An Economic Evaluation of ‘Sheds for Life’: A Community-Based Men’s Health Initiative for Men’s Sheds in Ireland
Abstract
:1. Introduction
1.1. Nature of Sheds for Life
1.2. Assessing Costs of Health Programs
2. Materials and Methods
2.1. Study Participants
2.2. Data Collection
2.3. Methodological Approach
3. Results
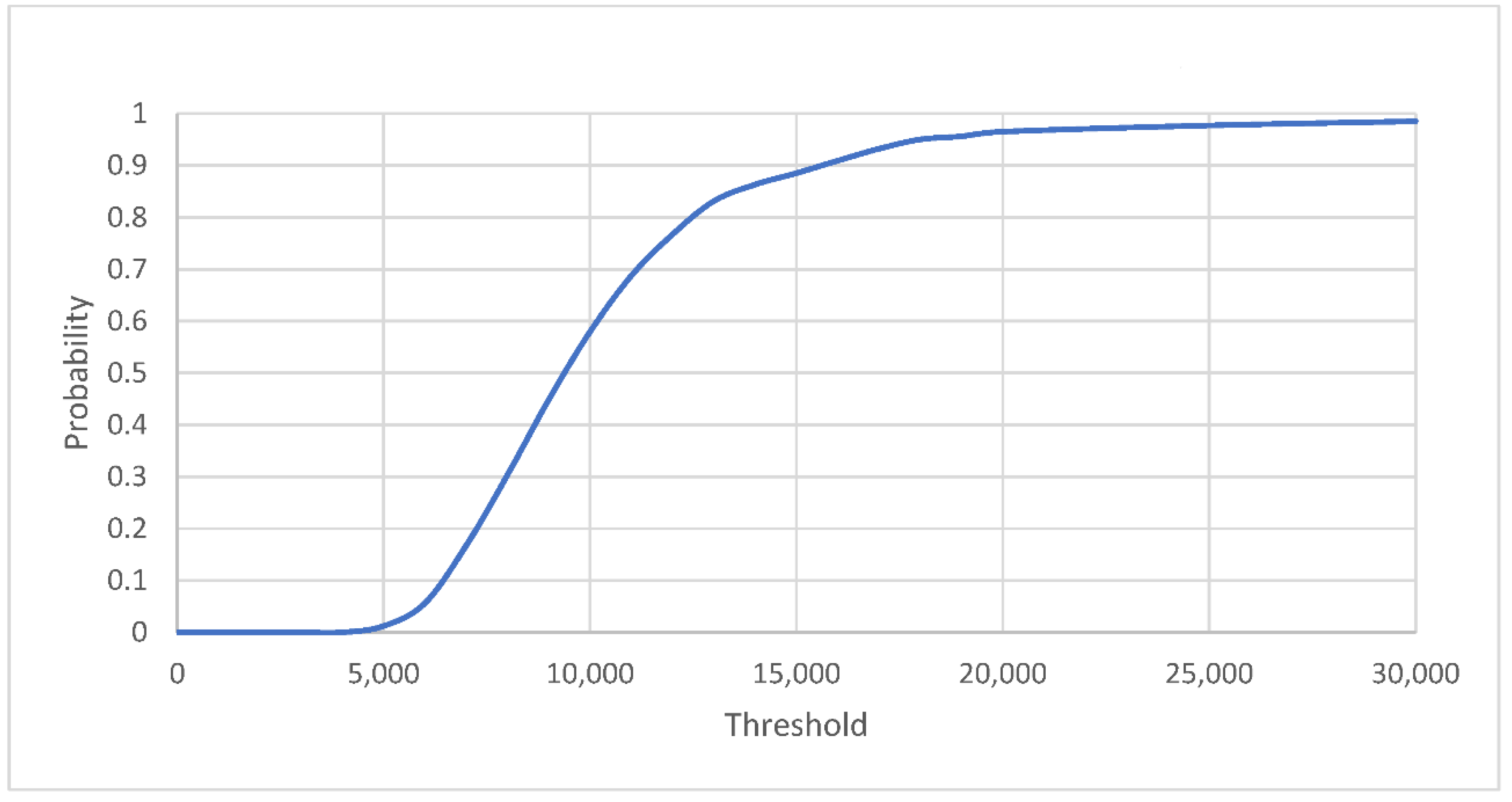
Sensitivity Analysis
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- WHO. The Health and Well-Being of Men in the WHO European Region: Better Health through A Gender Approach; World Health Organisation: Copenhagen, Denmark, 2018.
