Active Video Games Improve Muscular Fitness and Motor Skills in Children with Overweight or Obesity
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Outcomes
2.2.1. Anthropometry
2.2.2. Physical Activity
2.2.3. Pediatric Dynapenia
Counter Movement Jump Height
Maximal Isometric Strength
Handgrip Strength
Lean Mass
2.2.4. Motor Skills
2.3. Intervention
2.4. Statistical Analyses
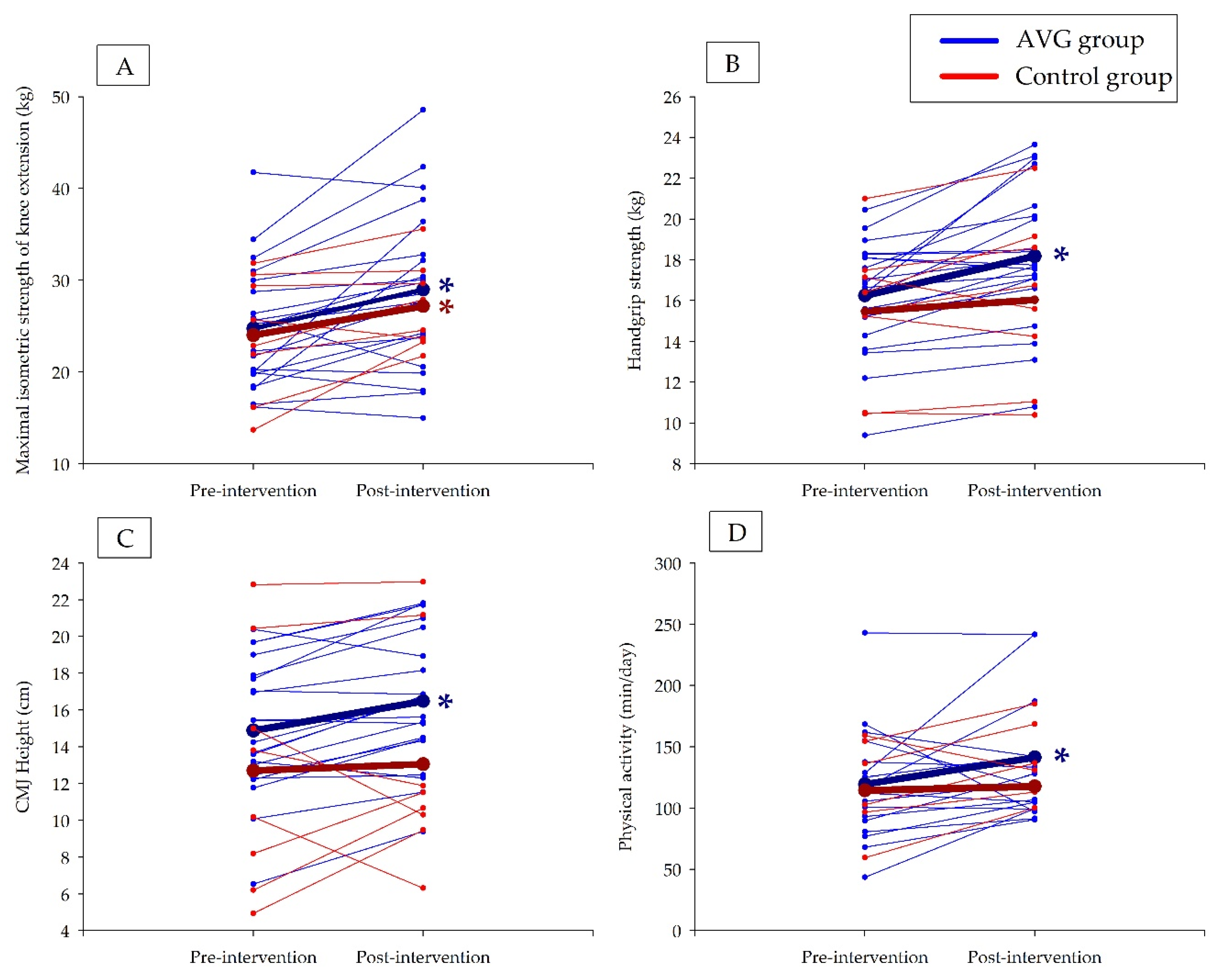
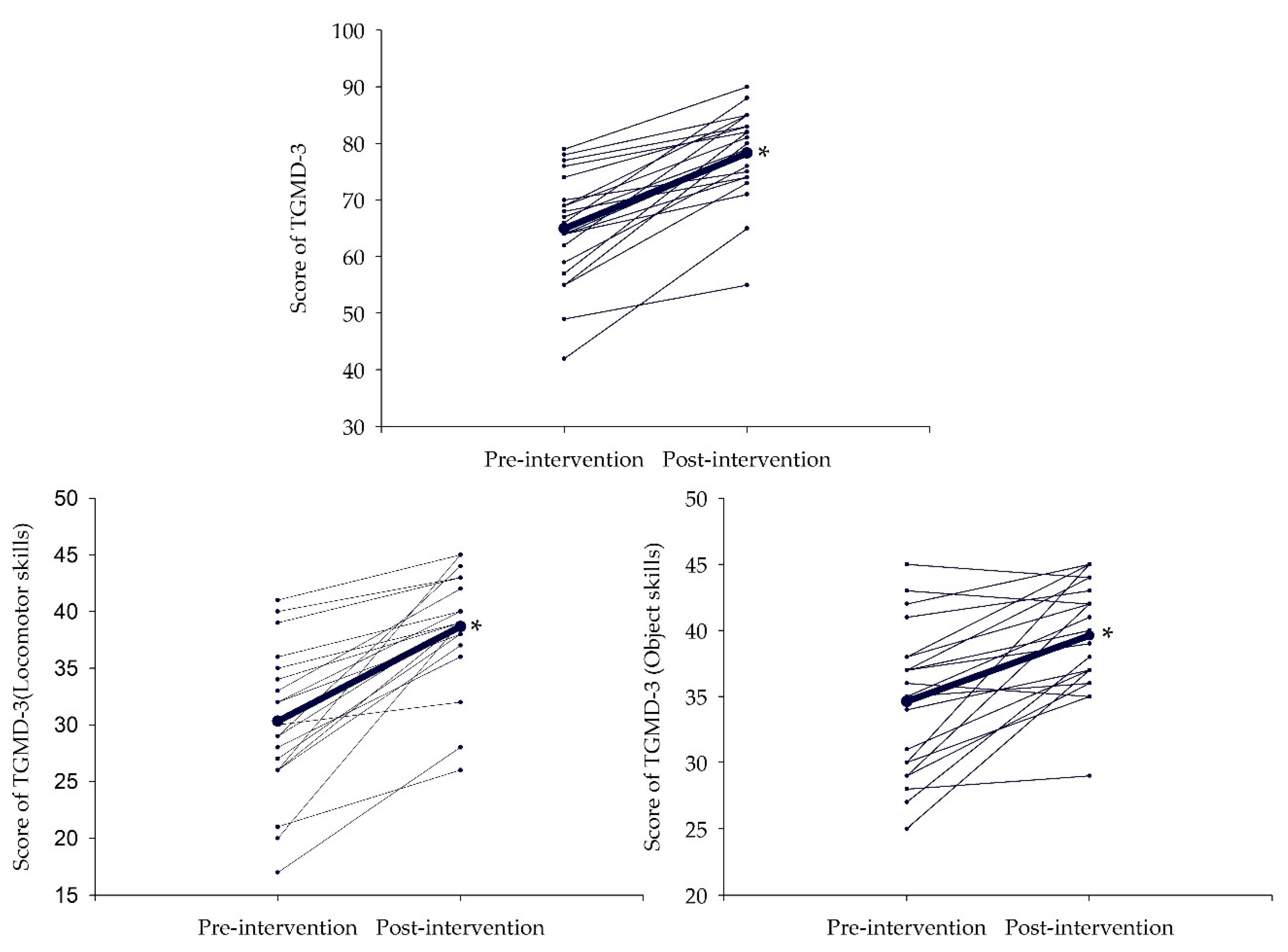
3. Results
4. Discussion
5. Limitations and Strengths
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ng, M.; Fleming, T.; Robinson, M.; Thomson, B.; Graetz, N.; Margono, C.; Mullany, E.C.; Biryukov, S.; Abbafati, C.; Abera, S.F.; et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: A systematic analysis for the Global Burden of Disease Study 2013. Lancet 2014, 384, 766–781. [Google Scholar] [CrossRef]
- World Health Organization. Obesity: Preventing and Managing the Global Epidemic; World Health Organization: Geneva, Switzerland, 2000; pp. 1–268.
