Perinatal Anxiety among Women during the COVID-19 Pandemic—A Cross-Sectional Study
Abstract
1. Introduction
- -
- Learning about respondents’ opinions on the support received from medical personnel and relatives.
- -
- Assessment of received social support impact on the perinatal anxiety level.
- -
- Assessment of perinatal care and education and its impact on experienced perinatal anxiety level.
- -
- Analysis of the relation between psychological condition and experienced perinatal anxiety level.
- -
- Assessment of the influence of selected obstetric factors on the experienced perinatal anxiety occurrence.
2. Materials and Methods
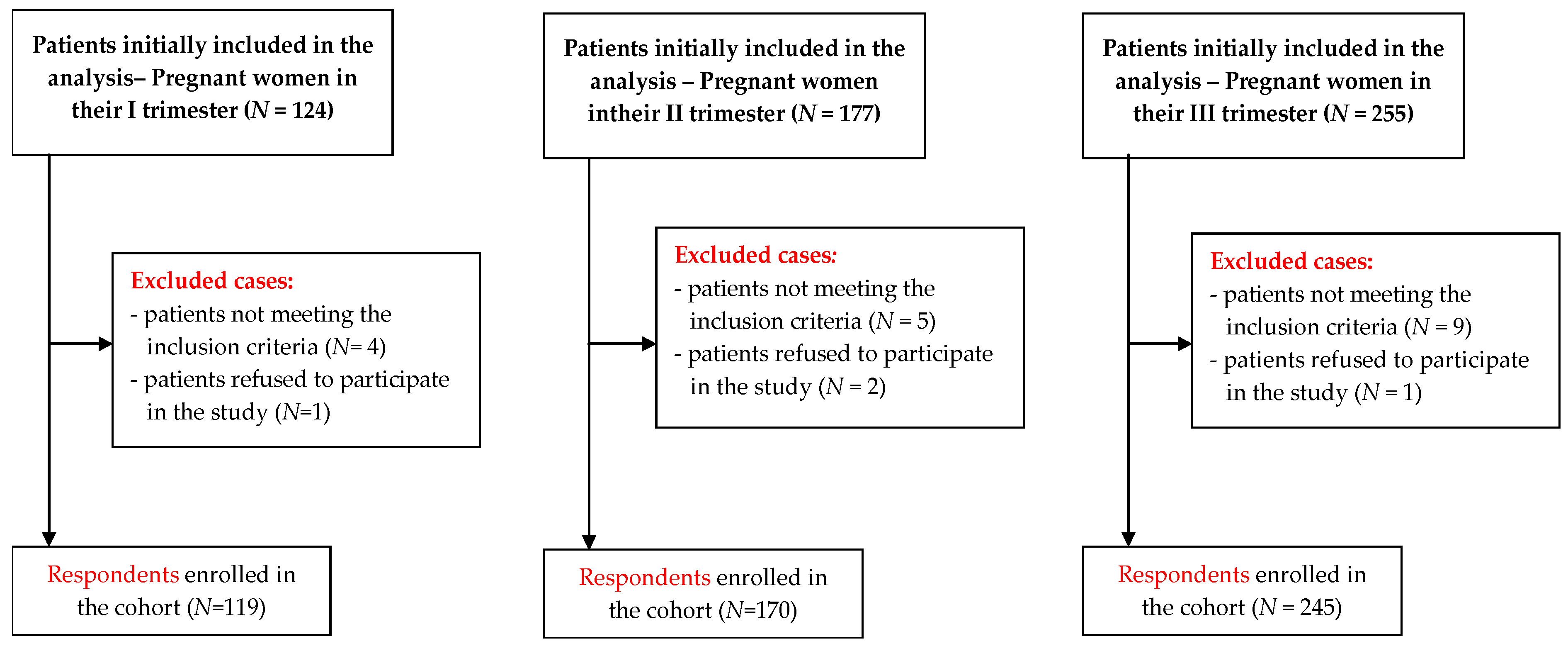
2.1. Study Design and Participants
- The State-Trait Anxiety Inventory (STAI) is a tool comprising two scales. The first part of the STAI (x-1) examines the level of anxiety as a current emotional state. It consists of 20 statements, for each of which the respondent chooses one of four possible answers (definitely, probably, probably not, definitely not). The responses to these statements describe the respondent’s feelings while filling out the questionnaire. The second part (x-2) concerns anxiety understood as a personality trait. It also consists of 20 statements that the respondent can answer, using a four-point scale (almost never, sometimes, often, almost always). The responses for this second part provide a picture of how the respondent usually feels [18,19]. The Cronbach’s alpha coefficient for the questionnaire for the studied group was 0.908 (x-1) and 0.869 (x-2), (Supplementary File).
