Psychological and Sociocultural Determinants in Childhood Asthma Disease: Impact on Quality of Life
Abstract
1. Introduction
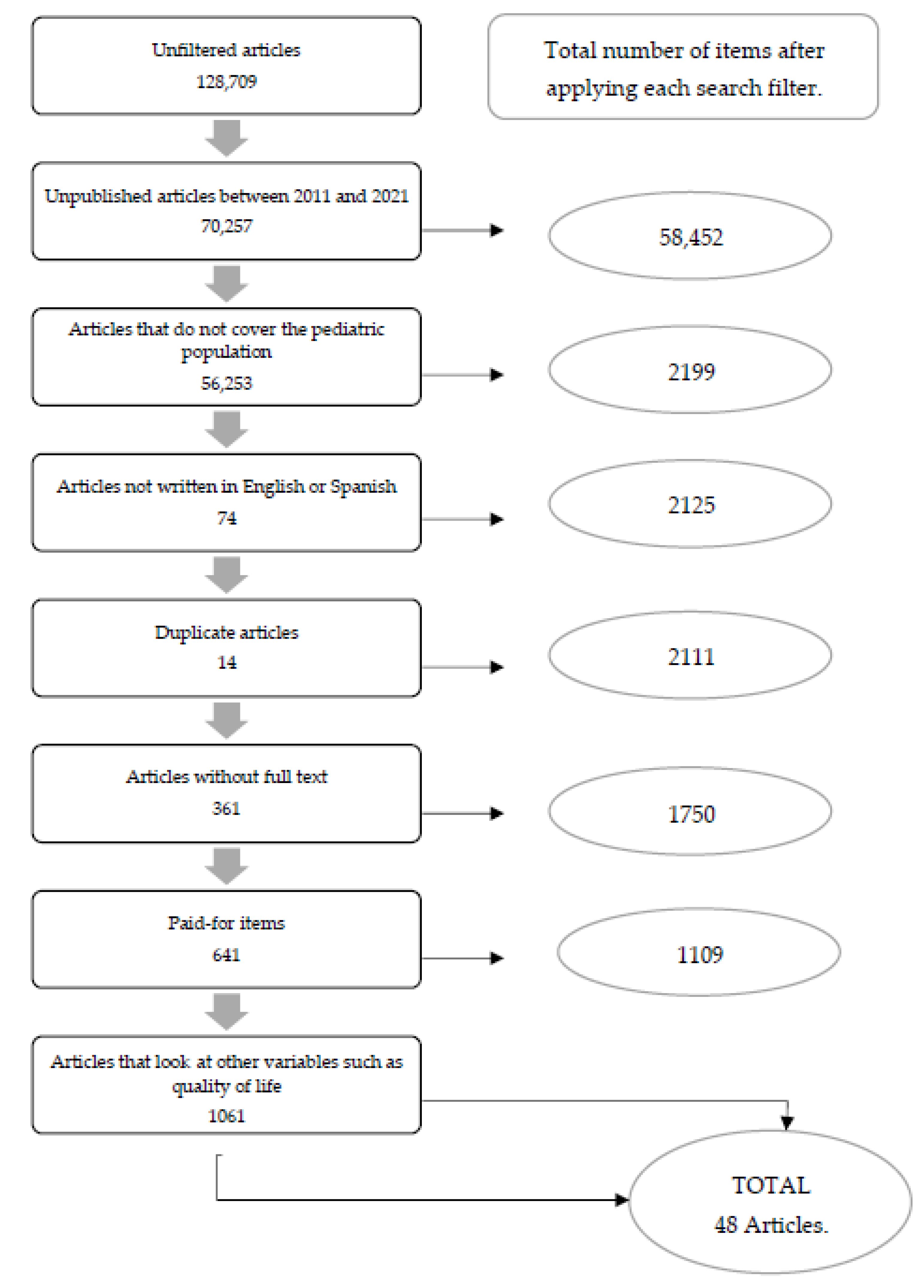
2. Methodology
3. Results
3.1. Psychological Dimension
3.1.1. Anxiety and Depression
3.1.2. ADHD
3.1.3. Personality Traits
3.1.4. Emotions and Stress
3.2. Sociocultural Dimension
3.2.1. Bullying
3.2.2. Academic Performance
3.2.3. Socioeconomic Status
3.2.4. Family and Social Relationships
3.3. Quality of Life
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| WHO | World Health Organization |
| ADHD | Attention-Deficit/Hyperactivity Disorder |
| CRP | C-reactive protein |
References
- Lacruz-Gascón, T.; Moraleda-Merino, J.; Graell-Berna, M.; Villa-Asensi, J.R.; Sepúlveda-García, A.R. Asma de inicio en la infancia: Descripción de su impacto en la personalidad y en el bienestar emocional en una muestra de mujeres adolescentes. Rev. Psicopatología Psicol. Clínica 2019, 24, 49–57. [Google Scholar] [CrossRef]
- Aktan, Z.D.; Berk, H.S.; Erdogan, F.; Öktem, S. Pediatrik Astımda Anksiyete, Depresyon, Somatizasyon ve Yaşam Kalitesi ile Serum IgE Düzeyi İlişkisi. Psikiyatr. Guncel Yaklasimlar—Curr. Approaches Psychiatry 2019, 11, 276–292. [Google Scholar] [CrossRef][Green Version]
- Secinti, E.; Thompson, E.J.; Richards, M.; Gaysina, D. Research Review: Childhood Chronic Physical Illness and Adult Emotional Health—A Systematic Review and Meta-Analysis. Available online: https://click.endnote.com/viewer?doi=10.1111%2Fjcpp.12727&token=WzMxNjMzOTcsIjEwLjExMTEvamNwcC4xMjcyNyJd.OTZ4Cra1Qo1aiH2U2zLw1vl2MaU (accessed on 25 November 2021).
- Asensi, R. Adaptación al Asma Bronquial en Pediatría: Ansiedad y Bienestar Psicológico. Rev. Psicol. Salud. 2019, 7, 20. Available online: https://dialnet.unirioja.es/servlet/articulo?codigo=6825034 (accessed on 25 November 2021).
- Ballardini, N.; Kramer, M.S.; Oken, E.; Henderson, A.J.; Bogdanovich, N.; Dahhou, M.; Patel, R.; Thompson, J.; Vilchuck, K.; Yang, S.; et al. Associations of atopic dermatitis and asthma with child behaviour: Results from the PROBIT cohort. Clin. Exp. Allergy 2019, 49, 1235–1244. [Google Scholar] [CrossRef] [PubMed]
- Bhagat, D.; Fagnano, M.; Halterman, J.S.; Reznik, M. Asthma symptoms, interactive physical play and behavioral and academic outcomes in urban children with persistent asthma. J. Asthma 2018, 56, 711–718. [Google Scholar] [CrossRef]
