Gender Disparities of Heart Disease and the Association with Smoking and Drinking Behavior among Middle-Aged and Older Adults, a Cross-Sectional Study of Data from the US Health and Retirement Study and the China Health and Retirement Longitudinal Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Data Source
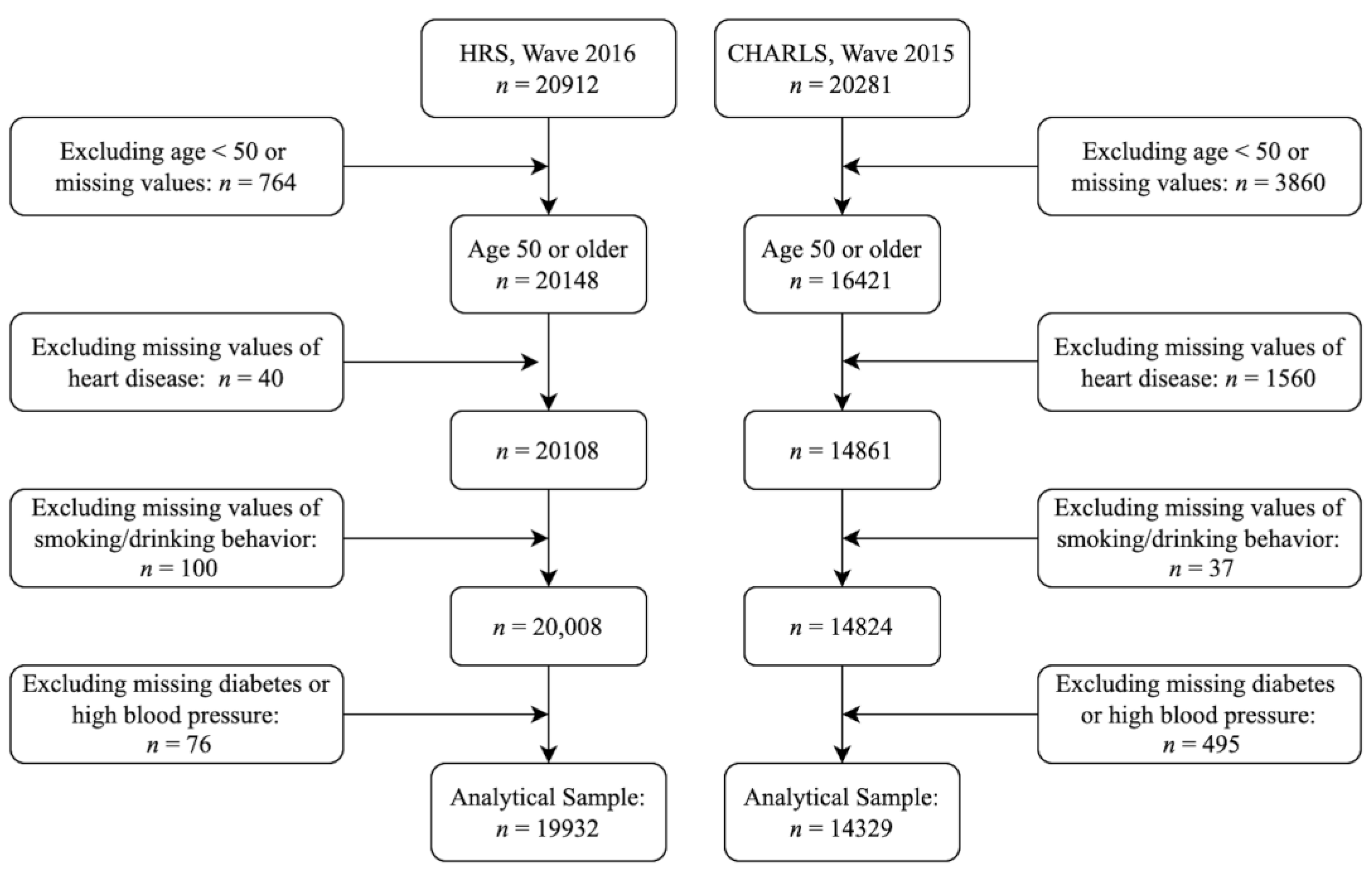
2.2. Analytical Sample
2.3. Variables
2.4. Statistical Analysis
3. Results
3.1. Sample Characteristics
3.2. Prevalence of Heart Disease by Age, Gender, and Smoking/Drinking Behavior
3.3. Prevalence Ratios of Heart Disease by Smoking/Drinking Behavior
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bots, S.H.; Peters, S.A.E.; Woodward, M. Sex differences in coronary heart disease and stroke mortality: A global assessment of the effect of ageing between 1980 and 2010. BMJ Glob. Health 2017, 2, e000298. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Roth, G.A.; Mensah, G.A.; Johnson, C.O.; Addolorato, G.; Ammirati, E.; Baddour, L.M.; Barengo, N.C.; Beaton, A.Z.; Benjamin, E.J.; Benziger, C.P.; et al. Global Burden of Cardiovascular Diseases and Risk Factors, 1990–2019: Update from the GBD 2019 Study. J. Am. Coll. Cardiol. 2020, 76, 2982–3021. [Google Scholar] [CrossRef] [PubMed]
- Mathers, C.D.; Loncar, D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med. 2006, 3, e442. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Health, United States 2019. Available online: https://www.cdc.gov/nchs/data/hus/2019/005-508.pdf (accessed on 1 June 2021).