- Ahluwalia, N.; Dalmasso, P.; Rasmussen, M.; Lipsky, L.; Currie, C.; Haug, E.; Kelly, C.; Damsgaard, M.T.; Due, P.; Tabak, I.; et al. Trends in overweight prevalence among 11-, 13- and 15-year-olds in 25 countries in Europe, Canada and USA from 2002 to 2010. Eur. J. Public Health 2015, 25, 28–32. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization Global Health Observatory (GHO) Data. Obesity and Overweight. Available online: https://www.who.int/gho/ncd/risk_factors/overweight_obesity/obesity_adolescents/en (accessed on 9 April 2020).
- Gasol Foundation. Estudio Pasos 2019. Physical Activity, Sedentarism and Obesity of Spanish Youth; Gasol Foundation: Geneva, Switzerland, 2019. [Google Scholar]
- Nittari, G.; Scuri, S.; Petrelli, F.; Pirillo, I.; Di Luca, N.M.; Grappasonni, I. Fighting obesity in children from European world health organization member states. Epidemiological data, medical-social aspects, and prevention programs. Clin. Ter. 2019, 170, E223–E230. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Consideration of the Evidence on Childhood Obesity for the Commission on Ending Childhood Obesity Report of the Ad Hoc Working Group on Science and Evidence for Ending Childhood Obesity; World Health Organization: Geneva, Switzerland, 2016.
