Examining Clinical Practice Guidelines for Exercise and Physical Activity as Part of Rehabilitation for People with Stroke: A Systematic Review
Abstract
1. Background
2. Methods
2.1. Registration, Selection Criteria
2.2. Databases
- National Institute of Health and Care Excellence (NICE)
- Turning Research Into Practice (TRIP)
- Scottish Intercollegiate Guideline Network (SIGN)
- International Guidelines Library
- British Medical Journal database (BMJ)
2.3. BMJ and International Guidelines Search Method
2.4. Search Strategy
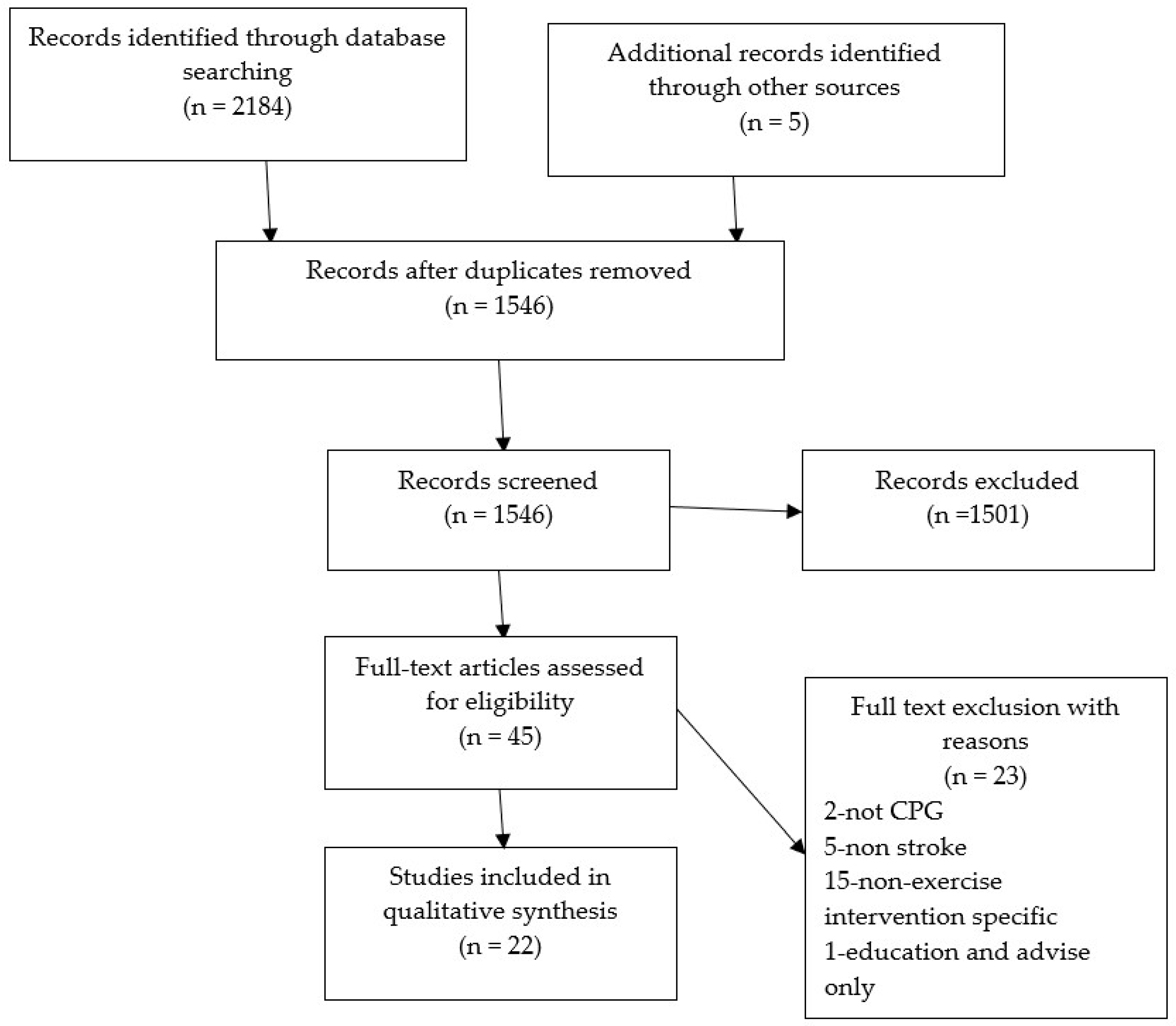
2.5. Screening and Selection Process
2.5.1. Quality Assessment
2.5.2. Data Extraction Method
2.5.3. Analysis and Synthesis
3. Results
4. Discussion
5. Conclusions
- Collectively well-known CPGs from the Global North are rigorous in their development, but only provide basic guidance on exercise in PwS.
- Specific information on exercise interventions is limited and requires clinicians to use their own experiences or knowledge, or to be aware of where to look for further guidance.
- The role of exercise in health is overwhelmingly strong, but proper implementation, reflection and evaluation of these services is imperative for long-term success and commissioning.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Stroke Association. Stroke Statistics Dashboard. 2019. Available online: https://www.stroke.org.uk/what-is-stroke/stroke-statistics (accessed on 21 September 2020).
