Sleep Duration and Bedtime in the PURE Poland Cohort Study and the Link with Noncommunicable Diseases
Abstract
:1. Introduction
2. Materials and Methods
- (1)
- During your longest or nocturnal sleep period, what time do you normally go to bed?
- (2)
- During your longest or nocturnal sleep period, what time do you normally wake up?
- (3)
- Do you usually take naps/siestas?
3. Results
3.1. Total Sleep Duration
3.2. Naps
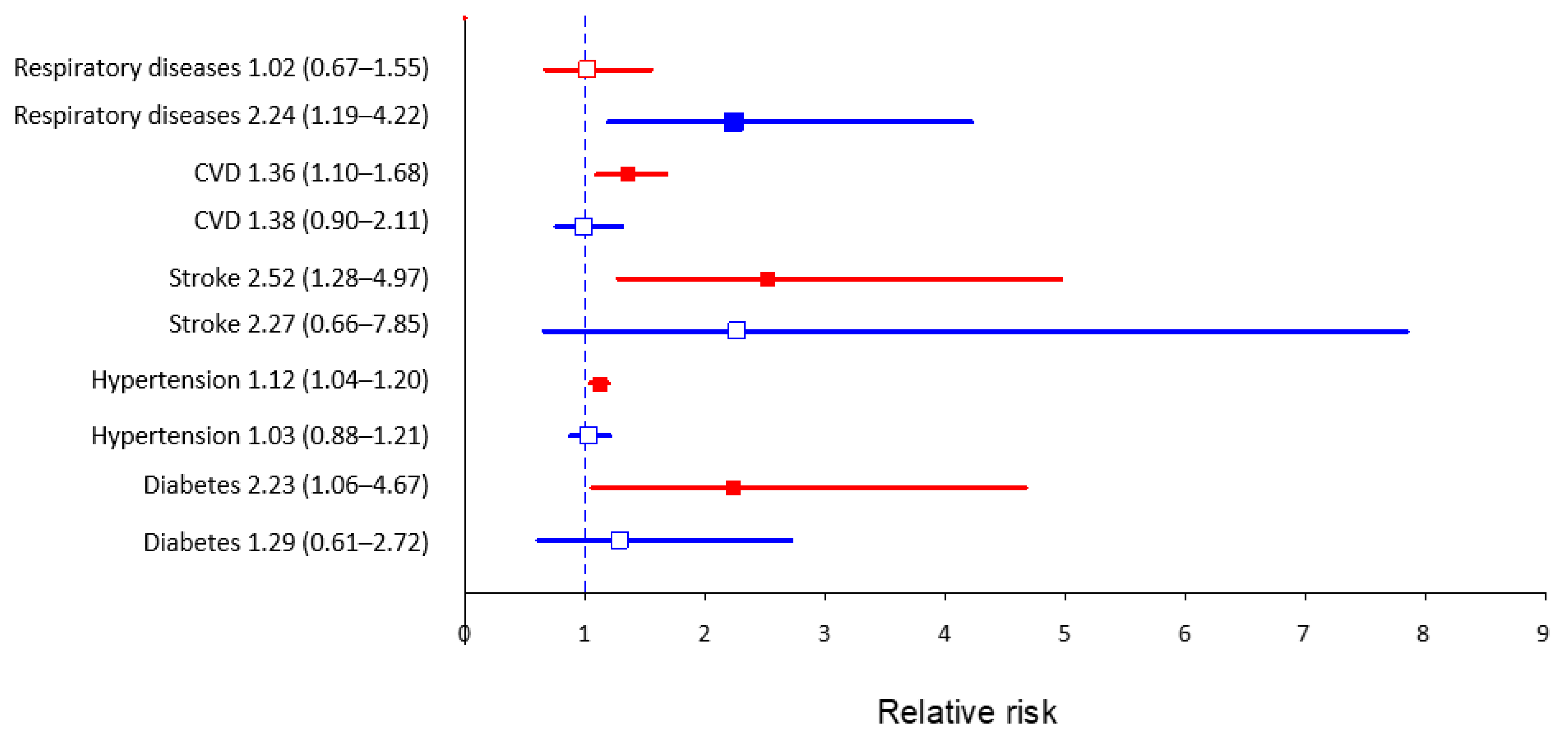
3.3. Total Sleep Duration and Bedtime According to Chosen Non-Communicable Diseases
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Medic, G.; Wille, M.; Hemels, M.E.H. Short- and long-term health consequences of sleep disruption. Nat. Sci. Sleep 2017, 9, 151–161. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Watson, N.F.; Badr, M.S.; Belenky, G.; Bliwise, D.L.; Buxton, O.M.; Buysse, D.; Dinges, D.F.; Gangwisch, J.; Grandner, M.A.; Kushida, C.; et al. Recommended amount of sleep for a healthy adult: A joint consensus statement of the American Academy of Sleep Medicine and Sleep Research Society. J. Clin. Sleep Med. 2015, 11, 591–592. [Google Scholar] [CrossRef] [PubMed]
- Jike, M.; Itani, O.; Watanabe, N.; Buysse, D.J.; Kaneita, Y. Long sleep duration and health outcomes: A systematic review, meta-analysis and meta-regression. Sleep Med. Rev. 2018, 39, 25–36. [Google Scholar]
- Wang, C.; Bangdiwala, S.I.; Rangarajan, S.; Lear, S.A.; AlHabib, K.F.; Mohan, V.; Teo, K.; Poirier, P.; Tse, L.A.; Liu, Z.; et al. Association of estimated sleep duration and naps with mortality and cardiovascular events: A study of 116,632 people from 21 countries. Eur. Heart J. 2019, 40, 1620–1629. [Google Scholar] [CrossRef] [PubMed]
- Itani, O.; Jike, M.; Watanabe, N.; Kaneita, Y. Short sleep duration and health outcomes: A systematic review, meta-analysis, and meta-regression. Sleep Med. 2017, 32, 246–256. [Google Scholar] [CrossRef] [PubMed]
- Yin, J.; Jin, X.; Shan, Z.; Li, S.; Huang, H.; Li, P.; Peng, X.; Peng, Z.; Yu, K.; Bao, W.; et al. Relationship of sleep duration with all-cause mortality and cardiovascular events: A systematic review and dose-response meta-analysis of prospective cohort studies. J. Am. Heart Assoc. 2017, 6, e005947. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chaput, J.P.; McNeil, J.; Després, J.P.; Bouchard, C.; Tremblay, A. Short sleep duration as a risk factor for the development of the metabolic syndrome in adults. Prev. Med. 2013, 57, 872–877. [Google Scholar] [CrossRef]