- Boeschoten, S.A.; Dulfer, K.; Boehmer, A.L.; Merkus, P.J.F.M.; Van Rosmalen, J.; De Jongste, J.C.; De Hoog, M.; Buysse, C.M.; the Dutch collaborative PICU research network (SKIC) * A complete list of research network participants is provided in the acknowledgments. Quality of life and psychosocial outcomes in children with severe acute asthma and their parents. Pediatr. Pulmonol. 2020, 55, 2883–2892. [Google Scholar] [CrossRef]
- Bronstein, C. ‘I am not crying. I am rubbing my eyes’: Annie and the hollow object. J. Child Psychother. 2014, 40, 135–149. [Google Scholar] [CrossRef]
- Chang, H.Y.; Seo, J.-H.; Kim, H.Y.; Kwon, J.-W.; Kim, B.-J.; Bin Kim, H.; Lee, S.-Y.; Jang, G.C.; Song, D.J.; Kim, W.K.; et al. Allergic Diseases in Preschoolers Are Associated with Psychological and Behavioural Problems. Allergy Asthma Immunol. Res. 2013, 5, 315–321. Available online: https://e-aair.org/DOIx.php?id=10.4168/aair.2013.5.5.315 (accessed on 25 November 2021). [CrossRef]
- Cheetham, T.J.; Turner-Cobb, J.M.; Gamble, T. Children’s implicit understanding of the stress-illness link: Testing development of health cognitions. Br. J. Health Psychol. 2016, 21, 781–795. [Google Scholar] [CrossRef]
- Chen, E.; Strunk, R.C.; Trethewey, A.; Schreier, H.M.; Maharaj, N.; Miller, G.E. Resilience in low-socioeconomic-status children with asthma: Adaptations to stress. J. Allergy Clin. Immunol. 2011, 128, 970–976. [Google Scholar] [CrossRef]
- Chen, M.-H.; Su, T.-P.; Chen, Y.-S.; Hsu, J.-W.; Huang, K.-L.; Chang, W.-H.; Chen, T.-J.; Bai, Y.-M. Asthma and attention-deficit/hyperactivity disorder: A nationwide population-based prospective cohort study. J. Child Psychol. Psychiatry 2013, 54, 1208–1214. [Google Scholar] [CrossRef]
- Connett, G.J.; Thomas, M. Dysfunctional Breathing in Children and Adults with Asthma. Front. Pediatr. 2018, 6, 406. [Google Scholar] [CrossRef]
- Cutuli, J.J.; Herbers, J.E.; Lafavor, T.L.; Ahumada, S.M.; Masten, A.S.; Oberg, C.N. Asthma and Adaptive Functioning among Homeless Kindergarten-Aged Children in Emergency Housing. J. Health Care Poor Underserved 2014, 25, 717–730. [Google Scholar] [CrossRef] [PubMed]
- Sollander, S.E.; Fabian, H.; Sarkadi, A.; Salari, R.; Fält, E.; Dahlberg, A.; Feldman, I.; Durbeej, N. Asthma and allergies correlate with mental health problems in preschool children. Acta Paediatr. 2020, 110, 1601–1609. [Google Scholar] [CrossRef] [PubMed]
