Using Distributed Lag Non-Linear Models to Estimate Exposure Lag-Response Associations between Long-Term Air Pollution Exposure and Incidence of Cardiovascular Disease
Abstract
:1. Introduction
2. Materials and Methods
2.1. Materials
2.1.1. Study Cohorts
Gothenburg
Malmö
Stockholm
- (1)
- The Diabetes Prevention Program (SDPP) aims to study the individual, hereditary, and environmental determinants of impaired glucose tolerance and diabetes, as well its related morbidities. A random sample of individuals of 35–59 years of age living in Stockholm County were recruited during 1992–1994 and 1996–1998. A self-administrated health questionnaire was used to obtain data on risk factors.
- (2)
- The cohort of 60-y-olds (60YO) aims to study the predictors of cardiovascular disease among men and women born in 1937 or 1938. The cohort invited randomly individuals who filled 60 years of age during the 1 July 1997 to 20 June 1998 and were living in Stockholm County. Baseline information was gathered using a questionnaire and health examination, including blood sampling.
- (3)
- The Screening Across the Lifespan Twin study and TwinGene (SALT) study was created with the aim to study the genetic and environmental influences on diseases. An individual invitation was sent, between 1998 and 2002, to twins born before 1958 registered in the Swedish Twin Registry. Participants were screened for a wide spectrum of diseases and filled in an extensive questionnaire. Participants in the SALT cohort who lived in Stockholm County were included.
- (4)
- The Swedish National Study on Aging and Care in Kungsholmen (SNAC-K webpage) aims to identify possible methods to improve health and care among elderly adults. Age stratified random sampling was used to recruit individuals of at least 60 years of age living at home or in an institution in Kungsholmen during 2001–2004. Baseline information consisted of a self-administrated questionnaire, a nurse administrated questionnaire, and an extensive medical examination.
Umeå
2.2. Health Outcomes
2.3. Air Pollution Exposure Assessment
2.4. Statistical Methods
2.4.1. Specification of DLNMs and Model Selection
2.4.2. Meta-Analysis
3. Results
3.1. Descriptives
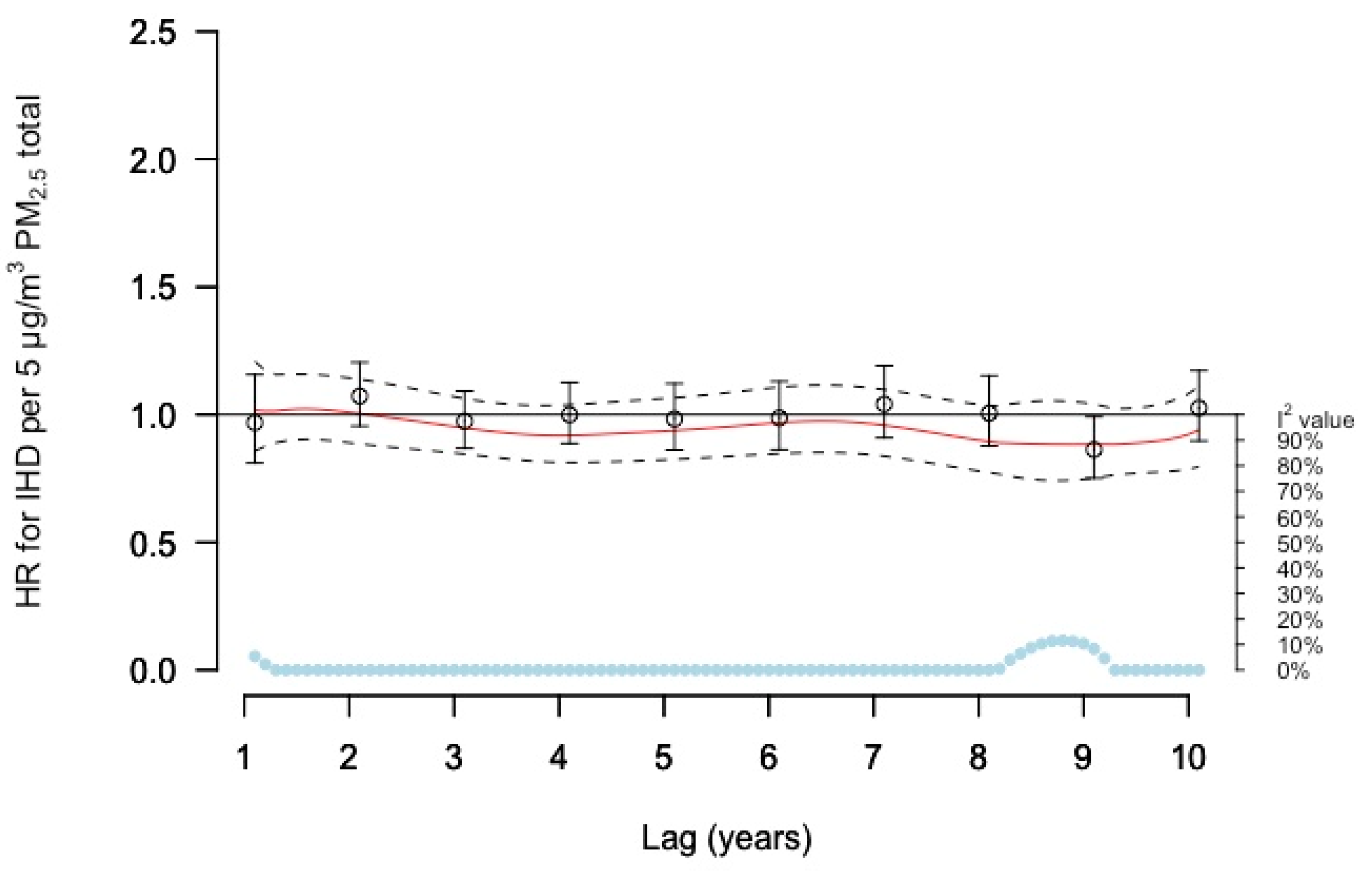
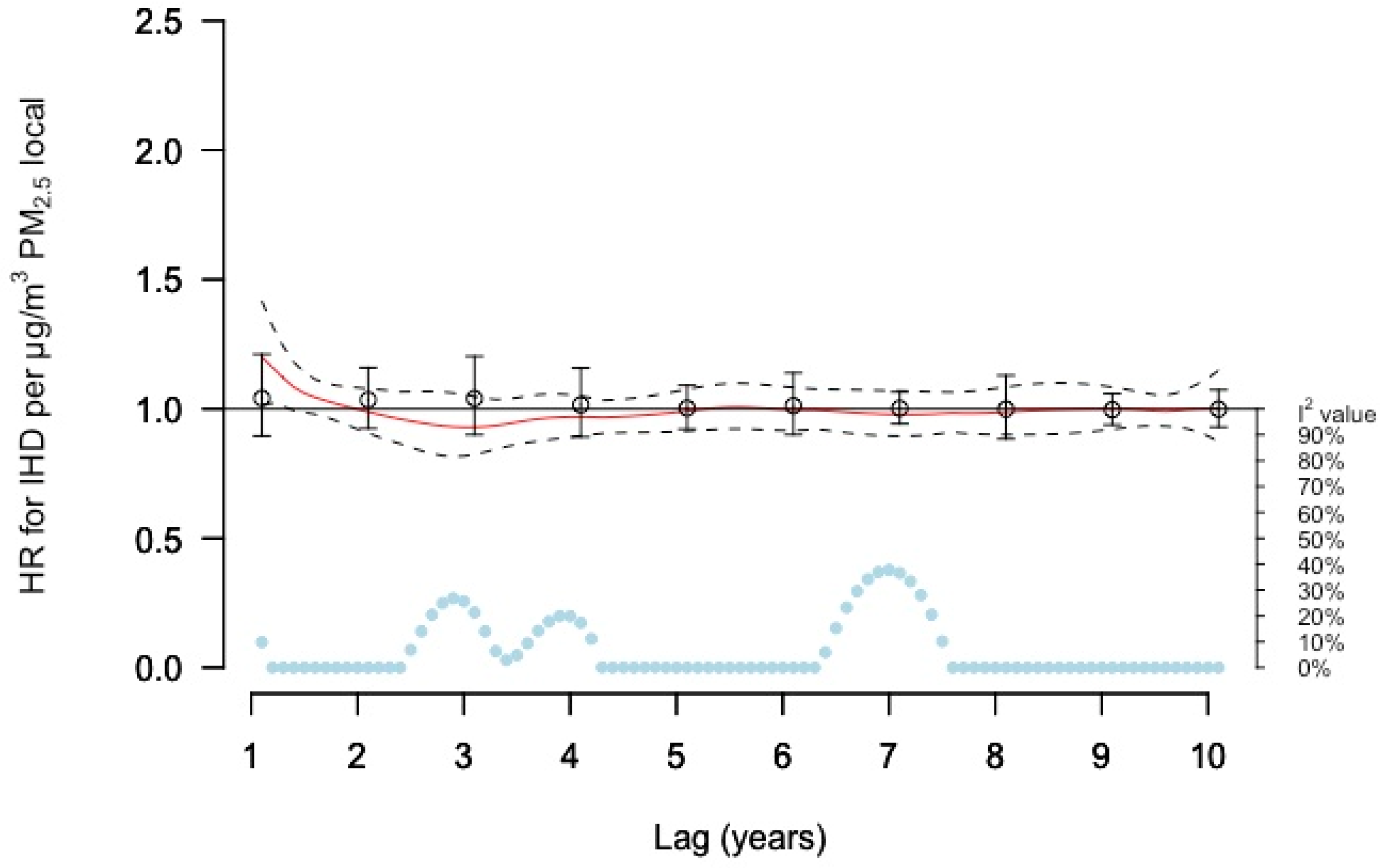
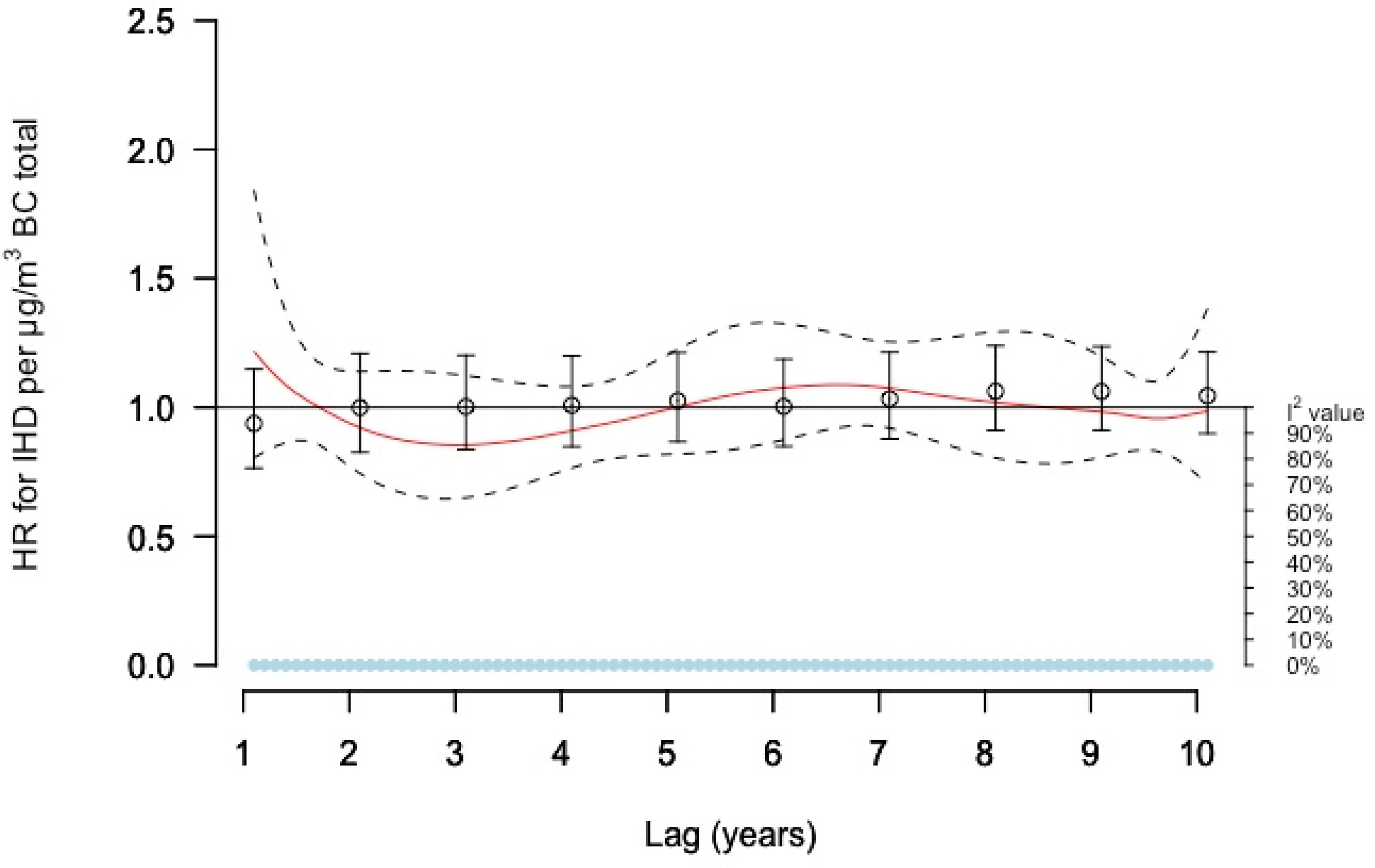
3.2. Associations with IHD
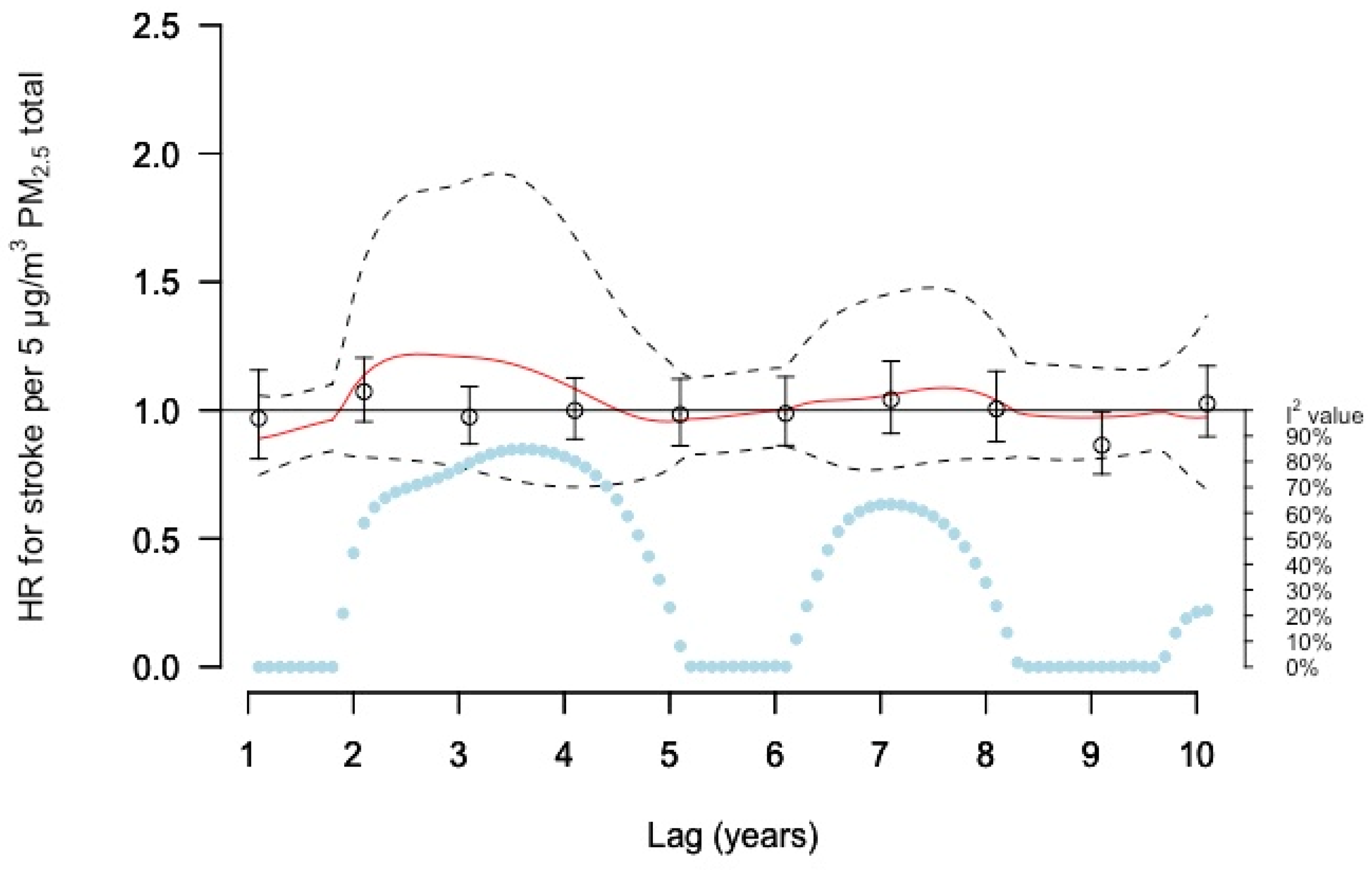
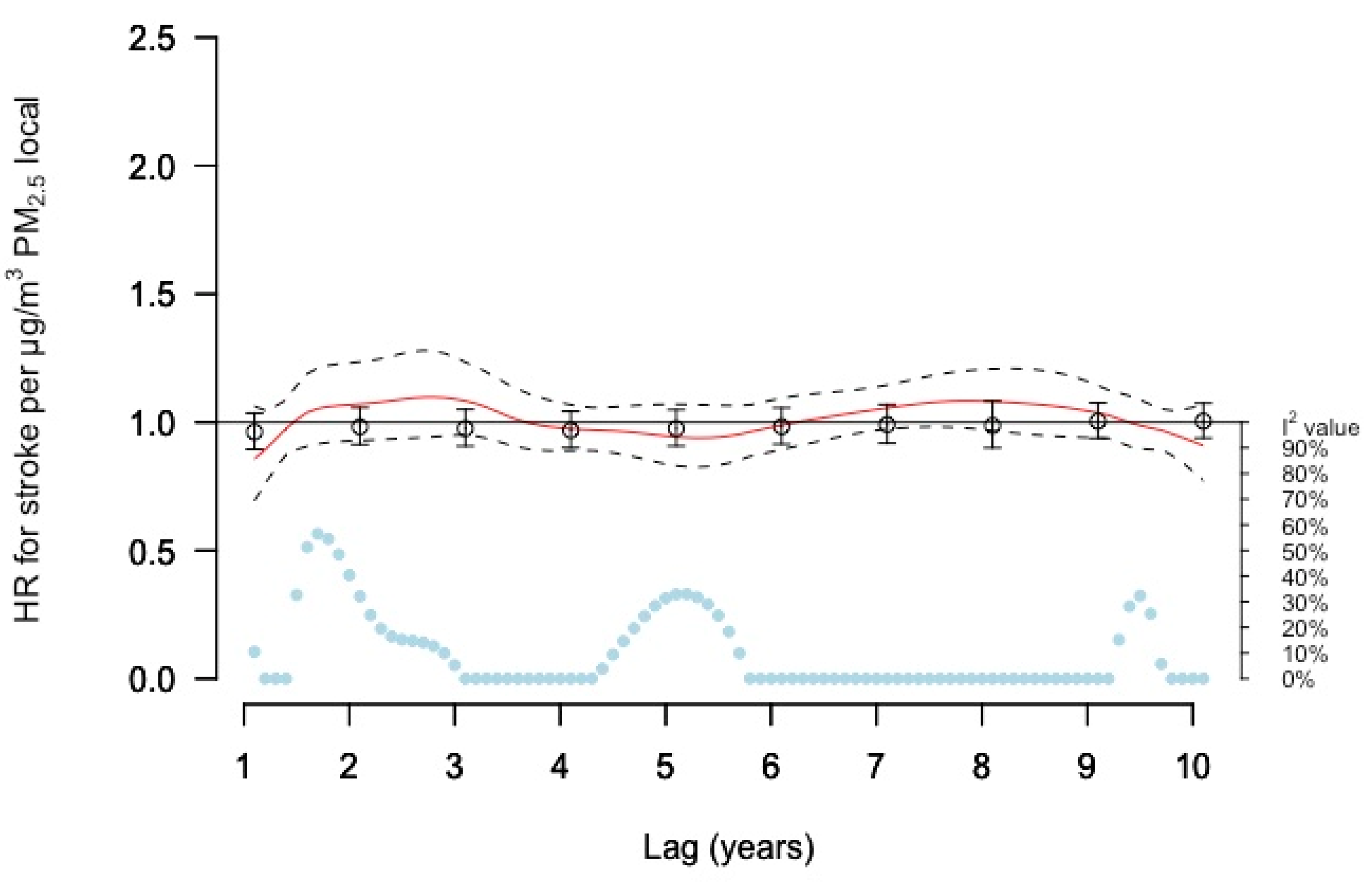
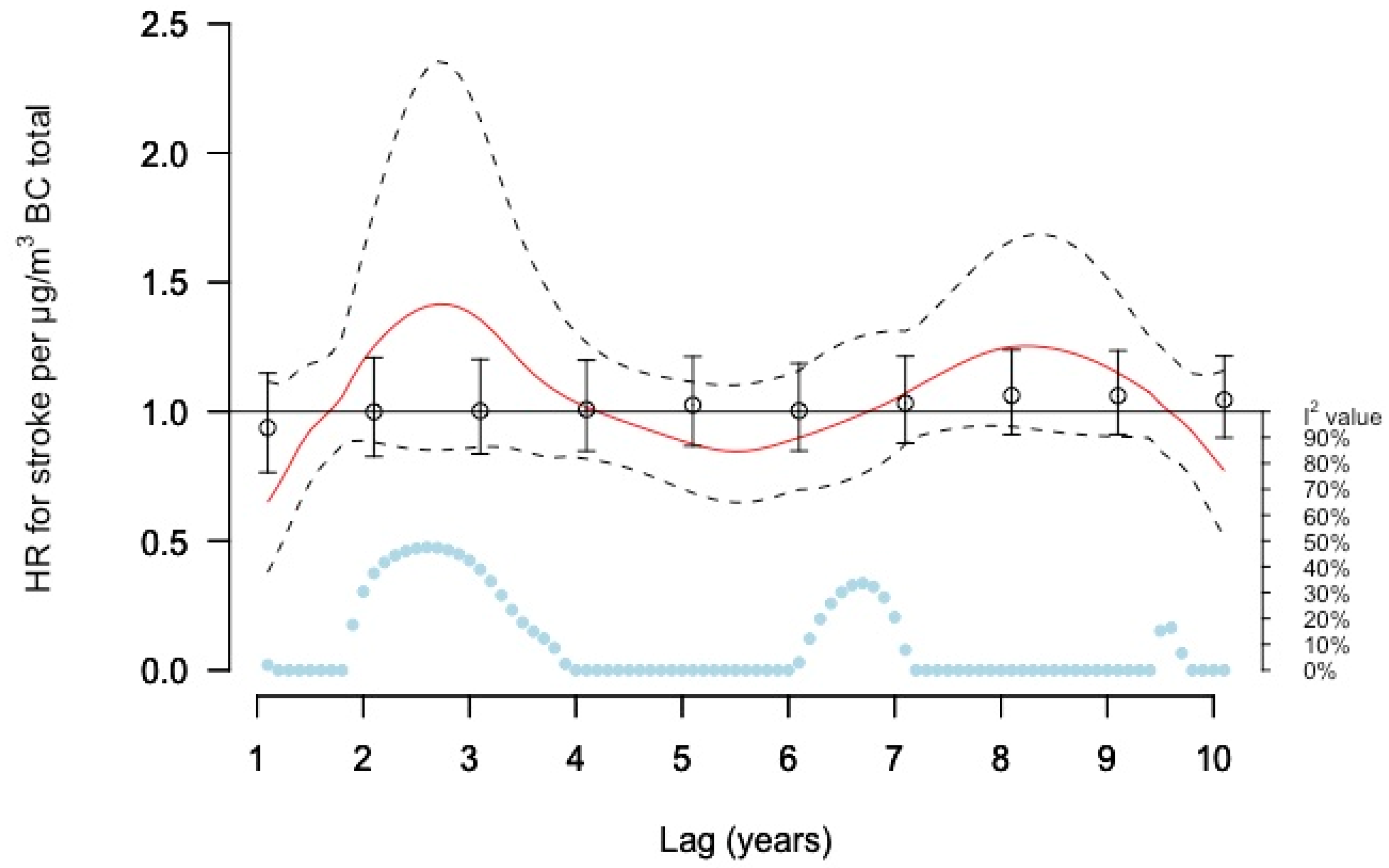
3.3. Associations with Stroke