- Zhu, J.; Cui, L.; Wang, K.; Xie, C.; Sun, N.; Xu, F.; Tang, Q.; Sun, C. Mortality pattern trends and disparities among Chinese from 2004 to 2016. BMC Public Health 2019, 19, 780. [Google Scholar] [CrossRef] [Green Version]
- Yoon, S.S.; Dillon, C.F.; Illoh, K.; Carroll, M. Trends in the Prevalence of Coronary Heart Disease in the U.S.: National Health and Nutrition Examination Survey, 2001–2012. Am. J. Prev. Med. 2016, 51, 437–445. [Google Scholar] [CrossRef] [Green Version]
- Li, H.; Ge, S.; Greene, B.; Dunbar-Jacob, J. Depression in the context of chronic diseases in the United States and China. Int. J. Nurs. Sci. 2018, 6, 117–122. [Google Scholar] [CrossRef]
- Rosenwohl-Mack, A.; Schumacher, K.; Fang, M.-L.; Fukuoka, Y. Experiences of aging in place in the United States: Protocol for a systematic review and meta-ethnography of qualitative studies. Syst. Rev. 2018, 7, 155. [Google Scholar] [CrossRef]
- Stone, C.L. A population-based measure of chronic disease severity for health planning and evaluation in the United States. AIMS Public Health 2020, 7, 44–65. [Google Scholar] [CrossRef]
- Report on Cardiovascular Diseases in China 2018. Available online: https://www.nccd.org.cn/Sites/Uploaded/File/2021/3/%E4%B8%AD%E5%9B%BD%E5%BF%83%E8%A1%80%E7%AE%A1%E7%97%85%E6%8A%A5%E5%91%8A2018%EF%BC%88English%EF%BC%89.pdf (accessed on 1 June 2021).
- Heart Disease. Centers for Disease Control and Prevention. 2021. Available online: https://www.cdc.gov/heartdisease/index.htm (accessed on 1 June 2021).
- Diabetes, Heart Disease, and Stroke. Available online: https://www.niddk.nih.gov/health-information/diabetes/overview/preventing-problems/heart-disease-stroke (accessed on 1 June 2021).
