P.; Berrigan, D.; Harris, T.B. Employment and physical activity in the U.S. Am. J. Prev. Med. 2011, 41, 136–145. [Google Scholar] [CrossRef] [PubMed]
- Blanchflower, D.G.; Bryson, A. Unemployment and sleep: Evidence from the United States and Europe. Econ. Hum. Biol. 2021, 43, 101042. [Google Scholar] [CrossRef]
- Lyu, X.; Dunietz, G.L.; O’Brien, L.; Chervin, R.; Shedden, K. 549 Associations of bedtime, wake-time and employment status by gender and race. Sleep 2021, 44, A216–A218. [Google Scholar] [CrossRef]
- Beccuti, G.; Pannain, S. Sleep and obesity. Curr. Opin. Clin. Nutr. Metab. Care 2011, 14, 402–412. [Google Scholar] [CrossRef] [PubMed]
- López-García, E.; Faubel, R.; León-Muñoz, L.; Zuluaga, M.C.; Banegas, J.R.; Rodríguez-Artalejo, F. Sleep duration, general and abdominal obesity, and weight change among the older adult population of Spain. Am. J. Clin. Nutr. 2008, 87, 310–316. [Google Scholar] [CrossRef] [PubMed]
- Chung, W.; Kim, R. A reversal of the association between education level and obesity risk during ageing: A gender-specific longitudinal study in South Korea. Int. J. Environ. Res. Public Health 2020, 17, 6755. [Google Scholar] [CrossRef]
- Wang, M.; Yi, Y.; Roebothan, B.; Colbourne, J.; Maddalena, V.; Wang, P.P.; Sun, G. Body mass index trajectories among middle-aged and elderly Canadians and associated health outcomes. J. Environ. Public Health 2016, 2016, 7014857. [Google Scholar] [CrossRef]
- Mirowsky, J.; Ross, C.E. Education, learned effectiveness and health. Lond. Rev. Educ. 2005, 3, 205–220. [Google Scholar] [CrossRef]
- Zajacova, A.; Lawrence, E.M. The relationship between education and health: Reducing disparities through a contextual approach. Annu. Rev. Public Health 2018, 39, 273–289. [Google Scholar] [CrossRef]


| Intercept (BMI at Baseline) | Linear Slope | |||||
|---|---|---|---|---|---|---|
| n | % | Mean | SD 1 | Mean | SD | |
| Lower BMI | 640 | 56.5 | 22.3 | 1.91 | −0.00 | 0.21 |
| Higher BMI | 492 | 43.5 | 26.5 | 2.16 | −0.01 | 0.26 |
| People with Disabilities (n = 283) | People without Disabilities (n = 849) | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Intercept (BMI at Baseline) | Linear Slope | Intercept (BMI at Baseline) | Linear Slope | |||||||||||
| Age | Cluster | n | % | Mean | SD | Mean | SD | n | % | Mean | SD | Mean | SD | |
| Men | 40–59 | Lower BMI | 49 | 69.0 | 23.5 | 2.58 | 0.02 | 0.13 | 130 | 61.0 | 22.5 | 1.88 | 0.00 | 0.18 |
| Higher BMI | 22 | 31.0 | 24.7 | 3.94 | 0.06 | 0.37 | 83 | 39.0 | 26.3 | 1.96 | 0.00 | 0.21 | ||
| 60–79 | Lower BMI | 63 | 76.8 | 22.5 | 1.98 | 0.01 | 0.19 | 5 | 2.0 | 22.1 | 1.58 | 0.00 | 0.00 | |
| Higher BMI | 19 | 23.2 | 26.9 | 2.87 | −0.10 | 0.26 | 241 | 98.0 | 23.3 | 2.36 | 0.01 | 0.19 | ||
| Women | 40–59 | Lower BMI | 27 | 77.1 | 22.8 | 2.84 | −0.04 | 0.26 | 54 | 51.4 | 21.3 | 2.09 | 0.03 | 0.20 |
