Population Access to Hospital Emergency Departments: The Spatial Analysis in Public Health Research
Abstract
1. Introduction
2. Literature Review
2.1. Spatial Analysis of Emergency Department Accessibility
2.2. The Access to Health Services—Theoretical Background
3. Materials and Methods
4. Results
4.1. The Hospital Emergency Department Network in Poland
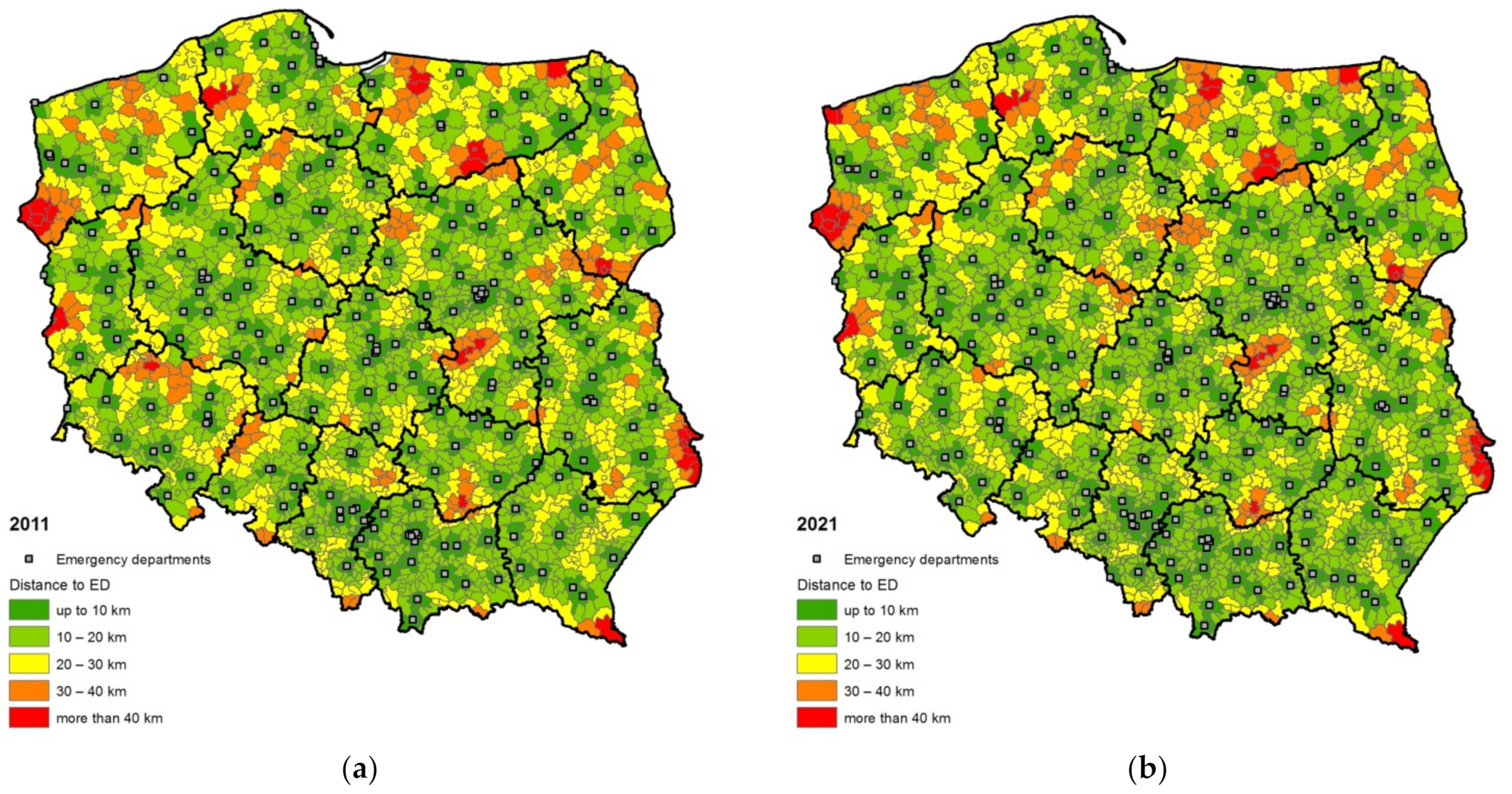
4.2. Spatial Accessibility of Hospital Emergency Departments
5. Discussion
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Sygit, K.M.; Sygit, M.; Wojtyła-Buciora, P.; Lubiniec, O.; Stelmach, W.; Krakowiak, J. Physical activity as an important element in organizing and managing the lifestyle of populations in urban and rural environments. Ann. Agric. Environ. Med. 2019, 26, 8–12. [Google Scholar] [CrossRef] [PubMed]
- Gąska, I.; Sygit, K.; Cipora, E.; Sygit, M.; Pacian, A.; Surmach, M.; Kaleta, D.; Rzeźnicki, A. Assessment of the Health Behaviours and Value-Based Health Analysis of People Aged 50+ Who Were Hospitalized Due to Cardiovascular Disease. Int. J. Environ. Res. Public Health 2021, 18, 4221. [Google Scholar] [CrossRef] [PubMed]
- Take Action for the Sustainable Development Goals. Available online: https://www.un.org/sustainabledevelopment/sustainable-development-goals/ (accessed on 1 December 2021).
