Challenges Experienced by Italian Nursing Home Staff in End-of-Life Conversations with Family Caregivers during COVID-19 Pandemic: A Qualitative Descriptive Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Research Design
2.2. Setting and Recruitment
2.3. Participants
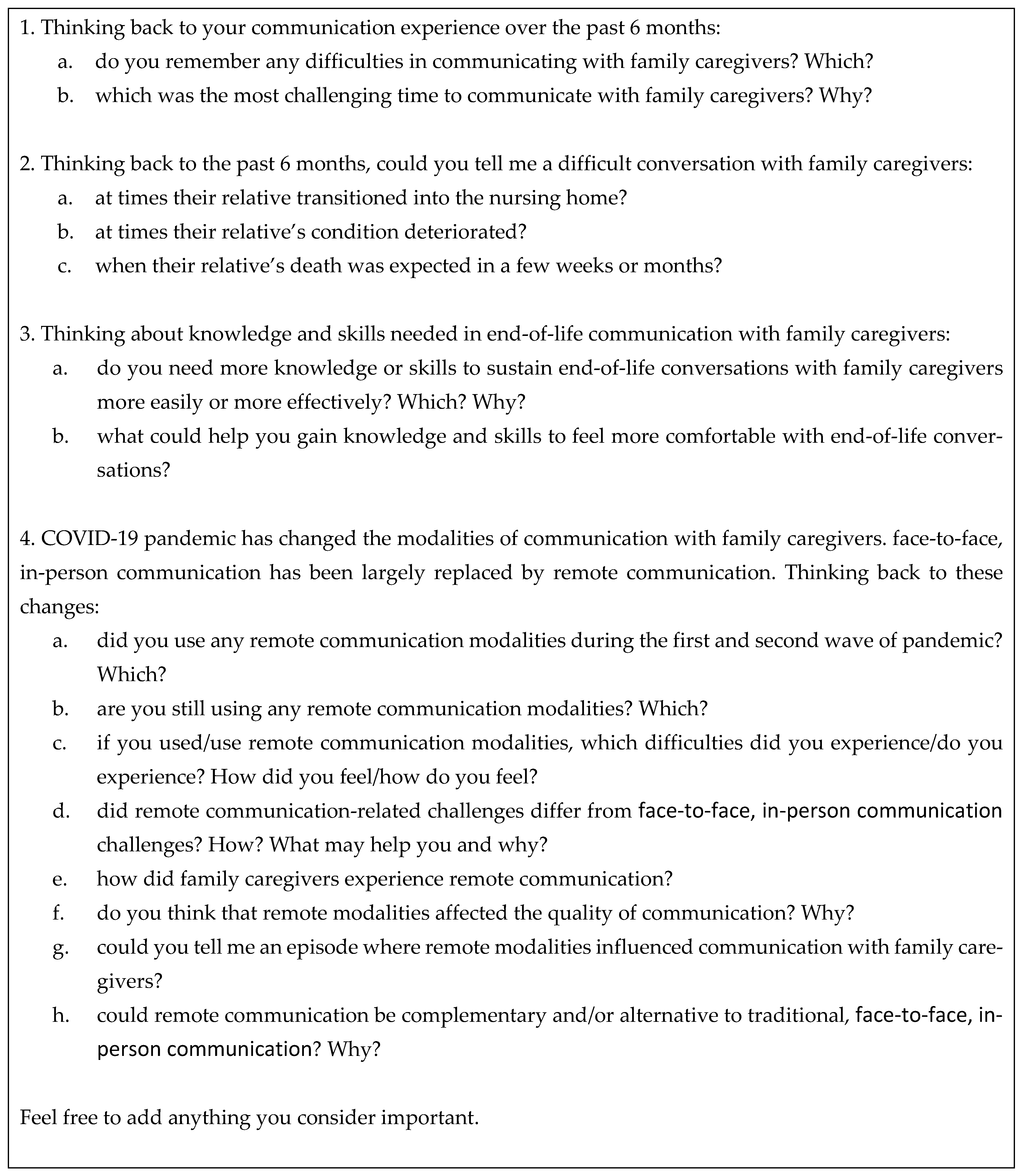
2.4. Data Collection
2.5. Transcription and Qualitative Data Analysis
2.6. Rigor and Trustworthiness
2.7. Quantitative Data Analysis
2.8. Ethical Considerations
3. Results
3.1. Theme 1. Communicating with Family Caregivers over the Overall Disease Trajectory
“The most important skill is adjusting to the person in front of you […], my role requires me to be supportive and welcoming.”(NH4/NH manager)
“Professionalism is having a full understanding of the situation, not only what happens during your shift […]. Thus, if they [FCs] ask me for advice you can provide the right guidance.”(NH5/nurse)
“We funnel communication into a contact person to avoid saying things that should not be said or are incorrect. When you give wrong information, you create fear. Therefore, communication should be centralized on specific figures who are responsible for interacting with and updating FCs.”(NH6/chief medical officer)
“Sometimes they [FCs] feel really guilty for leaving their relative here and not being close to them, and therefore we must reassure them, they need this.”(NH3/nurse)
“For me, to call and say, ‘Conditions are deteriorating’ or ‘Something is going wrong’, that’s the hardest time. I’d prefer that other colleagues do this communication”(NH4/NH manager)
“There’s a feeling of accomplishment, it’s not possible to go back so you really have to make the effort to get through that moment and give them [FCs] what they need. I think that’s the hardest part of the journey for me.”(NH2/chief medical officer)
“Before COVID it was easier, now it is less. Before we said ‘Come to the facility, let’s have a meeting all together with the head nurse, the physician and the chief medical officer and let’s try to make a picture’. Now it is more difficult to organize these meetings and it has become harder to make FCs accept death.”(NH5/NH manager)
3.2. Theme 2. Managing Challenging Emotions and Situations
“We have great difficulties with relatives of persons with dementia. They often have not realized yet the situation of their loved one, that there is a cognitive decay and disease progresses even if we are doing everything we can. Some people do not want to understand and communication becomes extremely difficult.”(NH6/psychologist)
“The daughter said ‘I was expecting a phone call every day’ and I calmy replied ‘It’s not possible call every day’. Then we shared that usually we don’t call FCs if no issues occur; we call FCs when something is going wrong or changing”.(NH6/chief nurse)
“The expectations of FCs are very high, so especially at the end of the meeting I underline the limits of the structure and difficulties that are likely to arise to prevent unfulfilled expectations from leading to aggressive behaviors”.(NH2/NH manager)
“Almost everyone asks: ‘How much time is left?’ And you don’t know what to answer because they [residents] often get worse, then stabilize, and sometimes they even seem to recover a little”.(NH2, head nurse)
“During pandemic it has been really hard. In usual conditions as it was some years ago, FCs could be angry but then they could enter the facility and see, you could explain and show them all that you had done and all that was still continuing to be done. Finally, they took confidence and also changed their behaviors. All of this was no more possible during COVID.”(NH6/chief nurse)
“When you have elderly parents as I have, you really feel involved. That resident may be you mum or dad … at that moment there is a very strong transfer in reverse. You really live it in a heavy way, you can’t detach anymore.”(NH2/psychologist)