- The Childbirth Anxiety Questionnaire (CAQ): a tool for gaining information on emotions associated with upcoming childbirth. The CAQ is made up of nine statements to which the respondent answers by choosing one of four categories (definitely, probably, probably not, definitely not) to which numerical values are assigned. The higher the score, the greater severity of childbirth anxiety [20]. The Cronbach’s alpha reliability coefficient for the research group was 0.824, (Supplementary File).
- The questionnaire specially prepared for this study takes into consideration the characteristics of the women being researched as well as questions concerning the research topic. The respondents answered on a five-point Likert scale (1—definitely not, 5—definitely yes) on the topics of determinants of childbirth anxiety they felt and healthcare conditions in the time of the SARS-CoV-2 virus pandemic.
2.2. Statistical Analysis
3. Results
“I am worried about the current epidemiological situation and the impossibility of family members being present for the delivery; even more, I am stressed about giving birth by myself.”
“I have brief attacks of hysteria, but they pass quickly.”
“The current epidemic greatly increases my anxiety before giving birth. My husband has promised to be with me for the delivery, our due-date is the end of September. Knowing that having family members at the delivery has still not been restored yet at the hospitals in my region causes additional, senseless anxiety and panic. And to what purpose? I am not afraid of a virus, I am afraid of trauma and post-partum depression caused by having my rights, peace, and dreams taken away. I cannot imagine being alone in such a difficult situation as giving birth to my first child.”
“The long years of fighting infertility have certainly influenced my perception of anxiety and childbirth, because I know that I may not have a second chance, so I am more afraid. And now this epidemic…”
“More than labor and delivery, I am afraid about successfully carrying the pregnancy, due to an earlier miscarriage and long, in my opinion, attempts to have a baby. My desire for a child is so great that I am not interested in the fact that I will feel pain, I am ready for anything, just to give birth successfully, especially in this situation with coronavirus.”
4. Discussion
Strengths and Limitations of the Study
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Kef, K. COVID-19: The Level of Knowledge, Anxiety and Symptom Presentation. Psychol. Res. Behav. Manag. 2021, 14, 541–548. [Google Scholar] [CrossRef] [PubMed]
- Stojanov, J.; Stankovic, M.; Zikic, O.; Stankovic, M.; Stojanov, A. The risk for nonpsychotic postpartum mood and anxiety disorders during the COVID-19 pandemic. Int.J. Psychiatry Med. 2021, 56, 228–239. [Google Scholar] [CrossRef] [PubMed]
- Bayrampour, H.; Ali, E.; McNeil, D.; Benzies, K.; MacQueen, G.; Tough, S. Pregnancy-related anxiety: A concept analysis. Int. J. Nurs. Stud. 2016, 55, 115–130. [Google Scholar] [CrossRef]
- Nechita, D.; Nechita, F.; Motorga, R. A review of influence the anxiety exerts on humanlife. Rom. J. Morphol. Embryol. 2018, 59, 1045–1051. [Google Scholar] [PubMed]
- Dennis, C.L.; Falah-Hassani, K.; Shiri, R. Prevalence of antenatal and postnatal anxiety: Systematic review and meta-analysis. Br. J. Psychiatry 2017, 210, 315–323. [Google Scholar] [CrossRef] [PubMed]
- Cardwell, M.S. Stress: Pregnancy considerations. Obstet. Gynecol. Surv. 2013, 68, 119–129. [Google Scholar] [CrossRef]
- Mah, B.L.; Pringle, K.G.; Weatherall, L.; Keogh, L.; Schumacher, T.; Eades, S.; Brown, A.; Lumbers, E.R.; Roberts, C.T.; Diehm, C.; et al. Pregnancy stress, healthy pregnancy and birth outcomes-the need for early preventative approaches in pregnant Australian Indigenous women: A prospective longitudinal cohort study. J. Dev. Orig. Health Dis. 2019, 10, 31–38. [Google Scholar] [CrossRef]
- Polte, C.; Junge, C.; von Soest, T.; Seidler, A.; Eberhard-Gran, M.; Garthus-Niegel, S. Impact of maternal perinatal anxiety on social-emotional development of 2-year-olds, a prospective study of Norwegian mothers and their offspring: The impact of perinatal anxiety on child development. Matern. Child Health J. 2019, 23, 386–396. [Google Scholar] [CrossRef]
- Noonan, M.; Jomeen, J.; Doody, O. A review of the involvement of partners and family members in psychosocial interventions for supporting women at risk of or experiencing perinatal depression and anxiety. Int. J. Environ. Res. Public Health 2021, 18, 5396. [Google Scholar] [CrossRef]
- Rozporządzenie Ministra Zdrowia z dnia 16 Sierpnia 2018 r. w Sprawie Standardu Organizacyjnego Opieki Okołoporodowej. Dz.U. 1756. 2018. Available online: https://isap.sejm.gov.pl/isap.nsf/download.xsp/WDU20180001756/O/D20181756.pdf (accessed on 16 December 2021).