- Wang, C.; Hu, B.; Rangarajan, S.; Bangdiwala, S.I.; Lear, S.A.; Mohan, V.; Gupta, R.; Alhabib, K.F.; Soman, B.; Abat, M.E.M.; et al. Association of bedtime with mortality and major cardiovascular events: An analysis of 112,198 individuals from 21 countries in the PURE study. Sleep Med. 2021, 80, 265–272. [Google Scholar] [CrossRef] [PubMed]
- Sabia, S.; Fayosse, A.; Dumurgier, J.; van Hees, V.T.; Paquet, C.; Sommerlad, A.; Kivimäki, M.; Dugravot, A.; Singh-Manoux, A. Association of sleep duration in middle and old age with incidence of dementia. Nat. Commun. 2021, 12, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Hertenstein, E.; Gabryelska, A.; Spiegelhalder, K.; Nissen, C.; Johann, A.F.; Umarova, R.; Riemann, D.; Baglioni, C.; Feige, B. Reference Data for Polysomnography-Measured and Subjective Sleep in Healthy Adults. J. Clin. Sleep Med. 2018, 14, 523–532. [Google Scholar] [CrossRef] [PubMed]
- Evans, M.A.; Buysse, D.J.; Marsland, A.L.; Wright, A.G.C.; Foust, J.; Carroll, L.W.; Kohli, N.; Mehra, R.; Jasper, A.; Srinivasan, S.; et al. Meta-analysis of age and actigraphy-assessed sleep characteristics across the lifespan. Sleep 2021, 44, zsab088. [Google Scholar] [CrossRef] [PubMed]
- Knutson, K.L.; Wu, D.; Patel, S.R.; Loredo, J.S.; Redline, S.; Cai, J.; Gallo, L.C.; Mossavar-Rahmani, Y.; Ramos, A.R.; Teng, Y.; et al. Association between sleep timing, obesity, diabetes: The hispanic community health study/study of latinos (hchs/sol) cohort study. Sleep 2017, 40, zsx014. [Google Scholar] [CrossRef]
- Yang, G.; Han, Y.Y.; Sun, T.; Li, L.; Rosser, F.; Forno, E.; Patel, S.R.; Chen, W.; Celedón, J.C. Sleep duration, current asthma, and lung function in a nationwide study of U.S. Adults. Am. J. Respir. Crit. Care Med. 2019, 200, 926–929. [Google Scholar] [CrossRef] [PubMed]
- Lakerveld, J.; Mackenbach, J.D.; Horvath, E.; Rutters, F.; Compernolle, S.; Bárdos, H.; De Bourdeaudhuij, I.; Charreire, H.; Rutter, H.; Oppert, J.M.; et al. The relation between sleep duration and sedentary behaviours in European adults. Obes. Rev. 2016, 17, 62–67. [Google Scholar] [CrossRef] [Green Version]
- Jonasdottir, S.S.; Minor, K.; Lehmann, S. Gender differences in nighttime sleep patterns and variability across the adult lifespan: A global-scale wearables study. Sleep 2021, 44, zsaa169. [Google Scholar] [CrossRef]
- Walch, O.J.; Cochran, A.; Forger, D.B. A global quantification of “normal” sleep schedules using smartphone data. Sci. Adv. 2016, 2, e1501705. [Google Scholar] [CrossRef] [PubMed]
- Boguszewski, R. Zdrowie i Prozdrowotne Zachowania Polaków [Health and Health-RELATED Behavior of Poles]; Centrum Badania Opinii Społecznej: Warszawa, Poland, 2016. [Google Scholar]