4. Discussion
4.1. Comparing Exposure Lag-Response Results Using Different Methods
4.2. Ihd and Long-Term PM2.5 Exposure
4.3. Stroke and Long-Term PM2.5 Exposure
4.4. IHD and Long-Term BC Exposure
4.5. Stroke and Long-Term BC Exposure
4.6. Application of These Results
4.7. Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Chen, J.; Hoek, G. Long-term exposure to PM and all-cause and cause-specific mortality: A systematic review and meta-analysis. Environ. Int. 2020, 143, 105974. [Google Scholar] [CrossRef]
- Yuan, S.; Wang, J.; Jiang, Q.; He, Z.; Huang, Y.; Li, Z.; Cai, L.; Cao, S. Long-term exposure to PM2.5 and stroke: A systematic review and meta-analysis of cohort studies. Environ. Res. 2019, 177, 108587. [Google Scholar] [CrossRef]
- Zhu, W.; Cai, J.; Hu, Y.; Zhang, H.; Han, X.; Zheng, H.; Wu, J. Long-term exposure to fine particulate matter relates with incident myocardial infarction (MI) risks and post-MI mortality: A meta-analysis. Chemosphere 2021, 267, 128903. [Google Scholar] [CrossRef]
- WHO. WHO Global Air Quality Guidelines: Particulate Matter (PM2.5 and PM10), Ozone, Nitrogen Dioxide, Sulfur Dioxide and Carbon Monoxide; World Health Organization: Geneva, Switzerland, 2021.
- Segersson, D.; Eneroth, K.; Gidhagen, L.; Johansson, C.; Omstedt, G.; Engström Nylén, A.; Forsberg, B. Health Impact of PM10, PM2.5 and Black Carbon Exposure Due to Different Source Sectors in Stockholm, Gothenburg and Umea, Sweden. Int. J. Environ. Res. Public Health 2017, 14, 742. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ahmed, C.M.S.; Jiang, H.; Chen, J.Y.; Lin, Y.-H. Traffic-Related Particulate Matter and Cardiometabolic Syndrome: A Review. Atmosphere 2018, 9, 336. [Google Scholar] [CrossRef] [Green Version]
- Kaufman, J.D.; Adar, S.D.; Barr, R.G.; Budoff, M.; Burke, G.L.; Curl, C.L.; Daviglus, M.L.; Roux, A.V.D.; Gassett, A.J.; Jacobs, D.R.; et al. Association between air pollution and coronary artery calcification within six metropolitan areas in the USA (the Multi-Ethnic Study of Atherosclerosis and Air Pollution): A longitudinal cohort study. Lancet 2016, 388, 696–704. [Google Scholar] [CrossRef] [Green Version]
- Alexeeff, S.E.; Liao, N.S.; Liu, X.; Van Den Eeden, S.K.; Sidney, S. Long-Term PM2.5 Exposure and Risks of Ischemic Heart Disease and Stroke Events: Review and Meta-Analysis. J. Am. Heart Assoc. 2021, 10, e016890. [Google Scholar] [CrossRef] [PubMed]