- Pringle, A.; Zwolinsky, S.; McKenna, J.; Robertson, S.; Daly-Smith, A.; White, A. Health improvement for men and hard-to-engage-men delivered in English Premier League football clubs. Health Educ. Res. 2014, 29, 503–520. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zwolinsky, S.; McKenna, J.; Pringle, A.; Daly-Smith, A.; Robertson, S.; White, A. Optimizing lifestyles for men regarded as ‘hard-to-reach’ through top-flight football/soccer clubs. Health Educ. Res. 2012, 28, 405–413. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Caperchione, C.M.; Bottorff, J.L.; Oliffe, J.L.; Johnson, S.T.; Hunt, K.; Sharp, P.; Fitzpatrick, K.M.; Price, R.; Goldenberg, S.L. The HAT TRICK programme for improving physical activity, healthy eating and connectedness among overweight, inactive men: Study protocol of a pragmatic feasibility trial. BMJ Open 2017, 7, e016940. [Google Scholar] [CrossRef] [PubMed]
- Kelly, L.; Harrison, M.; Richardson, N.; Carroll, P.; Robertson, S.; Keohane, A.; Donohoe, A. Reaching beyond the ‘worried well’: Pre-adoption characteristics of participants in ‘Men on the Move’, a community-based physical activity programme. J. Public Health 2019, 41, e192–e202. [Google Scholar] [CrossRef] [Green Version]
- Oliffe, J.L.; Rossnagel, E.; Bottorff, J.L.; Chambers, S.K.; Caperchione, C.; Rice, S.M. Community-based men’s health promotion programs: Eight lessons learnt and their caveats. Health Promot. Int. 2020, 35, 1230–1240. [Google Scholar] [CrossRef] [PubMed]
- Wilson, N.J.; Cordier, R. A narrative review of Men’s Sheds literature: Reducing social isolation and promoting men’s health and well-being. Health Soc. Care Community 2013, 21, 451–463. [Google Scholar] [CrossRef]
- Golding, B. The Men’s Shed Movement; Common Ground Research Networks: Champaign, IL, USA, 2015. [Google Scholar]
- Kelly, D.; Steiner, A.; Mason, H.; Teasdale, S. Men’s Sheds: A conceptual exploration of the causal pathways for health and well-being. Health Soc. Care Community 2019, 27, 1147–1157. [Google Scholar] [CrossRef] [Green Version]
- Bergin, N.; Richardson, N. ‘Sheds for Life’: Getting the balance right in delivering health promotion through Sheds in Ireland. Health Promot. Int. 2021, 36, 605–615. [Google Scholar] [CrossRef]
- Misan, G.M.; Oosterbroek, C.; Wilson, N.J. Informing Health Promotion in Rural Men’s Sheds by Examination of Participant Health Status, Concerns, Interests, Knowledge and Behaviours. Health Promot. J. Aust. 2016, 28, 207–216. [Google Scholar] [CrossRef]
- McGrath, A.; Murphy, N.; Richardson, N. Study protocol: Evaluation of sheds for life (SFL): A community-based men’s health initiative designed “for shedders by shedders” in Irish Men’s sheds using a hybrid effectiveness-implementation design. BMC Public Health 2021, 21, 801. [Google Scholar] [CrossRef]
- McGrath, A.; Murphy, N.; Richardson, N. The impact of the COVID-19 pandemic on the wellbeing of Irish Men’s Shed members. Health. Promot. Int. 2021, 36, 1007–1019. [Google Scholar] [CrossRef]
- Lefkowich, M.; Richardson, N. Men’s health in alternative spaces: Exploring men’s sheds in Ireland. Health Promot. Int. 2016, 33, 525–535. [Google Scholar] [CrossRef] [PubMed]
- Kelly, D.; Teasdale, S.; Steiner, A.; Mason, H. Men’s Sheds in Scotland: The potential for improving the health of men. J. Public Health Policy 2021, 42, 258–270. [Google Scholar] [CrossRef] [PubMed]