- Jones, A.P.; Bentham, G. Emergency medical service accessibility and outcome from road traffic accidents. Public Health 1995, 109, 169–177. [Google Scholar] [CrossRef]
- Richardson, D.B. Increase in patient mortality at 10 days associated with emergency department overcrowding. Med. J. Aust. 2006, 184, 213–216. [Google Scholar] [CrossRef] [PubMed]
- Nicholl, J.; West, J.; Goodacre, S.; Turner, J. The relationship between distance to hospital and patient mortality in emergencies: An observational study. Emerg. Med. J. 2007, 24, 665–668. [Google Scholar] [CrossRef]
- Brown, J.B.; Rosengart, M.R.; Billiar, T.R.; Peitzman, A.B.; Sperry, J.L. Distance matters: Effect of geographic trauma system resource organization on fatal motor vehicle collisions. J. Trauma Acute Care Surg. 2017, 83, 111. [Google Scholar] [CrossRef]
- Jakubaszko, J. Założenia organizacyjne systemu zintegrowanego ratownictwa medycznego. In Ratownik Medyczny; Jakubaszko, J., Ed.; Górnicki Wydawnictwo Medyczne: Wrocław, Poland, 2003. [Google Scholar]
- Leki, K. Pomoc doraźna w świetle ustawy o Państwowym Ratownictwie Medycznym. In Zdrowie i Jego Ochrona: Między Teorią a Praktyką; Korporowicz, V., Ed.; Oficyna Wydawnicza SGH: Warszawa, Poland, 2006; pp. 187–199. [Google Scholar]
- Poździoch, S. (Ed.) Ustawa o Państwowym Ratownictwie Medycznym. Komentarz, 2nd ed.; Wolters Kluwer Business: Warszawa, Poland, 2013. [Google Scholar]
- Szarpak, Ł. Organizacja szpitalnego oddziału ratunkowego. Ogólnopolski Przegląd Med. 2009, 12, 22–26. [Google Scholar]
- Magnusson, G. The role of proximity in the use of hospital emergency departments. Sociol. Health Illn. Cardiff. 1980, 2, 202–214. [Google Scholar] [CrossRef]
- Rudge, G.M.; Mohammed, M.A.; Fillingham, S.C.; Girling, A.; Sidhu, K.; Stevens, A.J. The combined influence of distance and neighborhood deprivation on emergency department attendance in a large English population: A retrospective database study. PLoS ONE 2013, 8, e67943. [Google Scholar] [CrossRef]
- Lee, J.E.; Sung, J.H.; Ward, W.B.; Fos, P.J.; Lee, W.J.; Kim, J.C. Utilization of the emergency room: Impact of geographic distance. Geospat. Health 2007, 1, 243–253. [Google Scholar] [CrossRef]
- Henneman, P.L.; Garb, J.L.; Capraro, G.A.; Li, H.; Smithline, H.A.; Wait, R.B. Geography and travel distance impact emergency department visits. J. Emerg. Med. 2011, 40, 333–339. [Google Scholar] [CrossRef]
- Vaz, S.; Ramos, P.; Santana, P. Distance effects on the accessibility to emergency departments in Portugal. Saúde E Soc. 2014, 23, 1154–1161. [Google Scholar] [CrossRef]
- Mayer, J.D. Seattle’s paramedic program: Geographical distribution, response times, and mortality. Soc. Sci. Med. 1979, 13, 45–51. [Google Scholar] [CrossRef]
- Mayer, J.D. Relations between two traditions of medical geography: Health systems planning and geographical epidemiology. Prog. Hum. Geogr. 1982, 2, 215–230. [Google Scholar] [CrossRef]
- Toregas, C.; Swain, R.; ReVelle, C.; Bergman, L. The Location of Emergency Service Facilities. Oper. Res. 1971, 19, 1363–1373. [Google Scholar] [CrossRef]
