Gaming Behaviors and the Association with Sleep Duration, Social Jetlag, and Difficulties Falling Asleep among Norwegian Adolescents
Abstract
:1. Introduction
2. Methods
2.1. Design and Data Collection
2.2. Measures
2.2.1. Gaming Behavior
2.2.2. Sleep Variables
2.2.3. Socioeconomic Status
2.2.4. Physical Activity
2.3. Statistics
3. Results
3.1. Baseline Characteristics
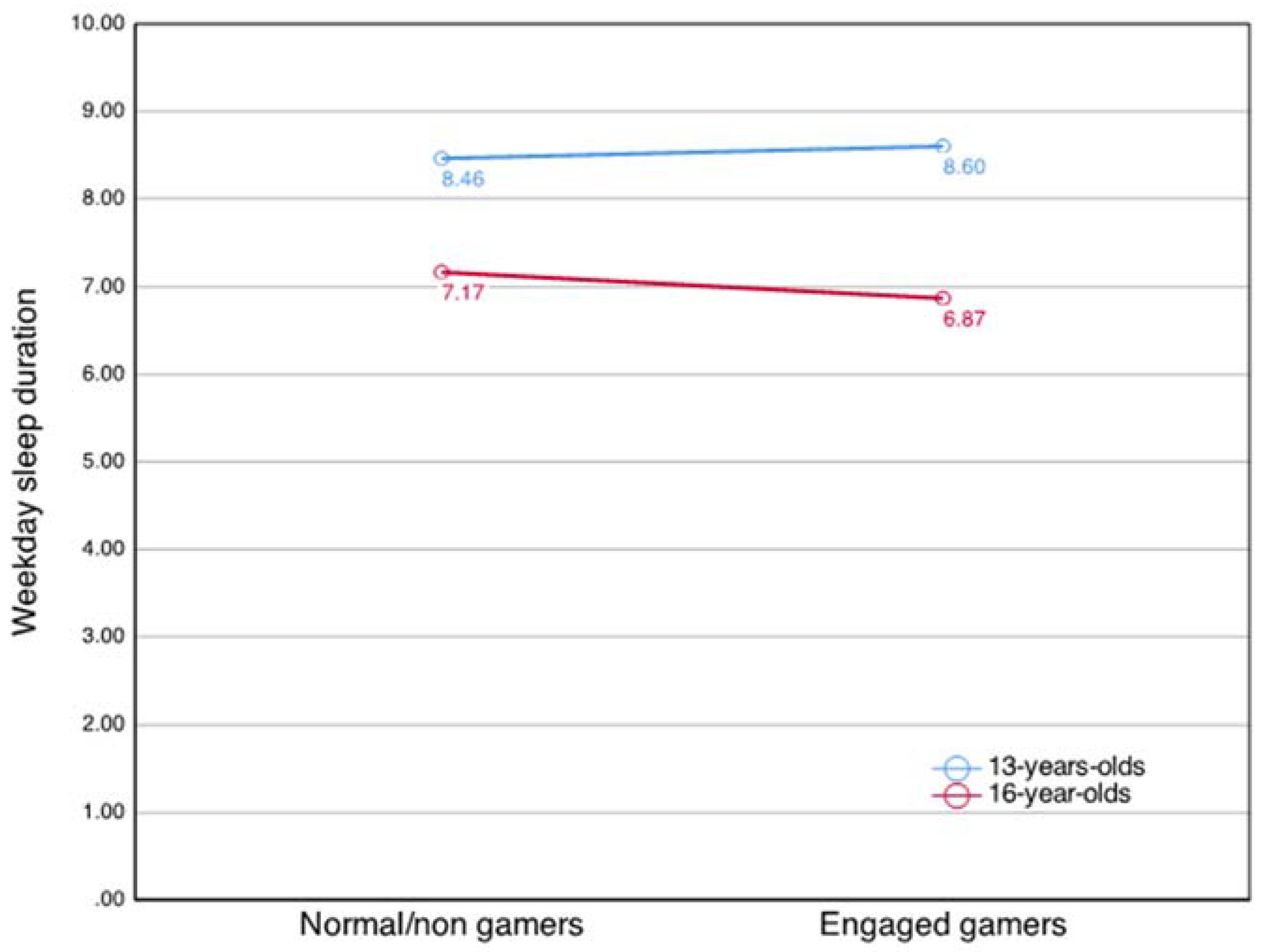
3.2. Association between Gaming Behavior and Sleep Duration in Weekdays and Weekends
3.3. Associations between Gaming Behaviors, Social Jetlag, and Problems Falling Asleep
4. Discussion
4.1. Strengths and Limitations
4.2. Implications and Directions for Future Research
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- King, D.; Delfabbro, P.; Liem, T.; Dobler, T.K. Internet Gaming Disorder: Theory, Assessment, Treatment, and Prevention; Elsevier Science & Technology: San Diego, CA, USA, 2018. [Google Scholar]
- WHO. Gaming Disorder. Available online: https://www.who.int/news-room/q-a-detail/gaming-disorder (accessed on 10 January 2022).