- Han, C.; Liu, F.; Yang, X.; Chen, J.; Li, J.; Cao, J.; Li, Y.; Shen, C.; Yu, L.; Liu, Z.; et al. Ideal cardiovascular health and incidence of atherosclerotic cardiovascular disease among Chinese adults: The China-PAR project. Sci. China Life Sci. 2018, 61, 504–514. [Google Scholar] [CrossRef]
- Li, Y.; Wang, D.D.; Ley, S.H.; Howard, A.G.; He, Y.; Lu, Y.; Danaei, G.; Hu, F.B. Potential Impact of Time Trend of Life-Style Factors on Cardiovascular Disease Burden in China. J. Am. Coll. Cardiol. 2016, 68, 818–833. [Google Scholar] [CrossRef]
- Lee, I.; Kim, S.; Kang, H. Lifestyle Risk Factors and All-Cause and Cardiovascular Disease Mortality: Data from the Korean Longitudinal Study of Aging. Int. J. Environ. Res. Public Health 2019, 16, 3040. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mokdad, A.H.; Marks, J.S.; Stroup, D.F.; Gerberding, J.L. Actual causes of death in the United States, 2000. JAMA 2004, 291, 1238–1245. [Google Scholar] [CrossRef] [PubMed]
- Shah, A.; Shah, J.; Shah, N.; Shah, R. Smoking prevalence and chronic diseases in China. Lancet Respir. Med. 2019, 7, e10. [Google Scholar] [CrossRef] [Green Version]
- Tolstrup, J.; Hvidtfeldt, U.A.; Flachs, E.M.; Spiegelman, D.; Heitmann, B.L.; Baelter, K.; Goldbourt, U.; Hallmans, G.; Knekt, P.; Liu, S.; et al. Smoking and Risk of Coronary Heart Disease in Younger, Middle-Aged, and Older Adults. Am. J. Public Health 2014, 104, 96–102. [Google Scholar] [CrossRef] [PubMed]
- Kouvari, M.; Panagiotakos, D.B.; Chrysohoou, C.; Georgousopoulou, E.; Notara, V.; Tousoulis, D.; Pitsavos, C. Gender-specific, Lifestyle-related Factors and 10-year Cardiovascular Disease Risk; the ATTICA and GREECS Cohort Studies. Curr. Vasc. Pharmacol. 2019, 17, 401–410. [Google Scholar] [CrossRef] [PubMed]
- Health and Retirement Study Data File. Available online: https://www.rand.org/well-being/social-and-behavioral-policy/centers/aging/dataprod/hrs-data.html (accessed on 1 June 2021).
- Thompson, M.D.; Pirkle, C.M.; Youkhana, F.; Wu, Y.Y. Gene-Obesogenic Environment Interactions on Body Mass Indices for Older Black and White Men and Women from the Health and Retirement Study. Int. J. Obes. 2020, 44, 1893–1905. [Google Scholar] [CrossRef]
- Hua, J. Stratum Differences in Health Behaviour of Elderly Group—An empirical research based on harmonized CHARLS. J. Phys. Conf. Ser. 2020, 1437, 012114. [Google Scholar] [CrossRef]
- Zhao, Y.; Hu, Y.; Smith, J.P.; Strauss, J.; Yang, G. Cohort Profile: The China Health and Retirement Longitudinal Study (CHARLS). Int. J. Epidemiol. 2014, 43, 61–68. [Google Scholar] [CrossRef] [Green Version]
- Zhao, Y.; Strauss, J.; Yang, G.; Giles, J.; Hu, P.; Hu, Y.; Lei, X.; Park, A.; Smith, J.P.; Wang, Y. China Health and Retirement Longitudinal Study, 2011–2012 National Baseline Users’ Guide; National School of Development, Peking University: Beijing, China, 2013. [Google Scholar]
- Ding, L.; Liang, Y.; Tan, E.C.K.; Hu, Y.; Zhang, C.; Liu, Y.; Xue, F.; Wang, R. Smoking, heavy drinking, physical inactivity, and obesity among middle-aged and older adults in China: Cross-sectional findings from the baseline survey of CHARLS 2011–2012. BMC Public Health 2020, 20, 1062. [Google Scholar] [CrossRef]
- Timeline of Events in China, Facing History and Ourselves. Available online: https://www.facinghistory.org/nanjing-atrocities-crimes-war/timeline-events-china (accessed on 1 June 2021).