“Some children wanted to see their relatives even though they were almost in coma. It was very challenging for me to make this video call and mediate between children and the dying resident”.(R5/educator)
“The FC often does not have a real understanding of what’s going on […]. It’s actually a lot of little signals that come through, so we need to say ‘Your mum/father needs some help now to eat’. I mean, we need to point out all the little signals that occur. We need to accompany FCs towards a new vision of their relative and this is a hard transition.”(NH2/psychologist)
“Everyone should recognize their role: which information could I provide if I’m asked? Only that concerning my role. This stuff creates so many problems. All professionals should be aware of their limits; I can answer up to a certain point, then I refer to the responsible person […] Thus, boundaries among roles are recognized. This is pivotal to provide right communication, what you say is correct within your scope, you don’t create confusion.”(NH5/NH manager)
“Administrative staff do not have to explain anything to FCs since they do not know anything but are intermediary, they have to learn how to mediate […]. This position is important if we want to establish good relationships with FCs.”(NH3/chief medical officer)
3.3. Theme 3. Establishing a Partnership between Healthcare Professionals and Family Caregivers
“Some FCs desire updating about the clinical health status and everything else is secondary. Others want to be informed about daily routine, if the mom has eaten, slept … and still others want to be reassured that their relative does not feel abandoned. We have to avoid mixing the plans and provide FCs what they need.”(NH3/chief medical officer)
“The relationship built with FCs over years is essential. If you establish good relationships, then when you get to the epilogue, death is peaceful with no aftermath. Short stays are more difficult because you haven’t had the time to build any relationships.”(NH2/NH manager)
“It happens that you have to fight with the doctors because they say, ‘She had a seizure, now we’ll bring her to the hospital to do a CT scan to figure out …’. ‘No’ I reply ‘once we’ve done the CT scan, the MRI and all the examinations, what do we do? Will she have surgery? No…’. So, we care for her humanely. To hospitalize means leaving them dying alone.”(NH1/NH manager)
“Initially they [FCs] say ‘Let’s do it, let’s do all what we can, let’s go to the hospital”, then as years pass, they [FCs] acknowledge disease-related suffering and tell you ‘If possible we would like (s)he stays here among people (s)he knows and we are able to stay with her/him as well”.(NH4/NH manager)
“Time really lacks, time is tyrant. If we had the opportunity to have more time, we would speak more with FCs and achieve solutions faster. When there is communication you are halfway there.”(NH6/chief nurse)
3.4. Theme 4. Addressing Healthcare Professionals’ Communication Skills and Training Needs
“I communicate well with FCs because I had the same experience with my parents, thereby I understand how they feel and know what they want to hear, what they need.”(NH6/chief nurse aide)
“I thought of myself as I was many years ago and of myself as I am now. Now I feel more useful because I have experience of things already seen and experienced. It is a matter of experience that has been gained in the field”.(NH6/psychologist)
“I’d like to take classes on how to engage with angry FCs. It is not easy to say the right words or have the right attitudes when someone is angry because of a feeling of helplessness. It is not easy to manage and contain such feeling of helplessness.”(NH5/nurse aide)