- Mayer, J.D. A Method for the Geographical Evaluation of Emergency Medical Service Performance. Public Health 1981, 71, 841–844. [Google Scholar] [CrossRef]
- Halseth, G.; Rosenberg, M.W. Locating Emergency Medical Services in Small Town and Rural Settings. Socio-Econ. Plan. Sci. 1991, 25, 295–304. [Google Scholar] [CrossRef]
- Brotcorne, L.; Laporte, G.; Semet, F. Ambulance location and relocation models. Eur. J. Oper. Res. 2003, 147, 451–463. [Google Scholar] [CrossRef]
- Henderson, S.G.; Mason, A.J. Ambulance Service Planning: Simulation and Data Visualization. In Operations Research and Health Care. A Handbook of Methods and Applications; Brandeau, M.L., Sainfort, F., Pierskalla, W.P., Eds.; Kluwer Academic Publishers: Boston, MA, USA, 2004; pp. 78–102. [Google Scholar]
- Schmid, V.; Doerner, K.F. Ambulance location and relocation problems with time-dependent travel times. Eur. J. Oper. Res. 2010, 207, 1293–1303. [Google Scholar] [CrossRef]
- Fone, L.D.; Christie, S.; Lester, N. Comparison of perceived and modeled geographical access to accident and emergency departments: A cross-sectional analysis from the Caerphilly Health and Social Needs Study. Int. J. Health Geogr. 2006, 5, 16. [Google Scholar] [CrossRef]
- Acton, J.P. Nonmonetary factors in the demand for medical services: Some empirical evidence. J. Political Econ. 1975, 83, 595–614. [Google Scholar] [CrossRef]
- Friedman, J.M.; Hagander, L.; Hughes, C.D.; Nash, K.A.; Linden, A.F.; Blossom, J.; Meara, J.G. Distance to hospital and utilization of surgical services in Haiti: Do children, delivering mothers, and patients with emergent surgical conditions experience greater geographical barriers to surgical care? Int. J. Health Plan. Manag. 2013, 28, 248–256. [Google Scholar] [CrossRef] [PubMed]
- Alegana, V.; Wright, J.A.; Pentrina, U.; Noor, A.M.; Snow, R.W.; Atkinson, P.M. Spatial modelling of health care utilization for treatment of fever in Namibia. Int. J. Health Geogr. 2012, 11, 6. [Google Scholar] [CrossRef] [PubMed]
- Brabyn, L.; Beere, P. Population access to hospital emergency departments and the impact of health reform in New Zealand. Health Inform. J. 2006, 12, 227–237. [Google Scholar] [CrossRef] [PubMed]
- Carr, B.G.; Branas, C.C.; Metlay, J.P.; Sullivan, A.F.; Camargo, C.A. Access to Emergency Care in the United States. Ann. Emerg. Med. 2009, 54, 261–269. [Google Scholar] [CrossRef]
- Hashtarkhani, S.; Kiani, B.; Bergquist, R.; Bagheri, N.; VafaeiNejad, R.; Tara, M. An age-integrated approach to improve measurement of potential spatial accessibility to emergency medical services for urban areas. Int. J. Health Plan. Manag. 2020, 35, 788–798. [Google Scholar] [CrossRef]
- Apornak, A. Human resources allocation in the hospital emergency department during COVID-19 pandemic. Int. J. Healthc. Manag. 2021, 14, 264–270. [Google Scholar] [CrossRef]