- Cui, Y.; Zhu, Q.; Lou, C.; Gao, E.; Cheng, Y.; Zabin, L.S.; Emerson, M.R. Gender differences in cigarette smoking and alcohol drinking among adolescents and young adults in Hanoi, Shanghai, and Taipei. J. Int. Med. Res. 2018, 46, 5257–5268. [Google Scholar] [CrossRef]
- Chuang, Y.C.; Chuang, K.Y. Gender differences in relationships between social capital and individual smoking and drinking behavior in Taiwan. Soc. Sci. Med. 2008, 67, 1321–1330. [Google Scholar] [CrossRef] [PubMed]
- Zhou, M.; Zhao, S.; Zhao, Z. Gender differences in health insurance coverage in China. Int. J. Equity Health 2021, 20, 52. [Google Scholar] [CrossRef] [PubMed]
- Gao, Z.; Chen, Z.; Sun, A.; Deng, X. Gender differences in cardiovascular disease. Med. Nov. Technol. Devices 2019, 4, 100025. [Google Scholar] [CrossRef]
- Abat, C.; Roussel, Y.; Chaudet, H.; Raoult, D. Alcohol and the global burden of disease. Lancet 2019, 393, 2390–2391. [Google Scholar] [CrossRef] [Green Version]
- Rehm, J.; Roerecke, M. Cardiovascular effects of alcohol consumption. Trends Cardiovasc. Med. 2017, 27, 534–538. [Google Scholar] [CrossRef]
- Chiva-Blanch, G.; Badimon, L. Benefits and Risks of Moderate Alcohol Consumption on Cardiovascular Disease: Current Findings and Controversies. Nutrients 2020, 2, 108. [Google Scholar] [CrossRef] [Green Version]
- Piepoli, M.F.; Abreu, A.; Albus, C.; Ambrosetti, M.; Brotons, C.; Catapano, A.L.; Corra, U.; Cosyns, B.; Deaton, C.; Graham, I.; et al. Update on cardiovascular prevention in clinical practice: A position paper of the European Association of Preventive Cardiology of the European Society of Cardiology. Eur. J. Prev. Cardiol. 2020, 27, 181–205. [Google Scholar] [CrossRef] [Green Version]
- Arnett, D.K.; Blumenthal, R.S.; Albert, M.A.; Buroker, A.B.; Goldberger, Z.D.; Hahn, E.J.; Himmelfarb, C.D.; Khera, A.; Lloyd-Jones, D.; McEvoy, J.W.; et al. 2019 ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J. Am. Coll. Cardiol. 2019, 74, 1376–1414. [Google Scholar] [CrossRef]
- Kloner, R.A.; Rezkalla, S.H. To Drink or Not to Drink? That Is the Question. Circulation 2007, 116, 1306–1317. [Google Scholar] [CrossRef]
- Wu, X.; Zhu, B.; Xu, S.; Bi, Y.; Liu, Y.; Shi, J. A cross country comparison for the burden of cardiovascular disease attributable to tobacco exposure in China, Japan, USA and world. BMC Public Health 2020, 20, 888. [Google Scholar] [CrossRef]
- Global Health Risks: Mortality and Burden of Disease Attributable to Selected Major Risks. World Health Organization. Available online: https://www.who.int/healthinfo/global_burden_disease/GlobalHealthRisks_report_full.pdf (accessed on 26 January 2022).