| Higher BMI | 8 | 22.9 | 29.5 | 6.54 | −0.20 | 0.45 | 51 | 48.6 | 26.3 | 2.40 | 0.00 | 0.22 | ||
| 60–79 | Lower BMI | 62 | 65.3 | 23.8 | 2.08 | −0.02 | 0.22 | 232 | 81.4 | 24.8 | 2.61 | −0.02 | 0.22 | |
| Higher BMI | 33 | 34.7 | 28.1 | 2.17 | −0.05 | 0.34 | 53 | 18.6 | 25.6 | 2.65 | −0.04 | 0.46 | ||
| Variables | People with Disabilities | People without Disabilities | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total | Lower BMI | Higher BMI | Total | Lower BMI | Higher BMI | ||||||||||
| n | n | % | n | % | X2 | p-Value | n | n | % | n | % | X2 | p-Value | ||
| Total | 283 | 161 | 56.9 | 122 | 43.1 | 849 | 479 | 56.4 | 370 | 43.6 | |||||
| Gender | Men | 153 | 100 | 65.4 | 53 | 34.6 | 9.003 | 0.003 | 459 | 295 | 64.3 | 164 | 35.7 | 24.357 | 0.000 |
| Women | 130 | 61 | 46.9 | 69 | 53.1 | 390 | 184 | 47.2 | 206 | 52.8 | |||||
| Age | 40–59 | 106 | 57 | 53.8 | 49 | 46.2 | 0.484 | 0.487 | 318 | 190 | 59.7 | 128 | 40.3 | 2.080 | 0.149 |
| 60–79 | 177 | 104 | 58.8 | 73 | 41.2 | 531 | 289 | 54.4 | 242 | 45.6 | |||||
| Residence area | Large city | 104 | 52 | 50.0 | 52 | 50.0 | 2.754 | 0.097 | 311 | 165 | 53.1 | 146 | 46.9 | 2.049 | 0.152 |
| Small city and rural | 179 | 109 | 60.9 | 70 | 39.1 | 538 | 314 | 58.4 | 224 | 41.6 | |||||
| Living alone | Yes | 32 | 11 | 34.4 | 21 | 65.6 | 6.459 | 0.011 | 70 | 30 | 42.9 | 40 | 57.1 | 5.122 | 0.024 |
| No | 251 | 150 | 59.8 | 101 | 40.2 | 779 | 449 | 57.6 | 330 | 42.4 | |||||
| Education | Less than middle school | 189 | 109 | 57.7 | 80 | 42.3 | 0.062 | 0.803 | 487 | 249 | 51.1 | 238 | 48.9 | 12.499 | 0.000 |
| More than high school | 94 | 52 | 55.3 | 42 | 44.7 | 362 | 230 | 63.5 | 132 | 36.5 | |||||
| Current economic | Yes | 128 | 84 | 65.6 | 44 | 34.4 | 6.634 | 0.010 | 543 | 329 | 60.6 | 214 | 39.4 | 10.189 | 0.001 |
| activity | No | 155 | 77 | 49.7 | 78 | 50.3 | 306 | 150 | 49.0 | 156 | 51.0 | ||||
| Adjusted income | 1st quintile (lowest) | 105 | 55 | 52.4 | 50 | 47.6 | 1.057 | 0.304 | 188 | 99 | 52.7 | 89 | 47.3 | 0.964 | 0.326 |
| 2nd–5th quintiles | 175 | 104 | 59.4 | 71 | 40.6 | 654 | 373 | 57.0 | 281 | 43.0 | |||||
| Type of health | National health insurance | 233 | 134 | 57.5 | 99 | 42.5 | 0.088 | 0.766 | 815 | 462 | 56.7 | 353 | 43.3 | 0.353 | 0.553 |
| insurance | Medical aid | 50 | 27 | 54.0 | 23 | 46.0 | 34 | 17 | 50.0 | 17 | 50.0 | ||||
| Heavy drinking | Yes | 25 | 14 | 56.0 | 11 | 44.0 | 0.000 | 1.000 | 111 | 68 | 61.3 | 43 | 38.7 | 1.002 | 0.317 |
| No | 258 | 147 | 57.0 | 111 | 43.0 | 738 | 411 | 55.7 | 327 | 44.3 | |||||
| Current smoking | Yes | 61 | 40 | 65.6 | 21 | 34.4 | 1.845 | 0.174 | 213 | 155 | 72.8 | 58 | 27.2 | 29.653 | 0.000 |
| No | 219 | 120 | 54.8 | 99 | 45.2 | 625 | 319 | 51.0 | 306 | 49.0 | |||||
| Variables | People with Disabilities | People without Disabilities | |||||||
