Are Gyms a Feasible Setting for Exercise Training Interventions in Patients with Cardiovascular Risk Factors? An Italian 10-Years Cross-Sectional Survey Comparison
Abstract
:1. Introduction
2. Materials and Methods
2.1. Survey
2.2. PASSI Surveillance
2.3. Statistical Analysis
3. Results
3.1. What Has Changed in the Last Decade?
3.2. Survey vs. PASSI Surveillance
4. Discussion
Limitations and Perspectives
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Hansen, D.; Niebauer, J.; Cornelissen, V.; Barna, O.; Neunhaeuserer, D.; Stettler, C.; Tonoli, C.; Greco, E.; Fagard, R.; Coninx, K.; et al. Exercise Prescription in Patients with Different Combinations of Cardiovascular Disease Risk Factors: A Consensus Statement from the EXPERT Working Group. Sports Med. 2018, 48, 1781–1797. [Google Scholar] [CrossRef] [PubMed]
- Negi, C.K.; Babica, P.; Bajard, L.; Bienertova-Vasku, J.; Tarantino, G. Insights into the molecular targets and emerging pharmacotherapeutic interventions for nonalcoholic fatty liver disease. Metabolism 2021, 126. [Google Scholar] [CrossRef] [PubMed]
- Booth, F.W.; Roberts, C.K.; Thyfault, J.P.; Ruegsegger, G.N.; Toedebusch, R.G. Role of Inactivity in Chronic Diseases: Evolutionary Insight and Pathophysiological Mechanisms. Physiol. Rev. 2017, 97, 1351–1402. [Google Scholar] [CrossRef] [PubMed]
- Archer, E.; Blair, S.N. Physical Activity and the Prevention of Cardiovascular Disease: From Evolution to Epidemiology. Prog. Cardiovasc. Dis. 2011, 53, 387–396. [Google Scholar] [CrossRef] [PubMed]
- Sandbakk, S.B.; Nauman, J.; Zisko, N.; Sandbakk, Ø.; Aspvik, N.P.; Stensvold, D.; Wisløff, U. Sedentary Time, Cardiorespiratory Fitness, and Cardiovascular Risk Factor Clustering in Older Adults--the Generation 100 Study. Mayo Clin. Proc. 2016, 91, 1525–1534. [Google Scholar] [CrossRef] [Green Version]
- Dyrstad, S.M.; Anderssen, S.A.; Edvardsen, E.; Hansen, B.H. Cardiorespiratory fitness in groups with different physical activity levels. Scand. J. Med. Sci. Sports 2015, 26, 291–298. [Google Scholar] [CrossRef]
- McCabe, M.P.; James, T. Strategies to Change Body Shape among Men and Women Who Attend Fitness Centers. Asia Pac. J. Public Health 2009, 21, 268–278. [Google Scholar] [CrossRef]
- Batrakoulis, A. European Survey of Fitness Trends for 2020. ACSM’S Health Fit. J. 2019, 23, 28–35. [Google Scholar] [CrossRef]
- Sallis, R.; Franklin, B.; Joy, L.; Ross, R.; Sabgir, D.; Stone, J. Strategies for Promoting Physical Activity in Clinical Practice. Prog. Cardiovasc. Dis. 2014, 57, 375–386. [Google Scholar] [CrossRef]
- Lim, G.B. Global burden of cardiovascular disease. Nat. Rev. Cardiol. 2013, 10, 59. [Google Scholar] [CrossRef]
- Lee, I.-M.; Bauman, A.E.; Blair, S.N.; Heath, G.W.; Kohl, H.W.; Pratt, M.; Hallal, P.C. Annual deaths attributable to physical inactivity: Whither the missing 2 million? Lancet 2013, 381, 992–993. [Google Scholar] [CrossRef]
- Stanaway, J.D.; Afshin, A.; Gakidou, E. Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks for 195 countries and territories, 1990-2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2018, 392, 1923–1994. [Google Scholar] [CrossRef] [Green Version]
- World Health Organization. Noncommunicable Diseases Country Profiles 2018. WHO. Published online 2018. Available online: https://www.who.int/nmh/publications/ncd-profiles-2018/en/ (accessed on 12 November 2020).