- Amini, H.; Dehlendorff, C.; Lim, Y.H.; Mehta, A.; Jørgensen, J.T.; Mortensen, L.H.; Westendorp, R.; Hoffmann, B.; Loft, S.; Cole-Hunter, T.; et al. Long-term exposure to air pollution and stroke incidence: A Danish Nurse cohort study. Environ. Int. 2020, 142, 105891. [Google Scholar] [CrossRef] [PubMed]
- Rodins, V.; Lucht, S.; Ohlwein, S.; Hennig, F.; Soppa, V.; Erbel, R.; Jöckel, K.H.; Weimar, C.; Hermann, D.M.; Schramm, S.; et al. Long-term exposure to ambient source-specific particulate matter and its components and incidence of cardiovascular events-The Heinz Nixdorf Recall study. Environ. Int. 2020, 142, 105854. [Google Scholar] [CrossRef] [PubMed]
- Wolf, K.; Hoffmann, B.; Andersen, Z.J.; Atkinson, R.W.; Bauwelinck, M.; Bellander, T.; Brandt, J.; Brunekreef, B.; Cesaroni, G.; Chen, J.; et al. Long-term exposure to low-level ambient air pollution and incidence of stroke and coronary heart disease: A pooled analysis of six European cohorts within the ELAPSE project. Lancet Planet. Health 2021, 5, e620–e632. [Google Scholar] [CrossRef]
- Olaniyan, T.; Pinault, L.; Li, C.; van Donkelaar, A.; Meng, J.; Martin, R.V.; Hystad, P.; Robichaud, A.; Ménard, R.; Tjepkema, M.; et al. Ambient air pollution and the risk of acute myocardial infarction and stroke: A national cohort study. Environ. Res. 2021, 204, 111975. [Google Scholar] [CrossRef]
- Gasparrini, A.; Armstrong, B.; Kenward, M.G. Distributed lag non-linear models. Stat. Med. 2010, 29, 2224–2234. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hart, J.E.; Puett, R.C.; Rexrode, K.M.; Albert, C.M.; Laden, F. Effect Modification of Long-Term Air Pollution Exposures and the Risk of Incident Cardiovascular Disease in US Women. J. Am. Heart Assoc. 2015, 4, e002301. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ljungman, P.L.S.; Andersson, N.; Stockfelt, L.; Andersson, E.M.; Nilsson Sommar, J.; Eneroth, K.; Gidhagen, L.; Johansson, C.; Lager, A.; Leander, K.; et al. Long-Term Exposure to Particulate Air Pollution, Black Carbon, and Their Source Components in Relation to Ischemic Heart Disease and Stroke. Environ. Health Perspect. 2019, 127, 107012. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Stockfelt, L.; Andersson, E.M.; Molnár, P.; Gidhagen, L.; Segersson, D.; Rosengren, A.; Barregard, L.; Sallsten, G. Long-term effects of total and source-specific particulate air pollution on incident cardiovascular disease in Gothenburg, Sweden. Environ. Res. 2017, 158, 61–71. [Google Scholar] [CrossRef]