“I strongly believe in case-based discussions in team. We start from the specific case to reflect on how we behaved and if we could have behaved differently, also as a warning for the future.”(NH2/NH manager)
“I remember a course I did, we were few and it was nice because it gave me the opportunity to confront with my colleagues and make a sort of exchange.”(NH5/nurse aide)
“We recently did a course on communication in the form of role-plays. There was a trained actress on what she had to say. […] It gave me several ideas on how managing meetings with FCs, it gave me a mental outline to move. Obviously, every meeting is unique but a practical basis to start is useful.”(NH5/chief nurse aide)
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Pfeifer, M.; Head, B.A. Which critical communication skills are essential for interdisciplinary end-of-life discussions? AMA J. Ethics 2018, 20, 724–731. [Google Scholar] [CrossRef]
- Raijmakers, N.J.; van Zuylen, L.; Costantini, M.; Caraceni, A.; Clark, J.B.; De Simone, G.; Lundquist, G.; Voltz, R.; Ellershaw, J.E.; van der Heide, A. Issues and needs in end-of-life decision making: An international modified Delphi study. Palliat. Med. 2012, 26, 947–953. [Google Scholar] [CrossRef] [PubMed]
- Gonella, S.; Basso, I.; Dimonte, V.; Martin, B.; Berchialla, P.; Campagna, S.; Di Giulio, P. Association Between End-of-life conversations in nursing homes and end-of-life care outcomes: A systematic review and meta-analysis. J. Am. Med. Dir. Assoc. 2019, 20, 249–261. [Google Scholar] [CrossRef] [PubMed]
- Street, R.L., Jr.; Makoul, G.; Arora, N.K.; Epstein, R.M. How does communication heal? Pathways linking clinician–patient communication to health outcomes. Patient Educ. Couns. 2009, 74, 295–301. [Google Scholar] [CrossRef] [PubMed]
- Sanders, J.J.; Curtis, J.R.; Tulsky, J.A. Achieving goal-concordant care: A conceptual model and approach to measuring serious illness communication and its impact. J. Palliat. Med. 2018, 21, S17–S27. [Google Scholar] [CrossRef] [PubMed]
- Teno, J.M.; Clarridge, B.R.; Casey, V.; Welch, L.C.; Wetle, T.; Shield, R.; Mor, V. Family perspectives on end-of-life care at the last place of care. JAMA 2004, 291, 88–93. [Google Scholar] [CrossRef] [PubMed]
- Sinuff, T.; Dodek, P.; You, J.J.; Barwich, D.; Tayler, C.; Downar, J.; Hartwick, M.; Frank, C.; Stelfox, H.T.; Heyland, D.K. Improving end-of-life communication and decision making: The development of a conceptual framework and quality indicators. J. Pain Symptom Manag. 2015, 49, 1070–1080. [Google Scholar] [CrossRef]
- Dy, S.M.; Kiley, K.B.; Ast, K.; Lupu, D.; Norton, S.A.; McMillan, S.C.; Herr, K.; Rotella, J.D.; Casarett, D.J. Measuring what matters: Top-ranked quality indicators for hospice and palliative care from the American Academy of Hospice and Palliative Medicine and Hospice and Palliative Nurses Association. J. Pain Symptom Manag. 2015, 49, 773–781. [Google Scholar] [CrossRef]
- van der Steen, J.T.; Radbruch, L.; Hertogh, C.M.; de Boer, M.E.; Hughes, J.C.; Larkin, P.; Francke, A.L.; Jünger, S.; Gove, D.; Firth, P.; et al. White paper defining optimal palliative care in older people with dementia: A Delphi study and recommendations from the European Association for Palliative Care. Palliat. Med. 2014, 28, 197–209. [Google Scholar] [CrossRef]
- Bowman, P.; Slusser, K.; Allen, D. Collaborative practice model: Improving the delivery of bad news. Clin. J. Oncol. Nurs. 2018, 22, 23–27. [Google Scholar] [CrossRef]
- Harrison Dening, K. Advance Care Planning in Dementia; All Ireland Institute of Hospice and Palliative Care: Dublin, Ireland, 2016; Video: 39.54 min; Available online: http://www.professionalpalliativehub.com/resource-centre/palliative-care-neurodegeneration-advance-care-planning-dementia (accessed on 15 November 2021).