- Wafa, H.A.; Wolfe, C.D.; Emmett, E.; Roth, G.A.; Johnson, C.O.; Wang, Y. Burden of stroke in Europe: Thirty-year projections of incidence, prevalence, deaths, and disability-adjusted life years. Stroke 2020, 51, 2418–2427. [Google Scholar] [CrossRef] [PubMed]
- Bradshaw, M. Clinical Practice Guidelines. In Evidence-Based Practice in Nursing: Foundations, Skills, and Roles; Springer Publishing Company: Berlin/Heidelberg, Germany, 2017; Chapter 9. [Google Scholar]
- Public Health England. Health Matters: Getting Every Adult Active Every Day. Resources to Help Increase Population Physical Activity and Highlighting the Associated Benefits. 2016. Available online: https://www.gov.uk/government/publications/health-matters-getting-every-adult-active-every-day/health-matters-getting-every-adult-active-every-day (accessed on 21 September 2020).
- World Health Organisation. Physical Activity Fact Sheet. 2020. Available online: https://www.who.int/news-room/fact-sheets/detail/physical-activity (accessed on 21 September 2020).
- European Commission. Special Eurobarometer 472 Report. 2018. Available online: https://www.ehfa-membership.com/sites/europeactive-euaffairs.eu/files/programme/New%20Eurobarometer%20on%20sport%20and%20physical%20activity.pdf (accessed on 21 September 2020).
- Jensen, J.L.; Marstrand, P.C.D. Motor skill training and strength training are associated with different plastic changes in the central nervous system. J. Appl. Physiol. 2016, 99, 1558–1568. [Google Scholar] [CrossRef] [PubMed]
- Mangine, G.T.; Hoffman, J.R.; Stout, J.R. The effect of training volume and intensity on improvements in muscular strength and size in resistance-trained men. Physiol. Rep. 2015, 3, e12472. [Google Scholar] [CrossRef] [PubMed]
- Saunders, D.H.; Greig, C.A.; Mead, G.E. Physical activity and exercise after stroke: Review of multiple meaningful benefits. Stroke-Am. Heart Assoc. 2014, 45, 3742–3747. [Google Scholar] [CrossRef]
- National Clinical Guideline for Stroke, 5th ed.; Royal College of Physicians (RCP): London, UK, 2016; Available online: https://www.rcplondon.ac.uk/guidelines-policy/stroke-guidelines (accessed on 21 September 2020).
- National Institute for Health and Care Excellence (NICE). Stroke Rehabilitation in Adults: Guidance (CG162). 2013. Available online: https://www.nice.org.uk/guidance/cg162 (accessed on 21 September 2020).
- Mezzani, A.; Hamm, L.F.; Jones, A.M.; McBride, P.E.; Moholdt, T.; Williams, M.A. Aerobic exercise intensity assessment and prescription in cardiac rehabilitation: A joint position statement of the European Association for Cardiovascular Prevention and Rehabilitation, the American Association of Cardiovascular and Pulmonary Rehabilitation and the Canadian Association of Cardiac Rehabilitation. Eur. J. Prev. Cardiol. 2013, 20, 442–467. [Google Scholar] [CrossRef]
- Stroke Association. Exercise and Stroke. 2018. Available online: https://www.stroke.org.uk/sites/default/files/exercise_and_stroke.pdf (accessed on 21 September 2020).
- Gordon, N.F.; Gulanick, M.; Costa, F.; Fletcher, G.; Franklin, B.A.; Roth, E.J.; Shephard, T. Physical activity and exercise recommendations for stroke survivors: An American Heart Association scientific statement from the Council on Clinical Cardiology, Subcommittee on Exercise, Cardiac Rehabilitation, and Prevention; the Council on Cardiovascular Nursing; the Council on Nutrition, Physical Activity, and Metabolism; and the Stroke Council. American Heart Association (AHA). Stroke 2004, 109, 2031–2041. [Google Scholar] [CrossRef]
- Best, C.; Wijck, F.V.; Young, S.D.; Dennis, J.; Smith, M.; Mead, G. Best Practice Guidance for the Development of Exercise after Stroke Services in Community Settings. 2010. Available online: https://services.nhslothian.scot/Stroke/community/Documents/BestPracticeGuidance_Exerciseafterstroke_Nov2010.pdf (accessed on 21 September 2020).
- Olney, S.J.; Nymark, J.; Brouwer, B.; Culham, E.; Day, A.; Parvataneni, K. A randomized controlled trial of supervised versus unsupervised exercise programs for ambulatory stroke survivors. Stroke 2006, 37, 476–481. [Google Scholar] [CrossRef]
- Collins, M.; Clifton, E.; Wijck, F.V.; Mead, G.E. Cost-effectiveness of physical fitness training for stroke survivors. J. R. Coll. Physicians Edinb. 2018, 48, 62–68. [Google Scholar] [CrossRef]
- Condon, C.; Lycan, S.; Duncan, P.; Bushnell, C. Reducing Readmissions After Stroke with a Structured Nurse Practitioner/Registered Nurse Transitional Stroke Program. Stroke 2016, 47, 1599–1604. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- University of York. Centre for Reviews and Dissemination. Systematic Reviews: Guidance for Undertaking Reviews in Healthcare. 2017. Available online: https://www.york.ac.uk/media/crd/SystematicReviews.pdf (accessed on 14 October 2020).