- Wilhelmsen, L.; Tibblin, G.; Werkö, L. A primary preventive study in Gothenburg, Sweden. Prev. Med. 1972, 1, 153–160. [Google Scholar] [CrossRef]
- Wilhelmsen, L.; Johansson, S.; Rosengren, A.; Wallin, I.; Dotevall, A.; Lappas, G. Risk factors for cardiovascular disease during the period 1985–1995 in Göteborg, Sweden. The GOT-MONICA Project. J. Intern. Med. 1997, 242, 199–211. [Google Scholar] [CrossRef]
- Manjer, J.; Carlsson, S.; Elmståhl, S.; Gullberg, B.; Janzon, L.; Lindström, M.; Mattisson, I.; Berglund, G. The Malmö diet and cancer study: Representativity, cancer incidence and mortality in participants and non-participants. Eur. J. Cancer Prev. 2001, 10, 489–499. [Google Scholar] [CrossRef] [Green Version]
- Korek, M.J.; Bellander, T.D.; Lind, T.; Bottai, M.; Eneroth, K.M.; Caracciolo, B.; de Faire, U.H.; Fratiglioni, L.; Hilding, A.; Leander, K.; et al. Traffic-related air pollution exposure and incidence of stroke in four cohorts from Stockholm. J. Expo. Sci. Environ. Epidemiol. 2015, 25, 517–523. [Google Scholar] [CrossRef] [Green Version]
- Norberg, M.; Wall, S.; Boman, K.; Weinehall, L. The Västerbotten Intervention Programme: Background, design and implications. Glob. Health Action 2010, 3, 4643. [Google Scholar] [CrossRef]
- WHO. International Statistical Classification of Diseases and Related Health Problems, 10th Revision; World Health Organization: Geneva, Switzerland, 2015.
- Hasslöf, H.; Molnár, P.; Andersson, E.M.; Spanne, M.; Gustafsson, S.; Stroh, E.; Engström, G.; Stockfelt, L. Long-term exposure to air pollution and atherosclerosis in the carotid arteries in the Malmö diet and cancer cohort. Environ. Res. 2020, 191, 110095. [Google Scholar] [CrossRef] [PubMed]
- R Core Team. R: A Language and Environment for Statistical Computing; R Core Team: Vienna, Austria, 2020. [Google Scholar]
- Beelen, R.; Raaschou-Nielsen, O.; Stafoggia, M.; Andersen, Z.J.; Weinmayr, G.; Hoffmann, B.; Wolf, K.; Samoli, E.; Fischer, P.; Nieuwenhuijsen, M.; et al. Effects of long-term exposure to air pollution on natural-cause mortality: An analysis of 22 European cohorts within the multicentre ESCAPE project. Lancet 2014, 383, 785–795. [Google Scholar] [CrossRef]
- Brook, R.D.; Rajagopalan, S.; Pope, C.A.; Brook, J.R.; Bhatnagar, A.; Diez-Roux, A.V.; Holguin, F.; Hong, Y.; Luepker, R.V.; Mittleman, M.A.; et al. Particulate Matter Air Pollution and Cardiovascular Disease: An Update to the Scientific Statement From the American Heart Association. Circulation 2010, 121, 2331–2378. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ben, A. Models for the Relationship between Ambient Temperature and Daily Mortality. Epidemiology 2006, 17, 624–631. [Google Scholar] [CrossRef]