- Farrell, A.K.; Slatcher, R.B.; Tobin, E.T.; Imami, L.; Wildman, D.; Luca, F.; Zilioli, S. Socioeconomic status, family negative emotional climate, and anti-inflammatory gene expression among youth with asthma. Psychoneuroendocrinology 2018, 91, 62–67. [Google Scholar] [CrossRef] [PubMed]
- Hammer-Helmich, L.; Linneberg, A.; Obel, C.; Thomsen, S.F.; Møllehave, L.T.; Glümer, C. Mental health associations with eczema, asthma and hay fever in children: A cross-sectional survey. BMJ Open 2016, 6, e012637. [Google Scholar] [CrossRef]
- Henrríquez, H.; Paola, C. Competencias Socioemocionales Como Factor Protector ante el Desarrollo de Síndromes Internalizantes y Externalizantes en los Adolescentes Víctimas del Conflicto Armado. Master’s Thesis, Universidad del Norte, Barranquilla, Colombia, 2016. [Google Scholar]
- Hsu, C.Y.; Lehman, H.K.; Wood, B.L.; Benipal, J.; Humayun, Q.; Miller, B.D. Comorbid Obesity and Depressive Symptoms in Childhood Asthma: A Harmful Synergy. J. Allergy Clin. Immunol. Pract. 2020, 8, 2689–2697. [Google Scholar] [CrossRef]
- Imami, B.L.; Tobin, M.E.T.; Kane, H.S.; Saleh, B.D.J.; Lupro, B.T.H.; Slatcher, R.B. Effects of Socioeconomic Status on Maternal and Child Positive Behaviors in Daily Life Among Youth with Asthma. J. Pediatr. Psychol. 2014, 40, 55–65. [Google Scholar] [CrossRef][Green Version]
- Kansen, H.M.; Le, T.; Meijer, Y.; Uiterwaal, C.S.P.M.; Knulst, A.C.; van der Ent, C.K.; van Erp, F.C. Perceived triggers of asthma impair quality of life in children with asthma. Clin. Exp. Allergy 2019, 49, 980–989. [Google Scholar] [CrossRef]
- Kelo, M.; Eriksson, E.; Eriksson, I. Perceptions of patient education during hospital visit-described by school-age children with a chronic illness and their parents. Scand. J. Caring Sci. 2012, 27, 894–904. [Google Scholar] [CrossRef]
- Kouzegaran, S.; Samimi, P.; Ahanchian, H.; Khoshkhui, M.; Behmanesh, F. Quality of Life in Children with Asthma versus Healthy Children. Open Access Maced. J. Med. Sci. 2018, 6, 1413–1418. [Google Scholar] [CrossRef] [PubMed]
- Agnafors, S.; Kjellström, A.N.; Torgerson, J.; Rusner, M. Somatic comorbidity in children and adolescents with psychiatric disorders. Eur. Child Adolesc. Psychiatry 2019, 28, 1517–1525. [Google Scholar] [CrossRef] [PubMed]
- Lahaye, M.; Van Broeck, N.; Bodart, E.; Luminet, O. Predicting quality of life in pediatric asthma: The role of emotional competence and personality. Qual. Life Res. 2012, 22, 907–916. [Google Scholar] [CrossRef] [PubMed]