- Arnett, D.K.; Blumenthal, R.S.; Albert, M.A.; Buroker, A.B.; Goldberger, Z.D.; Hahn, E.J.; Himmelfarb, C.D.; Khera, A.; Lloyd-Jones, D.; McEvoy, J.W.; et al. 2019 ACC/AHA Guideline on the primary prevention of cardiovascular disease: A report of the american college of cardiology/American heart association task force on clinical practice guidelines. Circulation 2019, 140, e596–e646. [Google Scholar] [CrossRef] [PubMed]
- Bull, F.C.; Al-Ansari, S.S.; Biddle, S.; Borodulin, K.; Buman, M.; Cardon, G.; Carty, C.; Chaput, J.-P.; Chastin, S.; Chou, R.; et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br. J. Sports Med. 2020, 54, 1451–1462. [Google Scholar] [CrossRef]
- Merianos, A.; Peiris, M. International Health Regulations. Lancet 2005, 366, 1249–1251. [Google Scholar] [CrossRef]
- World Health Assembly, 58. Fifty-eighth World Health Assembly, Geneva, 16–25 May 2005: Resolutions and decisions: Annex; World Health Organization: Geneva, Switzerland, 2005. [Google Scholar]
- Mokdad, A.H. The Behavioral Risk Factors Surveillance System: Past, Present, and Future. Annu. Rev. Public Health 2009, 30, 43–54. [Google Scholar] [CrossRef] [Green Version]
- Baldissera, S.; Campostrini, S.; Binkin, N.; Minardi, V.; Minelli, G.; Ferrante, G.; Salmaso, S. Features and Initial Assessment of the Italian Behavioral Risk Factor Surveillance System (PASSI), 2007-2008. Prev. Chronic Dis. 2010, 8, A24. [Google Scholar]
- Possenti, V.; PASSI Coordinating Group. Health profile of the PASSI surveillance system according to the second self-audit data. Annali Igiene 2019, 31, 202–210. [Google Scholar] [CrossRef]
- Williams, B.; Mancia, G.; Spiering, W.; Agabiti Rosei, E.; Azizi, M.; Burnier, M.; Clement, D.L.; Coca, A.; de Simone, G.; Dominiczak, A.; et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension. Eur. Heart J. 2018, 39, 3021–3104, Correction in Eur. Heart J. 2019, 40, 475. [Google Scholar] [CrossRef]
- Mach, F.; Baigent, C.; Catapano, A.L.; Koskinas, K.C.; Casula, M.; Badimon, L.; Chapman, M.J.; De Backer, G.G.; Delgado, V.; Ference, B.A.; et al. 2019 ESC/EAS guidelines for the management of dyslipidaemias: Lipid modification to reduce cardiovascular risk. Atherosclerosis 2019, 290, 140–205. [Google Scholar] [CrossRef] [Green Version]
- Health Organization Regional Office for Europe. Action Plan for the Prevention and Control of Noncommunicable Diseases in the WHO European Region. Published Online 2016. Available online: http://www.euro.who.int/pubrequest (accessed on 4 February 2022).
- Cosentino, F.; Grant, P.J.; Aboyans, V.; Bailey, C.J.; Ceriello, A.; Delgado, V.; Federici, M.; Filippatos, G.; Grobbee, D.E.; Hansen, T.B.; et al. 2019 ESC Guidelines on diabetes, pre-diabetes, and cardiovascular diseases developed in collaboration with the EASD. Eur. Heart J. 2020, 41, 255–323. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- World Health Organization. Rapid Communication on Forthcoming Changes to the Programmatic Management of Tuberculosis Preventive Treatment. Available online: http://apps.who.int/bookorders (accessed on 21 March 2020).
- Virani, S.S.; Alonso, A.; Aparicio, H.J.; Benjamin, E.J.; Bittencourt, M.S.; Callaway, C.W.; Carson, A.P.; Chamberlain, A.M.; Cheng, S.; Delling, F.N.; et al. Heart Disease and Stroke Statistics-2021 Update: A Report from the American Heart Association. Circulation 2021, 143, e254–e743. [Google Scholar] [CrossRef] [PubMed]
- Citing SurveyMonkey. Available online: https://help.surveymonkey.com/articles/en_US/kb/May-I-reference-SurveyMonkey-in-a-paper-or-thesis (accessed on 15 December 2020).