- Cramer, J.; Jørgensen, J.T.; Hoffmann, B.; Loft, S.; Bräuner, E.V.; Prescott, E.; Ketzel, M.; Hertel, O.; Brandt, J.; Jensen, S.S.; et al. Long-Term Exposure to Air Pollution and Incidence of Myocardial Infarction: A Danish Nurse Cohort Study. Environ. Health Perspect. 2020, 128, 57003. [Google Scholar] [CrossRef]
- Lin, H.; Guo, Y.; Di, Q.; Zheng, Y.; Kowal, P.; Xiao, J.; Liu, T.; Li, X.; Zeng, W.; Howard, S.W.; et al. Ambient PM2.5 and Stroke: Effect Modifiers and Population Attributable Risk in Six Low- and Middle-Income Countries. Stroke 2017, 48, 1191–1197. [Google Scholar] [CrossRef] [Green Version]
- To, T.; Zhu, J.; Villeneuve, P.J.; Simatovic, J.; Feldman, L.; Gao, C.; Williams, D.; Chen, H.; Weichenthal, S.; Wall, C.; et al. Chronic disease prevalence in women and air pollution—A 30-year longitudinal cohort study. Environ. Int. 2015, 80, 26–32. [Google Scholar] [CrossRef]
- Thurston, G.D.; Burnett, R.T.; Turner, M.C.; Shi, Y.; Krewski, D.; Lall, R.; Ito, K.; Jerrett, M.; Gapstur, S.M.; Diver, W.R.; et al. Ischemic Heart Disease Mortality and Long-Term Exposure to Source-Related Components of U.S. Fine Particle Air Pollution. Environ. Health Perspect. 2016, 124, 785–794. [Google Scholar] [CrossRef] [Green Version]
- Yang, Y.; Tang, R.; Qiu, H.; Lai, P.C.; Wong, P.; Thach, T.Q.; Allen, R.; Brauer, M.; Tian, L.; Barratt, B. Long term exposure to air pollution and mortality in an elderly cohort in Hong Kong. Environ. Int. 2018, 117, 99–106. [Google Scholar] [CrossRef] [Green Version]
- Jhun, I.; Kim, J.; Cho, B.; Gold, D.R.; Schwartz, J.; Coull, B.A.; Zanobetti, A.; Rice, M.B.; Mittleman, M.A.; Garshick, E.; et al. Synthesis of Harvard Environmental Protection Agency (EPA) Center studies on traffic-related particulate pollution and cardiovascular outcomes in the Greater Boston Area. J. Air Waste Manag. Assoc. 2019, 69, 900–917. [Google Scholar] [CrossRef]
- Kriit, H.K.; Williams, J.S.; Lindholm, L.; Forsberg, B.; Nilsson Sommar, J. Health economic assessment of a scenario to promote bicycling as active transport in Stockholm, Sweden. BMJ Open 2019, 9, e030466. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kriit, H.K.; Nilsson Sommar, J.; Forsberg, B.; Åström, S.; Svensson, M.; Johansson, C. A health economic assessment of air pollution effects under climate neutral vehicle fleet scenarios in Stockholm, Sweden. J. Transp. Health 2021, 22, 101084. [Google Scholar] [CrossRef]