|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | p-Value | OR | 95% CI | p-Value | ||||
| Gender | Men | Ref | Ref | ||||||
| Women | 1.94 | 1.07 | 3.53 | 0.029 | 1.20 | 0.84 | 1.72 | 0.324 | |
| Age | 40–59 | Ref | Ref | ||||||
| 60–79 | 0.62 | 0.35 | 1.11 | 0.108 | 0.78 | 0.55 | 1.10 | 0.156 | |
| Residence area | Large city | 1.32 | 0.78 | 2.24 | 0.298 | 1.20 | 0.89 | 1.62 | 0.228 |
| Small city and rural | Ref | Ref | |||||||
| Living alone | Yes | 2.36 | 1.01 | 5.55 | 0.049 | 1.47 | 0.85 | 2.55 | 0.166 |
| No | Ref | Ref | |||||||
| Education | Less than middle school | 0.81 | 0.44 | 1.50 | 0.504 | 1.54 | 1.11 | 2.15 | 0.010 |
| More than high school | Ref | Ref | |||||||
| Current economic | Yes | Ref | Ref | ||||||
| activity | No | 1.78 | 1.04 | 3.07 | 0.037 | 1.41 | 1.02 | 1.95 | 0.039 |
| Adjusted income | 1st quintile (lowest) | 1.25 | 0.71 | 2.22 | 0.440 | 0.98 | 0.68 | 1.41 | 0.897 |
| 2nd–5th quintiles | Ref | Ref | |||||||
| Type of health | National health insurance | Ref | Ref | ||||||
| insurance | Medical aid | 0.72 | 0.34 | 1.51 | 0.383 | 0.84 | 0.39 | 1.80 | 0.648 |
| Heavy drinking | Yes | 1.68 | 0.66 | 4.29 | 0.279 | 1.28 | 0.80 | 2.03 | 0.302 |
| No | Ref | Ref | |||||||
| Current smoking | Yes | 0.80 | 0.39 | 1.61 | 0.525 | 0.46 | 0.31 | 0.68 | 0.000 |
| No | Ref | Ref | |||||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Song, Y.-L.-A.; Park, J.-H. Differences in Body Mass Index Trajectories and Their Classification, Sociodemographic Characteristics, and Health Behaviors between People with and without Disabilities Using Korea Health Panel Survey Data. Int. J. Environ. Res. Public Health 2022, 19, 2827. https://doi.org/10.3390/ijerph19052827
Song Y-L-A, Park J-H. Differences in Body Mass Index Trajectories and Their Classification, Sociodemographic Characteristics, and Health Behaviors between People with and without Disabilities Using Korea Health Panel Survey Data. International Journal of Environmental Research and Public Health. 2022; 19(5):2827. https://doi.org/10.3390/ijerph19052827
Chicago/Turabian StyleSong, Yea-Li-A, and Jae-Hyun Park. 2022. "Differences in Body Mass Index Trajectories and Their Classification, Sociodemographic Characteristics, and Health Behaviors between People with and without Disabilities Using Korea Health Panel Survey Data" International Journal of Environmental Research and Public Health 19, no. 5: 2827. https://doi.org/10.3390/ijerph19052827
APA StyleSong, Y.-L.-A., & Park, J.-H. (2022). Differences in Body Mass Index Trajectories and Their Classification, Sociodemographic Characteristics, and Health Behaviors between People with and without Disabilities Using Korea Health Panel Survey Data. International Journal of Environmental Research and Public Health, 19(5), 2827. https://doi.org/10.3390/ijerph19052827