- Gjerberg, E.; Lillemoen, L.; Førde, R.; Pedersen, R. End-of-life care communications and shared decision-making in Norwegian nursing homes—Experiences and perspectives of patients and relatives. BMC Geriatr. 2015, 15, 103. [Google Scholar] [CrossRef] [PubMed]
- Hancock, K.; Clayton, J.M.; Parker, S.M.; Wal der, S.; Butow, P.N.; Carrick, S.; Currow, D.; Ghersi, D.; Glare, P.; Hagerty, R.; et al. Truth-telling in discussing prognosis in advanced life-limiting illnesses: A systematic review. Palliat. Med. 2007, 21, 507–517. [Google Scholar] [CrossRef] [PubMed]
- Almack, K.; Cox, K.; Moghaddam, N.; Pollock, K.; Seymour, J. After you: Conversations between patients and healthcare professionals in planning for end of life care. BMC Palliat. Care 2012, 11, 15. [Google Scholar] [CrossRef] [PubMed]
- Bergenholtz, H.; Timm, H.U.; Missel, M. Talking about end of life in general palliative care—What’s going on? A qualitative study on end-of-life conversations in an acute care hospital in Denmark. BMC Palliat. Care 2019, 18, 62. [Google Scholar] [CrossRef]
- De Vleminck, A.; Pardon, K.; Beernaert, K.; Deschepper, R.; Houttekier, D.; Van Audenhove, C.; Deliens, L.; Stichele, R.V. Barriers to advance care planning in cancer, heart failure and dementia patients: A focus group study on general practitioners’ views and experiences. PLoS ONE 2014, 9, e84905. [Google Scholar] [CrossRef]
- Schonfeld, T.L.; Stevens, E.A.; Lampman, M.A.; Lyons, W.L. Assessing challenges in end-of-life conversations with elderly patients with multiple morbidities. Am. J. Hosp. Palliat. Med. 2012, 29, 260–267. [Google Scholar] [CrossRef]
- Gonella, S.; Basso, I.; Clari, M.; Dimonte, V.; Di Giulio, P. A qualitative study of nurses’ perspective about the impact of end-of-life communication on the goal of end-of-life care in nursing home. Scand. J. Caring Sci. 2021, 35, 502–511. [Google Scholar] [CrossRef]
- Pino, M.; Parry, R.; Land, V.; Faull, C.; Feathers, L.; Seymour, J. Engaging terminally ill patients in end of life talk: How experienced palliative medicine doctors navigate the dilemma of promoting discussions about dying. PLoS ONE 2016, 11, e0156174. [Google Scholar] [CrossRef]
- Travers, A.; Taylor, V. What are the barriers to initiating end-of-life conversations with patients in the last year of life? Int. J. Palliat. Nurs. 2016, 22, 454–462. [Google Scholar] [CrossRef]
- Rubinelli, S.; Myers, K.; Rosenbaum, M.; Davis, D. Implications of the current COVID-19 pandemic for communication in healthcare. Patient Educ. Couns. 2020, 103, 1067–1069. [Google Scholar] [CrossRef]
- Mitchinson, L.; Dowrick, A.; Buck, C.; Hoernke, K.; Martin, S.; Vanderslott, S.; Robinson, H.; Rankl, F.; Manby, L.; Lewis-Jackson, S.; et al. Missing the human connection: A rapid appraisal of healthcare workers’ perceptions and experiences of providing palliative care during the COVID-19 pandemic. Palliat. Med. 2021, 35, 852–861. [Google Scholar] [CrossRef] [PubMed]
- Hanna, J.R.; Rapa, E.; Dalton, L.J.; Hughes, R.; Quarmby, L.M.; McGlinchey, T.; Donnellan, W.J.; Bennett, K.M.; Mayland, C.R.; Mason, S.R. Health and social care professionals’ experiences of providing end of life care during the COVID-19 pandemic: A qualitative study. Palliat. Med. 2021, 35, 1249–1257. [Google Scholar] [CrossRef]
