Health Care for Refugees in Europe: A Scoping Review
Abstract
:1. Introduction
- How do refugees and asylum seekers use health care in high-income European countries, and what barriers do they face?
- How do refugees experience access to health care in high-income European countries?
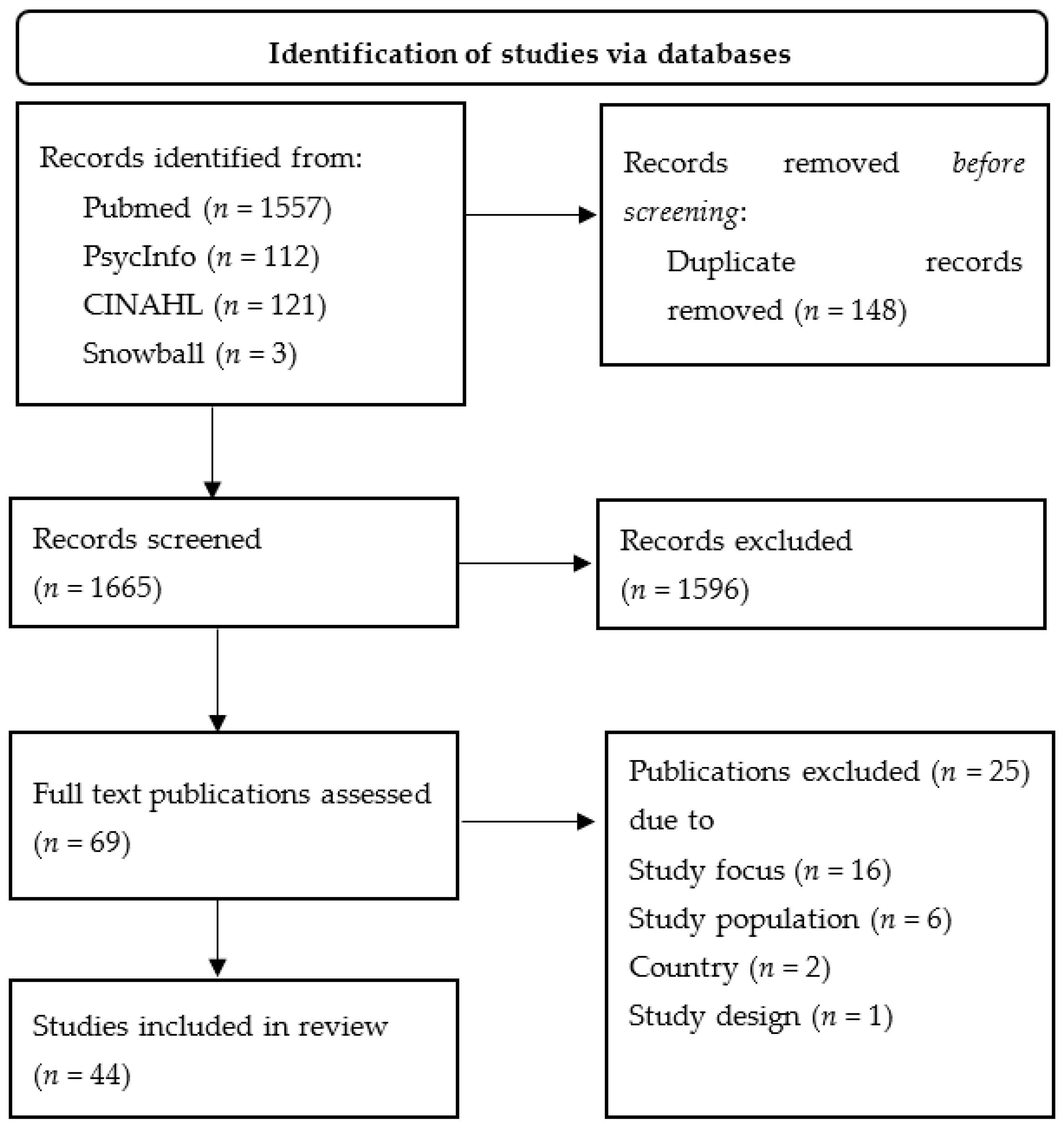
2. Materials and Methods
3. Results
3.1. Descriptive Results on Utilisation and Access Barriers
| Authors | Publication Year | Country | Setting | Study Design |
|---|---|---|---|---|
| Bauhoff and Göpffarth [24] | 2018 | Germany | Cost analysis | Quantitative |
| Bhatia and Wallace [8] | 2007 | UK | Primary Care | Qualitative |
| Bhui et al. [15] | 2006 | UK | Inpatient psychiatric care | Quantitative |
| Bianco et al. [31] | 2015 | Italy | Health care by NGOs | Quantitative |
| Biddle et al. [32] | 2019 | Germany | Inpatient and outpatient care | Quantitative |
| Bischoff et al. [40] | 2003 | Switzerland | Inpatient care | Quantitative |
| Blöchliger et al. [50] | 1998 | Switzerland | Primary Care | Quantitative |
| Boettcher et al. [18] | 2021 | Germany | Psychiatric care | Quantitative |
| Borgschulte et al. [29] | 2018 | Germany | Primary care | Mixed-Method |
| Bozorgmehr et al. [30] | 2015 | Germany | Primary Care | Quantitative |
| Chiarenza et al. [4] | 2019 | European countries | Transit | Mixed-Method |
| Cignacco et al. [28] | 2018 | Switzerland | Sexual and reproductive care | Mixed-Method |
| Claassen & Jäger [26] | 2018 | Germany | Primary Care | Quantitative |
| Fang et al. [12] | 2015 | UK | Primary Care | Qualitative |
| Feldmann et al. [47] | 2007a | Netherlands | Primary Care | Qualitative |
| Feldmann et al. [49] | 2007b | Netherlands | Primary Care | Qualitative |
| Führer et al. [19] | 2020 | Germany | Psychiatric care | Quantitative |
| Gerritsen et al. [34] | 2006 | Netherlands | Primary Care | Quantitative |
| Hahn et al. [10] | 2020 | Germany | Inpatient and outpatient care | Qualitative |
| Jäger et al. [27] | 2019 | Germany | Primary care | Quantitative |
| Jensen et al. [46] | 2014 | Denmark | Inpatient psychiatric Care | Qualitative |
| Kang et al. [13] | 2019 | UK | Primary Care | Qualitative |