- Bull, F.C.; Al-Ansari, S.S.; Biddle, S.; Borodulin, K.; Buman, M.P.; Cardon, G.; Carty, C.; Chaput, J.-P.; Chastin, S.; Chou, R.; et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br. J. Sports Med. 2020, 54, 1451–1462. [Google Scholar] [CrossRef]
- Guthold, R.; Stevens, G.A.; Riley, L.M.; Bull, F.C. Global trends in insufficient physical activity among adolescents: A pooled analysis of 298 population-based surveys with 1·6 million participants. Lancet Child Adolesc. Health 2020, 4, 23–35. [Google Scholar] [CrossRef]
- Faigenbaum, A.D.; Rial Rebullido, T.; MacDonald, J.P. Pediatric Inactivity Triad: A Risky PIT. Curr. Sports Med. Rep. 2018, 17, 45–47. [Google Scholar] [CrossRef] [PubMed]
- Micheli, L.; Mountjoy, M.; Engebretsen, L.; Hardman, K.; Kahlmeier, S.; Lambert, E.; Ljungqvist, A.; Matsudo, V.; McKay, H.; Sundberg, C.J. Fitness and health of children through sport: The context for action. Br. J. Sports Med. 2011, 45, 931–936. [Google Scholar] [CrossRef] [PubMed]
- Marin-Puyalto, J.; Mäestu, J.; Gómez-Cabello, A.; Lätt, E.; Remmel, L.; Purge, P.; Vicente-Rodríguez, G.; Jürimäe, J. Frequency and duration of vigorous physical activity bouts are associated with adolescent boys’ bone mineral status: A cross-sectional study. Bone 2019, 120, 141–147. [Google Scholar] [CrossRef] [PubMed]
- Marin-Puyalto, J.; Mäestu, J.; Gomez-Cabello, A.; Lätt, E.; Remmel, L.; Purge, P.; Casajús, J.A.; Vicente-Rodríguez, G.; Jürimäe, J. Vigorous physical activity patterns affect bone growth during early puberty in boys. Osteoporos. Int. 2018, 29, 2693–2701. [Google Scholar] [CrossRef]
- Poitras, V.J.; Gray, C.E.; Borghese, M.M.; Carson, V.; Chaput, J.P.; Janssen, I.; Katzmarzyk, P.T.; Pate, R.R.; Connor Gorber, S.; Kho, M.E.; et al. Systematic review of the relationships between objectively measured physical activity and health indicators in school-aged children and youth. Appl. Physiol. Nutr. Metab. 2016, 41, S197–S239. [Google Scholar] [CrossRef]
- Gomez-Bruton, A.; Gonzalez-Aguero, A.; Matute-Llorente, A.; Lozano-Berges, G.; Gomez-Cabello, A.; Moreno, L.A.; Casajus, J.A.; Vicente-Rodríguez, G. The muscle-bone unit in adolescent swimmers. Osteoporos. Int. 2019, 30, 1079–1088. [Google Scholar] [CrossRef] [PubMed]
- Smith, J.J.; Eather, N.; Morgan, P.J.; Plotnikoff, R.C.; Faigenbaum, A.D.; Lubans, D.R. The health benefits of muscular fitness for children and adolescents: A systematic review and meta-analysis. Sport. Med. 2014, 44, 1209–1223. [Google Scholar] [CrossRef] [PubMed]
- Garcia-Vicencio, S.; Coudeyre, E.; Kluka, V.; Cardenoux, C.; Jegu, A.G.; Fourot, A.V.; Ratel, S.; Martin, V. The bigger, the stronger? Insights from muscle architecture and nervous characteristics in obese adolescent girls. Int. J. Obes. 2016, 40, 245–251. [Google Scholar] [CrossRef] [PubMed]
- Tomlinson, D.J.; Erskine, R.M.; Morse, C.I.; Winwood, K.; Onambélé-Pearson, G. The impact of obesity on skeletal muscle strength and structure through adolescence to old age. Biogerontology 2016, 17, 467–483. [Google Scholar] [CrossRef] [PubMed]
- Tsiros, M.D.; Coates, A.M.; Howe, P.R.C.; Grimshaw, P.N.; Buckley, J.D. Obesity: The new childhood disability? Obes. Rev. 2011, 12, 26–36. [Google Scholar] [CrossRef]
- Ervin, R.B.; Fryar, C.D.; Wang, C.Y.; Miller, I.M.; Ogden, C.L. Strength and body weight in US children and adolescents. Pediatrics 2014, 134, e782–e789. [Google Scholar] [CrossRef]
- Moliner-Urdiales, D.; Ruiz, J.R.; Vicente-Rodriguez, G.; Ortega, F.B.; Rey-Lopez, J.P.; España-Romero, V.; Casajús, J.A.; Molnar, D.; Widhalm, K.; Dallongeville, J.; et al. Associations of muscular and cardiorespiratory fitness with total and central body fat in adolescents: The HELENA study. Br. J. Sports Med. 2011, 45, 101–108. [Google Scholar] [CrossRef]
- Garcia-Pastor, T.; Salinero, J.J.; Sanz-Frias, D.; Pertusa, G.; Del Coso, J. Body fat percentage is more associated with low physical fitness than with sedentarism and diet in male and female adolescents. Physiol. Behav. 2016, 165, 166–172. [Google Scholar] [CrossRef]
- Herda, T.J.; Ryan, E.D.; Kohlmeier, M.; Trevino, M.A.; Gerstner, G.R.; Roelofs, E.J. Examination of muscle morphology and neuromuscular function in normal weight and overfat children aged 7–10 years. Scand. J. Med. Sci. Sports 2018, 28, 2310–2321. [Google Scholar] [CrossRef]