- Kiejna, A.; Rymaszewska, J.; Wojtyniak, B.; Stokwiszewski, J. Characteristics of sleep disturbances in Poland-Results of the National Health Interview Survey. Acta Neuropsychiatr. 2004, 16, 124–129. [Google Scholar] [CrossRef]
- Kiejna, A.; Wojtyniak, B.; Rymaszewska, J.; Stokwiszewski, J. Prevalence of insomnia in Poland-Results of the National Health Interview Survey. Acta Neuropsychiatr. 2003, 15, 68–73. [Google Scholar] [CrossRef] [PubMed]
- Nowicki, Z.; Grabowski, K.; Cubała, W.J.; Nowicka-Sauer, K.; Zdrojewski, T.; Rutkowski, M.; Bandosz, P. Prevalence of self-reported insomnia in general population of Poland. Psychiatr. Pol. 2016, 50, 165–173. [Google Scholar] [CrossRef] [PubMed]
- Smyka, M.; Kosińska-Kaczyńska, K.; Sochacki-Wójcicka, N.; Zgliczyńska, M.; Wielgoś, M. Sleep problems in pregnancy—A cross-sectional study in over 7000 pregnant women in Poland. Int. J. Environ. Res. Public Health 2020, 17, 5306. [Google Scholar] [CrossRef] [PubMed]
- Lizończyk, I.; Jośko-Ochojska, J. Relationship between overweight, obesity and sleep disorders in adolescents from selected cities of upper silesia, Poland. Ann. Agric. Environ. Med. 2021, 28, 193–197. [Google Scholar] [CrossRef] [PubMed]
- Teo, K.; Chow, C.K.; Vaz, M.; Rangarajan, S.; Yusuf, S.; PURE Investigators-Writing Group. The Prospective Urban Rural Epidemiology (PURE) study: Examining the impact of societal influences on chronic noncommunicable diseases in low-, middle-, and high-income countries. Am. Heart J. 2009, 158, 1–7.e1. [Google Scholar] [CrossRef] [PubMed]
- Zatońska, K.; Zatoński, W.A.; Szuba, A. Prospective urban and rural epidemiology Poland–study design. J. Health Inequal. 2016, 2, 136–141. [Google Scholar] [CrossRef]
- Polskie Towarzystwo Diabetologiczne. Zalecenia kliniczne dotyczące postępowania u chorych na cukrzycę 2019. Diabetol. Prakt. 2019, 5, 7–10. [Google Scholar]
- Szuba, A.; Martynowicz, H.; Zatońska, K.; Ilow, R.; Regulska-Ilow, B.; Różańska, D.; Wołyniec, M.; Połtyn-Zaradna, K.; Zatoński, W.A. Prevalence of hypertension in Polish population of PURE Poland study. J. Health Inequal. 2017, 2, 157–162. [Google Scholar] [CrossRef] [Green Version]
- Jackson, C.L.; Gaston, S.A.; Liu, R.; Mukamal, K.; Rimm, E.B. The Relationship between Alcohol Drinking Patterns and Sleep Duration among Black and White Men and Women in the United States. Int. J. Environ. Res. Public Health 2018, 15, 557. [Google Scholar] [CrossRef] [Green Version]
- Cappuccio, F.P.; D’Elia, L.; Strazzullo, P.; Miller, M.A. Quantity and quality of sleep and incidence of type 2 diabetes: A systematic review and meta-analysis. Diabetes Care 2010, 33, 414–420. [Google Scholar] [CrossRef] [Green Version]