- Wang, C.L.; Liu, Y.Y.; Wu, C.H.; Wang, C.Y.; Wang, C.H.; Long, C.Y. Impact of COVID-19 on pregnancy. Int. J. Med. Sci. 2021, 18, 763–767. [Google Scholar] [CrossRef]
- Derya, Y.A.; Altiparmak, S.; AkÇa, E.; GÖkbulut, N.; Yilmaz, A.N. Pregnancy and birth planning during COVID-19. The effects of tele-education offered to pregnant women on prenatal distress and pregnancy-related anxiety. Midwifery 2021, 92, 102877. [Google Scholar] [CrossRef]
- Polizzi, C.; Burgio, S.; Lavanco, G.; Alesi, M. Parental Distress and perception of children’s executive functioning after the first COVID-19 lockdown in Italy. J. Clin. Med. 2021, 10, 4170. [Google Scholar] [CrossRef] [PubMed]
- Karaçam, Z.; Ançel, G. Depression, anxiety and influencing factors in pregnancy: A study in a Turkish population. Midwifery 2009, 25, 344–356. [Google Scholar] [CrossRef] [PubMed]
- Basu, A.; Kim, H.H.; Basaldua, R.; Choi, K.W.; Charron, L.; Kelsall, N.; Hernandez-Diaz, S.; Wyszynski, D.F.; Koenen, K.C. A cross-national study of factors associated with women’s perinatal mental health and wellbeing during the COVID-19 pandemic. PLoS ONE 2021, 16, e0249780. [Google Scholar] [CrossRef]
- Zhang, J.; Yu, H.; Gao, Y.; Xu, Q.; Yin, Y.; Zhou, R. Prevalence of Anxiety and Depression among Pregnant Women during the COVID-19 Pandemic: A Systematic Review and Meta-Analysis. 2020. Available online: https://assets.researchsquare.com/files/rs-87129/v1/7c0115bb-a955-417c-a457-2725e9eff1ab.pdf?c=1631857548 (accessed on 18 January 2022). [CrossRef]
- Vacaru, S.; Beijers, R.; Browne, P.D. The risk and protective factors of heightened prenatal anxiety and depression during the COVID-19 lockdown. Sci. Rep. 2021, 11, 20261. [Google Scholar] [CrossRef]
- Liu, K.; Chen, Y.; Wu, D.; Lin, R.; Wang, Z.; Pan, L. Effects of progressive muscle relaxation on anxiety and sleep quality in patients with COVID-19. Complement. Ther. Clin. Pract. 2020, 39, 101132. [Google Scholar] [CrossRef]
- Janik, K.; Cwalina, U.; Iwanowicz-Palus, G.; Cybulski, M. An assessment of the level of COVID-19 anxiety among pregnant women in Poland: A cross-sectional study. J. Clin. Med. 2021, 10, 5869. [Google Scholar] [CrossRef]
- Putyński, L.; Paciorek, M. Kwestionariusz lęku porodowego (KLP II) wersja zrewidowana–konstrukcja i właściwości psychometryczne. Acta Univ. Lodziensis. Folia Psychol. 2008, 12, 129–133. [Google Scholar]
- Ahmad, M.; Vismara, L. The psychological impact of COVID-19 pandemic on women’s mental health during pregnancy: A rapid evidence review. Int. J. Environ. Res. Public Health 2021, 18, 7112. [Google Scholar] [CrossRef]
- Brooks, S.K.; Webster, R.K.; Smith, L.E.; Woodland, L.; Wessely, S.; Greenberg, N.; Rubin, G.J. The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. Lancet 2020, 395, 912–920. [Google Scholar] [CrossRef]
- Shrestha, S.; Pun, K.D. Anxiety on primigravid women attending antenatal care: A hospital based cross-sectional study. Kathmandu Univ. Med. J. (KUMJ) 2018, 16, 23–27. [Google Scholar]
- Chan, C.Y.; Lee, A.M.; Lam, S.K.; Lee, C.P.; Leung, K.Y.; Koh, Y.W.; Tang, C.S.K. Antenatal anxiety in the first trimester: Risk factors and effects on anxiety and depression in the third trimester and 6-week postpartum. Open J. Psychiatry 2013, 301–310. [Google Scholar] [CrossRef][Green Version]