- Moliner-Urdiales, D.; Ruiz, J.R.; Ortega, F.B.; Jiménez-Pavón, D.; Vicente-Rodriguez, G.; Rey-López, J.P.; Martínez-Gómez, D.; Casajús, J.A.; Mesana, M.I.; Marcos, A.; et al. Secular trends in health-related physical fitness in Spanish adolescents: The AVENA and HELENA Studies. J. Sci. Med. Sport 2010, 13, 584–588. [Google Scholar] [CrossRef] [PubMed]
- Han, A.; Fu, A.; Cobley, S.; Sanders, R.H. Effectiveness of exercise intervention on improving fundamental movement skills and motor coordination in overweight/obese children and adolescents: A systematic review. J. Sci. Med. Sport 2018, 21, 89–102. [Google Scholar] [CrossRef] [PubMed]
- Bardid, F.; De Meester, A.; Tallir, I.; Cardon, G.; Lenoir, M.; Haerens, L. Configurations of actual and perceived motor competence among children: Associations with motivation for sports and global self-worth. Hum. Mov. Sci. 2016, 50, 1–9. [Google Scholar] [CrossRef]
- De Meester, A.; Maes, J.; Stodden, D.; Cardon, G.; Goodway, J.; Lenoir, M.; Haerens, L. Identifying profiles of actual and perceived motor competence among adolescents: Associations with motivation, physical activity, and sports participation. J. Sports Sci. 2016, 34, 2027–2037. [Google Scholar] [CrossRef] [PubMed]
- Lubans, D.R.; Morgan, P.J.; Cliff, D.P.; Barnett, L.M. Fundamental Movement Skills in Children and Adolescents. Sport Med. 2010, 40, 1019–1035. [Google Scholar] [CrossRef]
- Engel, A.C.; Broderick, C.R.; van Doorn, N.; Hardy, L.L.; Parmenter, B.J. Exploring the Relationship Between Fundamental Motor Skill Interventions and Physical Activity Levels in Children: A Systematic Review and Meta-analysis. Sport Med. 2018, 48, 1845–1857. [Google Scholar] [CrossRef] [PubMed]
- Thompson, W.R. Worldwide Survey of Fitness Trends for 2021. ACSM’s Health Fit. J. 2020, 25, 10–19. [Google Scholar] [CrossRef]
- Benzing, V.; Schmidt, M. Exergaming for Children and Adolescents: Strengths, Weaknesses, Opportunities and Threats. J. Clin. Med. 2018, 7, 422. [Google Scholar] [CrossRef] [PubMed]
- Comeras-Chueca, C.; Villalba-Heredia, L.; Pérez-Llera, M.; Lozano-Berges, G.; Marín-Puyalto, J.; Vicente-Rodríguez, G.; Matute-Llorente, Á.; Casajús, J.A.J.A.J.A.; González-Agüero, A. Assessment of active video games’ energy expenditure in children with overweight and obesity and differences by gender. Int. J. Environ. Res. Public Health 2020, 17, 6714. [Google Scholar] [CrossRef]
- Lamboglia, C.M.G.F.; da Silva, V.T.B.L.; de Vasconcelos Filho, J.E.; Pinheiro, M.H.N.P.; da Munguba, M.C.S.; Silva Júnior, F.V.I.; de Paula, F.A.R.; da Silva, C.A.B. Exergaming as a Strategic Tool in the Fight against Childhood Obesity: A Systematic Review. J. Obes. 2013, 2013, 438364. [Google Scholar] [CrossRef][Green Version]
- Gao, Z.; Chen, S.; Pasco, D.; Pope, Z. A meta-analysis of active video games on health outcomes among children and adolescents. Obes. Rev. 2015, 16, 783–794. [Google Scholar] [CrossRef]
- Mack, I.; Bayer, C.; Schäffeler, N.; Reiband, N.; Brölz, E.; Zurstiege, G.; Fernandez-Aranda, F.; Gawrilow, C.; Zipfel, S. Chances and Limitations of Video Games in the Fight against Childhood Obesity—A Systematic Review. Eur. Eat. Disord. Rev. 2017, 25, 237–267. [Google Scholar] [CrossRef] [PubMed]
- Gao, Z.; Zeng, N.; McDonough, D.J.; Su, X. A Systematic Review of Active Video Games on Youth’s Body Composition and Physical Activity. Int. J. Sports Med. 2020, 41, 561–573. [Google Scholar] [CrossRef]
- Gao, Z.; Chen, S. Are field-based exergames useful in preventing childhood obesity? A systematic review. Int. Assoc. Study Obes. 2014, 15, 676–691. [Google Scholar] [CrossRef] [PubMed]
- Kari, T. Promoting Physical Activity and Fitness with Exergames. In Transforming Gaming and Computer Simulation Technologies across Industries; IGI Global: Jyvaskyla, Finland, 2016. [Google Scholar]
- Kari, T. Can exergaming promote physical fitness and physical activity? Int. J. Gaming Comput. Simul. 2014, 6, 59–77. [Google Scholar] [CrossRef]
- Liang, Y.; Lau, P.W.C. Effects of active videogames on physical activity and related outcomes among healthy children: A systematic review. Games Health J. 2014, 3, 122–144. [Google Scholar] [CrossRef]
- De Medeirosa, P.; Capistranoa, R.; Almeida, M.; Aparecida, S.; Silva, T.; Cardoso, F. Exergames as a tool for the acquisition and development of motor skills and abilities: A systematic review. Rev. Paul. Pediatr. 2017, 35, 464–471. [Google Scholar]