- WHO. Inclusion of “Gaming Disorder” in ICD-11. Available online: https://www.who.int/news-room/detail/14-09-2018-inclusion-of-gaming-disorder-in-icd-11 (accessed on 9 November 2020).
- Tubbs, A.S.; Dollish, H.K.; Fernandez, F.; Grandner, M.A. Chapter 1—The basics of sleep physiology and behavior. In Sleep and Health; Grandner, M.A., Ed.; Academic Press: Cambridge, MA, USA, 2019; pp. 3–10. [Google Scholar]
- Buysse, D.J. Sleep Health: Can We Define It? Does It Matter? Sleep 2014, 37, 9–17. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gariepy, G.; Danna, S.; Gobina, I.; Rasmussen, M.; de Matos, M.G.; Tynjälä, J.; Janssen, I.; Kalman, M.; Villeruša, A.; Husarova, D.; et al. How Are Adolescents Sleeping? Adolescent Sleep Patterns and Sociodemographic Differences in 24 European and North American Countries. J. Adolesc. Health 2020, 66, S81–S88. [Google Scholar] [CrossRef] [PubMed]
- Ghekiere, A.; Van Cauwenberg, J.; Vandendriessche, A.; Inchley, J.; de Matos, M.G.; Borraccino, A.; Gobina, I.; Tynjälä, J.; Deforche, B.; De Clercq, B. Trends in sleeping difficulties among European adolescents: Are these associated with physical inactivity and excessive screen time? Int. J. Public Health 2018, 64, 487–498. [Google Scholar] [CrossRef] [Green Version]
- Hysing, M.; Pallesen, S.; Stormark, K.M.; Lundervold, A.J.; Sivertsen, B. Sleep patterns and insomnia among adolescents: A population-based study. J. Sleep Res. 2013, 22, 549–556. [Google Scholar] [CrossRef] [PubMed]
- Saxvig, I.W.; Bjorvatn, B.; Hysing, M.; Sivertsen, B.; Gradisar, M.; Pallesen, S. Sleep in older adolescents. Results from a large cross-sectional, population-based study. J. Sleep Res. 2021, 30, e13263. [Google Scholar] [CrossRef] [PubMed]
- Lovato, N.; Gradisar, M. A meta-analysis and model of the relationship between sleep and depression in adolescents: Recommendations for future research and clinical practice. Sleep Med. Rev. 2014, 18, 521–529. [Google Scholar] [CrossRef] [PubMed]
- Scott, J.; Kallestad, H.; Vedaa, O.; Sivertsen, B.; Etain, B. Sleep disturbances and first onset of major mental disorders in adolescence and early adulthood: A systematic review and meta-analysis. Sleep Med. Rev. 2021, 57, 101429. [Google Scholar] [CrossRef]
- Bauducco, S.; Richardson, C.; Gradisar, M. Chronotype, circadian rhythms and mood. Curr. Opin. Psychol. 2020, 34, 77–83. [Google Scholar] [CrossRef]
- Fatima, Y.; Doi, S.; Mamun, A.A. Longitudinal impact of sleep on overweight and obesity in children and adolescents: A systematic review and bias-adjusted meta-analysis. Obes. Rev. 2015, 16, 137–149. [Google Scholar] [CrossRef]
- Matthews, K.A.; Pantesco, E. Sleep characteristics and cardiovascular risk in children and adolescents: An enumerative review. Sleep Med. 2016, 18, 36–49. [Google Scholar] [CrossRef] [Green Version]
- Sabia, J.J.; Wang, K.; Cesur, R. Sleepwalking Through School: New Evidence on Sleep and Academic Achievement. Contemp. Econ. Policy 2016, 35, 331–344. [Google Scholar] [CrossRef]
- Galland, B.C.; Short, M.A.; Terrill, P.; Rigney, G.; Haszard, J.J.; Coussens, S.; Foster-Owens, M.; Biggs, S.N. Establishing normal values for pediatric nighttime sleep measured by actigraphy: A systematic review and meta-analysis. Sleep 2018, 41. [Google Scholar] [CrossRef] [PubMed]
- Wittmann, M.; Dinich, J.; Merrow, M.; Roenneberg, T. Social Jetlag: Misalignment of Biological and Social Time. Chronobiol. Int. 2006, 23, 497–509. [Google Scholar] [CrossRef] [PubMed]
- Crowley, S.J.; Wolfson, A.R.; Tarokh, L.; Carskadon, M.A. An update on adolescent sleep: New evidence informing the perfect storm model. J. Adolesc. 2018, 67, 55–65. [Google Scholar] [CrossRef]