- Kumar, S.; Raut, R.D.; Narkhede, B.E. A proposed collaborative framework by using artificial intelligence-internet of things (AI-IoT) in COVID-19 pandemic situation for healthcare workers. Int. J. Health Manag. 2020, 13, 337–345. [Google Scholar] [CrossRef]
- Boserup, B.; McKenney, M.; Elkbuli, A. The impact of the COVID-19 pandemic on emergency department visits and patient safety in the United States. Am. J. Emerg. Med. 2020, 38, 1732–1736. [Google Scholar] [CrossRef]
- Golinelli, D.; Campinoti, F.; Sanmarchi, F.; Rosa, S.; Beleffi, M.; Farina, G.; Tampieri, A.; Pia Fantini, M.; Giostra, F.; Santi, L. Patterns of Emergency Department visits for acute and chronic diseases during the two pandemic waves in Italy. Am. J. Emerg. Med. 2021, 50, 22–26. [Google Scholar] [CrossRef]
- Maćkiewicz, A.; Ratajczak, W. Towards a new definition of topological accessibility. Transp. Res. 1996, 30, 267–284. [Google Scholar] [CrossRef]
- Taylor, Z. Dostępność miejsc pracy, nauki, usług w obszarach wiejskich jako przedmiot badań geografii społeczno-ekonomicznej–próba analizy krytycznej. Przegląd Geogr. 1997, 69, 261–283. [Google Scholar]
- Domański, R. Accessibility, Efficiency, and Spatial Organization. Environ. Plan. A Econol. Space 1979, 11, 1189–1206. [Google Scholar] [CrossRef]
- Vickerman, R.W. Accessibility, attraction, and potential: A review of some concepts and their use in determining mobility. Environ. Plan. A 1974, 6, 675–691. [Google Scholar] [CrossRef]
- Ratajczak, W. Modelowanie Sieci Transportowych; Wydawnictwo Naukowe UAM: Poznań, Poland, 1999. [Google Scholar]
- Gutiérrez, J. Location, economic potential and daily accessibility: An analysis of the accessibility impact of the high-speed line Madrid-Barcelona-French border. J. Transp. Geogr. 2001, 9, 229–242. [Google Scholar] [CrossRef]
- Penchansky, R.; Thomas, J.W. The Concept of Access: Definition and Relationship to Consumer Satisfaction. Med. Care 1981, 19, 127–140. [Google Scholar] [CrossRef]
- Drury, P. Some spatial aspects of health service development: The British experience. Prog. Hum. Geogr. 1983, 7, 60–77. [Google Scholar] [CrossRef]
- Joseph, A.E.; Phillips, D.R. Accessibility and Utilization. Geographical Perspectives on Health Care Delivery; Harper & Row Ltd.: London, UK, 1984. [Google Scholar]
- Kowalczyk, A. Accessibility and availability of health care services in rural areas of Poland: A case study of the Sierpc medical district. Geogr. Med. 1987, 17, 47–61. [Google Scholar]
- Gulliford, M.; Figueroa-Munoz, J.; Morgan, M.; Hughes, D.; Gibson, B.; Beech, R.; Hudson, M. What does ‘access to health care’ mean? J. Health Serv. Res. Policy 2002, 7, 186–188. [Google Scholar] [CrossRef]
- Lerner, E.B.; Moscati, R.M. The Golden Hour: Scientific Fact or Medical “Urban Legend”? Acad. Emerg. Med. 2001, 8, 758–760. [Google Scholar] [CrossRef]
- Malczewski, J. Przestrzenna Organizacja Systemu Placówek Podstawowej Ochrony Zdrowia (na Przykładzie Dzielnicy Warszawa-Wola); PAN IGiPZ: Warszawa, Poland, 1989. [Google Scholar]
- Powęska, H. Dostępność Przestrzenna Usług Medycznych a Zachowania Medyczne Ludności; PAN IGiPZ: Warszawa, Poland, 1990. [Google Scholar]