- Chen, H.; Sun, H. Effects of Active Videogame and Sports, Play, and Active Recreation for Kids Physical Education on Children’s Health-Related Fitness and Enjoyment. Games Health J. 2017, 6, 312–318. [Google Scholar] [CrossRef] [PubMed]
- Foley, L.; Jiang, Y.; Ni Mhurchu, C.; Jull, A.; Prapavessis, H.; Rodgers, A.; Maddison, R.; Mhurchu, C.N.; Jull, A.; Prapavessis, H.; et al. The effect of active video games by ethnicity, sex and fitness: Subgroup analysis from a randomised controlled trial. Int. J. Behav. Nutr. Phys. Act. 2014, 11, S66–S67. [Google Scholar] [CrossRef]
- World Medical Association. World Medical Association Declaration of Helsinki, Ethical Principles for Scientific Requirements and Research Protocols. Bull. World Health Organ. 2013, 79, 373. [Google Scholar]
- Assembly, W.M.A.G.; Assembly, W.M.A.G.; Declaration, T.; Declaration, T.; Databases, H.; Declaration, T.; Database, H. Annexe 2. WMA Declaration of Taipei on ethical considerations regarding health databases and biobanks. J. Int. Bioéthique D’éthique Des. Sci. 2017, 28, 113. [Google Scholar] [CrossRef]
- Cole, T.J.; Bellizzi, M.C.; Flegal, K.M.; Dietz, W.H. Establishing a standard definition for child overweight and obesity worldwide: International survey. Br. Med. J. 2000, 320, 1240. [Google Scholar] [CrossRef] [PubMed]
- Esliger, D.W.; Rowlands, A.V.; Hurst, T.L.; Catt, M.; Murray, P.; Eston, R.G. Validation of the GENEA Accelerometer. Accelerometer. Med. Sei. Sport. Exerc. 2011, 43, 1085–1093. [Google Scholar] [CrossRef] [PubMed]
- Trost, S.G.; Pate, R.R.; Freedson, P.S.; Sallis, J.F.; Taylor, W.C. Using objective physical activity measures with youth: How many days of monitoring are needed? Med. Sci. Sports Exerc. 2000, 32, 426–431. [Google Scholar] [CrossRef] [PubMed]
- Van Hees, V.T.; Renström, F.; Wright, A.; Gradmark, A.; Catt, M.; Chen, K.Y.; Löf, M.; Bluck, L.; Pomeroy, J.; Wareham, N.J.; et al. Estimation of daily energy expenditure in pregnant and Non-Pregnant women using a Wrist-Worn Tri-Axial accelerometer. PLoS ONE 2011, 6, e22922. [Google Scholar] [CrossRef] [PubMed]
- Schaefer, C.A.; Nigg, C.R.; Hill, J.O.; Brink, L.A.; Browning, R.C. Establishing and evaluating wrist cutpoints for the GENEActiv accelerometer in youth. Med. Sci. Sports Exerc. 2014, 46, 826–833. [Google Scholar] [CrossRef] [PubMed]
- Focke, A.; Strutzenberger, G.; Jekauc, D.; Worth, A.; Woll, A.; Schwameder, H. Effects of age, sex and activity level on counter-movement jump performance in children and adolescents. Eur. J. Sport Sci. 2013, 13, 518–526. [Google Scholar] [CrossRef]
- Asmussen, E.; Bonde-Petersen, F. Storage of Elastic Energy in Skeletal Muscles in Man. Acta Physiol. Scand. 1974, 91, 385–392. [Google Scholar] [CrossRef] [PubMed]
- Beenakker, E.A.C.; Van Der Hoeven, J.H.; Fock, J.M.; Maurits, N.M. Reference values of maximum isometric muscle force obtained in 270 children aged 4–16 years by hand-held dynamometry. Neuromuscul. Disord. 2001, 11, 441–446. [Google Scholar] [CrossRef]
- Tomkinson, G.R.; Carver, K.D.; Atkinson, F.; Daniell, N.D.; Lewis, L.K.; Fitzgerald, J.S.; Lang, J.J.; Ortega, F.B. European normative values for physical fitness in children and adolescents aged 9–17 years: Results from 2 779 165 Eurofit performances representing 30 countries. Br. J. Sports Med. 2018, 52, 1445–1456. [Google Scholar] [CrossRef]
- Gracia-Marco, L.; Ortega, F.B.; Jiménez-Pavón, D.; Rodríguez, G.; Castillo, M.J.; Vicente-Rodríguez, G.; Moreno, L.A. Adiposity and bone health in Spanish adolescents. The HELENA study. Osteoporos. Int. 2012, 23, 937–947. [Google Scholar] [CrossRef]
- Weber, D.R.; Moore, R.H.; Leonard, M.B.; Zemel, B.S. Fat and lean BMI reference curves in children and adolescents and their utility in identifying excess adiposity compared with BMI and percentage body fat. Am. J. Clin. Nutr. 2013, 98, 49–56. [Google Scholar] [CrossRef]
- Webster, E.K.; Ulrich, D.A. Evaluation of the psychometric properties of the Test of Gross Motor Development-third edition. J. Mot. Learn. Dev. 2017, 5, 45–58. [Google Scholar] [CrossRef]
- Ultrich, D.; Webster, K. Test of Gross Motor Development—3rd edition (TGMD-3). Available online: https://sites.google.com/a/umich.edu/tgmd-3/home (accessed on 1 June 2020).
- Ulrich, D.A. Test of Gross Motor Development: Examiner’s Manual, 3rd ed.; Pro-ED: Austin, TX, USA, 2019. [Google Scholar]