| Klingberg et al. [35] | 2020 | Switzerland | Emergency care | Quantitative |
| Kohlenberger et al. [33] | 2019 | Austria | Inpatient and outpatient care | Quantitative |
| Laban et al. [16] | 2007 | Netherlands | Primary care | Quantitative |
| Lamkaddem et al. [38] | 2014 | Netherlands | Psychiatric Care | Quantitative |
| Maier et al. [23] | 2010 | Switzerland | Cost analysis | Quantitative |
| Mangrio et al. [43] | 2018 | Sweden | Inpatient and outpatient care | Mixed-Method |
| Mårtensson et al. [44] | 2020 | Sweden | Health care information | Qualitative |
| Melamed et al. [20] | 2019 | Switzerland | Psychiatric care | Qualitative |
| Norredam et al. [7] | 2005 | EU countries | Comparative study | Quantitative |
| O’Donnell [39] | 2007 | UK | Primary Care | Qualitative |
| O’Donnell [48] | 2008 | UK | Primary Care | Qualitative |
| Razavi et al. [45] | 2011 | Sweden | Long term health care | Qualitative |
| Riza et al. [37] | 2020 | EU | Inpatient and outpatient care | Quantitative |
| Schein et al. [42] | 2019 | Norway | Inpatient and outpatient care | Qualitative |
| Schneider et al. [11] | 2015 | Germany | Inpatient and outpatient care | Quantitative |
| Spura et al. [9] | 2017 | Germany | Inpatient and outpatient care | Qualitative |
| Toar et al. [21] | 2009 | Ireland | Psychiatric care | Quantitative |
| Van Loenen et al. [14] | 2017 | EU | Primary Care | Qualitative |
| Wångdahl et al. [36] | 2018 | Sweden | Health literacy | Quantitative |
| Wenner et al. [25] | 2020 | Germany | Inpatient and outpatient care | Quantitative |
| Wetzke et al. [17] | 2018 | Germany | Primary Care | Quantitative |
| Zander et al. [41] | 2013 | Sweden | Inpatient and outpatient care | Qualitative |
3.2. Lived Experiences of Asylum Seekers and Refugees Using Health Care in Host Countries
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Eurostat. Asylbewerber und Erstmalige Asylbewerber nach Staatsangehörigkeit, Alter und Geschlecht—Jährliche Aggregierte Daten (Gerundet). Data File. 2021. Available online: https://appsso.eurostat.ec.europa.eu/nui/show.do?dataset=migr_asyappctza&lang=de (accessed on 8 January 2022).