- Kahyaoglu, S.H.; Kucukkaya, B. Anxiety, depression, and related factors in pregnant women during the COVID-19 pandemic in Turkey: A web-based cross-sectional study. Perspect. Psychiatr. Care 2021, 57, 860–868. [Google Scholar] [CrossRef] [PubMed]
- Naz, S.; Muhammad, D.; Ahmad, A. Pregnant women perceptions regarding their husbands and in-laws’ support during pregnancy: A qualitative study. Pan. Afr. Med. J. 2021, 39, 229. [Google Scholar] [CrossRef]
- Iwanowicz-Palus, G.; Mróz, M.; Bień, A.; Jurek, K. Social support and subjective assessment of psychophysical condition, health, and satisfaction with quality of life among women after pregnancy loss. BMC Pregnancy Childbirth 2021, 21, 750. [Google Scholar] [CrossRef] [PubMed]
- Bäckström, C.; Thorstensson, S.; Pihlblad, J.; Forsman, A.C.; Larsson, M. Parents’ experiences of receiving professional support through extended home visits during pregnancy and early childhood-A Phenomenographic study. Front. Public Health 2021, 9, 578917. [Google Scholar] [CrossRef]
- Brooks, S.K.; Weston, D.; Greenberg, N. Psychological impact of infectious disease outbreaks on pregnant women: Rapid evidence review. Public Health 2020, 189, 26–36. [Google Scholar] [CrossRef]
- Baran, J.; Leszczak, J.; Baran, R.; Biesiadecka, A.; Weres, A.; Czenczek-Lewandowska, E.; Kalandyk-Osinko, K. Prenatal and Postnatal Anxiety and Depression in Mothers during the COVID-19 Pandemic. J. Clin. Med. 2021, 10, 3193. [Google Scholar] [CrossRef]
- Reid, K.M.; Taylor, M.G. Social support, stress, and maternal postpartum depression: A comparison of supportive relationships. Soc. Sci. Res. 2015, 54, 246–262. [Google Scholar] [CrossRef]
- Hassanzadeh, R.; Abbas-Alizadeh, F.; Meedya, S.; Mohammad-Alizadeh-Charandabi, S.; Mirghafourvand, M. Primiparous women’s knowledge and satisfaction based on their attendance at childbirth preparation classes. Nurs. Open 2021, 8, 2558–2566. [Google Scholar] [CrossRef]
- Karlström, A.; Nystedt, A.; Johansson, M.; Hildingsson, I. Behind the myth--few women prefer caesarean section in the absence of medical or obstetrical factors. Midwifery 2011, 27, 620–627. [Google Scholar] [CrossRef] [PubMed]
- Swift, E.M.; Zoega, H.; Stoll, K.; Avery, M.; Gottfreðsdóttir, H. Enhanced antenatal care: Combining one-to-one and group Antenatal Care models to increase childbirth education and address childbirth fear. Women Birth 2021, 34, 381–388. [Google Scholar] [CrossRef] [PubMed]
- Kuciel, N.; Sutkowska, E.; Biernat, K.; Hap, K.; Mazurek, J.; Demczyszak, I. Assessment of the level of anxiety and pain in women who do and do not attend childbirth classes during the SARS-CoV-2 pandemic. Risk Manag. Healthc Policy 2021, 14, 4489–4497. [Google Scholar] [CrossRef] [PubMed]
- Hassanzadeh, R.; Abbas-Alizadeh, F.; Meedya, S.; Mohammad-Alizadeh-Charandabi, S.; Mirghafourvand, M. Fear of childbirth, anxiety and depression in three groups of primiparous pregnant women not attending, irregularly attending and regularly attending childbirth preparation classes. BMC Womens Health 2020, 20, 180. [Google Scholar] [CrossRef]
- Farewell, C.V.; Jewell, J.; Walls, J.; Leiferman, J.A. A Mixed-Methods Pilot Study of Perinatal Risk and Resilience During COVID-19. J. Prim. Care Community Health 2020, 11, 2150132720944074. [Google Scholar] [CrossRef] [PubMed]