- Batra, K.; Singh, T.P.; Sharma, M.; Batra, R.; Schvaneveldt, N. Investigating the psychological impact of COVID-19 among healthcare workers: A meta-analysis. Int. J. Environ. Res. Public Health 2020, 17, 9096. [Google Scholar] [CrossRef] [PubMed]
- Smaling, H.J.A.; Tilburgs, B.; Achterberg, W.P.; Visser, M. The impact of social distancing due to the COVID-19 pandemic on people with dementia, family carers and healthcare professionals: A qualitative study. Int. J. Environ. Res. Public Health 2022, 19, 519. [Google Scholar] [CrossRef] [PubMed]
- Hado, E.; Feinberg, L.F. Amid the COVID-19 pandemic, meaningful communication between family caregivers and residents of long-term care facilities is imperative. J. Aging Soc. Policy 2020, 32, 410–415. [Google Scholar] [CrossRef] [PubMed]
- Sandelowski, M. Whatever happened to qualitative description? Res. Nurs. Health 2000, 23, 334–340. [Google Scholar] [CrossRef]
- Tong, A.; Sainsbury, P.; Craig, J. Consolidated criteria for reporting qualitative research (COREQ): A 32-item checklist for interviews and focus groups. Int. J. Qual. Health Care 2007, 19, 349–357. [Google Scholar] [CrossRef]
- Guest, G.; Bunce, A.; Johnson, L. How many interviews are enough? An experiment with data saturation and variability. Field Methods 2006, 18, 59–82. [Google Scholar] [CrossRef]
- Anderson, R.J.; Bloch, S.; Armstrong, M.; Stone, P.; Low, J. Communication between healthcare professionals and relatives of patients approaching the end-of-life: A systematic review of qualitative evidence. Palliat. Med. 2019, 33, 926–941. [Google Scholar] [CrossRef]
- Moir, C.; Roberts, R.; Martz, K.; Perry, J.; Tivis, L.J. Communicating with patients and their families about palliative and end-of-life care: Comfort and educational needs of nurses. Int. J. Palliat. Nurs. 2015, 21, 109–112. [Google Scholar] [CrossRef]
- Braun, V.; Clarke, V. Using thematic analysis in psychology. Qual. Res. Psychol. 2006, 3, 77–101. [Google Scholar] [CrossRef]
- Morse, J.M. Critical analysis of strategies for determining rigor in qualitative inquiry. Qual. Health Res. 2015, 25, 1212–1222. [Google Scholar] [CrossRef] [PubMed]
- Holloway, I.; Galvin, K. Qualitative Research in Nursing and Healthcare; John Wiley & Sons: Hoboken, NJ, USA, 2016. [Google Scholar]
- Konietzny, C.; Kaasalainen, S.; Haas, V.D.-B.; Merla, C.; Te, A.; Di Sante, E.; Kalfleish, L.; Hadjistavropoulos, T. Muscled by the system: Informal caregivers’ experiences of transitioning an older adult into long-term care. Can. J. Aging/La Rev. Can. Vieil. 2018, 37, 464–473. [Google Scholar] [CrossRef] [PubMed]
- Merla, C.; Wickson-Griffiths, A.; Kaasalainen, S.; Bello-Haas, V.D.; Banfield, L.; Hadjistavropoulos, T.; Di Sante, E. Perspective of family members of transitions to alternative levels of care in Anglo-Saxon countries. Curr. Gerontol. Geriatr. Res. 2018, 2018, 4892438. [Google Scholar] [CrossRef]
- mySupport Study. Scaling up the Family Carer Decision Support Intervention: A Transnational Effectiveness-Implementation Evaluation. 2019–2022. Available online: https://mysupportstudy.eu (accessed on 14 December 2021).