- Fritz, C.O.; Morris, P.E.; Richler, J.J. Effect size estimates: Current use, calculations, and interpretation. J. Exp. Psychol. Gen. 2012, 141, 2–18. [Google Scholar] [CrossRef] [PubMed]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences; Academic Press: Cambridge, MA, USA, 2013. [Google Scholar]
- Calcaterra, V.; Larizza, D.; Codrons, E.; De Silvestri, A.; Brambilla, P.; Abela, S.; Arpesella, M.; Vandoni, M. Improved metabolic and cardiorespiratory fitness during a recreational training program in obese children. J. Pediatr. Endocrinol. Metab. 2013, 26, 271–276. [Google Scholar] [CrossRef]
- Duman, F.; Kokaçya, M.H.; Doğru, E.; Katayıfcı, N.; Canbay, Ö.; Aman, F. The role of active video-accompanied exercises in improvement of the obese state in children: A prospective study from Turkey. JCRPE J. Clin. Res. Pediatr. Endocrinol. 2016, 8, 334–340. [Google Scholar] [CrossRef]
- Huang, H.-H.; Cook, L.; Harrison, J.; O’keefe, N.; Schultz, K.; Curtis, D.A. Exercise by playing active video gaming in overweight and obese children. J. Phys. Ther. Sport Med. 2017, 1, 3. [Google Scholar] [CrossRef]
- Maddison, R.; Foley, L.; Ni Mhurchu, C.; Jiang, Y.; Jull, A.; Prapavessis, H.; Hohepa, M.; Rodgers, A. Effects of active video games on body composition: A randomized controlled trial. Am. J. Clin. Nutr. 2011, 94, 156–163. [Google Scholar] [CrossRef] [PubMed]
- Adamo, K.B.; Rutherford, J.A.; Goldfield, G.S. Effects of interactive video game cycling on overweight and obese adolescent health. Appl. Physiol. Nutr. Metab. 2010, 35, 805–815. [Google Scholar] [CrossRef]
- Staiano, A.E.; Marker, A.M.; Beyl, R.A.; Hsia, D.S.; Katzmarzyk, P.T.; Newton, R.L. A randomized controlled trial of dance exergaming for exercise training in overweight and obese adolescent girls. Pediatr. Obes. 2017, 12, 120–128. [Google Scholar] [CrossRef]
- Staiano, A.E.; Beyl, R.A.; Guan, W.; Hendrick, C.A.; Hsia, D.S.; Newton, R.L. Home-based exergaming among children with overweight and obesity: A randomized clinical trial. Pediatr. Obes. 2018, 13, 724–733. [Google Scholar] [CrossRef]
- Kuzik, N.; Carson, V.; Andersen, L.B.; Sardinha, L.B.; Grøntved, A.; Hansen, B.H.; Ekelund, U. Physical Activity and Sedentary Time Associations with Metabolic Health Across Weight Statuses in Children and Adolescents. Obesity 2017, 25, 1762–1769. [Google Scholar] [CrossRef] [PubMed]
- Santos, A.; Silva-Santos, S.; Duncan, M.; Lagoa, M.J.; Vale, S.; Mota, J. Relationship among changes in sedentary time, physical activity, and body mass index in young schoolchildren: A 3-year longitudinal study. Pediatr. Exerc. Sci. 2018, 30, 426–432. [Google Scholar] [CrossRef] [PubMed]
- LeBlanc, A.G.; Chaput, J.P.; McFarlane, A.; Colley, R.C.; Thivel, D.; Biddle, S.J.H.; Maddison, R.; Leatherdale, S.T.; Tremblay, M.S. Active Video Games and Health Indicators in Children and Youth: A Systematic Review. PLoS ONE 2013, 8, e65351. [Google Scholar] [CrossRef]
- Peng, W.; Lin, J.-H.H.; Crouse, J. Is playing exergames really exercising? A meta-analysis of energy expenditure in active video games. Cyberpsychol. Behav. Soc. Netw. 2011, 14, 681–688. [Google Scholar] [CrossRef]
- Biddiss, E.; Irwin, J. Active Video Games to Promote Physical Activity in Children and Youth A Systematic Review. Arch Pediatr Adolesc. Med. 2010, 164, 664–672. [Google Scholar] [CrossRef]
- Sween, J.; Wallington, S.F.; Sheppard, V.; Taylor, T.; Llanos, A.A.; Adams-Campbell, L.L. The role of exergaming in improving physical activity: A review. J. Phys. Act. Health 2014, 11, 864–870. [Google Scholar] [CrossRef]
- Oliveira, C.B.; Pinto, R.Z.; Saraiva, B.T.C.C.; Tebar, W.R.; Delfino, L.D.; Franco, M.R.; Silva, C.C.M.M.; Christofaro, D.G.D.D. Effects of active video games on children and adolescents: A systematic review with meta-analysis. Scand. J. Med. Sci. Sports 2020, 30, 4–12. [Google Scholar] [CrossRef]
- Van Biljon, A.; Longhurst, G.K. The influence of exergaming on the functional fitness in overweight and obese children. Recreat. Danc. 2012, 18, 984–991. [Google Scholar]
- Argarini, R.; Herawati, L.; Irwadi, I.; Arum Cahyaning Putri, E.; Meinar Sari, G. Fundamental Movement Skill Approach to Combat Childhood Obesity in Surabaya, Indonesia: Potential Effects of Video Games Based Exercises (Exergaming). Talent Dev. Excell. 2020, 12, 3026–3034. [Google Scholar]