- Kelly, D.; Steiner, A.; Mason, H.; Teasdale, S. Men’s sheds as an alternative healthcare route? A qualitative study of the impact of Men’s sheds on user’s health improvement behaviours. BMC Public Health 2021, 21, 553. [Google Scholar] [CrossRef] [PubMed]
- Proctor, E.; Silmere, H.; Raghavan, R.; Hovmand, P.; Aarons, G.; Bunger, A.; Griffey, R.; Hensley, M. Outcomes for implementation research: Conceptual distinctions, measurement challenges, and research agenda. Adm. Policy. Ment. Health. 2011, 38, 65–76. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Koorts, H.; Eakin, E.; Estabrooks, P.; Timperio, A.; Salmon, J.; Bauman, A. Implementation and scale up of population physical activity interventions for clinical and community settings: The PRACTIS guide. Int. J. Behav. Nutr. Phys. Act. 2018, 15, 51. [Google Scholar] [CrossRef]
- Damschroder, L.J.; Aron, D.C.; Keith, R.E.; Kirsh, S.R.; Alexander, J.A.; Lowery, J.C. Fostering implementation of health services research findings into practice: A consolidated framework for advancing implementation science. Implement. Sci. 2009, 4, 50. [Google Scholar] [CrossRef] [Green Version]
- Vaughan, K.; Kok, M.C.; Witter, S.; Dieleman, M. Costs and cost-effectiveness of community health workers: Evidence from a literature review. Hum. Resour. Health 2015, 13, 71. [Google Scholar] [CrossRef] [Green Version]
- Baker, P. Men’s health: Time for a new approach. Phys. Ther. Rev. 2018, 23, 144–150. [Google Scholar] [CrossRef] [Green Version]
- Brott, A.; Dougherty, A.; Williams, S.T.; Matope, J.H.; Fadich, A.; Taddelle, M. The Economic Burden Shouldered by Public and Private Entities as a Consequence of Health Disparities Between Men and Women. Am. J. Mens. Health 2011, 5, 528–539. [Google Scholar] [CrossRef] [Green Version]
- Krueger, H.; Goldenberg, S.L.; Koot, J.; Andres, E. Don’t Change Much: The Economic Impact of Modest Health Behavior Changes in Middle-Aged Men. Am. J. Mens. Health 2016, 11, 275–283. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bolnick, H.J.; Bui, A.L.; Bulchis, A.; Chen, C.; Chapin, A.; Lomsadze, L.; Mokdad, A.H.; Millard, F.; Dieleman, J.L. Health-care spending attributable to modifiable risk factors in the USA: An economic attribution analysis. Lancet Public Health 2020, 5, e525–e535. [Google Scholar] [CrossRef]
- Kelly, L.; Harrison, M.; Richardson, N.; Carroll, P.; Egan, T.; Ormond, G.; Robertson, S. Economic evaluation of ‘Men on the Move’, a ‘real world’ community-based physical activity programme for men. Eur. J. Public Health 2021, 31, 156–160. [Google Scholar] [CrossRef] [PubMed]
- HIQA. Guidelines for the Economic Evaluation of Health Technologies in Ireland; Health Information and Quality Authority: Dublin, Ireland, 2020. [Google Scholar]
- Whitehead, S.J.; Ali, S. Health outcomes in economic evaluation: The QALY and utilities. Br. Med. Bull. 2010, 96, 5–21. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- van der Vliet, N.; Suijkerbuijk, A.W.M.; de Blaeij, A.T.; de Wit, G.A.; van Gils, P.F.; Staatsen, B.A.M.; Mass, R.; Polder, J.J. Ranking Preventive Interventions from Different Policy Domains: What Are the Most Cost-Effective Ways to Improve Public Health? Int. J. Environ. Res. Public Health 2020, 17, 2160. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Byford, S.; Raftery, J. Perspectives in economic evaluation. BMJ 1998, 316, 1529–1530. [Google Scholar] [CrossRef]
- Central Statistics Office. Census of Population 2016-Profile 2 Population Distribution and Movements; Central Statistics Office: Dublin, Ireland, 2017.