- Shan, Z.; Ma, H.; Xie, M.; Yan, P.; Guo, Y.; Bao, W.; Rong, Y.; Jackson, C.L.; Hu, F.B.; Liu, L. Sleep duration and risk of type 2 diabetes: A meta-analysis of prospective studies. Diabetes Care 2015, 38, 529–537. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cappuccio, F.P.; Cooper, D.; Delia, L.; Strazzullo, P.; Miller, M.A. Sleep duration predicts cardiovascular outcomes: A systematic review and meta-analysis of prospective studies. Eur. Heart J. 2011, 32, 1484–1492. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Leng, Y.; Cappuccio, F.P.; Wainwright, N.W.J.; Surtees, P.G.; Luben, R.; Brayne, C.; Khaw, K.T. Sleep duration and risk of fatal and nonfatal stroke: A prospective study and meta-analysis. Neurology 2015, 84, 1072–1079. [Google Scholar] [CrossRef] [PubMed]
- Li, W.; Wang, D.; Cao, S.; Yin, X.; Gong, Y.; Gan, Y.; Zhou, Y.; Lu, Z. Sleep duration and risk of stroke events and stroke mortality: A systematic review and meta-analysis of prospective cohort studies. Int. J. Cardiol. 2016, 223, 870–876. [Google Scholar] [CrossRef]
- Li, J.; Vitiello, M.V.; Gooneratne, N.S. Sleep in Normal Aging. Sleep Med. Clin. 2018, 13, 1–11. [Google Scholar] [CrossRef]
- Furihata, R.; Kaneita, Y.; Jike, M.; Ohida, T.; Uchiyama, M. Napping and associated factors: A Japanese nationwide general population survey. Sleep Med. 2016, 20, 72–79. [Google Scholar] [CrossRef]
- Hagen, E.W.; Barnet, J.H.; Hale, L.; Peppard, P.E. Changes in Sleep Duration and Sleep Timing Associated with Retirement Transitions. Sleep 2016, 39, 665. [Google Scholar] [CrossRef] [Green Version]
- Basner, M.; Spaeth, A.M.; Dinges, D.F. Sociodemographic characteristics and waking activities and their role in the timing and duration of sleep. Sleep 2014, 37, 1889–1906. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yan, B.; Fan, Y.; Zhao, B.; He, X.; Yang, J.; Chen, C.; Ma, X. Association between late bedtime and diabetes mellitus: A large community-based study. J. Clin. Sleep Med. 2019, 15, 1621–1627. [Google Scholar] [CrossRef] [PubMed]
- Jansen, E.C.; Dunietz, G.L.; Matos-Moreno, A.; Solano, M.; Lazcano-Ponce, E.; Sánchez-Zamorano, L.M. Bedtimes and Blood Pressure: A Prospective Cohort Study of Mexican Adolescents. Am. J. Hypertens. 2020, 33, 269–277. [Google Scholar] [CrossRef] [PubMed]
- Sutherland, E.R. Nocturnal asthma: Underlying mechanisms and treatment. Curr. Allergy Asthma Rep. 2005, 5, 161–167. [Google Scholar] [CrossRef] [PubMed]
- Scheer, F.A.J.L.; Hilton, M.F.; Evoniuk, H.L.; Shiels, S.A.; Malhotra, A.; Sugarbaker, R.; Ayers, R.T.; Israel, E.; Massaro, A.F.; Shea, S.A. The endogenous circadian system worsens asthma at night independent of sleep and other daily behavioral or environmental cycles. Proc. Natl. Acad. Sci. USA 2021, 118, e2018486118. [Google Scholar] [CrossRef]