- Gasparrini, A.; Scheipl, F.; Armstrong, B.; Kenward, M.G. A penalized framework for distributed lag non-linear models. Biometrics 2017, 73, 938–948. [Google Scholar] [CrossRef] [PubMed]
- Vodonos, A.; Awad, Y.A.; Schwartz, J. The concentration-response between long-term PM2.5 exposure and mortality; A meta-regression approach. Environ. Res. 2018, 166, 677–689. [Google Scholar] [CrossRef] [PubMed]
- Brown, K.W.; Sarnat, J.A.; Suh, H.H.; Coull, B.A.; Koutrakis, P. Factors influencing relationships between personal and ambient concentrations of gaseous and particulate pollutants. Sci. Total Environ. 2009, 407, 3754–3765. [Google Scholar] [CrossRef]
- Norberg, M.; Blomstedt, Y.; Lönnberg, G.; Nyström, L.; Stenlund, H.; Wall, S.; Weinehall, L. Community participation and sustainability–evidence over 25 years in the Västerbotten Intervention Programme. Glob. Health Action 2012, 5, 19166. [Google Scholar] [CrossRef]
- Olsson, D.; Johansson, C.; Forsberg, B. Associations between Vehicle Exhaust Particles and Ozone at Home Address and Birth Weight. Int. J. Environ. Res. Public Health 2020, 17, 3836. [Google Scholar] [CrossRef]
- Andersson, E.M.; Ögren, M.; Molnár, P.; Segersson, D.; Rosengren, A.; Stockfelt, L. Road traffic noise, air pollution and cardiovascular events in a Swedish cohort. Environ. Res. 2020, 185, 109446. [Google Scholar] [CrossRef]
- Sommar, J.N.; Andersson, E.M.; Andersson, N.; Sallsten, G.; Stockfelt, L.; Ljungman, P.L.S.; Segersson, D.; Eneroth, K.; Gidhagen, L.; Molnar, P.; et al. Long-term exposure to particulate air pollution and black carbon in relation to natural and cause specific mortality: A multi-cohort study in Sweden. BMJ Open 2021, 11, e046040. [Google Scholar]
- Stockfelt, L.; Andersson, E.M.; Molnár, P.; Rosengren, A.; Wilhelmsen, L.; Sallsten, G.; Barregard, L. Long term effects of residential NO(x) exposure on total and cause-specific mortality and incidence of myocardial infarction in a Swedish cohort. Environ. Res. 2015, 142, 197–206. [Google Scholar] [CrossRef] [Green Version]
| Gothenburg, GOT- MONICA | Gothenburg, PPS | Malmö, MDC | Stockholm, CEANS | Umeå, VIP | ||
|---|---|---|---|---|---|---|
| Participants (n) | 4500 | 5850 | 25 722 | 21 549 | 41941 | |
| Baseline data collection (calendar years) | 1985, 1990, 1995 | 1970–1974 | 1991–1996 | 1992–2004 | 1990–2013 | |
| Age at enrolment (years; median (range)) | 46 (25–66) | 51 (46–56) | 57 (44–73) | 57 (35–104) | 54 (29–84) | |