- Grant, M.J.; Booth, A. A typology of reviews: An analysis of 14 review types and associated methodologies. Health Inf. Libr. J. 2009, 26, 91–108. [Google Scholar] [CrossRef]
- Booth, A. Unpacking your literature search toolbox: On search styles and tactics. Health Inf. Libr. J. 2008, 25, 3137. [Google Scholar] [CrossRef] [PubMed]
- Zeng, X.I.; Zhang, Y.; Kwong, J.S.; Zhang, C.; Li, S.; Sun, F.; Du, L. The methodological quality assessment tools for preclinical and clinical studies, systematic review and meta-analysis, and clinical practice guideline: A systematic review. J. Evid. Based Med. 2015, 8, 2–10. [Google Scholar] [CrossRef] [PubMed]
- Slade, S.C.; Clermont, E.D.; Underwood, M.; Buchbinder, R.; Beck, B.; White, C. Consensus on Exercise Reporting Template (CERT): Modified Delphi Study. Phys. Ther. 2016, 96, 1514–1524. [Google Scholar] [CrossRef]
- Slade, S.C.; Finnegan, S.; Dionne, C.E.; Underwood, M.; Buchbinder, R. The Consensus on Exercise Reporting Template (CERT) applied to exercise interventions in musculoskeletal trials demonstrated good rater agreement and incomplete reporting. J. Clin. Epidemiol. 2018, 103, 120–130. [Google Scholar] [CrossRef] [PubMed]
- Winstein, C.J.; Stein, J.; Arena, R.; Bates, B.; Cherney, L.R.; Cramer, S.C.; Zorowitz, R.D. Guidelines for adult stroke rehabilitation and recovery: A guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 2016, 47, e98–e169. [Google Scholar] [CrossRef]
- Kernan, W.N.; Ovbiagele, B.; Black, H.R.; Bravata, D.M.; Chimowitz, M.I.; Ezekowitz, M.D.; Wilson, J.A. Guidelines for the prevention of stroke in patients with stroke and transient ischemic attack: A guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 2014, 45, 2160–2236. [Google Scholar] [CrossRef]
- Sall, J.; Eapen, B.C.; Tran, J.E.; Bowles, A.O.; Bursaw, A.; Rodgers, M.E. The management of stroke rehabilitation: A synopsis of the 2019 US Department of Veterans Affairs and US Department of Defense clinical practice guideline. Ann. Intern. Med. 2019, 171, 916–924. [Google Scholar] [CrossRef]
- Goldstein, L.B.; Adams, R.; Alberts, M.J.; Appel, L.J.; Brass, L.M.; Bushnell, C.D.; Sacco, R.L. Primary prevention of ischemic stroke: A guideline from the American heart association/American stroke association stroke council: Cosponsored by the atherosclerotic peripheral vascular disease interdisciplinary working group; cardiovascular nursing council; clinical cardiology council; nutrition, physical activity, and metabolism council; and the quality of care and outcomes research interdisciplinary working group: The American academy of neurology affirms the value of this guideline. Stroke 2006, 37, 1583–1633. [Google Scholar]
- Registered Nurses’ Association of Ontario. Stroke Assessment across the Continuum of Care. 2005. Available online: https://rnao.ca/bpg/guidelines/stroke-assessment-across-continuum-care (accessed on 21 September 2020).
- Kraus, W.E.; Bittner, V.; Appel, L.; Blair, S.N.; Church, T.; Després, J.P.; Whitsel, L. The National Physical Activity Plan: A call to action from the American Heart Association: A science advisory from the American Heart Association. Circulation 2015, 131, 1932–1940. [Google Scholar] [CrossRef]
- National Institute for Health and Clinical Excellence Stroke and TIA: Clinical Knowledge Summaries. 2017. Available online: https://cks.nice.org.uk/topics/stroke-tia (accessed on 21 September 2020).
- National Institute for Health and Clinical Excellence Stroke and Transient Ischaemic Attack in over 16s: Diagnosis and Initial Management—Clinical Guidelines. 2019. Available online: https://cks.nice.org.uk/topics/stroke-tia/over-16 (accessed on 21 September 2020).
- National Institute for Health and Care Excellence. The Physical Activity: Exercise Referral Schemes: Guidance (PH54). 2014. Available online: https://www.nice.org.uk/guidance/ph54/resources/physical-activity-exercise-referral-schemes-pdf-1996418406085 (accessed on 21 September 2020).
- Aerobic Exercise after Stroke. Canadian Partnership for Stroke Recovery. 2013. Available online: CPSR_Guide_Patients-English_WEB3.pdf (accessed on 21 September 2020).