- Jankowski, K.S. Social jet lag: Sleep-corrected formula. Chronobiol. Int. 2017, 34, 531–535. [Google Scholar] [CrossRef]
- Díaz-Morales, J.F.; Escribano, C. Social jetlag, academic achievement and cognitive performance: Understanding gender/sex differences. Chronobiol. Int. 2015, 32, 822–831. [Google Scholar] [CrossRef] [Green Version]
- Sun, W.; Ling, J.; Zhu, X.; Lee, T.M.-C.; Li, S.X. Associations of weekday-to-weekend sleep differences with academic performance and health-related outcomes in school-age children and youths. Sleep Med. Rev. 2019, 46, 27–53. [Google Scholar] [CrossRef]
- Henderson, S.E.M.; Brady, E.M.; Robertson, N. Associations between social jetlag and mental health in young people: A systematic review. Chronobiol. Int. 2019, 36, 1316–1333. [Google Scholar] [CrossRef]
- Caliandro, R.; Streng, A.A.; van Kerkhof, L.W.M.; van der Horst, G.T.J.; Chaves, I. Social Jetlag and Related Risks for Human Health: A Timely Review. Nutrients 2021, 13, 4543. [Google Scholar] [CrossRef]
- Cain, N.; Gradisar, M. Electronic media use and sleep in school-aged children and adolescents: A review. Sleep Med. 2010, 11, 735–742. [Google Scholar] [CrossRef]
- Exelmans, L.; Bulck, J.V.D. Bedtime, shuteye time and electronic media: Sleep displacement is a two-step process. J. Sleep Res. 2017, 26, 364–370. [Google Scholar] [CrossRef] [PubMed]
- Wu, X.; Tao, S.; Zhang, Y.; Zhang, S.; Tao, F. Low Physical Activity and High Screen Time Can Increase the Risks of Mental Health Problems and Poor Sleep Quality among Chinese College Students. PLoS ONE 2015, 10, e0119607. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Melkevik, O.; Torsheim, T.; Iannotti, R.J.; Wold, B. Is spending time in screen-based sedentary behaviors associated with less physical activity: A cross national investigation. Int. J. Behav. Nutr. Phys. Act. 2010, 7, 46. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Choo, H.; Sim, T.; Liau, A.K.F.; Gentile, D.A.; Khoo, A. Parental Influences on Pathological Symptoms of Video-Gaming Among Children and Adolescents: A Prospective Study. J. Child Fam. Stud. 2015, 24, 1429–1441. [Google Scholar] [CrossRef]
- van der Lely, S.; Frey, S.; Garbazz, a.C.; Wirz-Justice, A.; Jenni, O.G.; Steiner, R.; Wolf, S.; Cajochen, C.; Bromundt, V.; Schmidt, C. Blue Blocker Glasses as a Countermeasure for Alerting Effects of Evening Light-Emitting Diode Screen Exposure in Male Teenagers. J. Adolesc. Health 2015, 56, 113–119. [Google Scholar] [CrossRef]
- Wood, B.; Rea, M.S.; Plitnick, B.; Figueiro, M.G. Light level and duration of exposure determine the impact of self-luminous tablets on melatonin suppression. Appl. Ergon. 2013, 44, 237–240. [Google Scholar] [CrossRef]
- Chang, A.-M.; Aeschbach, D.; Duffy, J.F.; Czeisler, C.A. Evening use of light-emitting eReaders negatively affects sleep, circadian timing, and next-morning alertness. Proc. Natl. Acad. Sci. USA 2015, 112, 1232–1237. [Google Scholar] [CrossRef] [Green Version]
- Zerbini, G.; Kantermann, T.; Merrow, M. Strategies to decrease social jetlag: Reducing evening blue light advances sleep and melatonin. Eur. J. Neurosci. 2020, 51, 2355–2366. [Google Scholar] [CrossRef]
- King, D.L.; Gradisar, M.; Drummond, A.; Lovato, N.; Wessel, J.; Micic, G.; Douglas, P.; Delfabbro, P. The impact of prolonged violent video-gaming on adolescent sleep: An experimental study. J. Sleep Res. 2012, 22, 137–143. [Google Scholar] [CrossRef]