- Toles, M.; Song, M.-K.; Lin, F.-C.; Hanson, L.C. Perceptions of family decision-makers of nursing home residents with advanced dementia regarding the quality of communication around end-of-life care. J. Am. Med. Dir. Assoc. 2018, 19, 879–883. [Google Scholar] [CrossRef]
- Melin-Johansson, C.; Sveen, J.; Lövgren, M.; Udo, C. A third of dying patients do not have end-of-life discussions with a physician: A nationwide registry study. Palliat. Support. Care 2021, 1–6. [Google Scholar] [CrossRef]
- Reinke, L.F.; Feemster, L.C.; McDowell, J.; Gunnink, E.; Tartaglione, E.V.; Udris, E.; Curtis, J.R.; Au, D.H. The long term impact of an end-of-life communication intervention among veterans with COPD. Heart Lung 2017, 46, 30–34. [Google Scholar] [CrossRef]
- Miralles, O.; Sanchez-Rodriguez, D.; Marco, E.; Annweiler, C.; Baztan, A.; Betancor, É.; Cambra, A.; Cesari, M.; Fontecha, B.J.; Gąsowski, J.; et al. Unmet needs, health policies, and actions during the COVID-19 pandemic: A report from six European countries. Eur. Geriatr. Med. 2020, 12, 193–204. [Google Scholar] [CrossRef]
- Wammes, J.D.; Kolk, M.D.; van den Besselaar Md, J.H.; MacNeil-Vroomen Ph, D.J.; Buurman-van Es Rn, B.M.; van Rijn Ph, D.M. Evaluating perspectives of relatives of nursing home residents on the nursing home visiting restrictions during the COVID-19 crisis: A Dutch cross-sectional survey study. J. Am. Med. Dir. Assoc. 2020, 21, 1746–1750.e3. [Google Scholar] [CrossRef]
- Zmora, R.; Statz, T.L.; Birkeland, R.W.; McCarron, H.R.; Finlay, J.M.; Rosebush, C.E.; Gaugler, J.E. Transitioning to long-term care: Family caregiver experiences of dementia, communities, and counseling. J. Aging Health 2021, 33, 133–146. [Google Scholar] [CrossRef]
- Childers, J.W.; Back, A.L.; Tulsky, J.A.; Arnold, R.M. REMAP: A framework for goals of care conversations. J. Oncol. Pract. 2017, 13, e844–e850. [Google Scholar] [CrossRef] [PubMed]
- Haley, E.M.; Meisel, D.; Gitelman, Y.; Dingfield, L.; Casarett, D.J.; O’Connor, N.R. Electronic goals of care alerts: An innovative strategy to promote primary palliative care. J. Pain Symptom Manag. 2017, 53, 932–937. [Google Scholar] [CrossRef] [PubMed]
- VitalTalk. VitalTalk Makes Communication Skills for Serious Illness Learnable. Available online: https://www.vitaltalk.org/ (accessed on 22 October 2021).
- Valdimarsdóttir, U.; Helgason Ásgeir, R.; Fürst, C.-J.; Adolfsson, J.; Steineck, G. Awareness of husband’s impending death from cancer and long-term anxiety in widowhood: A nationwide follow-up. Palliat. Med. 2004, 18, 432–443. [Google Scholar] [CrossRef] [PubMed]
- Cagle, J.G.; Unroe, K.T.; Bunting, M.; Bernard, B.L.; Miller, S.C. Caring for dying patients in the nursing home: Voices from frontline nursing home staff. J. Pain Symptom Manag. 2017, 53, 198–207. [Google Scholar] [CrossRef]
- Brighton, L.J.; Selman, L.E.; Bristowe, K.; Edwards, B.; Koffman, J.; Evans, C.J. Emotional labour in palliative and end-of-life care communication: A qualitative study with generalist palliative care providers. Patient Educ. Couns. 2019, 102, 494–502. [Google Scholar] [CrossRef]
- Borghi, L.; Meyer, E.C.; Vegni, E.; Oteri, R.; Almagioni, P.; Lamiani, G. Twelve years of the Italian Program to Enhance Relational and Communication Skills (PERCS). Int. J. Environ. Res. Public Health 2021, 18, 439. [Google Scholar] [CrossRef]
- James, H.; Crawford, G.B. Healthcare interpreters and difficult conversations: A survey. BMJ Support. Palliat. Care 2021. [Google Scholar] [CrossRef]
- Gonella, S.; Basso, I.; De Marinis, M.G.; Campagna, S.; Di Giulio, P. Good end-of-life care in nursing home according to the family carers’ perspective: A systematic review of qualitative findings. Palliat. Med. 2019, 33, 589–606. [Google Scholar] [CrossRef]
- Toscani, F.; Farsides, C. Deception, catholicism, and hope: Understanding problems in the communication of unfavorable prognoses in traditionally-catholic countries. Am. J. Bioeth. 2006, 6, W6–W18. [Google Scholar] [CrossRef]
- Bern-Klug, M. A conceptual model of family surrogate end-of-life decision-making process in the nursing home setting: Goals of care as guiding stars. J. Soc. Work End-of-Life Palliat. Care 2014, 10, 59–79. [Google Scholar] [CrossRef]
- Morrison, R.S.; Meier, D.E.; Arnold, R.M. What’s wrong with advance care planning? JAMA 2021, 326, 1575–1576. [Google Scholar] [CrossRef] [PubMed]
- Anziani e pandemia. Geriatri: “Rsa, Piano Vaccinale Battaglia Vinta. Ma serve un Geriatra in Ogni Struttura”. Available online: https://www.quotidianosanita.it/lavoro-e-professioni/articolo.php?articolo_id=101864 (accessed on 28 January 2022).