- Mehdizadehkashi, A.; Chaichian, S.; Haghighi, L.; Eshraghi, N.; Bordbar, A.; Hashemi, N.; Derakhshan, R.; Mirgalobayat, S.; Rokhgireh, S.; Tahermanesh, K. The Impact of COVID-19 Pandemic on Stress and Anxiety of Non-infected Pregnant Mothers. J. Reprod. Infertil. 2021, 22, 125–132. [Google Scholar] [CrossRef] [PubMed]
- Mortazavi, F.; Mehrabadi, M. Predictors of fear of childbirth and normal vaginal birth among Iranian postpartum women: A cross-sectional study. BMC Pregnancy Childbirth 2021, 21, 316. [Google Scholar] [CrossRef]
- Størksen, H.T.; Garthus-Niegel, S.; Adams, S.S.; Vangen, S.; Eberhard-Gran, M. Fear of childbirth and elective caesarean section: A population-based study. BMC Pregnancy Childbirth 2015, 15, 221. [Google Scholar] [CrossRef]
- Malhotra, Y.; Miller, R.; Bajaj, K.; Sloma, A.; Wieland, D.; Wilcox, W. No change in cesarean section rate during COVID-19 pandemic in New York City. Eur. J. Obstet. Gynecol. Reprod. Biol. 2020, 253, 328–329. [Google Scholar] [CrossRef]
| Participants’ Characteristics | I Trimester | II Trimester | III Trimester | Total | |
|---|---|---|---|---|---|
| % (n) | % (n) | % (n) | |||
| Age | <20 | 2.5 (3) | 0.6 (1) | 2.4 (6) | 1.9 (10) |
| 20–29 | 78.2 (93) | 64.1 (109) | 61.2 (150) | 65.9 (352) | |
| 30–39 | 19.3 (23) | 33.5 (57) | 34.3 (84) | 30.7 (164) | |
| ≥40 | - | 1.8 (3) | 2.0 (5) | 1.5 (8) | |
| Residence | urban—province capital | 36.1 (43) | 38.8 (66) | 41.2 (101) | 39.3 (210) |
| other cities | 40.3 (48) | 37.6 (64) | 33.5 (82) | 36.3 (194) | |
| rural | 23.5 (28) | 23.5 (40) | 25.3 (62) | 24.3 (130) | |
| Education | university | 63.9 (76) | 64.2 (109) | 60.0 (147) | 62.2 (332) |
| other educational stages | 36.1 (43) | 35.8 (61) | 40.0 (98) | 37.8 (202) | |
| Professional activity | currently does not work | 18.5 (22) | 65.9 (112) | 81.2 (199) | 68.2 (364) |
| does not work professionally at all | 44.5 (53) | 13.5 (23) | 6.1 (15) | 11.2 (60) | |
| (she) works | 37.0 (44) | 20.6 (35) | 12.7 (31) | 20.8 (110) | |
| Relationship status | married/informal relationship | 89.1 (106) | 90.0 (153) | 92.7 (227) | 91.0 (486) |
| single | 10.9 (13) | 10.0 (17) | 7.3 (18) | 9.0 (48) | |
| Self-reported financial standing | good | 73.9 (88) | 74.7 (127) | 73.1 (179) | 73.8 (394) |
| bad | 26.1 (31) | 25.3 (43) | 26.9 (66) | 26.2 (140) | |
| Having children | no, it’s the first pregnancy | 58.8 (70) | 63.5 (108) | 69.4 (170) | 65.2 (348) |
| one child | 26.9 (32) | 28.8 (49) | 23.7 (58) | 26.0 (139) | |
| two or more children | 14.3 (17) | 7.7 (13) | 6.9 (17) | 8.8 (47) | |
| The person providing care | doctor | 67.2 (80) | 73.5 (125) | 66.9 (164) | 69.1 (369) |
| midwife | 5.9 (7) | 1.2 (2) | 0.4 (1) | 1.9 (10) | |
| doctor and midwife | 25.2 (30) | 24.1 (41) | 31.8 (78) | 27.9 (149) | |
| she was not under the care of a doctor/midwife | 1.7 (2) | 1.2 (2) | 0.8 (2) | 1.1 (6) | |
| Participation in Childbirth Classes | yes—face-to-face meeting with the midwife | 30.3 (36) | 18.8 (32) | 31.8 (78) | 27.3 (146) |
| yes—video- and teleconferences | 0.8 (1) | 10.0 (17) | 12.3 (30) | 9.0 (48) | |
| no, she did not have the opportunity/possibility | 5.9 (7) | 14.1 (24) | 25.7 (63) | 17.6 (94) | |
| no, she was not interested | 12.6 (15) | 23.5 (40) | 24.1 (59) | 21.3 (114) | |
| has not participated yet but would like to | 50.4 (60) | 33.5 (57) | 6.1 (15) | 24.7 (132) | |
| Pregnancy Trimester | Childbirth Anxiety | |||||||
| Anxiety as a State | Anxiety as a Trait | |||||||