- Gentile, D.A.; Bender, P.K.; Anderson, C.A. Violent video game effects on salivary cortisol, arousal, and aggressive thoughts in children. Comput. Hum. Behav. 2017, 70, 39–43. [Google Scholar] [CrossRef]
- Mei, X.; Zhou, Q.; Li, X.; Jing, P.; Wang, X.; Hu, Z. Sleep problems in excessive technology use among adolescent: A systemic review and meta-analysis. Sleep Sci. Pr. 2018, 2, 9. [Google Scholar] [CrossRef]
- Hale, L.; Guan, S. Screen time and sleep among school-aged children and adolescents: A systematic literature review. Sleep Med. Rev. 2015, 21, 50–58. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hena, M.; Garmy, P. Social Jetlag and Its Association With Screen Time and Nighttime Texting Among Adolescents in Sweden: A Cross-Sectional Study. Front. Neurosci. 2020, 14, 122. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gamble, A.L.; D’Rozario, A.; Bartlett, D.J.; Williams, S.; Bin, Y.S.; Grunstein, R.R.; Marshall, N.S. Adolescent Sleep Patterns and Night-Time Technology Use: Results of the Australian Broadcasting Corporation’s Big Sleep Survey. PLoS ONE 2014, 9, e111700. [Google Scholar] [CrossRef] [Green Version]
- Kristensen, J.H.; Pallesen, S.; King, D.L.; Hysing, M.; Erevik, E.K. Problematic Gaming and Sleep: A Systematic Review and Meta-Analysis. Front. Psychiatry 2021, 12. [Google Scholar] [CrossRef]
- Aarseth, E.; Bean, A.M.; Boonen, H.; Carras, M.C.; Coulson, M.; Das, D.; Deleuze, J.; Dunkels, E.; Edman, J.; Ferguson, C.J.; et al. Scholars’ open debate paper on the World Health Organization ICD-11 Gaming Disorder proposal. J. Behav. Addict. 2017, 6, 267–270. [Google Scholar] [CrossRef]
- Griffiths, M.D.; Van Rooij, A.J.; Kardefelt-Winther, D.; Starčević, V.; Király, O.; Pallesen, S.; Müller, K.; Dreier, M.; Carras, M.; Prause, N.; et al. Working towards an international consensus on criteria for assessing internet gaming disorder: A critical commentary on Petry et al. Addiction 2015, 111, 167–175. [Google Scholar] [CrossRef] [Green Version]
- King, D.; Chamberlain, S.R.; Carragher, N.; Billieux, J.; Stein, D.; Mueller, K.; Potenza, M.N.; Rumpf, H.J.; Saunders, J.; Starcevic, V.; et al. Screening and assessment tools for gaming disorder: A comprehensive systematic review. Clin. Psychol. Rev. 2020, 77, 101831. [Google Scholar] [CrossRef]
- Brown, R. Some Contributions of the Study of Gambling to the Study of Other Addictions; University of Nevada Press: Reno, NV, USA, 1993. [Google Scholar]
- King, D.L.; Delfabbro, P.H.; Gainsbury, S.M.; Dreier, M.; Greer, N.; Billieux, J. Unfair play? Video games as exploitative monetized services: An examination of game patents from a consumer protection perspective. Comput. Hum. Behav. 2019, 101, 131–143. [Google Scholar] [CrossRef]
- Lemmens, J.S.; Valkenburg, P.M.; Peter, J. Development and Validation of a Game Addiction Scale for Adolescents. Media Psychol. 2009, 12, 77–95. [Google Scholar] [CrossRef]
- Charlton, J.P.; Danforth, I.D. Distinguishing addiction and high engagement in the context of online game playing. Comput. Hum. Behav. 2007, 23, 1531–1548. [Google Scholar] [CrossRef] [Green Version]
- Charlton, J.P.; Danforth, I.D.W. Validating the distinction between computer addiction and engagement: Online game playing and personality. Behav. Inf. Technol. 2010, 29, 601–613. [Google Scholar] [CrossRef]
- Brunborg, G.S.; Hanss, D.; Mentzoni, R.A.; Pallesen, S. Core and peripheral criteria of video game addiction in the game addiction scale for adolescents. Cyberpsychol. Behav. Soc. Netw. 2015, 18, 280–285. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brunborg, G.; Mentzoni, R.A.; Melkevik, O.R.; Torsheim, T.; Samdal, O.; Hetland, J.; Andreassen, C.S.; Palleson, S. Gaming Addiction, Gaming Engagement, and Psychological Health Complaints Among Norwegian Adolescents. Media Psychol. 2013, 16, 115–128. [Google Scholar] [CrossRef]