- Post Stroke Community Based Exercise Guidelines: A Resource for Community Based Exercise Providers. Developed by the Post Stroke Community Based Exercise Guidelines Working Group of the Ontario Stroke Network. 2015. Available online: https://www.strokenetworkseo.ca/sites/strokenetworkseo.ca/files/osn-post-stroke-community-based-exercise-guidelines-2016-final.pdf (accessed on 21 September 2020).
- Wein, T.; Lindsay, M.P.; Cote, R.; Foley, N.; Berlingieri, J.; Bhogal, S.; Gladstone, D.J. Canadian stroke best practice recommendations: Secondary prevention of stroke, practice guidelines. Int. J. Stroke 2018, 13, 420–443. [Google Scholar] [CrossRef] [PubMed]
- Quinn, T.J.; Paolucci, S.; Sunnerhagen, K.S.; Sivenius, J.; Walker, M.F.; Toni, D.; Lees, K.R. Evidence-based stroke rehabilitation: An expanded guidance document from the European Stroke Organisation (ESO) guidelines for management of ischaemic stroke and transient ischaemic attack. J. Rehabil. Med. 2009, 41, 99–111. [Google Scholar] [CrossRef] [PubMed]
- Ministry of Health, Social Policy and Equality. Clinical Practice Guideline for the Management of Stroke Patients in Primary Health Care. 2009. (GuiaSalud-Spanish) Guidelines. Available online: https://portal.guiasalud.es/wp-content/uploads/2019/01/GPC_466_Ictus_AP_Lain_Entr_compl_en.pdf (accessed on 21 September 2020).
- Lywodraeth Cmyru-Welsh Government. Stroke Delivery Plan: 2017 to 2020. 2020. Available online: https://gov.wales/sites/default/files/publications/2018-12/stroke-delivery-plan-2017-to-2020.pdf (accessed on 21 September 2020).
- Stroke Council of the Malaysian Society of Neurosciences. Clinical Practice Guidelines—Management of Ischemic Stroke, 2nd ed.; 2012. Available online: https://www.moh.gov.my/moh/resources/Penerbitan/CPG/CARDIOVASCULAR/10a.pdf (accessed on 21 September 2020).
- Royal Dutch Society for Physical Therapy (Koninklijk Nederlands Genootschap voor Fysiotherapie, KNGF). KNGF Clinical Practice Guideline for Physical Therapy in Patients with Stroke. 2014. Available online: https://www.dsnr.nl/wp-content/uploads/2012/03/stroke_practice_guidelines_2014.pdf (accessed on 21 September 2020).
- Australian Stroke Foundation. Clinical Guidelines for Stroke Management (Living Stroke Guidelines). 2020. Available online: https://informme.org.au/en/Guidelines/Clinical-Guidelines-for-Stroke-Management (accessed on 21 September 2020).
- Bender, M. High burden of stroke risk factors in developing countries: The case study of Bosnia-Herzegovina. Mater. Socio-Med. 2017, 29, 277. [Google Scholar] [CrossRef] [PubMed]
- Poungvarin, N. Stroke in the developing world. Lancet 1998, 352, S19–S22. [Google Scholar] [CrossRef]
- Norris, M.; Kilbride, C.; Mohagheghi, A.; Victor, C.; Jones, T.; Dean, C. Exercise instructor led functional training programme for community dwelling stroke survivors: A qualitative study. Int. J. Ther. Rehabil. 2013, 20, 597–605. [Google Scholar] [CrossRef][Green Version]
- Poltawski, L.; Boddy, K.; Forster, A.; Goodwin, V.A.; Pavey, A.C.; Dean, S. Motivators for uptake and maintenance of exercise: Perceptions of long-term stroke survivors and implications for design of exercise programmes. Disabil. Rehabil. 2014, 37, 795–801. [Google Scholar] [CrossRef]
- Simpson, L.A.; Eng, J.J.; Tawashy, A.E. Exercise perceptions among people with stroke: Barriers and facilitators to participation. Int. J. Ther. Rehabil. 2013, 18, 9. [Google Scholar] [CrossRef]
- Lorenz, D.S.; Reiman, M.P.; Walker, J.C. Periodization: Current review and suggested implementation for athletic rehabilitation. Sports Health 2010, 2, 509–518. [Google Scholar] [CrossRef]
- Billinger, S.A.; Boyne, P.; Coughenour, E. Does aerobic exercise and the FITT principle fit into stroke recovery? Curr. Neurol. Neurosci. Rep. 2015, 15, 519. [Google Scholar] [CrossRef]
- Salter, K.; Campbell, N.; Richardson, M.; Mehta, S.; Jutai, J.; Teasell, R. Outcome Measures in Stroke Rehabilitation. Evid.-Based Rev. Stroke Rehabil. 2005, 27, 191–207. [Google Scholar]
- NHS England. Patient Activation Measure (PAM). 2018. Available online: https://www.england.nhs.uk/wp-content/uploads/2018/04/patient-activation-measure-quick-guide.pdf (accessed on 21 September 2020).