- Sorveglianza Passi. Available online: https://www.epicentro.iss.it/passi/ (accessed on 17 April 2021).
- Watts, P.; Webb, E.; Netuveli, G. The role of sports clubs in helping older people to stay active and prevent frailty: A longitudinal mediation analysis. Int. J. Behav. Nutr. Phys. Act. 2017, 14, 95. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Palermi, S.; Sacco, A.M.; Belviso, I.; Romano, V.; Montesano, P.; Corrado, B.; Sirico, F. Guidelines for Physical Activity—A Cross-Sectional Study to Assess Their Application in the General Population. Have We Achieved Our Goal? Int. J. Environ. Res. Public Health 2020, 17, 3980. [Google Scholar] [CrossRef] [PubMed]
- Pazmino, L.; Esparza, W.; Aladro-Gonzalvo, A.; León, E. Impact of Work and Recreational Physical Activity on Prediabetes Condition among U.S. Adults: NHANES 2015–2016. Int. J. Environ. Res. Public Health 2021, 18, 1378. [Google Scholar] [CrossRef] [PubMed]
- Magistro, D.; Carlevaro, F.; Magno, F.; Simon, M.; Camp, N.; Kinrade, N.; Zecca, M.; Musella, G. Effects of 1 Year of Lifestyle Intervention on Institutionalized Older Adults. Int. J. Environ. Res. Public Health 2021, 18, 7612. [Google Scholar] [CrossRef]
- Pinto, R.; Melo, X.; Angarten, V.; Pires, M.L.; Borges, M.; Santos, V.; Abreu, A.; Santa-Clara, H. The effects of 12-months supervised periodized training on health-related physical fitness in coronary artery disease: A randomized controlled trial. J. Sports Sci. 2021, 39, 1893–1902. [Google Scholar] [CrossRef]
- Jönsson, T.; Hansson, E.E.; Thorstensson, C.; Eek, F.; Bergman, P.; Dahlberg, L.E. The effect of education and supervised exercise on physical activity, pain, quality of life and self-efficacy an intervention study with a reference group. BMC Musculoskelet. Disord. 2018, 19, 198. [Google Scholar] [CrossRef]
- Storer, T.W.; Dolezal, B.A.; Berenc, M.N.; Timmins, J.E.; Cooper, C.B. Effect of Supervised, Periodized Exercise Training vs. Self-Directed Training on Lean Body Mass and Other Fitness Variables in Health Club Members. J. Strength Cond. Res. 2014, 28, 1995–2006. [Google Scholar] [CrossRef]
- Biddle, S.J.H.; Hagger, M.S.; Chatzisarantis, N.L.D.; Lippke, S. Theoretical Frameworks in Exercise Psychology. In Handbook of Sport Psychology; John Wiley & Sons, Inc.: Hoboken, NJ, USA, 2012; pp. 537–559. [Google Scholar]
- Palestre della Salute Regione del Veneto. Available online: https://www.regione.veneto.it/web/sanita/palestre-della-salute (accessed on 17 April 2021).
- Foccardi, G.; Hansen, D.; Quinto, G.; Favero, C.; Coninx, K.; Ruiz, G.R.; Dendale, P.; Niebauer, J.; Ermolao, A.; Neunhaeuserer, D. How do General Practitioners assess physical activity and prescribe exercise in patients with different cardiovascular diseases? An Italian pilot study. Eur. J. Prev. Cardiol. 2020, 28, e20–e24. [Google Scholar] [CrossRef]
- Sallis, R. Exercise is medicine: A call to action for physicians to assess and prescribe exercise. Physician Sportsmed. 2015, 43, 22–26. [Google Scholar] [CrossRef] [PubMed]
- Lobelo, F.; Stoutenberg, M.; Hutber, A. The Exercise is Medicine Global Health Initiative: A 2014 update. Br. J. Sports Med. 2014, 48, 1627–1633. [Google Scholar] [CrossRef] [PubMed]
- NCDs|Global Action Plan on Physical Activity 2018–2030: More Active People for a Healthier World. WHO Published Online 2019. Available online: http://www.who.int/ncds/prevention/physical-activity/global-action-plan-2018-2030/en/ (accessed on 1 June 2021). Published online 2019.