- Thorsteinsson, E.; Potrebny, T.; Arnarsson Ársaell, M.; Tynjälä, J.; Välimaa, R.; Eriksson, C. Trends in sleeping difficulty among adolescents in five Nordic countries 2002–2014. Nord. Välfärdsforskning Nord. Welf. Res. 2019, 4, 77–87. [Google Scholar] [CrossRef] [Green Version]
- Wittek, C.T.; Finserås, T.R.; Pallesen, S.; Mentzoni, R.A.; Hanss, D.O.; Griffiths, M.; Molde, H. Prevalence and Predictors of Video Game Addiction: A Study Based on a National Representative Sample of Gamers. Int. J. Ment. Health Addict. 2016, 14, 672–686. [Google Scholar] [CrossRef] [Green Version]
- Inchley, J.; Currie, D.; Cosma, A.; Samdal, O. Health Behaviour in School-Aged Children (HBSC) Study Protocol: Background, Methodology and Mandatory Items for the 2017/18 Survey; CAHRU: St Andrews, Scotland, 2018. [Google Scholar]
- WHO. Spotlight on Adolescent Health and Well-Being. Findings from the 2017/2018 Health Behaviour in School-Aged Children (HBSC) Survey in Europe and Canada. International Report; WHO Regional Office for Europe: Copenhagen, Denmark, 2020; Volume 2. [Google Scholar]
- Torsheim, T.; Cavallo, F.; Levin, K.A.; Schnohr, C.; Mazur, J.; Niclasen, B.; Currie, C. Psychometric validation of the Revised Family Affluence Scale: A latent variable approach. Child. Indic. Res. 2016, 9, 771–784. [Google Scholar] [CrossRef] [Green Version]
- Prochaska, J.J.; Sallis, J.F.; Long, B.A. Physical Activity Screening Measure for Use with Adolescents in Primary Care. Arch. Pediatr. Adolesc. Med. 2001, 155, 554–559. [Google Scholar] [CrossRef]
- Enders, C.K. Applied Missing Data Analysis; Guilford Press: New York, NY, USA, 2010. [Google Scholar]
- Männikkö, N.; Ruotsalainen, H.; Miettunen, J.; Pontes, H.M.; Kääriäinen, M. Problematic gaming behaviour and health-related outcomes: A systematic review and meta-analysis. J. Health Psychol. 2017, 25, 67–81. [Google Scholar] [CrossRef] [Green Version]
- Hawi, N.S.; Samaha, M.; Griffiths, M.D. Internet gaming disorder in Lebanon: Relationships with age, sleep habits, and academic achievement. J. Behav. Addict. 2018, 7, 70–78. [Google Scholar] [CrossRef]
- Männikkö, N.; Ruotsalainen, H.; Tolvanen, A.; Kääriäinen, M. Problematic Gaming Is Associated with Some Health-Related Behaviors Among Finnish Vocational School Students. Int. J. Ment. Health Addict. 2020, 18, 993–1007. [Google Scholar] [CrossRef] [Green Version]
- Al Asqah, M.I.; Al Orainey, A.I.; Shukr, M.A.; Al Oraini, H.M.; Al Turki, Y.A. The prevalence of internet gaming disorder among medical students at King Saud University, Riyadh, Saudi Arabia. Saudi Med. J. 2020, 41, 1359–1363. [Google Scholar] [CrossRef] [PubMed]
- Hysing, M.; Pallesen, S.; Stormark, K.M.; Jakobsen, R.; Lundervold, A.J.; Sivertsen, B. Sleep and use of electronic devices in adolescence: Results from a large population-based study. BMJ Open 2015, 5, e006748. [Google Scholar] [CrossRef] [Green Version]
- Pyper, E.; Harrington, D.; Manson, H. Do parents’ support behaviours predict whether or not their children get sufficient sleep? A cross-sectional study. BMC Public Health 2017, 17, 432. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Männikkö, N.; Billieux, J.; Kääriäinen, M. Problematic digital gaming behavior and its relation to the psychological, social and physical health of Finnish adolescents and young adults. J. Behav. Addict. 2015, 4, 281–288. [Google Scholar] [CrossRef] [PubMed]