- Jones, F.; Riazi, A. Self-efficacy and self-management after stroke: A systematic review. Disabil. Rehabil. 2011, 33, 797–810. [Google Scholar] [CrossRef] [PubMed]
- McGregor, G.; Nichols, S.; Hamborg, T.; Bryning, L.; Tudor-Edwards, R.; Markland, D.; Backx, K. High-intensity interval training versus moderate-intensity steady-state training in UK cardiac rehabilitation programmes (HIIT or MISS UK): Study protocol for a multicentre randomised controlled trial and economic evaluation. BMJ Open 2016, 6, e012843. [Google Scholar] [CrossRef] [PubMed]
- Boss, H.M.; Van Schaik, S.M.; Deijle, I.A.; de Melker, E.C.; van den Berg, B.T.; den Berg-Vos, V. Safety and feasibility of post-stroke care and exercise after minor ischemic stroke or transient ischemic attack: MotiveS & MoveIT. NeuroRehabilitation 2014, 34, 401–407. [Google Scholar] [PubMed]
| Exclusion Code | Category | Inclusion |
|---|---|---|
| 1 | Paper type | Clinical Practice Guidance including national and local/institution guidelines |
| 2 | Age of participants | 18 years or older |
| 3 | Clinical group | Stroke |
| 4 | Intervention type | Exercise and exercise and rehabilitation |
| 5 | Intervention | Intervention |
| 6 | Language | English |
| 7 | No clear evidence from summary or abstract |
| Ref no | Guideline Name | Date | Publisher |
|---|---|---|---|
| Guidelines for Health | |||
| [31] | The National Physical Activity Plan: A Call to Action from the American Heart Association | 2015 | American Heart Association |
| [28] | Management of Stroke Rehabilitation | 2019 | VA/DoD Clinical Practice Guidelines |
| Guidelines for Prevention | |||
| [38] | Guidelines for management of ischaemic stroke and transient ischaemic attack 2008 | 2008 | European Stroke Organisation |
| [27] | Guidelines for the Prevention of Stroke in Patients with Stroke and Transient Ischemic Attack (Secondary Stroke Prevention) | 2014 | American Heart Association |
| [37] | Canadian stroke best practice recommendations: secondary prevention of stroke, sixth edition practice guidelines | 2018 | CPG Infobase |
| Guidelines for Health and Prevention | |||
| [14] | Physical activity and exercise recommendations for stroke survivors: an American Heart Association scientific statement from the Council on Clinical Cardiology | 2004 | American Heart Association |
| [30] | Stroke Assessment Across the Continuum of Care | 2005 | Registered Nurses’ Association of Ontario |
| [29] | Primary prevention of ischemic stroke: a guideline from the American Heart Association/American Stroke Association Stroke Council | 2006 | American Heart Association |
| [39] | CPG for the Management of Stroke Patients in Primary Health Care | 2009 | GuiaSalud-Spanish guidelines |
| [41] | Clinical Practice Guidelines—Management of Ischemic Stroke 2nd edition. | 2012 | Stroke Council of the Malaysian Society of Neurosciences |
| [35] | Aerobic exercise after stroke | 2013 | Canadian Partnership for Stroke Recovery |
| [34] | Physical activity: exercise referral schemes: guidance (PH54) | 2014 | National Institute for Health and Care Excellence—NICE |
| [32] | Stroke and TIA | 2017 | NICE Clinical Knowledge Summaries |
| [40] | Stroke delivery plan: 2017 to 2020 | 2017 | Welsh Government |
| [33] | Stroke and transient ischaemic attack in over 16s: diagnosis and initial management | 2019 | National Institute for Health and Clinical Excellence—Clinical Guidelines |
| Guidelines for Health, Prevention and Rehabilitation | |||
| [15] | Best Practice Guidance for the Development of Exercise after Stroke Service in Community Settings | 2010 | University of Edinburgh |
| [11] | Stroke rehabilitation in adults: guidance (CG162) | 2013 | National Institute for Health and Care Excellence—NICE |
| [42] | KNGF Clinical Practice Guideline for Physical Therapy in patients with stroke | 2014 | Royal Dutch Society for Physical Therapy (Koninklijk Nederlands Genootschap voor Fysiotherapie, KNGF) |
| [36] | Post Stroke Community Based Exercise Guidelines: A resource for community based exercise providers. | 2015 | Post Stroke Community Based Exercise Guidelines Working Group of the Ontario Stroke Network |