| M | SD | M | SD | |||||
| I trimester | 40.97 | 8.46 | 40.97 | 8.77 | ||||
| II trimester | 41.12 | 9.24 | 42.35 | 8.63 | ||||
| III trimester | 42.40 | 8.42 | 42.20 | 8.75 | ||||
| Statistic | F = 1.58 p = 0.207 η2 = 0.01 | F = 1.03 p = 0.35 η2 = <0.01 | ||||||
| Anxiety Level | Pregnancy Trimester | |||||||
| I | II | III | ||||||
| % (n) | % (n) | % (n) | ||||||
| Low | 42.8 (51) | 37 (63) | 42 (103) | |||||
| Elevated | 11.8 (14) | 16.5 (28) | 15.5 (38) | |||||
| High | 15.1 (18) | 25.2 (30) | 14.7 (36) | |||||
| Very High | 30.3 (36) | 41.20 (49) | 27.8 (68) | |||||
| Statistic | Chi2 = 2.6868 p = 0.846 C = 0.07 | |||||||
| Pregnancy in the current epidemiological situation contributes to increased feelings of anxiety | I | II | III | |||||
| % (n) | % (n) | %(n) | ||||||
| Yes | 57.2 (68) | 56.5 (96) | 60 (147) | |||||
| No Opinion | 11.8 (14) | 13.5 (23) | 17.1 (42) | |||||
| No | 31.1 (37) | 30.0 (51) | 22.9 (56) | |||||
| Statistic | Chi2 = 43.5963 p = 0.008 C = 0.2747 | |||||||
| Completion of the pregnancy in accord with prior ideas/plans would lessen feelings of anxiety. | Opinion | |||||||
| Yes | No Opinion | No | ||||||
| Average Rank | Me | Average Rank | Me | Average Rank | Me | |||
| Childbirth Anxiety | 351.05 | 15.00 | 246.56 | 14.00 | 265.72 | 18.00 | ||
| Statistic | p = 0.004 | |||||||
| Source of Support/Factors | Pregnancy Trimester | Yes | No Opinion/ Not Applicable | No | Statistic |
|---|---|---|---|---|---|
| % (n) | % (n) | % (n) | |||
| In the current epidemiological situation, the support of the doctor in charge of the pregnancy was appropriate | I | 76.5 (91) | 16.8 (20) | 6.7 (8) | Chi2 = 10.2185 |
| II | 79.4 (135) | 7.6 (13) | 12.9 (22) | p = 0.036 | |
| III | 75.5 (185) | 9.8 (24) | 14.7 (36) | C = 0.1370 | |
| In the current epidemiological situation, the support of the midwife providing prenatal education was appropriate | I | 42.0 (50) | 52.9 (63) | 5.0 (6) | Chi2 = 28.9580 |
| II | 31.2 (53) | 52.9 (90) | 15.8 (27) | p = 7.972 | |
| III | 42.4 (104) | 34.7 (85) | 22.8 (56) | C = 0.2268 | |
| The support of loved ones (partner, family, friends) is important | I | 95.8 (114) | 3.4 (4) | 0.8 (1) | Chi2 = 11.0432 |
| II | 100 (170) | - | - | p = 0.026 | |
| III | 99.2 (243) | 0.8 (2) | - | C = 0.1423 | |
| I am receiving sufficient support from my loved ones | I | 91.6 (109) | 3.4 (4) | 5.0 (6) | Chi2 = 1.5008 |
| II | 90.6 (154) | 2.9 (5) | 6.5 (11) | p = 0.826 | |
| III | 89.4 (219) | 2.4 (6) | 8.2 (20) | C = 0.0529 | |
| My marital/partnership relations have an influence on the level of childbirth anxiety | I | 86.5 (103) | 7.6 (9) | 5.9 (7) | Chi2 = 7.1569 |
| II | 91.8 (156) | 4.1 (7) | 4.1 (7) | p = 0.127 | |
| III | 93.5 (229) | 2.0 (5) | 4.5 (11) | C = 0.1150 | |
| The presence of a companion during childbirth helps to lessen perinatal anxiety | I | 77.3 (92) | 13.4 (16) | 9.2 (12) | Chi2 = 10.0701 |
| II | 78.2 (133) | 18.8 (32) | 3.0 (5) | p = 0.089 | |
| III | 78.8 (193) | 13.9 (34) | 7.3 (18) | C = 0.1360 | |
| Birthing school/prenatal education prepares you for childbirth physically | I | 61.4 (73) | 25.2 (30) | 13.4 (16) | Chi2 = 16.5734 |
| II | 56.5 (96) | 33.5 (57) | 10.0 (17) | p = 0.002 | |
| III | 47.3 (116) | 29.4 (72) | 23.3 (57) | C = 0.1734 | |
| Birthing school/prenatal education prepares you for childbirth psychologically | I | 71.4 (85) | 21.0 (25) | 7.5 (9) | Chi2 = 2.7928 |