- Rehbein, F.; Kliem, S.; Baier, D.; Mößle, T.; Petry, N.M. Prevalence of internet gaming disorder in German adolescents: Diagnostic contribution of the nine DSM-5 criteria in a state-wide representative sample. Addiction 2015, 110, 842–851. [Google Scholar] [CrossRef] [PubMed]
- King, D.L.; Delfabbro, P.H.; Zwaans, T.; Kaptsis, D. Sleep Interference Effects of Pathological Electronic Media Use during Adolescence. Int. J. Ment. Health Addict. 2013, 12, 21–35. [Google Scholar] [CrossRef]
- Wang, Q.; Mati, K.; Cai, Y. The link between problematic internet use, problematic gaming, and psychological distress: Does sleep quality matter? BMC Psychiatry 2021, 21, 103. [Google Scholar] [CrossRef]
- Wong, H.Y.; Mo, H.Y.; Potenza, M.N.; Chan, M.N.M.; Lau, W.M.; Chui, T.K.; Pakpour, A.H.; Lin, C.-Y. Relationships between Severity of Internet Gaming Disorder, Severity of Problematic Social Media Use, Sleep Quality and Psychological Distress. Int. J. Environ. Res. Public Health 2020, 17, 1879. [Google Scholar] [CrossRef] [Green Version]
- Yu, Y.; Yang, X.; Wang, S.; Wang, H.; Chang, R.; Tsamlag, L.; Zhang, S.; Xu, C.; Yu, X.; Cai, Y.; et al. Serial multiple mediation of the association between internet gaming disorder and suicidal ideation by insomnia and depression in adolescents in Shanghai, China. BMC Psychiatry 2020, 20, 1–9. [Google Scholar] [CrossRef]
- Lin, C.-Y.; Potenza, M.N.; Broström, A.; Pakpour, A.H. Internet gaming disorder, psychological distress, and insomnia in adolescent students and their siblings: An actor-partner interdependence model approach. Addict. Behav. Rep. 2021, 13, 100332. [Google Scholar] [CrossRef] [PubMed]
- Al Gammal, M.A.F.S.; Elsheikh, M.M.A.; Abozahra, A.A.E. Internet Addiction and Internet Gaming Disorder and Associated Insomnia among a Sample of Al-Azhar University Students, Clinical Study. Egypt. J. Hosp. Med. 2019, 77, 5718–5726. [Google Scholar] [CrossRef]
- Eggermont, S.; Bulck, J.V.D. Nodding off or switching off? The use of popular media as a sleep aid in secondary-school children. J. Paediatr. Child. Health 2006, 42, 428–433. [Google Scholar] [CrossRef] [PubMed]
- Bulck, J.V.D. Television Viewing, Computer Game Playing, and Internet Use and Self-Reported Time to Bed and Time out of Bed in Secondary-School Children. Sleep 2004, 27, 101–104. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nakayama, H.; Matsuzaki, T.; Mihara, S.; Kitayuguchi, T.; Higuchi, S. Relationship between problematic gaming and age at the onset of habitual gaming. Pediatr. Int. 2020, 62, 1275–1281. [Google Scholar] [CrossRef]
- Csikszentmihalyi, M. Flow and Education. In Applications of Flow in Human Development and Education: The Collected Works of Mihaly Csikszentmihalyi; Csikszentmihalyi, M., Ed.; Springer: Dordrecht, The Netherlands, 2014; pp. 129–151. [Google Scholar]
- Smith, L.J.; Gradisar, M.; King, D.; Short, M. Intrinsic and extrinsic predictors of video-gaming behaviour and adolescent bedtimes: The relationship between flow states, self-perceived risk-taking, device accessibility, parental regulation of media and bedtime. Sleep Med. 2017, 30, 64–70. [Google Scholar] [CrossRef]
- Barr, M.; Copeland-Stewart, A. Playing Video Games During the COVID-19 Pandemic and Effects on Players’ Well-Being. Games Cult. 2021, 17, 122–139. [Google Scholar] [CrossRef]
- Ipsos. Video Gaming in Lockdown—The Impact of Covid-19 on Video Gameplay Behaviours and Attitudes; Ipsos: Paris, France, 2020. [Google Scholar]
- Teng, Z.; Pontes, H.M.; Nie, Q.; Griffiths, M.D.; Guo, C. Depression and anxiety symptoms associated with internet gaming disorder before and during the COVID-19 pandemic: A longitudinal study. J. Behav. Addict. 2021, 10, 169–180. [Google Scholar] [CrossRef]