- Dixon, J.; Knapp, M. Whose job? The staffing of advance care planning support in twelve international healthcare organizations: A qualitative interview study. BMC Palliat. Care 2018, 17, 78. [Google Scholar] [CrossRef] [PubMed]
- Evenblij, K.; Koppel, M.T.; Smets, T.; Widdershoven, G.A.M.; Onwuteaka-Philipsen, B.D.; Pasman, H.R.W. Are care staff equipped for end-of-life communication? A cross-sectional study in long-term care facilities to identify determinants of self-efficacy. BMC Palliat. Care 2019, 18, 1. [Google Scholar] [CrossRef] [PubMed]
- Mitchell, S.L.; Teno, J.M.; Kiely, D.K.; Shaffer, M.L.; Jones, R.; Prigerson, H.G.; Volicer, L.; Givens, J.L.; Hamel, M.B. The clinical course of advanced dementia. N. Engl. J. Med. 2009, 361, 1529–1538. [Google Scholar] [CrossRef] [PubMed]
- Smedbäck, J.; Öhlén, J.; Årestedt, K.; Alvariza, A.; Fürst, C.-J.; Håkanson, C. Palliative care during the final week of life of older people in nursing homes: A register-based study. Palliat. Support. Care 2017, 15, 417–424. [Google Scholar] [CrossRef]
- Thompson, G.N.; McClement, S.; Menec, V.H.; Chochinov, H.M. Understanding bereaved family members’ dissatisfaction with end-of-life care in nursing homes. J. Gerontol. Nurs. 2012, 38, 49–60. [Google Scholar] [CrossRef]
- Anstey, S.; Powell, T.; Coles, B.; Hale, R.; Gould, D. Education and training to enhance end-of-life care for nursing home staff: A systematic literature review. BMJ Support. Palliat. Care 2016, 6, 353–361. [Google Scholar] [CrossRef]
- Brighton, L.J.; Koffman, J.; Hawkins, A.; McDonald, C.; O’Brien, S.; Robinson, V.; Khan, S.A.; George, R.; Higginson, I.J.; Selman, L.E. A systematic review of end-of-life care communication skills training for generalist palliative care providers: Research quality and reporting guidance. J. Pain Symptom Manag. 2017, 54, 417–425. [Google Scholar] [CrossRef]
- Chung, H.-O.; Oczkowski, S.J.W.; Hanvey, L.; Mbuagbaw, L.; You, J.J. Educational interventions to train healthcare professionals in end-of-life communication: A systematic review and meta-analysis. BMC Med. Educ. 2016, 16, 131. [Google Scholar] [CrossRef]
- Grabowski, D.C.; O’malley, A.J.; Afendulis, C.C.; Caudry, D.J.; Elliot, A.; Zimmerman, S. Culture change and nursing home quality of care. Gerontologist 2014, 54, S35–S45. [Google Scholar] [CrossRef]
- Nilsen, P.; Wallerstedt, B.; Behm, L.; Ahlström, G. Towards evidence-based palliative care in nursing homes in Sweden: A qualitative study informed by the organizational readiness to change theory. Implement. Sci. 2018, 13, 1. [Google Scholar] [CrossRef] [PubMed]
| Characteristics | N |
|---|---|
| STRUCTURE VARIABLES | |
| Private/public NH | 4/2 |
| Number of beds available, mean (range) | 81 (37–122) |
| ≤60 | 2 |
| 61–119 | 3 |
| ≥120 | 1 |
| Number of beds for functionally independent residents, mean (range) | 12.4 (0–40) |
| Number of beds for functionally dependent residents, mean (range) | 57.7 (14–122) |
| Alzheimer unit | 2 |
| Facilities with beds of palliative care continuity | 1 |
| Staffing, full-time equivalent, mean (SD) | |
| Nurse aide | 39.0 (22.0) |
| Nurse | 5.7 (2.8) |
| Physiotherapist | 1.02 (0.21) |
| Physician | 0.7 (0.5) |
| Educator | 0.66 (0.51) |
| Psychologist | 0.5 (0.2) |
| PROCESS VARIABLES | |
| Presence of written procedures on | |
| how to welcome residents and their families at admission | 6 |
| how to communicate resident’s clinical deterioration and/or end-of-life conditions | 5 |
| pain management in cognitively competent residents | 6 |
| pain management in cognitively impaired residents | 2 |
| bereavement management | 3 |
| Meetings with family caregivers | |
| when a resident’s condition worsens | 6 |
| to explore family caregivers’ preferences for end-of-life care | 5 |
| to explore their spiritual needs | 4 |
| to present the opportunity to activate the palliative care service in the 6 months before the study start | 4 |
| to present the opportunity of hospice referral in the 6 months before the study start | - |
| Meetings with residents | |
| to explore their preferences for end-of-life care | 4 |
| to explore their spiritual needs | 4 |
| Documentation of residents’ and/or family caregivers preferences for end-of-life care | 4 |
| Availability of a priest on regular basis | 6 |
| Availability to reach other spiritual guides on request | 4 |