| [26] | AHA/ASA Guidelines for Adult Stroke Rehabilitation and Recovery | 2016 | American Heart Association |
| [10] | National clinical guideline for stroke: 5th edition | 2016 | Royal College of Physicians (RCP) |
| [43] | Clinical Guidelines for Stroke Management (Living Stroke Guidelines) | 2020 | Australian Stroke Foundation |
| Guideline | Publisher | Scope and Purpose | Stake Holder Involvement | Rigour of Development | Clarity of Presentation | Applicability | Editorial Independence | |||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | 18 | 19 | 20 | 21 | 22 | 23 | ||
| Aerobic exercise after stroke | Canadian Partnership for Stroke Recovery | 6 | 5 | 5 | 5 | 3 | 6 | 5 | 5 | 5 | 5 | 5 | 5 | 7 | 1 | 5 | 5 | 7 | 5 | 5 | 1 | 1 | 1 | 1 |
| AHA/ASA Guidelines for Adult Stroke Rehabilitation and Recovery | American Heart Association | 7 | 7 | 6 | 6 | 6 | 7 | 3 | 5 | 5 | 6 | 3 | 6 | 5 | 1 | 6 | 6 | 7 | 1 | 2 | 1 | 2 | 6 | 6 |
| Best Practice Guidance for the Development of Exercise after Stroke Services in Community Settings | University of Edinburgh | 7 | 7 | 7 | 6 | 1 | 7 | 4 | 5 | 4 | 5 | 7 | 6 | 1 | 6 | 5 | 5 | 7 | 5 | 7 | 1 | 5 | 6 | 6 |
| Canadian stroke best practice recommendations: secondary prevention of stroke, sixth edition practice guidelines | 7 | 7 | 7 | 7 | 7 | 6 | 7 | 7 | 7 | 7 | 6 | 7 | 7 | 6 | 7 | 7 | 7 | 2 | 1 | 1 | 2 | 7 | 7 | |
| Clinical Guidelines for Stroke Management (Living Guidelines) | Australian Stroke Foundation | 7 | 7 | 7 | 6 | 1 | 7 | 7 | 7 | 7 | 7 | 6 | 7 | 7 | 7 | 6 | 7 | 7 | 7 | 5 | 5 | 6 | 7 | 7 |
| Clinical Practice Guidelines, Management of Ischemic Stroke, 2nd edition 2012. | Malaysian society of Neurosciences, Academy of medicine Malaysia, Ministry of Health malaysia) | 6 | 6 | 7 | 2 | 1 | 7 | 1 | 5 | 7 | 6 | 5 | 5 | 7 | 7 | 6 | 6 | 6 | 6 | 2 | 2 | 6 | 1 | 1 |
| CPG for the Management of Stroke Patients in Primary Health Care | GuiaSalud-Spanish guidelines | 7 | 7 | 6 | 6 | 6 | 6 | 6 | 6 | 6 | 6 | 5 | 6 | 6 | 5 | 6 | 6 | 7 | 1 | 6 | 0 | 0 | 6 | 6 |
| Guidelines for management of ischemic stroke and transient ischemic attack 2008 | European Stroke Organisation | 6 | 6 | 5 | 5 | 1 | 1 | 1 | 1 | 1 | 4 | 5 | 5 | 1 | 1 | 6 | 6 | 6 | 1 | 1 | 1 | 1 | 1 | 1 |
| Guidelines for the Prevention of Stroke in Patients with Stroke and Transient Ischemic Attack (Secondary Stroke Prevention) | American Heart Association | 7 | 7 | 6 | 6 | 1 | 7 | 5 | 6 | 5 | 6 | 5 | 6 | 6 | 1 | 6 | 6 | 7 | 6 | 2 | 6 | 2 | 6 | 6 |
| KNGF Clinical Practice Guideline for Physical Therapy in patients with stroke | Royal Dutch Society for Physical Therapy | 7 | 7 | 7 | 7 | 6 | 7 | 7 | 7 | 7 | 7 | 7 | 7 | 7 | 7 | 7 | 7 | 7 | 7 | 7 | 7 | 7 | 6 | 6 |
| Management of Stroke Rehabilitation—VA/DoD Clinical Practice Guidelines | US Department of Veterans Affairs | 6 | 6 | 6 | 6 | 6 | 6 | 5 | 6 | 6 | 6 | 6 | 7 | 6 | 6 | 6 | 6 | 7 | 6 | 5 | 5 | 1 | 7 | 7 |
| National clinical guideline for stroke: 5th edition | Royal College of Physicians | 6 | 6 | 6 | 6 | 6 | 6 | 5 | 6 | 6 | 6 | 6 | 7 | 6 | 6 | 6 | 6 | 7 | 6 | 5 | 5 | 1 | 7 | 7 |
| Physical activity and exercise recommendations for stroke survivors: an American Heart Association scientific statement from the Council on Clinical Cardiology | American Heart Association | 6 | 6 | 7 | 3 | 1 | 1 | 1 | 1 | 1 | 1 | 5 | 5 | 1 | 1 | 6 | 1 | 7 | 1 | 1 | 1 | 1 | 1 | 1 |
| Physical activity: exercise referral schemes: guidance (PH54) | National Institute for Health and Care Excellence | 7 | 7 | 6 | 7 | 7 | 7 | 7 | 7 | 7 | 7 | 6 | 6 | 7 | 6 | 6 | 5 | 7 | 7 | 7 | 7 | 6 | 7 | 7 |
| Post Stroke Community Based Exercise Guidelines A Resource for Community Based Exercise Providers | Ontario Stroke Network | 7 | 6 | 6 | 6 | 6 | 7 | 5 | 2 | 1 | 1 | 5 | 6 | 7 | 5 | 6 | 6 | 6 | 2 | 5 | 1 | 2 | 6 | 6 |
| Primary prevention of ischemic stroke: a guideline from the American Heart Association/American Stroke Association Stroke Council | American Heart Association | 7 | 7 | 7 | 7 | 1 | 6 | 6 | 6 | 6 | 6 | 7 | 7 | 7 | 1 | 7 | 7 | 7 | 4 | 1 | 1 | 6 | 7 | 7 |