| II | 72.4 (123) | 22.9 (39) | 4.7 (8) | p = 0.593 | |
| III | 69.3 (170) | 21.6 (53) | 8.9 (22) | C= 0.0721 | |
| The subject of childbirth anxiety was brought up during meetings with the midwife/in birthing school | I | 33.6 (40) | 55.5 (66) | 10.9 (13) | Chi2 = 11.9339 |
| II | 34.7 (59) | 58.2 (99) | 7.1 (12) | p = 0.017 | |
| III | 45.7 (112) | 42.9 (105) | 11.5 (28) | C = 0.1478 | |
| Birthing school/prenatal education helps for coping with perinatal anxiety | I | 55.5 (66) | 32.8 (39) | 11.8 (14) | Chi2 = 0.7100 |
| II | 57.0 (97) | 34.1 (58) | 8.9 (15) | p = 0.950 | |
| III | 57.9 (140) | 33.1 (81) | 9.8 (24) | C = 0.0364 | |
| The subject of SARS-CoV-2 (coronavirus) was brought up during meetings/teleconferences with the family midwife or in classes at the birthing school | I | 16.8 (20) | 77.3 (92) | 9.36 (7) | Chi2 = 31.9594 |
| II | 17.6 (30) | 75.9 (129) | 13.37 (11) | p = 0.001 | |
| III | 36.7 (90) | 53.5 (131) | 19.27 (24) | C = 0.2376 | |
| The current epidemiological situation was discussed during meetings/video conferences with the family midwife or in classes at the birthing school | I | 17.6 (21) | 78.2 (98) | 1.7 (5) | Ch2 = 33.8456 |
| II | 18.2 (31) | 75.3 (128) | 1.8 (11) | p < 0.001 | |
| III | 38.8 (95) | 53.1 (130) | 4.1 (20) | C = 0.2441 | |
| Perinatal care has an influence on feelings of childbirth anxiety | I | 73.1 (87) | 21.0 (25) | 5.8 (7) | Chi2 = 10.4824 |
| II | 78.8 (134) | 18.8 (32) | 2.4 (4) | p = 0.033 | |
| III | 79.2 (194) | 12.7 (31) | 8.1 (20) | C = 0.1387 | |
| Knowing about the standards of perinatal care helps in coping with anxiety | I | 58.8 (70) | 31.1 (37) | 10.1 (12) | Chi2 = 18.2418 |
| II | 75.2 (128) | 15.9 (27) | 8.9 (15) | p = 0.001 | |
| III | 79.2 (194) | 13.1 (32) | 7.7 (19) | C = 0.1817 | |
| Concluding the pregnancy by means of Cesarean section would lessen anxiety | I | 31.1 (37) | 14.3 (17) | 54.6 (65) | Chi2 = 5.0353 |
| II | 26.4 (45) | 22.4 (38) | 51.2 (87) | p = 0.283 | |
| III | 23.3 (57) | 19.2 (47) | 57.5 (141) | C = 0.0966 |
| Sources of Support | ||||||
| Psychological Condition | Loved Ones | Attending Physician | Family Midwife Providing Prenatal Education | |||
| Average Rank | Me | Average Rank | Me | Average Rank | Me | |
| Bad | 208.04 | 4.00 | 228.13 | 4.00 | 226.22 | 3.00 |
| Good | 283.64 | 5.00 | 278.19 | 4.00 | 278.70 | 3.00 |
| Statistic | Z = −5.16 | p = 0.001 | Z = −3.27 | p = 0.001 | Z = −3.40 | p = 0.001 |
| Physical Condition | Loved Ones | Attending Physician | Family midwife providing prenatal education | |||
| Average Rank | Me | Average Rank | Me | Average Rank | Me | |
| Bad | 261.43 | 4.00 | 249.70 | 4.00 | 241.72 | 3.00 |
| Good | 272.42 | 5.00 | 281.92 | 4.00 | 288.38 | 3.00 |
| Statistic | Z = −0.91 | p = 0.363 | Z = −2.56 | p = 0.011 | Z = −3.67 | p < 0.001 |
| Factors Affecting Childbirth Anxiety | ||||||
| Manner of pregnancy conclusion | Perinatal care and Birthing school | Pregnancy in the current epidemiological situation contributes to increased feelings of anxiety | Concluding the pregnancy by meansof Cesarean section would lessen anxiety | |||
| M | SD | M | SD | M | SD | |
| Not Applicable | 22.69 | 3.50 | 3.65 | 1.20 | 2.48 | 1.31 |
| Delivery without Complications | 22.15 | 4.24 | 3.17 | 1.37 | 2.01 | 1.21 |