- Homepage Moving Medicine. Available online: https://movingmedicine.ac.uk/ (accessed on 1 June 2021).
- Chatterjee, R.; Chapman, T.; Brannan, M.G.; Varney, J. GPs’ knowledge, use, and confidence in national physical activity and health guidelines and tools: A questionnaire-based survey of general practice in England. Br. J. Gen. Pract. 2017, 67, e668–e675. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pojednic, R.; Bantham, A.; Arnstein, F.; Kennedy, M.A.; Phillips, E. Bridging the gap between clinicians and fitness professionals: A challenge to implementing exercise as medicine. BMJ Open Sport Exerc. Med. 2018, 4, e000369. [Google Scholar] [CrossRef] [Green Version]
| 2007 Survey n = 1049 | 2017 Survey n = 919 | p | |
|---|---|---|---|
| Gender (female) | 472 (45.0) | 441 (48.0) | 0.422 |
| Age | |||
| 18–35 years | 667 (63.6) | 513 (55.8) | 0.079 |
| 35–50 years | 273 (26.5) | 213 (23.2) | 0.187 |
| 50–69 years | 104 (9.9) | 193 (21.0) | <0.001 |
| Arterial hypertension | 52 (4.9) | 79 (8.6) | 0.001 |
| Hypercholesterolemia | 62 (5.9) | 108 (11.8) | <0.001 |
| Overweight | 252 (24.0) | 213 (23.2) | 0.660 |
| Diabetes | 12 (1.1) | 13 (1.4) | 0.593 |
| Smokers | 301 (28.7) | 230 (25.0) | 0.068 |
| Heart disease | 17 (1.6) | 13 (1.4) | 0.710 |
| Medical referral | 55 (5.2) | 71 (7.7) | 0.035 |
| Benefits from PA | 1026 (97.8) | 906 (98.6) | 0.938 |
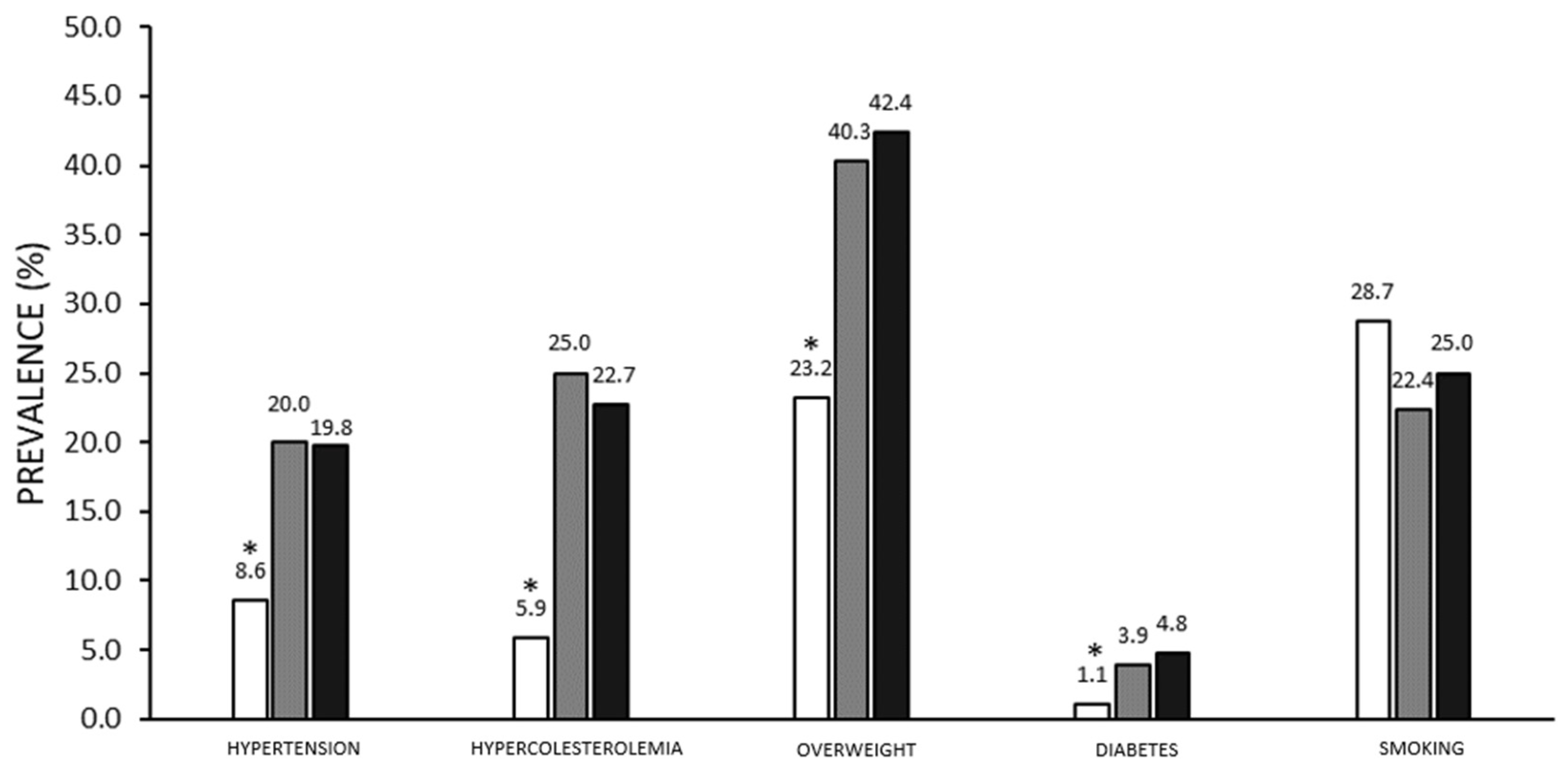
| 2007 Survey n = 1049 | 2007 PASSI n = 3219 | p | 2017 Survey n = 919 | 2017 PASSI n = 20059 | p | |
|---|---|---|---|---|---|---|
| Hypertension | 52 (4.7) | 731 (22.7) | <0.001 | 79 (8.6) | 4012 (20) | <0.001 |
| 18–35 years | 15 (2.2) | 72 (7.4) | <0.001 | 3 (0.5) | 180 (3.5) | <0.001 |
| 35–50 years | 22 (7.9) | 186 (16.5) | <0.001 | 21 (9.9) | 893 (13.1) | 0.167 |
| 50–69 years | 15 (14.4) | 473 (42.5) | <0.001 | 55 (28.5) | 2939 (36.3) | 0.026 |
| Male | 36 (6.2) | 388 (23.8) | <0.001 | 40 (8.4) | 1872 (18.9) | <0.001 |