- Krouse, H.J.; Krouse, J.H. Diurnal variability of lung function and its association with sleep among patients with asthma. J. Asthma 2007, 44, 759–763. [Google Scholar] [CrossRef]
- Budhiraja, R.; Siddiqi, T.A.; Quan, S.F. Sleep Disorders in Chronic Obstructive Pulmonary Disease: Etiology, Impact, and Management. J. Clin. Sleep Med. 2015, 11, 259. [Google Scholar] [CrossRef] [PubMed] [Green Version]

| Variable | Total Sleep Duration (Hours) | |||
|---|---|---|---|---|
| <6 n = 205 | 6–8 n = 1162 | >8 n = 656 | p-Value ** | |
| Age (years), Me (Q1, Q3) | 53 (45, 57) | 54 (47, 60) | 60 (52, 65) | <0.001 |
| Sex | ||||
| Female, n (%) | 116 (9.1) | 707 (55.5) | 451 (35.4) | <0.001 |
| Male, n (%) | 89 (11.9) | 455 (60.7) | 205 (27.4) | |
| Place of residence | ||||
| Urban, n (%) | 145 (12.1) | 730 (60.8) | 325 (27.1) | <0.001 |
| Rural, n (%) | 60 (7.3) | 432 (52.5) | 331 (40.2) | |
| Marital status | ||||
| Never married, n (%) | 18 (12.3) | 92 (63.0) | 36 (24.7) | 0.057 |
| Married/living together, n (%) | 152 (10.1) | 870 (58.0) | 478 (31.9) | |
| Separated/divorced/widowed, n (%) | 35 (9.3) | 200 (53.1) | 142 (37.6) | |
| Education | ||||
| Primary or unknown, n (%) | 13 (4.2) | 126 (41.2) | 167 (54.6) | <0.001 |
| Vocational, n (%) | 25 (7.7) | 193 (59.6) | 106 (32.7) | |
| Secondary, n (%) | 97 (12.2) | 444 (56.1) | 251 (31.7) | |
| Higher, n (%) | 70 (11.6) | 399 (66.4) | 132 (22.0) | |
| Professional activity | ||||
| Professionally active, n (%) | 161 (14.5) | 756 (67.9) | 196 (17.6) | <0.001 |
| Retired, n (%) | 35 (5.0) | 316 (45.0) | 352 (50.0) | |
| Pensioner, n (%) | 9 (4.3) | 90 (43.5) | 108 (52.2) | |
| Bedtime | ||||
| 6 p.m.–10 p.m., n (%) | 7 (1.0) | 348 (45.4) | 411 (53.6) | <0.001 |
| 10 p.m.–0 a.m., n (%) | 147 (12.9) | 760 (66.6) | 234 (20.5) | |
| 0 a.m.–4 a.m., n (%) | 51 (43.9) | 54 (46.6) | 11 (9.5) | |
| Naps | ||||
| Taking naps, n (%) | 74 (11.7) | 346 (54.6) | 214 (33.7) | 0.137 |
| Average nap time (min), M ± SD | 47.5 ± 36.4 | 38.5 ± 24.3 | 42.9 ± 27.0 | 0.015 |
| Attitudes toward tobacco smoking | ||||
| Never smokers, n (%) | 89 (9.3) | 520 (54.3) | 349 (36.4) | <0.001 |
| Former smokers, n (%) | 59 (9.2) | 401 (62.5) | 182 (28.3) | |
| Current smokers, n (%) | 57 (13.5) | 241 (57.0) | 125 (29.6) | |
| Attitudes toward alcohol consumption | ||||
| Never drinkers, n (%) | 44 (9.7) | 240 (53.1) | 168 (37.2) | <0.001 |
| Former drinkers, n (%) | 18 (8.7) | 99 (47.6) | 91 (43.6) | |
| Current drinkers, n (%) | 143 (10.5) | 823 (60.4) | 397 (29.1) | |
| Physical activity, MET × min/week * | N = 190 | N = 1063 | N = 612 | |