| Women (%) | 52 | 0 | 62 | 58 | 52 | |
| Smoking status (%) | Current smoker | 29 | 39 | 27 | 21 | 21 |
| Former smoker | 23 | 33 | 31 | 36 | 27 | |
| Never smoker | 42 | 27 | 37 | 41 | 43 | |
| Missing data | 5 | 0.1 | 6 | 2 | 0 | |
| Leisure time physical activity (%) | Sedentary | 17 | 24 | 18 | 61 a | 14 |
| Moderate | 62 | 58 | 59 | 26 b | 41 | |
| Intermediate and vigorous | 18 | 17 | 17 | 8 c | 44 | |
| Missing data | 2 | 1 | 6 | 4 | 1 | |
| Alcohol consumption d (%) | Daily | 1 | 7 | 5 | ||
| Weekly | 24 | 55 | 13 | |||
| Seldom | 38 | 31 | 44 | |||
| Never | 5 | 6 | 34 | |||
| Missing data | 31 | 2 | 8 | |||
| Married/living with partner (%) | No | 21 | 14 | 31 | 29 | 17 |
| Yes | 47 | 86 | 63 | 69 | 79 | |
| Missing data | 31 | 0 | 6 | 1 | 4 | |
| Education level (%) | Primary school or less | 12 | 66 | 68 | 30 | 37 |
| Up to secondary school or equivalent | 32 | 21 | 17 | 36 | 25 | |
| University degree and more | 19 | 11 | 14 | 31 | 29 | |
| Missing data | 3 | 0 | 1 | 3 | 9 | |
| Occupation (%) | Gainfully employed | 57 | 66 | 80 | ||
| Unemployed/not gainfully employed | 7 | 6 | 4 | |||
| Retired | 30 | 27 | 3 | |||
| Missing data | 6 | 1 | 13 | |||
| Socioeconomic index by occupation (%) | Blue collar | 47 | 35 | 26 | ||
| Low-and intermediate white collar and self-employed | 23 | 48 | 51 | |||
| High level white collar and self-employed professional with academic degrees | 30 | 10 | 18 | |||
| Missing data | 0 | 6 | 4 | |||
| Mean income by SAMS 1994 (SEK) | 154,780 | 148,602 | 144,641 | 304,384 e | 130,076 |
| Exposure (μg/m3) | Gothenburg, GOT-MONICA | Gothenburg, PPS | Malmö, MDC | Stockholm, CEANS | Umeå, VIP | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean | Range | IQR | Mean | Range | IQR | Mean | Range | IQR | Mean | Range | IQR | Mean | Range | IQR | |
| Total | |||||||||||||||
| PM2.5 | 8.5 | 2.9–16.4 | 2.68 | 9.1 | 2.9–16.8 | 2.44 | 10.9 | 6.6–18.4 | 1.63 | 7.7 | 4.6–24.9 | 2.52 | 5.9 | 3.7–22.5 | 1.18 |
| BC | 0.9 | 0.2–4.3 | 0.39 | 1.0 | 0.2–4.5 | 0.39 | 0.9 | 0.7–1.9 | 0.15 | 0.7 | 0.4–4.8 | 0.42 | 0.5 | 0.2–7.8 | 0.13 |
| Local | |||||||||||||||
| PM2.5 | 2.7 | 0.2–9.9 | 1.42 | 3.1 | 0.2–9.6 | 1.27 | 1.4 | 0.3–6.5 | 0.55 | 1.7 | 0.1–18.7 | 1.23 | 1.3 | 0.2–6.9 | 0.55 |
| Gothenburg, MONICA | Gothenburg, PPS | Malmö, MDC | Stockholm, CEANS | Umeå, VIP | |
|---|---|---|---|---|---|
| Number of IHD cases (% women) | 233 (33) | 557 (0) | 2026 (46) | 1343 (47) | 983 (54) |