- Fazeli, S.; Zeidi, I.M.; Lin, C.-Y.; Namdar, P.; Griffiths, M.D.; Ahorsu, D.K.; Pakpour, A.H. Depression, anxiety, and stress mediate the associations between internet gaming disorder, insomnia, and quality of life during the COVID-19 outbreak. Addict. Behav. Rep. 2020, 12, 100307. [Google Scholar] [CrossRef]
- She, R.; Wong, K.; Lin, J.; Leung, K.; Zhang, Y.; Yang, X. How COVID-19 stress related to schooling and online learning affects adolescent depression and Internet gaming disorder: Testing Conservation of Resources theory with sex difference. J. Behav. Addict. 2021, 10, 953–966. [Google Scholar] [CrossRef]
- Arora, T.; Broglia, E.; Pushpakumar, D.; Lodhi, T.; Taheri, S. An Investigation into the Strength of the Association and Agreement Levels between Subjective and Objective Sleep Duration in Adolescents. PLoS ONE 2013, 8, e72406. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Variable | Estimate |
| Female gender % (n) | 50.2 (1614) |
| Age % (n) | |
| 13-year olds | 31.7 (1024) |
| 16-year olds | 68.3 (2204) |
| Family Affluence % (n) | |
| Low | 20.6 (646) |
| Middle | 62.4 (1957) |
| High | 17.0 (534) |
| MVPA ≥ 5 days % (n) | 36.3 (1174) |
| Family affluence (SD) | 7.79 (1.80) |
| Gaming behavior % (n) | |
| Addicted | 4.40 (123) |
| Problem | 14.9 (416) |
| Engaged | 6.40 (179) |
| Normal/nongamers | 74.2 (2069) |
| Sleep measures | |
| Weekday sleep duration (SD) | 7.83 (1.17) |
| Weekend sleep duration (SD) | 9.64 (1.36) |
| Social Jetlag (SD) * | 1.88 (1.13) |
| Weekly sleeping difficulties % (n) | 23.2 (774) |
| Model 1 | Model 2 | Model 3 | |||||||
|---|---|---|---|---|---|---|---|---|---|
| b | CI 95% | p | b | CI 95% | p | b | CI 95% | p | |
| Addicted | −0.48 | [−0.71, −0.25] | 0.000 | −0.56 | [−0.80, −0.31] | 0.000 | −0.40 | [−0.84, −0.46] | 0.079 |
| Problem | −0.07 | [−0.20, 0.06] | 0.293 | −0.09 | [−0.21, 0.04] | 0.172 | 0.26 | [−0.16, 0.21] | 0.788 |
| Engaged | −0.15 | [−0.35, 0.06] | 0.161 | −0.13 | [−0.34, 0.08] | 0.217 | 0.15 | [−0.12, 0.42] | 0.284 |
| Age 16 | −1.15 | [−1.28, −1.02] | 0.000 | −1.08 | [−1.21, −0.95] | 0.000 | |||
| Gender female | −0.07 | [−0.18, 0.03] | 0.151 | −0.08 | [−0.19, 0.17] | 0.033 | |||
| SES | 0.01 | [−0.03, 0.02] | 0.562 | −0.01 | [−0.04, 0.02] | 0.532 | |||
| MVPA ≥ 5 days | 0.09 | [−0.19, −0.01] | 0.046 | −0.10 | [0.19, 0.01] | 0.038 | |||
| Addicted × age | −0.23 | [−0.76, −0.30] | 0.390 | ||||||
| Problem × age | −0.19 | [−0.25, −0.02] | 0.133 | ||||||
| Engaged × age | −0.45 | [−0.82, −0.06] | 0.022 | ||||||
| Random intercept | 80.02 | [7.91, 8.13] | 0.000 | 8.84 | [8.60, 90.07] | 0.000 | 8.79 | [8.55, 90.03] | 0.000 |
| Model 1 | Model 2 | Model 3 | |||||||
|---|---|---|---|---|---|---|---|---|---|
| b | CI 95% | p | b | CI 95% | p | b | CI 95% | p | |
| Addicted | −0.42 | [−0.72, −0.13] | 0.004 | −0.40 | [−0.69, −0.11] | 0.008 | −0.48 | [−0.94, −0.01] | 0.045 |
| Problem | −0.10 | [−0.25, 0.05] | 0.176 | −0.08 | [−0.24, 0.06] | 0.332 | −0.12 | [−0.32, 0.09] | 0.281 |
| Engaged | −0.24 | [−0.49, 0.00] | 0.054 | −0.32 | [−0.58, −0.05] | 0.019 | −0.50 | [−0.92, −0.09] | 0.016 |
| Age 16 | −0.51 | [−0.62, 0.40] | 0.000 | −0.54 | [−0.66, −0.43] | 0.000 | |||
| Gender female | 0.09 | [−0.04, 0.22] | 0.181 | 0.09 | [−0.04, 0.21] | 0.193 | |||
| SES | 0.00 | [−0.03, 0.04] | 0.791 | 0.01 | [−0.03, 0.04] | 0.776 | |||
| MVPA ≥ 5 days | 0.01 | [−0.10, 0.12] | 0.888 | 0.01 | [−0.10, 0.12] | 0.860 | |||
| Addicted × age | 0.11 | [−0.50, 0.72] | 0.722 | ||||||