| Low (<600), n (%) | 3 (4.9) | 33 (54.1) | 25 (41) | 0.157 |
| Moderate (600–3000), n (%) | 48 (9.4) | 281 (54.9) | 183 (35.7) | |
| High (>3000), n (%) | 139 (10.8) | 749 (58.0) | 404 (31.3) | |
| Blood pressure | ||||
| SBP (mm Hg), Mean ± SD | 145 ± 19 | 144 ± 21 | 147 ± 23 | 0.015 |
| DBP (mm Hg), Mean ± SD | 87 ± 11 | 86 ± 12 | 86 ± 11 | 0.314 |
| HR (bmp), Mean ± SD | 74 ± 13 | 72 ± 10 | 72 ± 11 | 0.042 |
| Body Mass Index (BMI) | ||||
| BMI (kg/m2), Mean ± SD | 27.9 ± 4.8 | 28.0 ± 5.0 | 28.5 ± 5.2 | 0.059 |
| Underweight, n (%) | 1 (6.6) | 7 (46.7) | 7 (46.7) | 0.271 |
| Normal, n (%) | 61 (10.7) | 336 (58.9) | 173 (30.4) | |
| Overweight, n (%) | 84 (10.4) | 476 (58.9) | 248 (30.7) | |
| Obesity, n (%) | 59 (9.4) | 343 (54.4) | 227 (36.2) | |
| Waist-to-hip ratio (WHR) | ||||
| WHR (-), Mean ± SD | 0.884 ± 0.094 | 0.880 ± 0.094 | 0.900 ± 0.100 | 0.005 |
| Normal, n (%) | 78 (11.0) | 449 (63.3) | 182 (25.7) | <0.001 |
| Central obesity, n (%) | 127 (9.7) | 713 (54.3) | 474 (36.1) | |
| Noncommunicable diseases | ||||
| Diabetes, n (%) | 12 (6.0) | 86 (43.2) | 101 (50.8) | <0.001 |
| Hypertension, n (%) | 125 (10.3) | 664 (54.5) | 430 (35.3) | 0.002 |
| Cardiovascular diseases, n (%) | 41 (9.3) | 212 (48.3) | 186 (42.4) | <0.001 |
| Respiratory diseases, n (%) | 14 (12.8) | 60 (55.1) | 35 (32.1) | 0.621 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zatońska, K.; Basiak-Rasała, A.; Połtyn-Zaradna, K.; Kinastowski, K.; Szuba, A. Sleep Duration and Bedtime in the PURE Poland Cohort Study and the Link with Noncommunicable Diseases. Int. J. Environ. Res. Public Health 2022, 19, 403. https://doi.org/10.3390/ijerph19010403
Zatońska K, Basiak-Rasała A, Połtyn-Zaradna K, Kinastowski K, Szuba A. Sleep Duration and Bedtime in the PURE Poland Cohort Study and the Link with Noncommunicable Diseases. International Journal of Environmental Research and Public Health. 2022; 19(1):403. https://doi.org/10.3390/ijerph19010403
Chicago/Turabian StyleZatońska, Katarzyna, Alicja Basiak-Rasała, Katarzyna Połtyn-Zaradna, Krystian Kinastowski, and Andrzej Szuba. 2022. "Sleep Duration and Bedtime in the PURE Poland Cohort Study and the Link with Noncommunicable Diseases" International Journal of Environmental Research and Public Health 19, no. 1: 403. https://doi.org/10.3390/ijerph19010403
APA StyleZatońska, K., Basiak-Rasała, A., Połtyn-Zaradna, K., Kinastowski, K., & Szuba, A. (2022). Sleep Duration and Bedtime in the PURE Poland Cohort Study and the Link with Noncommunicable Diseases. International Journal of Environmental Research and Public Health, 19(1), 403. https://doi.org/10.3390/ijerph19010403