| Delivery with Complications | 22.25 | 3.96 | 3.50 | 1.33 | 3.12 | 1.48 |
| Statistic | F = 1.09 | p = 0.336 | F = 5.34 | p = 0.005 | F = 19.95 | p < 0.001 |
| Participation in Childbirth Classes | Perinatal care and Birthing school | Pregnancy in the current epidemiological situation contributes to increased feelings of anxiety | Concluding the pregnancy by means of Cesarean section would lessen anxiety | |||
| M | SD | M | SD | M | SD | |
| Yes | 24.13 | 3.76 | 3.58 | 1.25 | 2.46 | 1.39 |
| No | 21.60 | 3.37 | 3.49 | 1.29 | 2.58 | 1.38 |
| Statistic | T = 7.98 | p < 0.001 | T = 0.80 | p = 0.426 | T = −0.95 | p = 0.341 |
| Psychological Condition | Childbirth Anxiety | |||
| Anxiety as a State | Anxiety as a Trait | |||
| M | SD | M | SD | |
| Bad | 48.75 | 7.38 | 49.23 | 6.46 |
| Good | 39.75 | 8.03 | 40.00 | 8.20 |
| Statistic | T = 10.80 | p < 0.001 | T = 12.72 | p < 0.001 |
| Physical Condition | Anxiety as a State | Anxiety as a Trait | ||
| M | SD | M | SD | |
| Bad | 44.13 | 8.57 | 44.95 | 8.30 |
| Good | 39.68 | 8.32 | 39.55 | 8.31 |
| Statistic | T = 6.05 | p < 0.001 | T = 7.48 | p < 0.001 |
| The course of the previous birth | Anxiety as a State | ANXIETY AS A Trait | ||
| M | SD | M | SD | |
| Not Applicable | 41.57 | 8.42 | 42.12 | 8.67 |
| Delivery without Complications | 41.79 | 8.62 | 41.76 | 8.78 |
| Delivery with Complications | 41.84 | 9.52 | 41.77 | 8.86 |
| Statistic | F = 0.05 | p = 0.948 | F = 0.10 | p = 0.901 |
| Participation in Childbirth Classes | Anxiety as a State | Anxiety as a Trait | ||
| M | SD | M | SD | |
| Yes | 41.21 | 9.04 | 40.80 | 8.77 |
| No | 41.94 | 8.52 | 42.64 | 8.63 |
| Statistic | T = −0.92 | p = 0.356 | T = −2.35 | p = 0.019 |
| Factors | Anxiety as a State | Anxiety as a Trait | |
|---|---|---|---|
| Support during the current epidemiological situation from the OB-GYN treating the pregnancy | r | −0.15 | −0.17 |
| p | <0.001 | <0.001 | |
| Support during the current epidemiological situation from a family midwife providing prenatal education | r | −0.13 | −0.18 |
| p | 0.002 | <0.001 | |
| Maternal experience | rho | 0.01 | −0.02 |
| p | 0.882 | 0.628 | |
| Number of pregnancies | rho | 0.02 | −0.01 |
| p | 0.653 | 0.860 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Iwanowicz-Palus, G.; Mróz, M.; Korda, A.; Marcewicz, A.; Palus, A. Perinatal Anxiety among Women during the COVID-19 Pandemic—A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2022, 19, 2603. https://doi.org/10.3390/ijerph19052603
Iwanowicz-Palus G, Mróz M, Korda A, Marcewicz A, Palus A. Perinatal Anxiety among Women during the COVID-19 Pandemic—A Cross-Sectional Study. International Journal of Environmental Research and Public Health. 2022; 19(5):2603. https://doi.org/10.3390/ijerph19052603
Chicago/Turabian StyleIwanowicz-Palus, Grażyna, Mariola Mróz, Aleksandra Korda, Agnieszka Marcewicz, and Agnieszka Palus. 2022. "Perinatal Anxiety among Women during the COVID-19 Pandemic—A Cross-Sectional Study" International Journal of Environmental Research and Public Health 19, no. 5: 2603. https://doi.org/10.3390/ijerph19052603
APA StyleIwanowicz-Palus, G., Mróz, M., Korda, A., Marcewicz, A., & Palus, A. (2022). Perinatal Anxiety among Women during the COVID-19 Pandemic—A Cross-Sectional Study. International Journal of Environmental Research and Public Health, 19(5), 2603. https://doi.org/10.3390/ijerph19052603