- Barnett, L.M.; Lai, S.K.; Veldman, S.L.C.; Hardy, L.L.; Cliff, D.P.; Morgan, P.J.; Zask, A.; Lubans, D.R.; Shultz, S.P.; Ridgers, N.D.; et al. Correlates of Gross Motor Competence in Children and Adolescents: A Systematic Review and Meta-Analysis. Sport Med. 2016, 46, 1663–1688. [Google Scholar] [CrossRef]
- Jaakkola, T.; Yli-Piipari, S.; Huotari, P.; Watt, A.; Liukkonen, J. Fundamental movement skills and physical fitness as predictors of physical activity: A 6-year follow-up study. Scand. J. Med. Sci. Sport 2016, 26, 74–81. [Google Scholar] [CrossRef]
- Lai, S.K.; Costigan, S.A.; Morgan, P.J.; Lubans, D.R.; Stodden, D.F.; Salmon, J.; Barnett, L.M. Do school-based interventions focusing on physical activity, fitness, or fundamental movement skill competency produce a sustained impact in these outcomes in children and adolescents? A systematic review of follow-up studies. Sport Med. 2014, 44, 67–79. [Google Scholar] [CrossRef]
- Cattuzzo, M.T.; dos Santos Henrique, R.; Ré, A.H.N.; de Oliveira, I.S.; Melo, B.M.; de Sousa Moura, M.; de Araújo, R.C.; Stodden, D. Motor competence and health related physical fitness in youth: A systematic review. J. Sci. Med. Sport 2016, 19, 123–129. [Google Scholar] [CrossRef]
- Stricker, P.R.; Faigenbaum, A.D.; McCambridge, T.M. Resistance training for children and adolescents. Pediatrics 2020, 145, e20201011. [Google Scholar] [CrossRef]
- Grainger, F.; Innerd, A.; Graham, M.; Wright, M. Integrated Strength and Fundamental Movement Skill Training in Children: A Pilot Study. Children 2020, 7, 161. [Google Scholar] [CrossRef]
- Behan, S.; Belton, S.; Peers, C.; O’Connor, N.E.; Issartel, J. Exploring the relationships between fundamental movement skills and health related fitness components in children. Eur. J. Sport Sci. 2020, 17, 1–11. [Google Scholar] [CrossRef]
| Variable | Time | All (n = 29) | AVG Group (n = 21) | Control Group (n = 8) | ||||
|---|---|---|---|---|---|---|---|---|
| Mean ± SD | Mean ± SD | Effect Size r | p Value | Mean ± SD | Effect Size r | p Value | ||
| Age (years) | 1 | 10.1 ± 0.8 | 10.2 ± 0.8 | 0.88 | <0.001 | 9.7 ± 0.8 | 0.89 | 0.012 |
| 2 | 10.7 ± 0.8 * | 10.8 ± 0.8 * | 10.5 ± 0.8 * | |||||
| Weight (kg) | 1 | 53.4 ± 8.9 | 55.3 ± 8.8 | 0.74 | 0.001 | 48.2 ± 7.2 | 0.84 | 0.017 |
| 2 | 56.3 ± 9.8 * | 57.7 ± 9.5 * | 52.5 ± 10.3 * | |||||
| Height (cm) | 1 | 144.7 ± 7.5 | 146.0 ± 6.7 | 0.88 | <0.001 | 141.1 ± 8.8 | 0.89 | 0.012 |
| 2 | 148.9 ± 7.4 * | 149.6 ± 7.1 * | 147.0 ± 8.3 * | |||||
| BMI (kg/m2) | 1 | 25.4 ± 2.7 | 25.9 ± 2.9 | 0.15 | 0.498 | 24.1 ± 1.7 | <0.00 | 0.990 |
| 2 | 25.3 ± 3.0 | 25.7 ± 3.0 | 24.1 ± 2.8 | |||||
| BMI Z-Score | 1 | 1.96 ± 0.33 | 1.99 ± 0.36 | 0.71 | 0.001 | 1.89 ± 0.18 | 0.54 | 0.123 |
| 2 | 1.84 ± 0.38 * | 1.89 ± 0.41 | 1.72 ± 0.28 | |||||
| BMI percentile | 1 | 96.8 ± 2.1 | 96.9 ± 2.35 | 0.42 | 0.053 | 96.6 ± 1.4 | 0.59 | 0.093 |
| 2 | 95.7 ± 4.0 * | 95.9 ± 4.5 | 95.1 ± 2.5 | |||||
| Variable | Time | AVG Group (n = 21) | Control Group (n = 8) | AVG Group | Control Group | ||||
|---|---|---|---|---|---|---|---|---|---|
| Change | Effect Size r | p Value | Change | Effect Size r | p Value | ||||
| Mean ± SD | Mean ± SD | ||||||||
| Knee extension maximal isometric strength (kg) | 1 | 24.8 ± 6.6 | 24.0 ± 6.7 | 4.2 ± 5.7 * | 0.66 | 0.003 | 3.2 ± 3.7 * | 0.74 | 0.036 |
| 2 | 29.0 ± 8.8 | 27.2 ± 4.7 | |||||||
| Knee extension maximal isometric strength relative to body weight (kg/body weight in kg) | 1 | 0.46 ± 0.13 | 0.50 ± 0.12 | 0.05 ± 0.10 * | 0.47 | 0.030 | 0.03 ± 0.11 | 0.15 | 0.674 |
| 2 | 0.51 ± 0.15 | 0.53 ± 0.08 | |||||||
| Knee extension maximal isometric strength Z-Score | 1 | 0.24 ± 1.36 | 0.46 ± 1.07 | 0.52 ± 1.38 | 0.39 | 0.073 | 0.14 ± 0.98 | 0.30 | 0.401 |
| 2 | 0.76 ± 2.04 | 0.59 ± 1.17 | |||||||
| Knee extension maximal isometric strength Z-Score | 1 | 0.24 ± 1.36 | 0.46 ± 1.07 | 0.52 ± 1.38 | 0.39 | 0.073 | 0.14 ± 0.98 | 0.30 | 0.401 |
| 2 | 0.76 ± 2.04 | 0.59 ± 1.17 | |||||||
| Hand-grip strength (kg) | 1 | 16.3 ± 2.6 | 15.5 ± 3.6 | 1.93 ± 1.93 * | 0.82 | <0.001 | 0.57 ± 1.40 | 0.35 | 0.327 |
| 2 | 18.2 ± 3.4 | 16.0 ± 4.1 | |||||||
| Hand-grip strength relative to body weight (kg/body weight in kg) | 1 | 0.30 ± 0.05 | 0.32 ± 0.06 | 0.02 ± 0.03 * | 0.65 | 0.003 | −0.02 ± 0.03 | 0.45 | 0.208 |
| 2 | 0.32 ± 0.53 | 0.31 ± 0.05 | |||||||
| Percentile of hand-grip strength | 1 | 45.5 ± 24.0 | 43.8 ± 19.2 | 3.3 ± 18.8 | 0.13 | 0.544 | −5.0 ± 16.9 | 0.23 | 0.516 |