- Lahaye, M.; Fantini-Hauwel, C.; Van Broeck, N.; Bodart, E.; Luminet, O. Emotional competence and quality of life of children with asthma: The mediating effect of coping strategies. Psychol. Health 2011, 26, 1678–1695. Available online: https://www.tandfonline.com/doi/abs/10.1080/08870446.2011.562606 (accessed on 25 November 2021). [CrossRef]
- Layte, R.; McCrory, C. Paediatric chronic illness and educational failure: The role of emotional and behavioural problems. Soc. Psychiatry 2012, 48, 1307–1316. [Google Scholar] [CrossRef]
- Lim, J.; Wood, B.L.; Miller, B.D.; Simmens, S.J. Effects of paternal and maternal depressive symptoms on child internalizing symptoms and asthma disease activity: Mediation by interparental negativity and parenting. J. Fam. Psychol. 2011, 25, 137–146. [Google Scholar] [CrossRef]
- Lowther, H.; Newman, E.; Sharp, K.; McMurray, A. Attentional bias to respiratory- and anxiety-related threat in children with asthma. Cogn. Emot. 2015, 30, 953–967. [Google Scholar] [CrossRef]
- Lyznicki, J.M.; McCaffree, M.A.; Robinowitz, C.B. Childhood Bullying: Implications for Physicians. Am. Fam. Physician 2004, 70, 1723–1728. Available online: https://pubmed.ncbi.nlm.nih.gov/29431974/ (accessed on 25 November 2021).
- Matsunaga, N.Y.; Ribeiro, M.A.; Saad, I.A.B.; Morcillo, A.M.; Ribeiro, J.D.; Toro, A.A.D.C. Evaluation of quality of life according to asthma control and asthma severity in children and adolescents. J. Bras. Pneumol. 2015, 41, 502–508. [Google Scholar] [CrossRef]
- Mirabelli, M.C.; Hsu, J.; Gower, W.A. Comorbidities of asthma in U.S. children. Respir. Med. 2016, 116, 34–40. [Google Scholar] [CrossRef]
- Moola, F.J.; Faulkner, G.; White, L.; Kirsh, J.A. The psychological and social impact of camp for children with chronic illnesses: A systematic review update. Child Care Health Dev. 2013, 40, 615–631. [Google Scholar] [CrossRef] [PubMed]
- Nanda, M.K.; LeMasters, G.K.; Levin, L.; Rothenberg, M.E.; Assa’Ad, A.H.; Newman, N.; Bernstein, D.; Khurana-Hershey, G.; Lockey, J.E.; Ryan, P.H. Allergic Diseases and Internalizing Behaviors in Early Childhood. Pediatrics 2016, 137, e20151922. [Google Scholar] [CrossRef]
- Nicu, O.; Stasii, E. P16 The emotional state in bronchial asthma in children. Abstracts 2019, 104, A162. [Google Scholar] [CrossRef]
- Organización Mundial de la Salud. (s. f.). Asma. Who. It. Available online: https://www.who.int/es/news-room/fact-sheets/detail/asthma (accessed on 27 April 2021).