- Twigg, L. Health based geographical information systems: Their potential examined in the light of existing data sources. Soc. Sci. Med. 1990, 30, 143–155. [Google Scholar] [CrossRef]
- Parker, E.B.; Campbell, J.L. Measuring access to primary medical care: Some examples of the use of geographical information systems. Health Place 1998, 4, 183–193. [Google Scholar] [CrossRef]
- Fortney, J.; Rost, K.; Warren, J. Comparing Alternative Methods of Measuring Geographic Access to Health Services. Health Serv. Outcomes Res. Methodol. 2000, 1, 173–184. [Google Scholar] [CrossRef]
- Brabyn, L.; Skelly, C. Modeling population access to New Zealand public hospitals. Int. J. Health Geogr. 2002, 1, 3. [Google Scholar] [CrossRef] [PubMed]
- Patel, A.B.; Waters, N.M.; Ghali, W.A. Determining geographic areas and populations with timely access to cardiac catheterization facilities for acute myocardial infarction care in Alberta, Canada. Int. J. Health Geogr. 2007, 6, 47. [Google Scholar] [CrossRef] [PubMed]
- Longley, P.A.; Goodchild, M.F.; Maguire, D.J.; Rhind, D.W. Geographic Information Systems and Science; John Wiley & Sons: Toronto, ON, Canada, 2005. [Google Scholar]
- Jones, S.G.; Ashby, A.J.; Momin, S.R.; Naidoo, A. Spatial Implications Associated with Using Euclidean Distance Measurements and Geographic Centroid Imputation in Health Care Research. HSR Health Serv. Res. 2010, 45, 316–327. [Google Scholar] [CrossRef] [PubMed]
- Gaca, M.; Witkowski, A. Realizacja programu medycyny ratunkowej w perspektywie województwa wielkopolskiego. Przew. Lek. 2007, 2, 240–246. [Google Scholar]
- Kostrzewa, D.; Sierocka, A.; Woźniak, B.; Iltchev, P.; Marczak, M. Wpływ zmian finansowania świadczeń w IP/SOR na zarządzanie strategiczne w szpitalu. Mark. Rynek 2015, 9, 253–266. [Google Scholar]
- Hoffmann, K.; Elhag, A.E.; Bryl, W. Globalna eskalacja zapotrzebowania na świadczenia w szpitalnych oddziałach ratunkowych–analiza problemu. Hygeia 2018, 53, 241–246. [Google Scholar]
- W SOR-ach jak w Soczewce Skupiają się Problemy, z Którymi Boryka się System. Available online: https://serwisy.gazetaprawna.pl/zdrowie/artykuly/1408767,problemy-sluzby-zdrowia-sor.html (accessed on 1 December 2021).
- Paplicki, M. Bezpieczeństwo Zdrowotne Obywatela w Polskim Systemie Ratownictwa Medycznego; E-Wydawnictwo, Prawnicza i Ekonomiczna Biblioteka Cyfrowa, Wydział Prawa, Administracji i Ekonomii Uniwersytetu Wrocławskiego: Wrocław, Poland, 2020. [Google Scholar] [CrossRef]
- Mayer, J.D. The distance behaviour of hospital patients: A disaggregated analysis. Soc. Sci. Med. 1983, 17, 819–827. [Google Scholar] [CrossRef]
- Coucelis, H.; Getis, A. A Conceptualising and measuring accessibility within physical and virtual spaces. In Information, Place and Cyberspace: Issues and Accessibility; Janelle, D., Hodge, D., Eds.; Springer: Berlin/Heidelberg, Germany, 2000. [Google Scholar]
- Sánchez-Mangas, R.; García-Ferrrer, A.; De Juan, A.; Arroyo, A.M. The probability of death in road traffic accidents. How important is a quick medical response? Accid. Anal. Prev. 2010, 42, 1048–1056. [Google Scholar] [CrossRef] [PubMed]