| 2 | 48.8 ± 24.7 | 38.8 ± 23.6 | |||||||
| CMJ (cm) | 1 | 14.9 ± 3.6 | 16.1 ± 4.6 | 1.6 ± 1.5 * | 0.73 | 0.001 | 0.2 ± 2.5 | 0.10 | 0.779 |
| 2 | 16.5 ± 3.6 | 16.3 ± 4.1 | |||||||
| CMJ Z-Score | 1 | −1.21 ± 0.80 | −0.96 ± 0.92 | 0.22 ± 0.40 * | 0.49 | 0.025 | −0.01 ± 0.58 | 0.05 | 0.889 |
| 2 | −0.99 ± 0.77 | −0.97 ± 0.79 | |||||||
| Total lean mass (kg) | 1 | 30.7 ± 4.6 | 27.4 ± 5.0 | 2.0 ± 1.5 * | 0.83 | <0.001 | 2.3 ± 2.2 * | 0.84 | 0.017 |
| 2 | 32.7 ± 5.0 | 29.7 ± 6.3 | |||||||
| Index of subtotal lean mass | 1 | 9.85 ± 1.99 | 9.15 ± 1.79 | 3.82 ± 1.79 * | 0.88 | <0.001 | 3.61 ± 2.15 * | 0.89 | 0.012 |
| 2 | 13.66 ± 1.40 | 12.76 ± 1.7 | |||||||
| Z-Score of index of subtotal lean mass | 1 | 1.15 ± 0.47 | 1.05 ± 0.34 | −0.72 ± 0.65 * | 0.75 | 0.001 | −1.11 ± 0.82 * | 0.84 | 0.017 |
| 2 | 0.44 ± 0.76 | −0.06 ± 0.8 | |||||||
| Legs lean mass (kg) | 1 | 5.5 ± 1.0 | 4.9 ± 1.0 | 0.4 ± 0.3 * | 0.85 | <0.001 | 0.6 ± 0.6 * | 0.79 | 0.025 |
| 2 | 5.9 ± 1.0 | 5.4 ± 1.4 | |||||||
| Arms lean mass (kg) | 1 | 1.4 ± 0.2 | 1.2 ± 0.2 | 0.1 ± 0.1 * | 0.79 | <0.001 | 0.1 ± 0.2 * | 0.79 | 0.025 |
| 2 | 1.5 ± 0.3 | 1.4 ± 0.3 | |||||||
| Variable | Time | AVG Group (n = 16) | Control Group (n = 7) | AVG Group | Control Group | ||||
|---|---|---|---|---|---|---|---|---|---|
| Change | Effects Size r | p Value | Change | Effects Size r | p Value | ||||
| Mean ± SD | Mean ± SD | ||||||||
| ST (min/day) | 1 | 841.9 ± 52.7 | 826.0 ± 51.2 | −195.9 ± 311.2 * | 0.53 | 0.034 | −12.3 ± 268.2 | 0.26 | 0.499 |
| 2 | 813.9 ± 53.6 | 824.2 ± 49.3 | |||||||
| LPA (min/day) | 1 | 71.3 ± 20.3 | 77.9 ± 30.9 | 89.9 ± 121.4 * | 0.58 | 0.020 | −12.8 ± 154.9 | 0.06 | 0.866 |
| 2 | 84.1 ± 19.2 | 76.1 ± 19.0 | |||||||
| MPA (min/day) | 1 | 44.5 ± 22.9 | 35.10 ± 16.82 | 51.3 ± 142.2 | 0.44 | 0.079 | 36.6 ± 119.2 | 0.38 | 0.310 |
| 2 | 51.8 ± 26.7 | 40.3 ± 16.6 | |||||||
| VPA (min/day) | 1 | 3.9 ± 5.0 | 1.5 ± 1.1 | 9.6 ± 20.6 | 0.45 | 0.069 | −0.3 ± 6.2 | 0.10 | 0.799 |
| 2 | 5.3 ± 5.9 | 1.5 ± 1.2 | |||||||
| MVPA (min/day) | 1 | 48.4 ± 27.4 | 36.6 ± 17.8 | 60.9 ± 161.2 | 0.47 | 0.063 | 36.3 ± 124.3 | 0.32 | 0.398 |
| 2 | 57.1 ± 32.3 | 41.83 ± 17.7 | |||||||
| PA (min/day) | 1 | 119.7 ± 43.9 | 122.7 ± 40.5 | 150.8 ± 258.5 * | 0.53 | 0.034 | 23.5 ± 275.6 | 0.26 | 0.499 |
| 2 | 141.2 ± 46.4 | 109.3 ± 33.5 | |||||||
| Variable | Pre-Intervention (n = 21) Mean ± SD | Post-Intervention (n = 21) Mean ± SD | Effects Size r | p Value |
|---|---|---|---|---|
| Total motor skills score (points) | 64.7 ± 9.7 | 78.3 ± 8.1 * | 0.88 | <0.001 |
| Locomotor skills (points) | 30.3 ± 6.5 | 38.7 ± 5.0 * | 0.88 | <0.001 |
| Object control skills (points) | 34.6 ± 5.6 | 39.6 ± 4.3 * | 0.81 | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Comeras-Chueca, C.; Villalba-Heredia, L.; Perez-Lasierra, J.L.; Marín-Puyalto, J.; Lozano-Berges, G.; Matute-Llorente, Á.; Vicente-Rodríguez, G.; Gonzalez-Aguero, A.; Casajús, J.A. Active Video Games Improve Muscular Fitness and Motor Skills in Children with Overweight or Obesity. Int. J. Environ. Res. Public Health 2022, 19, 2642. https://doi.org/10.3390/ijerph19052642
Comeras-Chueca C, Villalba-Heredia L, Perez-Lasierra JL, Marín-Puyalto J, Lozano-Berges G, Matute-Llorente Á, Vicente-Rodríguez G, Gonzalez-Aguero A, Casajús JA. Active Video Games Improve Muscular Fitness and Motor Skills in Children with Overweight or Obesity. International Journal of Environmental Research and Public Health. 2022; 19(5):2642. https://doi.org/10.3390/ijerph19052642
Chicago/Turabian StyleComeras-Chueca, Cristina, Lorena Villalba-Heredia, Jose Luis Perez-Lasierra, Jorge Marín-Puyalto, Gabriel Lozano-Berges, Ángel Matute-Llorente, Germán Vicente-Rodríguez, Alex Gonzalez-Aguero, and José A. Casajús. 2022. "Active Video Games Improve Muscular Fitness and Motor Skills in Children with Overweight or Obesity" International Journal of Environmental Research and Public Health 19, no. 5: 2642. https://doi.org/10.3390/ijerph19052642
APA StyleComeras-Chueca, C., Villalba-Heredia, L., Perez-Lasierra, J. L., Marín-Puyalto, J., Lozano-Berges, G., Matute-Llorente, Á., Vicente-Rodríguez, G., Gonzalez-Aguero, A., & Casajús, J. A. (2022). Active Video Games Improve Muscular Fitness and Motor Skills in Children with Overweight or Obesity. International Journal of Environmental Research and Public Health, 19(5), 2642. https://doi.org/10.3390/ijerph19052642