- Koplan, J.; Eriksen, M. Smoking cessation for Chinese men and prevention for women. Lancet 2015, 386, 1422–1423. [Google Scholar] [CrossRef] [Green Version]

| US (n = 19,932) | China (n = 14,329) | |||
|---|---|---|---|---|
| Men (46.6%) | Women (53.4%) | Men (48.7%) | Women (51.3%) | |
| n (wt%) | n (wt%) | n (wt%) | n (wt%) | |
| Heart disease | ||||
| No | 6190 (75.5) | 8969 (79.4) | 5833 (83.9) | 5640 (77.1) |
| Yes | 2205 (24.5) | 2568 (20.6) | 1166 (16.1) | 1690 (22.9) |
| Age group (years) | ||||
| 50–59 | 2980 (38.6) | 3868 (34.8) | 2695 (38.7) | 2946 (40.2) |
| 60–69 | 2492 (33.7) | 3363 (33.5) | 2671 (37.2) | 2747 (35.7) |
| 70–79 | 1720 (18.4) | 2432 (18.8) | 1293 (18.3) | 1219 (17.0) |
| 80+ | 1203 (9.3) | 1874 (12.9) | 340 (5.8) | 418 (7.1) |
| Median and maximum | 64 and 103 | 65 and 107 | 62 and 101 | 62 and 105 |
| Smoking and drinking behavior | ||||
| Neither | 1151 (12.8) | 3204 (24.3) | 449 (6.9) | 5224 (71.1) |
| Only drinking | 2019 (28.1) | 2703 (26.5) | 732 (10.2) | 1380 (19.3) |
| Only smoking | 1750 (18.4) | 2283 (17.9) | 1538 (21.8) | 505 (6.7) |
| Both | 3475 (40.7) | 3347 (31.3) | 4280 (61.1) | 221 (2.9) |
| Education | ||||
| Less than high school | 1460 (11.9) | 1998 (12.5) | 5836 (82.3) | 6743 (91.7) |
| High school or equivalent | 4207 (48.4) | 6141 (51.6) | 946 (14.5) | 514 (7.0) |
| Associate degree or higher | 2728 (39.7) | 3398 (35.9) | 217 (3.1) | 73 (1.3) |
| Household income | ||||
| Tertile 1 | 2176 (21.4) | 4437 (30.9) | 1441 (19.5) | 1596 (20.9) |
| Tertile 2 | 2897 (30.5) | 3748 (30.5) | 1499 (20.2) | 1528 (19.8) |
| Tertile 3 | 3322 (48.1) | 3352 (38.6) | 1509 (22.4) | 1550 (22.3) |
| Did not report | - | - | 2550 (37.8) | 2656 (37.0) |
| High blood pressure | ||||
| No | 3236 (42.7) | 4475 (45.3) | 4551 (64.4) | 4533 (61.9) |
| Yes | 5159 (57.3) | 7062 (54.7) | 2448 (35.6) | 2797 (38.1) |
| Diabetes | ||||
| No | 6013 (75.2) | 8479 (77.5) | 6317 (90.2) | 6430 (87.8) |
| Yes | 2382 (24.8) | 3058 (22.5) | 682 (9.8) | 900 (12.2) |
| Sleep quality | ||||
| Restless | 1729 (21.1) | 2901 (25.0) | 1755 (24.4) | 2998 (39.4) |
| Good | 6614 (78.4) | 8572 (74.6) | 4839 (69.3) | 3851 (52.7) |
| Did not report | 52 (0.5) | 64 (0.5) | 405 (6.3) | 481 (7.9) |
| BMI | ||||
| Normal | 1779 (20.0) | 3125 (29.3) | 3517 (49.0) | 3330 (45.5) |
| Overweight | 3571 (43.6) | 3563 (30.7) | 1423 (20.8) | 1856 (24.2) |
| Obese | 2907 (35.1) | 4368 (36.0) | 191 (2.7) | 397 (4.9) |
| Underweight | 83 (0.8) | 239 (2.1) | 381 (5.1) | 377 (5.1) |
| Did not report | 55 (0.5) | 242 (1.9) | 1487 (22.5) | 1370 (20.3) |
| Race/ethnicity | ||||
| White | 4924 (73.9) | 6628 (73.8) | - | - |
| Hispanic | 1369 (10.0) | 1785 (10.0) | - | - |
| Black | 1650 (10.0) | 2583 (11.2) | - | - |
| Other | 452 (6.1) | 541 (5.0) | - | - |
| Country | Variables | Men | Women | ||
|---|---|---|---|---|---|