| Female | 16 (3.4) | 343 (21.6) | <0.001 | 39 (8.8) | 2140 (21.0) | <0.001 |
| Hypercholesterolemia | 62 (5.9) | 927 (28.8) | <0.001 | 108 (11.8) | 4594 (22.9) | <0.001 |
| 18–35 years | 24 (3.6) | 141 (14.4) | <0.001 | 22 (4.3) | 406 (7.9) | 0.003 |
| 35–50 years | 26 (9.4) | 272 (24.1) | <0.001 | 34 (16.0) | 1289 (18.9) | 0.280 |
| 50–69 years | 12 (11.5) | 514 (46.2) | <0.001 | 52 (26.9) | 2899 (35.8) | 0.011 |
| Male | 29 (5.0) | 266 (28.6) | <0.001 | 44 (9.2) | 2240 (22.7) | <0.001 |
| Female | 33 (7.0) | 461 (29.0) | <0.001 | 64 (14.5) | 2354 (11.7) | <0.001 |
| Overweight | 252 (24.0) | 1352 (42.0) | <0.001 | 213 (23.2) | 8084 (40.3) | <0.001 |
| 18–35 years | 135 (20.2) | 225 (23.0) | 0.186 | 108 (21.1) | 1150 (22.4) | 0.486 |
| 35–50 years | 81 (29.1) | 431 (38.2) | 0.005 | 71 (33.3) | 2612 (38.3) | 0.142 |
| 50–69 years | 36 (34.6) | 696 (62.5) | <0.001 | 34 (17.6) | 4322 (53.3) | <0.001 |
| Male | 186 (32.2) | 828 (50.8) | <0.001 | 116 (24.3) | 4925 (49.9) | <0.001 |
| Female | 66 (14.0) | 524 (33.0) | <0.001 | 97 (22.0) | 3159 (31.0) | <0.001 |
| Diabetes | 12 (1.1) | 129 (4.0) | <0.001 | 13 (1.4) | 943 (4.7) | <0.001 |
| 18–35 years | 4 (0.6) | 5 (0.5) | 0.058 | 2 (0.4) | 62 (1.2) | 0.095 |
| 35–50 years | 2 (0.7) | 32 (2.8) | 0.039 | 1 (0.5) | 136 (2.0) | 0.113 |
| 50–69 years | 6 (5.8) | 92 (8.3) | 0.371 | 10 (5.2) | 745 (9.2) | 0.055 |
| Male | 7 (1.2) | 72 (4.4) | <0.001 | 6 (1.3) | 577 (5.8) | <0.001 |
| Female | 5 (1.1) | 57 (3.6) | 0.009 | 7 (1.6) | 366 (3.6) | 0.025 |
| Smokers | 301 (28.7) | 827 (25.7) | 0.055 | 230 (25.0) | 4509 (22.5) | 0.071 |
| 18–35 years | 212 (31.8) | 340 (34.7) | 0.214 | 150 (29.2) | 1532 (29.8) | 0.779 |
| 35–50 years | 66 (23.7) | 299 (26.5) | 0.342 | 44 (20.7) | 1555 (22.8) | 0.462 |
| 50–69 years | 23 (22.1) | 188 (16.9) | 0.178 | 36 (18.7) | 1422 (17.5) | 0.690 |
| Male | 170 (29.5) | 470 (28.9) | 0.781 | 133 (27.8) | 2595 (26.3) | 0.458 |