- Shen, Y.C.; Hsia, R.Y. Does Decreased Access to Emergency Departments Affect Patient Outcomes? Analysis of Acute Myocardial Infarction Population 1996–2005. Health Serv. Res. 2012, 47, 188–210. [Google Scholar] [CrossRef] [PubMed]
- Nakamura, T.; Okayama, M.; Aihara, M.; Kajii, E. Injury mortality and accessibility to emergency care in Japan: An observational epidemiological study. Open Access Emerg. Med. OAEM 2014, 6, 27–32. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Mościcka, A.; Bielecka, E.; Tomala, J. Mapa dostępności czasowej szpitalnych oddziałów ratunkowych w Warszawie. Logistyka 2014, 5, 1147–1153. [Google Scholar]
- Sitek, K.; Pokojski, W.; Gołębiowska, I. Evaluation of time availability of the selected rescue service of a large city. A case study of Warsaw. Pol. Cartogr. Rev. 2020, 52, 176–186. [Google Scholar] [CrossRef]
- Fleet, R.; Poitras, J.; Archambault, P.; Tounkara, F.K.; Chauny, J.-M.; Ouimet, M.; Gauthier, J.; Dupuis, G.; Tanguay, A.; Levesque, J.-F.; et al. Portrait of rural emergency departments in Québec and utilization of the provincial emergency department management Guide: Cross sectional survey. BMC Health Serv. Res. 2015, 15, 572. [Google Scholar] [CrossRef]
- Poździoch, S.; Guła, P. (Eds.) Ustawa o Państwowym Ratownictwie Medycznym. Komentarz; Wolters Kluwer Polska Sp. zo.o.: Warszawa, Poland, 2008. [Google Scholar]
- Luo, W.; Wang, F. Measures of spatial accessibility to health care in a GIS environment: Synthesis and a case study in the Chicago region. Environ. Plan. B Plan. Des. 2003, 30, 865–884. [Google Scholar] [CrossRef]

| Region | No. of HEDs in 2011 | No. of HEDs in 2021 | ||||
|---|---|---|---|---|---|---|
| Functioning | Planned | Level of Completion | Functioning | Planned | Level of Completion | |
| Dolnośląskie | 13 | 16 | 81% | 16 | 16 | 100% |
| Kujawsko-Pomorskie | 12 | 12 | 100% | 10 | 12 | 83% |
| Lubelskie | 19 | 19 | 100% | 17 | 20 | 85% |
| Lubuskie | 8 | 8 | 100% | 8 | 8 | 100% |
| Łódzkie | 17 | 17 | 100% | 20 | 23 | 87% |
| Małopolskie | 22 | 22 | 100% | 21 | 21 | 100% |
| Mazowieckie | 30 | 32 | 94% | 32 | 35 | 91% |
| Opolskie | 6 | 6 | 100% | 7 | 7 | 100% |
| Podkarpackie | 12 | 14 | 86% | 14 | 15 | 93% |
| Podlaskie | 11 | 12 | 92% | 13 | 15 | 87% |
| Pomorskie | 12 | 13 | 92% | 13 | 14 | 93% |
| Śląskie | 10 | 23 | 43% | 14 | 21 | 67% |
| Świętokrzyskie | 9 | 11 | 82% | 10 | 11 | 91% |
| Warmińsko-Mazurskie | 11 | 12 | 92% | 11 | 12 | 92% |
| Wielkopolskie | 26 | 27 | 96% | 25 | 27 | 93% |
| Zachodniopomorskie | 11 | 12 | 100% | 10 | 10 | 100% |
| POLAND | 229 | 256 | 89% | 241 | 267 | 90% |
| Region | Share of Population Living within a Given Distance from the Nearest HED | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 2011 | 2021 | |||||||||
| Up to 10 km | 10–20 km | 20–30 km | 30–40 km | >40 km | up to 10 km | 10–20 km | 20–30 km | 30–40 km | >40 km | |