| adjPR * (95% CI) | p | adjPR * (95% CI) | p | ||
| US | Age (years) | ||||
| 50–59 | Ref | Ref | |||
| 60–69 | 1.55 (1.33, 1.81) | <0.001 | 1.51 (1.27, 1.79) | <0.001 | |
| 70–79 | 2.11 (1.84, 2.43) | <0.001 | 1.89 (1.63, 2.19) | <0.001 | |
| 80+ | 3.04 (2.64, 3.49) | <0.001 | 2.51 (2.14, 2.96) | <0.001 | |
| Smoking/drinking behavior | |||||
| Neither | Ref | Ref | |||
| Only drinking | 0.75 (0.63, 0.89) | 0.001 | 0.92 (0.78, 1.09) | 0.309 | |
| Only smoking | 1.16 (1.01, 1.35) | 0.046 | 1.34 (1.21, 1.49) | <0.001 | |
| Both | 1.02 (0.89, 1.16) | 0.817 | 0.97 (0.85, 1.11) | 0.675 | |
| China | Age (years) | ||||
| 50–59 | Ref | Ref | |||
| 60–69 | 1.68 (1.40, 2.01) | <0.001 | 1.36 (1.19, 1.55) | <0.001 | |
| 70–79 | 2.31 (1.95, 2.73) | <0.001 | 1.50 (1.30, 1.74) | <0.001 | |
| 80+ | 1.96 (1.40, 2.74) | <0.001 | 1.31 (1.04, 1.65) | 0.024 | |
| Smoking/drinking behavior | |||||
| Neither | Ref | Ref | |||
| Only drinking | 1.23 (0.87, 1.76) | 0.246 | 1.01 (0.86, 1.18) | 0.948 | |
| Only smoking | 1.35 (0.94, 1.95) | 0.103 | 1.48 (1.29, 1.70) | <0.001 | |
| Both | 1.26 (0.91, 1.74) | 0.162 | 1.54 (1.25, 1.89) | <0.001 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Li, Y.; Lu, Y.; Hurwitz, E.L.; Wu, Y. Gender Disparities of Heart Disease and the Association with Smoking and Drinking Behavior among Middle-Aged and Older Adults, a Cross-Sectional Study of Data from the US Health and Retirement Study and the China Health and Retirement Longitudinal Study. Int. J. Environ. Res. Public Health 2022, 19, 2188. https://doi.org/10.3390/ijerph19042188
Li Y, Lu Y, Hurwitz EL, Wu Y. Gender Disparities of Heart Disease and the Association with Smoking and Drinking Behavior among Middle-Aged and Older Adults, a Cross-Sectional Study of Data from the US Health and Retirement Study and the China Health and Retirement Longitudinal Study. International Journal of Environmental Research and Public Health. 2022; 19(4):2188. https://doi.org/10.3390/ijerph19042188
Chicago/Turabian StyleLi, Yifei, Yuanan Lu, Eric L. Hurwitz, and Yanyan Wu. 2022. "Gender Disparities of Heart Disease and the Association with Smoking and Drinking Behavior among Middle-Aged and Older Adults, a Cross-Sectional Study of Data from the US Health and Retirement Study and the China Health and Retirement Longitudinal Study" International Journal of Environmental Research and Public Health 19, no. 4: 2188. https://doi.org/10.3390/ijerph19042188
APA StyleLi, Y., Lu, Y., Hurwitz, E. L., & Wu, Y. (2022). Gender Disparities of Heart Disease and the Association with Smoking and Drinking Behavior among Middle-Aged and Older Adults, a Cross-Sectional Study of Data from the US Health and Retirement Study and the China Health and Retirement Longitudinal Study. International Journal of Environmental Research and Public Health, 19(4), 2188. https://doi.org/10.3390/ijerph19042188