- Shaw, R.; Fenwick, E.; Baker, G.; McAdam, C.; Fitzsimons, C.; Mutrie, N. ‘Pedometers cost buttons’: The feasibility of implementing a pedometer based walking programme within the community. BMC Public Health 2011, 11, 200. [Google Scholar] [CrossRef] [Green Version]
- Brazier, J.; Roberts, J.; Deverill, M. The estimation of a preference-based measure of health from the SF-36. J. Health Econ. 2002, 21, 271–292. [Google Scholar] [CrossRef] [Green Version]
- O’Mahony, J.F.; Coughlan, D. The Irish Cost-Effectiveness Threshold: Does it Support Rational Rationing or Might it Lead to Unintended Harm to Ireland’s Health System? Pharmacoeconomics 2016, 34, 5–11. [Google Scholar] [CrossRef]
- Guillon, M.; Rochaix, L.; Dupont, J.K. Cost-effectiveness of interventions based on physical activity in the treatment of chronic conditions: A systematic literature review. Int. J. Technol. Assess Health Care 2018, 34, 481–497. [Google Scholar] [CrossRef]
- Epstein, D. Beyond the cost-effectiveness acceptability curve: The appropriateness of rank probabilities for presenting the results of economic evaluation in multiple technology appraisal. Health Econ. 2019, 28, 801–807. [Google Scholar] [CrossRef] [PubMed]
- Gandjour, A. Willingness to pay for new medicines: A step towards narrowing the gap between NICE and IQWiG. BMC Health Serv. Res. 2020, 20, 343. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Reeves, P.; Edmunds, K.; Searles, A.; Wiggers, J. Economic evaluations of public health implementation-interventions: A systematic review and guideline for practice. Public Health 2019, 169, 101–113. [Google Scholar] [CrossRef] [PubMed]
- Baker, P.; Shand, T. Men’s health: Time for a new approach to policy and practice? J. Glob. Health 2017, 7, 010306. [Google Scholar] [CrossRef] [PubMed]
- Rapport, F.; Clay-Williams, R.; Churruca, K.; Shih, P.; Hogden, A.; Braithwaite, J. The struggle of translating science into action: Foundational concepts of implementation science. J. Eval. Clin. Pract. 2018, 24, 117–126. [Google Scholar] [CrossRef] [Green Version]
- Henchoz, K.; Cavalli, S.; Girardin, M. Health perception and health status in advanced old age: A paradox of association. J. Aging Stud. 2008, 22, 282–290. [Google Scholar] [CrossRef]
- Kelly, D.; Steiner, A. The impact of community Men’s Sheds on the physical health of their users. Health Place 2021, 71, 102649. [Google Scholar] [CrossRef]
- Wyke, S.; Hunt, K.; Gray, C.; Fenwick, E.; Bunn, C.; Donnan, P.; Rauchhaus, P.; Mutrie, N.; Anderson, A.S.; Boyer, N.; et al. Football Fans in Training (FFIT): A randomised controlled trial of a gender-sensitised weight loss and healthy living programme for men – end of study report. Public Health Res. 2015, 3, 1–130. [Google Scholar] [CrossRef] [Green Version]
- Wyke, S.; Bunn, C.; Andersen, E.; Silva, M.N.; Van Nassau, F.; McSkimming, P.; Kolovos, S.; Gill, J.M.; Gray, C.M.; Hunt, K.; et al. The effect of a programme to improve men’s sedentary time and physical activity: The European Fans in Training (EuroFIT) randomised controlled trial. PLoS Med. 2019, 16, e1002736. [Google Scholar]
- Van Nassau, F.; Van Der Ploeg, H.P.; Abrahamsen, F.; Andersen, E.; Anderson, A.S.; Bosmans, J.E.; Bunn, C.; Chalmers, M.; Clissmann, C.; Gill, J.M.; et al. Study protocol of European Fans in Training (EuroFIT): A four-country randomised controlled trial of a lifestyle program for men delivered in elite football clubs. BMC Public Health 2016, 16, 598. [Google Scholar] [CrossRef] [Green Version]