| -average age in years | 70.8 | 84.1 | 76.3 | 72.9 | 67.5 |
| Number of stroke cases (% women) | 153 (46) | 400 (0) | 1578 (54) | 941 (54) | 542 (50) |
| -average age in years | 71.4 | 84.0 | 77.4 | 75.5 | 66.4 |
| Average follow-up time (years) | |||||
| IHD | 9.2 | 7 | 20.1 | 10.6 | 8.5 |
| Stroke | 9.3 | 7.2 | 20.1 | 10.6 | 8.5 |
| Total number of person-years | |||||
| IHD | 35,010 | 17,245 | 287,531 | 220,314 | 208,965 |
| Stroke | 35,794 | 18,819 | 281,621 | 225,226 | 203,477 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kriit, H.K.; Andersson, E.M.; Carlsen, H.K.; Andersson, N.; Ljungman, P.L.S.; Pershagen, G.; Segersson, D.; Eneroth, K.; Gidhagen, L.; Spanne, M.; et al. Using Distributed Lag Non-Linear Models to Estimate Exposure Lag-Response Associations between Long-Term Air Pollution Exposure and Incidence of Cardiovascular Disease. Int. J. Environ. Res. Public Health 2022, 19, 2630. https://doi.org/10.3390/ijerph19052630
Kriit HK, Andersson EM, Carlsen HK, Andersson N, Ljungman PLS, Pershagen G, Segersson D, Eneroth K, Gidhagen L, Spanne M, et al. Using Distributed Lag Non-Linear Models to Estimate Exposure Lag-Response Associations between Long-Term Air Pollution Exposure and Incidence of Cardiovascular Disease. International Journal of Environmental Research and Public Health. 2022; 19(5):2630. https://doi.org/10.3390/ijerph19052630
Chicago/Turabian StyleKriit, Hedi Katre, Eva M. Andersson, Hanne K. Carlsen, Niklas Andersson, Petter L. S. Ljungman, Göran Pershagen, David Segersson, Kristina Eneroth, Lars Gidhagen, Mårten Spanne, and et al. 2022. "Using Distributed Lag Non-Linear Models to Estimate Exposure Lag-Response Associations between Long-Term Air Pollution Exposure and Incidence of Cardiovascular Disease" International Journal of Environmental Research and Public Health 19, no. 5: 2630. https://doi.org/10.3390/ijerph19052630
APA StyleKriit, H. K., Andersson, E. M., Carlsen, H. K., Andersson, N., Ljungman, P. L. S., Pershagen, G., Segersson, D., Eneroth, K., Gidhagen, L., Spanne, M., Molnar, P., Wennberg, P., Rosengren, A., Rizzuto, D., Leander, K., Yacamán-Méndez, D., Magnusson, P. K. E., Forsberg, B., Stockfelt, L., & Sommar, J. N. (2022). Using Distributed Lag Non-Linear Models to Estimate Exposure Lag-Response Associations between Long-Term Air Pollution Exposure and Incidence of Cardiovascular Disease. International Journal of Environmental Research and Public Health, 19(5), 2630. https://doi.org/10.3390/ijerph19052630