| Stroke and TIA Clinical Knowledge Summaries | National insitiute for Health and Clinical Excellence | 7 | 7 | 7 | 7 | 7 | 7 | 7 | 7 | 7 | 7 | 6 | 7 | 7 | 7 | 7 | 7 | 7 | 1 | 3 | 3 | 7 | 7 | 7 |
| Stroke and transient ischemic attack in over 16s: diagnosis and initial management | National Institute for Health and Clinical Excellence | 7 | 7 | 7 | 7 | 7 | 7 | 7 | 7 | 7 | 7 | 6 | 7 | 7 | 7 | 7 | 7 | 7 | 1 | 6 | 4 | 7 | 7 | 7 |
| Stroke Assessment Across the Continuum of Care | Registered Nurses’ Association of Ontario | 7 | 7 | 7 | 5 | 6 | 7 | 3 | 1 | 5 | 1 | 1 | 6 | 6 | 7 | 7 | 6 | 6 | 6 | 6 | 1 | 6 | 5 | 5 |
| Stroke delivery plan 2017 to 2020 | Welsh Government | 7 | 7 | 7 | 7 | 1 | 7 | 1 | 1 | 1 | 1 | 5 | 1 | 7 | 6 | 7 | 6 | 5 | 1 | 6 | 4 | 5 | 4 | 4 |
| Stroke rehabilitation in adults: guidance (CG162) | National Institute for Health and Care Excellence | 7 | 7 | 7 | 7 | 7 | 7 | 7 | 7 | 7 | 7 | 6 | 7 | 7 | 7 | 7 | 7 | 7 | 1 | 6 | 4 | 7 | 7 | 7 |
| The National Physical Activity Plan: A Call to Action from the American Heart Association | American Heart Association | 6 | 6 | 5 | 7 | 1 | 6 | 1 | 1 | 1 | 5 | 5 | 6 | 7 | 1 | 5 | 5 | 6 | 1 | 1 | 1 | 1 | 7 | 7 |
| Guideline | Publisher | Domains from CERT | |||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| What: Materials | Who: Provider | Where: Location | When, How Much: Dosage | Tailoring: What, How | How Well, Planned, Actual | Pre Checks | During Checks | Post Checks | |||||||||||||||
| 1 | 2 | 3 | 4 | 5 | 6 | 7a | 7b | 8 | 9 | 10 | 11 | 12 | 13 | 14a | 14b | 15 | 16a | 16b | |||||
| Aerobic exercise after stroke | Canadian Partnership for Stroke Recovery | 1 | 0.5 | 0.5 | 0.5 | 0.5 | 0.5 | 0.5 | 0.5 | 0 | 0.5 | 0.5 | 0 | 0.5 | 0.5 | 0.5 | 0.5 | 0.5 | 0 | 0 | 0.5 | 0 | 0 |
| AHA/ASA Guidelines for Adult Stroke Rehabilitation and Recovery | American Heart Association | 0.5 | 0 | 0.5 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0.5 | 0.5 | 0.5 | 0 | 0 | 0 | 0 | 0 | 0 |
| Best Practice Guidance for the Development of Exercise after Stroke Service in Community Settings | University of Edinburgh | 1 | 1 | 1 | 0.5 | 0.5 | 0.5 | 0.5 | 0.5 | 0.5 | 0.5 | 0.5 | 1 | 0.5 | 1 | 1 | 1 | 1 | 0.5 | 0 | 0.5 | 0.5 | 0.5 |
| Canadian stroke best practice recommendations: secondary prevention of stroke, sixth edition practice guidelines | CPG Infobase | 0.5 | 0.5 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0.5 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Clinical Guidelines for Stroke Management (Living Guidelines) | Australian Stroke Foundation | 0.5 | 0 | 0.5 | 0.5 | 0 | 0 | 0 | 1 | 0.5 | 0.5 | 0.5 | 0.5 | 1 | 0.5 | 0.5 | 0.5 | 0 | 0 | 0.5 | 1 | 0 | 1 |
| Clinical Practice Guidelines, Management of Ischemic Stroke, 2nd edition 2012. | Malaysian society of Neurosciences, Academy of medicine Malaysia, Ministry of Health malaysia) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| CPG for the Management of Stroke Patients in Primary Health Care | GuiaSalud- Spanish guidelines | 0.5 | 0 | 0.5 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0.5 | 0 | 0.5 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Guidelines for management of ischemic stroke and transient ischemic attack 2008 | European Stroke Organisation | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0.5 | 0 | 0 | 0 | 0 | 0 | 0 | 0.5 | 0.5 | 0 | 0 | 0 | 0 | 0 | 0 |
| Guidelines for the Prevention of Stroke in Patients with Stroke and Transient Ischemic Attack (Secondary Stroke Prevention) | American Heart Association | 0.5 | 0.5 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0.5 | 0.5 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| KNGF Clinical Practice Guideline for Physical Therapy in patients with stroke | Royal Dutch Society for Physical Therapy | 1 | 0.5 | 0.5 | 1 | 0.5 | 0 | 1 | 1 | 0 | 0.5 | 1 | 0.5 | 1 | 0.5 | 1 | 1 | 0.5 | 0.5 | 0.5 | 1 | 0 | 1 |