| Figures involved in answering family caregivers’ concerns during the facility selection | |
| NH director | 6 |
| Chief medical officer | 6 |
| Nurse | 6 |
| Administrative staff | 2 |
| Figures involved in updating the care plan | |
| Chief medical officer | 6 |
| Nurse | 6 |
| Family caregivers | 6 |
| Psychologist | 2 |
| Nurse aide | 2 |
| Physiotherapist | 1 |
| Figures involved in communicating a resident’s clinical deterioration to family caregivers | |
| Chief medical officer | 4 |
| Nurse | 3 |
| NH director | 2 |
| OUTCOME VARIABLES | |
| Referral of residents to palliative care services in the 6 months before study start | 1 |
| Extra activities | |
| Pet therapy | 4 |
| Music therapy | 3 |
| Occupational therapy | 3 |
| Bio-dance | 2 |
| Board games | 2 |
| Others a | 3 |
| Healthcare Professionals (n = 21) | N |
|---|---|
| Female gender | 17 |
| Age, years, mean (range) | 50 (25–73) |
| Education | |
| Junior high school licence | 2 |
| Bachelor degree | 10 |
| Master degree | 9 |
| Professional profile | |
| Nursing home manager | 4 |
| Chief nurse | 4 |
| Chief medical officer | 3 |
| Nurse | 3 |
| Psychologist | 3 |
| Educator | 2 |
| Chief nurse aide | 1 |
| Nurse aide | 1 |
| Overall working experience, years, mean (range) | 16 (1–50) |
| Working experience in nursing home, years, mean (range) | 8.5 (0.5–25) |
| Employment | |
| Permanent full-time | 14 |
| Freelance Permanent part-time | 6 |
| Permanent part-time | 1 |
| Themes | Communicating with Family Caregivers over the Overall Disease Trajectory | Managing Challenging Emotions and Situations | Establishing a Partnership between Healthcare Professionals and Family Caregivers | Addressing Healthcare Professionals’ Communication Skills and Training Needs |
|---|---|---|---|---|
| Categories | Supportive communication Traditional communication Remote communication Healthcare professionals’ attitudes and professionalism Admission phase Approaching and at end-of-life phase After death phase | Managing family caregivers’ denial of the resident’s worsening condition Managing prognostic discordance Managing family caregivers’ expectations Managing healthcare professionals’ uncertainty about prognosis Managing family caregivers’ complex and turbulent emotions Managing healthcare professionals’ complex and turbolent emotions Overcoming challenges | Fulfilling family caregivers’ information and supportive needs Establishing trusting relationships Sharing decisions with family caregivers and among healthcare professionals Exploring family caregivers’ preferences for end-of-life care Healthcare professionals’ shortage and burden Time constraints | Source of communication skills Healthcare professionals’ education needs to sustain communication with family caregivers Preferred training to gain communication skills |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gonella, S.; Di Giulio, P.; Antal, A.; Cornally, N.; Martin, P.; Campagna, S.; Dimonte, V. Challenges Experienced by Italian Nursing Home Staff in End-of-Life Conversations with Family Caregivers during COVID-19 Pandemic: A Qualitative Descriptive Study. Int. J. Environ. Res. Public Health 2022, 19, 2504. https://doi.org/10.3390/ijerph19052504
Gonella S, Di Giulio P, Antal A, Cornally N, Martin P, Campagna S, Dimonte V. Challenges Experienced by Italian Nursing Home Staff in End-of-Life Conversations with Family Caregivers during COVID-19 Pandemic: A Qualitative Descriptive Study. International Journal of Environmental Research and Public Health. 2022; 19(5):2504. https://doi.org/10.3390/ijerph19052504
Chicago/Turabian StyleGonella, Silvia, Paola Di Giulio, Alexandra Antal, Nicola Cornally, Peter Martin, Sara Campagna, and Valerio Dimonte. 2022. "Challenges Experienced by Italian Nursing Home Staff in End-of-Life Conversations with Family Caregivers during COVID-19 Pandemic: A Qualitative Descriptive Study" International Journal of Environmental Research and Public Health 19, no. 5: 2504. https://doi.org/10.3390/ijerph19052504
APA StyleGonella, S., Di Giulio, P., Antal, A., Cornally, N., Martin, P., Campagna, S., & Dimonte, V. (2022). Challenges Experienced by Italian Nursing Home Staff in End-of-Life Conversations with Family Caregivers during COVID-19 Pandemic: A Qualitative Descriptive Study. International Journal of Environmental Research and Public Health, 19(5), 2504. https://doi.org/10.3390/ijerph19052504