| Problem × age | 0.05 | [−0.25, 0.34] | 0.740 | ||||||
| Engaged × age | 0.30 | [−0.21, 0.82] | 0.257 | ||||||
| Random intercept | 9.71 | [9.63, 9.79] | 0.000 | 9.95 | [9.62, 10.27] | 0.000 | 9.97 | [9.65, 10.28] | 0.000 |
| Model 1 | Model 2 | Model 3 | |||||||
|---|---|---|---|---|---|---|---|---|---|
| b | CI 95% | p | b | CI 95% | p | b | CI 95% | p | |
| Addicted | 0.35 | [0.13, 0.57] | 0.002 | 0.26 | [0.02, 0.51] | 0.038 | 0.23 | [−0.15, 0.61] | 0.232 |
| Problem | 0.22 | [0.11, 0.34] | 0.000 | 0.14 | [0.03, 0.25] | 0.014 | 0.18 | [0.03, 0.33] | 0.019 |
| Engaged | 0.29 | [0.10, 0.48] | 0.003 | 0.30 | [0.12, 0.49] | 0.001 | 0.40 | [0.15, 0.65] | 0.002 |
| Age 16 | 0.14 | [0.02, 0.26] | 0.023 | 0.16 | [0.04, 0.29] | 0.013 | |||
| Gender female | −0.16 | [−0.25, −0.06] | 0.001 | −0.15 | [−0.25, −0.06] | 0.001 | |||
| SES | 0.03 | [0.01, 0.06] | 0.006 | −0.03 | [0.01, 0.06] | 0.007 | |||
| MVPA ≥ 5 days | 0.07 | [−0.01, 0.16] | 0.097 | −0.07 | [−0.01, 0.16] | 0.103 | |||
| Addicted × age | 0.04 | [−0.44, 0.53] | 0.860 | ||||||
| Problem × age | −0.08 | [−0.29, 0.14] | 0.475 | ||||||
| Engaged × age | −0.16 | [−0.52, 0.20] | 0.385 | ||||||
| Random intercept | 1.84 | [1.77, 1.90] | 0.000 | 1.52 | [1.30, 1.74] | 0.000 | 1.51 | [1.29, 1.73] | 0.000 |
| Model 1 | Model 2 | Model 3 | |||||||
|---|---|---|---|---|---|---|---|---|---|
| O.R | CI 95% | p | O.R | CI 95% | p | O.R | CI 95% | p | |
| Addicted | 1.48 | [0.97, 2.27] | 0.072 | 1.89 | [1.19, 3.02] | 0.007 | 1.83 | [0.76, 4.40] | 0.179 |
| Problem | 1.58 | [1.25, 1.99] | 0.000 | 1.98 | [1.51, 2.60] | 0.000 | 2.08 | [1.38, 3.14] | 0.000 |
| Engaged | 1.38 | [0.96,2.00] | 0.082 | 1.42 | [0.91, 2.21] | 0.120 | 1.30 | [0.68, 2.48] | 0.433 |
| Age 16 | 1.17 | [0.95, 1.45] | 0.135 | 1.18 | [0.94, 1.49] | 0.157 | |||
| Gender female | 1.71 | [1.36, 2.15] | 0.000 | 1.71 | [1.36, 2.15] | 0.000 | |||
| SES | 0.95 | [0.91, 1.00] | 0.059 | 0.95 | [0.91, 1.00] | 0.057 | |||
| MVPA ≥ 5 days | 1.23 | [1.02, 1.49] | 0.028 | 1.23 | [1.02, 1.49] | 0.027 | |||
| Addicted × age | 1.05 | [0.38, 2.93] | 0.926 | ||||||
| Problem × age | 0.92 | [0.55, 1.52] | 0.730 | ||||||
| Engaged × age | 1.15 | [0.50, 2.63] | 0.743 | ||||||
| Random intercept | 0.29 | [0.26, 0.33] | 0.000 | 0.23 | [0.14, 0.36] | 0.000 | 0.23 | [0.14, 0.36] | 0.000 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hamre, R.; Smith, O.R.F.; Samdal, O.; Haug, E. Gaming Behaviors and the Association with Sleep Duration, Social Jetlag, and Difficulties Falling Asleep among Norwegian Adolescents. Int. J. Environ. Res. Public Health 2022, 19, 1765. https://doi.org/10.3390/ijerph19031765
Hamre R, Smith ORF, Samdal O, Haug E. Gaming Behaviors and the Association with Sleep Duration, Social Jetlag, and Difficulties Falling Asleep among Norwegian Adolescents. International Journal of Environmental Research and Public Health. 2022; 19(3):1765. https://doi.org/10.3390/ijerph19031765
Chicago/Turabian StyleHamre, Regina, Otto Robert Frans Smith, Oddrun Samdal, and Ellen Haug. 2022. "Gaming Behaviors and the Association with Sleep Duration, Social Jetlag, and Difficulties Falling Asleep among Norwegian Adolescents" International Journal of Environmental Research and Public Health 19, no. 3: 1765. https://doi.org/10.3390/ijerph19031765
APA StyleHamre, R., Smith, O. R. F., Samdal, O., & Haug, E. (2022). Gaming Behaviors and the Association with Sleep Duration, Social Jetlag, and Difficulties Falling Asleep among Norwegian Adolescents. International Journal of Environmental Research and Public Health, 19(3), 1765. https://doi.org/10.3390/ijerph19031765