- Polizzi, C.; Fontana, V.; Carollo, A.; Bono, A.; Burgio, S.; Perricone, G. Sibship and Self-Esteem in Children with Asthma. Pediatr. Rep. 2016, 8, 21–26. [Google Scholar] [CrossRef] [PubMed]
- Raymond, K.P.; Fiese, B.H.; Winter, M.A.; Knestel, A.; Everhart, R.S. Helpful Hints: Caregiver-Generated Asthma Management Strategies and Their Relation to Pediatric Asthma Symptoms and Quality of Life. J. Pediatr. Psychol. 2012, 37, 414–423. Available online: https://academic.oup.com/jpepsy/article/37/4/414/894976 (accessed on 25 November 2021). [CrossRef][Green Version]
- Ritz, T.; Kroll, J.L.; Patel, S.V.; Chen, J.R.; Yezhuvath, U.S.; Aslan, S.; Khan, D.A.; Pinkham, A.E.; Rosenfield, D.; Brown, E.S. Central nervous system signatures of affect in asthma: Associations with emotion-induced bronchoconstriction, airway inflammation, and asthma control. J. Appl. Physiol. 2019, 126, 1725–1736. [Google Scholar] [CrossRef]
- Rodríguez, E.M.; Kumar, H.; Bearman, S.K.; von Buttlar, A.M.; Sánchez-Johnsen, L. Physician perceptions of children’s coping with asthma are associated with children’s psychosocial and disease functioning. Fam. Syst. Health 2018, 36, 327–337. [Google Scholar] [CrossRef]
- Rodriguez, E.M.; Kumar, H.; Draeger, A.; Sanchez-Johnsen, L. Coping with asthma in racially and ethnically diverse urban children: The role of emotional problems in disease control. Child. Health Care 2015, 46, 151–169. [Google Scholar] [CrossRef]
- Rosenberg, S.L.; Miller, G.E.; Brehm, J.M.; Celedón, J.C. Stress and Asthma: Novel Insights on Genetic, Epigenetic, and Immunologic Mechanisms. 2014. Available online: http://europepmc.org/backend/ptpmcrender.fcgi?accid=PMC4252392&blobtype=pdf (accessed on 25 November 2021).
- Shaikhan, F.M.; Makhlouf, M.M. Quality of life among caregivers of asthmatic children attending pulmonology clinics at Hamad General Hospital, Qatar. SAGE Open Med. 2020, 8, 2050312120973500. [Google Scholar] [CrossRef]
- Shanahan, L.; Copeland, W.E.; Worthman, C.M.; Angold, A.; Costello, E.J. Children with Both Asthma and Depression Are at Risk for Heightened Inflammation. J. Pediatr. 2013, 163, 1443–1447. [Google Scholar] [CrossRef]
- Silva, N.; Crespo, C.; Carona, C.; Bullinger, M.; Canavarro, M.C. Why the (dis)agreement? Family context and child-parent perspectives on health-related quality of life and psychological problems in paediatric asthma: Child-parent (dis)agreement on adaptation outcomes. Child Care Health Dev. 2014, 41, 112–121. [Google Scholar] [CrossRef] [PubMed]
- Stewart, M.; Masuda, J.R.; Letourneau, N.; Anderson, S.; McGhan, S. “I Want to Meet Other Kids Like Me”: Support Needs of Children with Asthma and Allergies. Issues Compr. Pediatr. Nurs. 2011, 34, 62–78. [Google Scholar] [CrossRef] [PubMed]
- Thabrew, H.; Stasiak, K.; Hetrick, S.E.; Wong, S.; Huss, J.H.; Merry, S.N. E-Health interventions for anxiety and depression in children and adolescents with long-term physical conditions. Cochrane Database Syst. Rev. 2018, 2018, CD012489. [Google Scholar] [CrossRef]
- Beltri, R.T.; Fuentes, C. Psicopatía: Una entidad clínica controvertida pero necesaria en psiquiatría forense. Rev. Española Med. Leg. 2008, 34, 25–35. [Google Scholar] [CrossRef]
- Trastornos Psicóticos. (s. f.). National Library of Medicine. Available online: https://medlineplus.gov/spanish/psychoticdisorders.html (accessed on 2 May 2021).