| Female | 131 (27.8) | 357 (22.5) | 0.018 | 97 (22.0) | 1914 (18.8) | 0.092 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vecchiato, M.; Quinto, G.; Palermi, S.; Foccardi, G.; Mazzucato, B.; Battista, F.; Duregon, F.; Michieletto, F.; Neunhaeuserer, D.; Ermolao, A. Are Gyms a Feasible Setting for Exercise Training Interventions in Patients with Cardiovascular Risk Factors? An Italian 10-Years Cross-Sectional Survey Comparison. Int. J. Environ. Res. Public Health 2022, 19, 2407. https://doi.org/10.3390/ijerph19042407
Vecchiato M, Quinto G, Palermi S, Foccardi G, Mazzucato B, Battista F, Duregon F, Michieletto F, Neunhaeuserer D, Ermolao A. Are Gyms a Feasible Setting for Exercise Training Interventions in Patients with Cardiovascular Risk Factors? An Italian 10-Years Cross-Sectional Survey Comparison. International Journal of Environmental Research and Public Health. 2022; 19(4):2407. https://doi.org/10.3390/ijerph19042407
Chicago/Turabian StyleVecchiato, Marco, Giulia Quinto, Stefano Palermi, Giulia Foccardi, Barbara Mazzucato, Francesca Battista, Federica Duregon, Federica Michieletto, Daniel Neunhaeuserer, and Andrea Ermolao. 2022. "Are Gyms a Feasible Setting for Exercise Training Interventions in Patients with Cardiovascular Risk Factors? An Italian 10-Years Cross-Sectional Survey Comparison" International Journal of Environmental Research and Public Health 19, no. 4: 2407. https://doi.org/10.3390/ijerph19042407
APA StyleVecchiato, M., Quinto, G., Palermi, S., Foccardi, G., Mazzucato, B., Battista, F., Duregon, F., Michieletto, F., Neunhaeuserer, D., & Ermolao, A. (2022). Are Gyms a Feasible Setting for Exercise Training Interventions in Patients with Cardiovascular Risk Factors? An Italian 10-Years Cross-Sectional Survey Comparison. International Journal of Environmental Research and Public Health, 19(4), 2407. https://doi.org/10.3390/ijerph19042407