| Management of Stroke Rehabilitation- VA/DoD Clinical Practice Guidelines | U.S Department of Vetrans Affairs | 0.5 | 0 | 0.5 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0.5 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| National clinical guideline for stroke: 5th edition | Royal College of Physicians | 0.5 | 0.5 | 0.5 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0.5 | 0 | 0 | 0 | 0.5 | 0.5 | 0.5 | 0 | 0 | 0 | 0 | 0 |
| Physical activity and exercise recommendations for stroke survivors: an American Heart Association scientific statement from the Council on Clinical Cardiology | American Heart Association | 1 | 0 | 0.5 | 0.5 | 1 | 0.5 | 1 | 1 | 0 | 0 | 0 | 0.5 | 0.5 | 1 | 1 | 1 | 0.5 | 0 | 0 | 0 | 0 | 0 |
| Physical activity: exercise referral schemes: guidance (PH54) | National Institute for Health and Care Excellence | 1 | 0 | 0.5 | 0 | 0.5 | 0.5 | 0 | 0.5 | 0 | 0.5 | 0.5 | 0 | 0.5 | 0.5 | 0.5 | 0 | 0 | 0.5 | 0 | 0 | 0 | 0 |
| Post Stroke Community BasedExercise Guidelines. A Resource for Community Based Exercise Providers | Ontario Stroke Network | 1 | 1 | 0.5 | 0.5 | 0.5 | 0 | 0.5 | 0.5 | 0.5 | 0.5 | 0.5 | 0.5 | 0.5 | 0.5 | 1 | 1 | 0.5 | 0.5 | 0 | 0 | 0 | 0 |
| Primary prevention of ischemic stroke: a guideline from the American Heart Association/American Stroke Association Stroke Council | American Heart Association | 0.5 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0.5 | 0 | 0 | 0.5 | 0.5 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Stroke and TIA—Clinical Knowledge Summaries | National Institute for Health and Clinical Excellence | 0.5 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0.5 | 0 | 0 | 0 | 0.5 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Stroke and transient ischemic attack in over 16s: diagnosis and initial management—Clinical Guidelines | National Institute for Health and Clinical Excellence | 0 | 0 | 0 | 0.5 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0.5 | 0.5 | 0.5 | 0 | 0 | 0 | 0 | 0 | 0 |
| Stroke Assessment Across the Continuum of Care | Registered Nurses’ Association of Ontario | 0.5 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0.5 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Stroke delivery plan 2017 to 2020 | Welsh Government | 0.5 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0.5 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Stroke rehabilitation in adults: guidance (CG162) | National Institute for Health and Care Excellence | 1 | 0.5 | 0 | 0 | 0 | 0 | 0.5 | 0.5 | 0 | 0 | 0 | 0 | 0 | 0.5 | 0.5 | 0.5 | 0 | 0 | 0 | 0 | 0 | 0 |
| The National Physical Activity Plan: A Call to Action from the American Heart Association | American Heart Association | 0.5 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0.5 | 0.5 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Church, G.; Ali, A.; Smith, C.L.; Broom, D.; Sage, K. Examining Clinical Practice Guidelines for Exercise and Physical Activity as Part of Rehabilitation for People with Stroke: A Systematic Review. Int. J. Environ. Res. Public Health 2022, 19, 1707. https://doi.org/10.3390/ijerph19031707
Church G, Ali A, Smith CL, Broom D, Sage K. Examining Clinical Practice Guidelines for Exercise and Physical Activity as Part of Rehabilitation for People with Stroke: A Systematic Review. International Journal of Environmental Research and Public Health. 2022; 19(3):1707. https://doi.org/10.3390/ijerph19031707
Chicago/Turabian StyleChurch, Gavin, Ali Ali, Christine Leslie Smith, Dave Broom, and Karen Sage. 2022. "Examining Clinical Practice Guidelines for Exercise and Physical Activity as Part of Rehabilitation for People with Stroke: A Systematic Review" International Journal of Environmental Research and Public Health 19, no. 3: 1707. https://doi.org/10.3390/ijerph19031707
APA StyleChurch, G., Ali, A., Smith, C. L., Broom, D., & Sage, K. (2022). Examining Clinical Practice Guidelines for Exercise and Physical Activity as Part of Rehabilitation for People with Stroke: A Systematic Review. International Journal of Environmental Research and Public Health, 19(3), 1707. https://doi.org/10.3390/ijerph19031707