- Hutchins, S.S.; Brown, C.; Mayberry, R.; Sollecito, W. Value of a small control group for estimating intervention effectiveness: Results from simulations of immunization effectiveness studies. J. Comp. Eff. Res. 2015, 4, 227–238. [Google Scholar] [CrossRef] [PubMed]
| Item | Costs € ** | |||
|---|---|---|---|---|
| Baseline to 3 Months * | 3 Months to 6 Months ** | 6 Months to 12 Months | Overall | |
| Costs of delivering physical activity | 13,200 | N/A | N/A | |
| Full health check | 25,260 | N/A | N/A | |
| Mental health workshop | 9600 | N/A | N/A | |
| Healthy food made easy | 19,800 | N/A | N/A | |
| Costs of optional components e.g., digital literacy, cancer awareness, oral health | 17,200 | N/A | N/A | |
| Miscellaneous costs e.g., admin costs | 212 | N/A | N/A | |
| SFL awards event | 0 | 4546 | N/A | |
| Salary costs including health and wellbeing manager, health administrator | 31,863 | 2278 | 2278 | |
| Travel and subsistence | 2289 | 809 | 809 | |
| Total Costs | 119,424 | 7633 | 3087 | 130,144 |
| Costs per participant (n = 421) | 309.13 | |||
| Baseline | 3M | 6M | 12M | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| IG | CG | Baseline Mean p-Value ** | IG | CG | 3M Mean p-Value ** | IG | CG | IG | CG | |
| N | 379 | 87 | 237 | 75 | 214 | 0 | 266 | 0 | ||
| Physical Functioning | 2.17 | 2.28 | 0.45 | 1.70 | 2.23 | 0.00 | 1.59 | * | 1.74 | * |
| Role Limitations | 1.49 | 1.63 | 0.11 | 1.32 | 1.61 | 0.01 | 1.24 | * | 1.24 | * |
| Social Functioning | 1.41 | 1.60 | 0.06 | 1.30 | 1.53 | 0.02 | 1.18 | * | 1.28 | * |
| Pain | 2.07 | 2.13 | 0.69 | 1.95 | 2.12 | 0.31 | 1.82 | * | 1.75 | * |
| Mental Health | 2.15 | 2.22 | 0.52 | 1.86 | 2.27 | 0.00 | 1.88 | * | 1.99 | * |
| Vitality | 3.45 | 3.26 | 0.10 | 3.77 | 3.24 | 0.00 | 3.72 | * | 3.70 | * |
| Group | Baseline | 3M | 6M | 12M |
|---|---|---|---|---|
| IG-N | 374 | 233 | 210 | 260 |
| IG-Average Utility | 0.795 | 0.827 * | 0.847 ** | 0.838 ** |
| Utility Change | 0.033 | 0.020 | −0.009 | |
| QALYs Gained | 7.595 | 4.222 | −2.480 | |
| CG-N | 85 | 72 | 0 | 0 |
| CG-Average Utility | 0.777 | 0.787 | ||
| Utility Change | 0.010 | |||
| QALYs Gained | 0.072 | |||
| Program Costs | 119,424 | 7633 | ||
| Cost per QALY | 15,724 | 1808 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
McGrath, A.; Murphy, N.; Egan, T.; Ormond, G.; Richardson, N. An Economic Evaluation of ‘Sheds for Life’: A Community-Based Men’s Health Initiative for Men’s Sheds in Ireland. Int. J. Environ. Res. Public Health 2022, 19, 2204. https://doi.org/10.3390/ijerph19042204
McGrath A, Murphy N, Egan T, Ormond G, Richardson N. An Economic Evaluation of ‘Sheds for Life’: A Community-Based Men’s Health Initiative for Men’s Sheds in Ireland. International Journal of Environmental Research and Public Health. 2022; 19(4):2204. https://doi.org/10.3390/ijerph19042204
Chicago/Turabian StyleMcGrath, Aisling, Niamh Murphy, Tom Egan, Gillian Ormond, and Noel Richardson. 2022. "An Economic Evaluation of ‘Sheds for Life’: A Community-Based Men’s Health Initiative for Men’s Sheds in Ireland" International Journal of Environmental Research and Public Health 19, no. 4: 2204. https://doi.org/10.3390/ijerph19042204
APA StyleMcGrath, A., Murphy, N., Egan, T., Ormond, G., & Richardson, N. (2022). An Economic Evaluation of ‘Sheds for Life’: A Community-Based Men’s Health Initiative for Men’s Sheds in Ireland. International Journal of Environmental Research and Public Health, 19(4), 2204. https://doi.org/10.3390/ijerph19042204