- Walker, V.G. Factors Related to Emotional Responses in School-aged Children Who Have Asthma. Issues Ment. Health Nurs. 2012, 33, 406–429. Available online: http://europepmc.org/backend/ptpmcrender.fcgi?accid=PMC3516871&blobtype=pdf (accessed on 25 November 2021). [CrossRef][Green Version]
- Walker, V.G. Exploration of the Influence of Factors Identified in the Literature on School-aged Children’s Emotional Responses to Asthma. J. Pediatr. Nurs. 2017, 33, 54–62. [Google Scholar] [CrossRef]
- Winter, M.A.; Fiese, B.H.; Spagnola, M.; Anbar, R.D. Asthma severity, child security, and child internalizing: Using story stem techniques to assess the meaning children give to family and disease-specific events. J. Fam. Psychol. 2011, 25, 857–867. [Google Scholar] [CrossRef]
| Inclusion Criteria | Exclusion Criteria | |
|---|---|---|
| Articles covering information from the last 10 years (2011–2021) | Articles whose sample is a pediatric population | Articles whose study population is adults or the elderly |
| Articles in English or Spanish | Articles with full text | Documents containing only abstracts |
| Articles looking at other variables such as quality of life or personality | ||
| Unfiltered Articles | Articles from 2011 to 2021 | Articles Containing Pediatric Population (0–12 Years) | Articles in English and Spanish | Duplicate Articles | Full Text Articles | Free Articles | Total Articles That Fit the Topic under Study | |
|---|---|---|---|---|---|---|---|---|
| PUBMED | 983 | 326 | 216 | 206 | 203 | 193 | 84 | 7 |
| WEB OF SCIENCE | 1653 | 601 | 409 | 380 | 377 | 348 | 150 | 12 |
| PSICODOC | 16 | 6 | 1 | 1 | 1 | 1 | 1 | 1 |
| PUBPSYCH | 648 | 159 | 158 | 146 | 146 | 145 | 45 | 7 |
| SCOPUS | 1.528 | 540 | 382 | 371 | 371 | 369 | 166 | 8 |
| SCIELO | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| PSYCINFO | 908 | 228 | 144 | 139 | 134 | 39 | 5 | 1 |
| PSYCHOLOGY AND BEHAVIORAL SCIENCES SOLLECTIONS | 5.305 | 2.237 | 240 | 240 | 239 | 234 | 234 | 7 |
| PSYCHOLOGY DATABASE (PROQUEST CENTRAL) | 108.187 | 48.794 | 404 | 401 | 399 | 234 | 234 | 3 |
| CUIDEN | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| COCHRANE | 51 | 34 | 26 | 26 | 26 | 26 | 26 | 1 |
| CINAHL | 9.430 | 5.527 | 219 | 215 | 215 | 161 | 161 | 1 |
| TOTAL | 128.709 | 58.452 | 2.199 | 2.125 | 2.111 | 1.750 | 1.109 | 48 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Plaza-González, S.; Zabala-Baños, M.d.C.; Astasio-Picado, Á.; Jurado-Palomo, J. Psychological and Sociocultural Determinants in Childhood Asthma Disease: Impact on Quality of Life. Int. J. Environ. Res. Public Health 2022, 19, 2652. https://doi.org/10.3390/ijerph19052652
Plaza-González S, Zabala-Baños MdC, Astasio-Picado Á, Jurado-Palomo J. Psychological and Sociocultural Determinants in Childhood Asthma Disease: Impact on Quality of Life. International Journal of Environmental Research and Public Health. 2022; 19(5):2652. https://doi.org/10.3390/ijerph19052652
Chicago/Turabian StylePlaza-González, Sheila, María del Carmen Zabala-Baños, Álvaro Astasio-Picado, and Jesús Jurado-Palomo. 2022. "Psychological and Sociocultural Determinants in Childhood Asthma Disease: Impact on Quality of Life" International Journal of Environmental Research and Public Health 19, no. 5: 2652. https://doi.org/10.3390/ijerph19052652
APA StylePlaza-González, S., Zabala-Baños, M. d. C., Astasio-Picado, Á., & Jurado-Palomo, J. (2022). Psychological and Sociocultural Determinants in Childhood Asthma Disease: Impact on Quality of Life. International Journal of Environmental Research and Public Health, 19(5), 2652. https://doi.org/10.3390/ijerph19052652