| Dolnośląskie | 45.6 | 26.0 | 23.6 | 4.5 | 0.2 | 53.0 | 29.8 | 16.5 | 0.6 | 0.0 |
| Kujawsko-Pomorskie | 53.7 | 25.9 | 17.8 | 2.6 | 0.0 | 50.9 | 24.8 | 20.0 | 4.3 | 0.0 |
| Lubelskie | 51.9 | 24.4 | 18.1 | 3.3 | 2.2 | 51.4 | 23.2 | 20.3 | 3.1 | 2.1 |
| Lubuskie | 47.6 | 22.9 | 23.6 | 3.5 | 2.4 | 48.0 | 24.0 | 22.3 | 3.4 | 2.3 |
| Łódzkie | 60.7 | 26.8 | 11.6 | 0.8 | 0.0 | 60.9 | 28.1 | 10.1 | 0.9 | 0.0 |
| Małopolskie | 60.8 | 33.5 | 5.1 | 0.5 | 0.0 | 60.4 | 33.8 | 5.3 | 0.5 | 0.0 |
| Mazowieckie | 58.9 | 26.4 | 10.0 | 4.3 | 0.3 | 60.5 | 27.8 | 8.0 | 3.5 | 0.3 |
| Opolskie | 33.5 | 32.6 | 23.5 | 10.5 | 0.0 | 39.1 | 35.0 | 24.1 | 1.7 | 0.0 |
| Podkarpackie | 45.1 | 39.1 | 15.6 | 0.1 | 0.1 | 50.2 | 40.8 | 8.8 | 0.1 | 0.1 |
| Podlaskie | 52.8 | 22.1 | 17.1 | 6.3 | 1.8 | 58.7 | 21.0 | 13.4 | 5.2 | 1.7 |
| Pomorskie | 57.6 | 22.0 | 15.4 | 4.0 | 1.1 | 58.2 | 26.0 | 13.2 | 1.6 | 1.0 |
| Śląskie | 50.2 | 35.7 | 13.3 | 0.7 | 0.0 | 60.7 | 30.0 | 9.0 | 0.3 | 0.0 |
| Świętokrzyskie | 50.2 | 30.7 | 12.4 | 6.2 | 0.4 | 49.6 | 31.4 | 13.3 | 5.3 | 0.4 |
| Warmińsko-Mazurskie | 42.8 | 17.5 | 26.3 | 7.8 | 5.7 | 42.0 | 18.8 | 26.0 | 7.6 | 5.7 |
| Wielkopolskie | 52.5 | 31.3 | 14.2 | 2.0 | 0.0 | 51.7 | 32.0 | 13.5 | 2.9 | 0.0 |
| Zachodniopomorskie | 46.1 | 16.7 | 23.6 | 11.5 | 2.1 | 43.4 | 19.3 | 20.5 | 12.1 | 4.8 |
| POLAND | 52.4 | 28.2 | 15.2 | 3.5 | 0.7 | 54.7 | 28.6 | 13.2 | 2.7 | 0.8 |
| Region | 2011 | 2021 |
|---|---|---|
| Dolnośląskie | 13.2 | 10.7 |
| Kujawsko-Pomorskie | 10.6 | 11.6 |
| Lubelskie | 11.9 | 12.4 |
| Lubuskie | 12.6 | 12.5 |
| Łódzkie | 8.0 | 7.9 |
| Małopolskie | 8.5 | 8.9 |
| Mazowieckie | 9.2 | 8.7 |
| Opolskie | 15.4 | 13 |
| Podkarpackie | 11.4 | 10.1 |
| Podlaskie | 11.6 | 10.2 |
| Pomorskie | 10.0 | 9.3 |
| Śląskie | 11.1 | 9.3 |
| Świętokrzyskie | 11.1 | 11.1 |
| Warmińsko-Mazurskie | 15.2 | 15.1 |
| Wielkopolskie | 10.2 | 10.7 |
| Zachodniopomorskie | 15.2 | 16.6 |
| POLAND | 11.0 | 10.4 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kisiała, W.; Rącka, I.; Suszyńska, K. Population Access to Hospital Emergency Departments: The Spatial Analysis in Public Health Research. Int. J. Environ. Res. Public Health 2022, 19, 1437. https://doi.org/10.3390/ijerph19031437
Kisiała W, Rącka I, Suszyńska K. Population Access to Hospital Emergency Departments: The Spatial Analysis in Public Health Research. International Journal of Environmental Research and Public Health. 2022; 19(3):1437. https://doi.org/10.3390/ijerph19031437
Chicago/Turabian StyleKisiała, Wojciech, Izabela Rącka, and Katarzyna Suszyńska. 2022. "Population Access to Hospital Emergency Departments: The Spatial Analysis in Public Health Research" International Journal of Environmental Research and Public Health 19, no. 3: 1437. https://doi.org/10.3390/ijerph19031437
APA StyleKisiała, W., Rącka, I., & Suszyńska, K. (2022). Population Access to Hospital Emergency Departments: The Spatial Analysis in Public Health Research. International Journal of Environmental Research and Public Health, 19(3), 1437. https://doi.org/10.3390/ijerph19031437