- Brandenberger, J.; Tylleskär, T.; Sontag, K.; Peterhans, B.; Ritz, N. A systematic literature review of reported challenges in health care delivery to migrants and refugees in high-income countries: The 3C model. BMC Public Health 2019, 19, 755. [Google Scholar] [CrossRef]
- Smith, J. Migrant health is public health, and public health needs to be political. Lancet Public Health 2018, 3, e418. [Google Scholar] [CrossRef] [Green Version]
- Chiarenza, A.; Dauvrin, M.; Chiesa, V.; Baatout, S.; Verrept, H. Supporting access to healthcare for refugees and migrants in European countries under particular migratory pressure. BMC Health Serv. Res. 2019, 19, 513. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lebano, A.; Hamed, S.; Bradby, H.; Gil-Salmerón, A.; Durá-Ferrandis, E.; Garcés-Ferrer, J.; Azzedine, F.; Riza, E.; Karnaki, P.; Zota, D.; et al. Migrants’ and refugees’ health status and healthcare in Europe: A scoping literature review. BMC Public Health 2020, 20, 1039. [Google Scholar] [CrossRef] [PubMed]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L.; et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef] [Green Version]
- Norredam, M.; Mygind, A.; Krasnik, A. Access to health care for asylum seekers in the European Union—a comparative study of country policies. Eur. J. Public Health 2006, 16, 286–290. [Google Scholar] [CrossRef] [Green Version]
- Bhatia, R.; Wallace, P. Experiences of refugees and asylum seekers in general practice: A qualitative study. BMC Fam. Pract. 2007, 8, 48. [Google Scholar] [CrossRef] [Green Version]
- Spura, A.; Kleinke, M.; Robra, B.P.; Ladebeck, N. How do asylum seekers experience access to medical care? Bundesgesundheitsblatt Gesundh. Gesundh. 2017, 60, 462–470. [Google Scholar] [CrossRef] [PubMed]
- Hahn, K.; Steinhäuser, J.; Goetz, K. Equity in Health Care: A Qualitative Study with Refugees, Health Care Professionals, and Administrators in One Region in Germany. BioMed Res. Int. 2020, 2020, 4647389. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schneider, C.; Joos, S.; Bozorgmehr, K. Disparities in health and access to healthcare between asylum seekers and residents in Germany: A population-based cross-sectional feasibility study. BMJ Open 2015, 5, e008784. [Google Scholar] [CrossRef] [Green Version]
- Fang, M.L.; Sixsmith, J.; Lawthom, R.; Mountian, I.; Shahrin, A. Experiencing ‘pathologized presence and normalized absence’; understanding health related experiences and access to health care among Iraqi and Somali asylum seekers, refugees and persons without legal status. BMC Public Health 2015, 15, 923. [Google Scholar] [CrossRef] [PubMed]
- Kang, C.; Tomkow, L.; Farrington, R. Access to primary health care for asylum seekers and refugees: A qualitative study of service user experiences in the UK. Br. J. Gen. Pract. 2019, 69, e537–e545. [Google Scholar] [CrossRef] [PubMed]
- van Loenen, T.; van den Muijsenbergh, M.; Hofmeester, M.; Dowrick, C.; van Ginneken, N.; Mechili, E.A.; Angelaki, A.; Ajdukovic, D.; Bagic, H.; Pavlic, D.R.; et al. Primary care for refugees and newly arrived migrants in Europe: A qualitative study on health needs, barriers and wishes. Eur. J. Public Health 2018, 28, 82–87. [Google Scholar] [CrossRef]
- Bhui, K.; Audini, B.; Singh, S.; Duffett, R.; Bhugra, D. Representation of asylum seekers and refugees among psychiatric inpatients in London. Psychiatr. Serv. 2006, 57, 270–272. [Google Scholar] [CrossRef] [PubMed]
- Laban, C.J.; Gernaat, H.B.; Komproe, I.H.; De Jong, J.T. Prevalence and predictors of health service use among Iraqi asylum seekers in the Netherlands. Soc. Psychiatry Psychiatr. Epidemiol. 2007, 42, 837–844. [Google Scholar] [CrossRef] [Green Version]
- Wetzke, M.; Happle, C.; Vakilzadeh, A.; Ernst, D.; Sogkas, G.; Schmidt, R.E.; Behrens, G.M.N.; Dopfer, C.; Jablonka, A. Healthcare Utilization in a Large Cohort of Asylum Seekers Entering Western Europe in 2015. Int. J. Environ. Res. Public Health 2018, 15, 2163. [Google Scholar] [CrossRef] [Green Version]
- Boettcher, V.S.; Nowak, A.C.; Neuner, F. Mental health service utilization and perceived barriers to treatment among adult refugees in Germany. Eur. J. Psychotraumatol. 2021, 12, 1910407. [Google Scholar] [CrossRef]
- Führer, A.; Niedermaier, A.; Kalfa, V.; Mikolajczyk, R.; Wienke, A. Serious shortcomings in assessment and treatment of asylum seekers’ mental health needs. PLoS ONE 2020, 15, e0239211. [Google Scholar] [CrossRef]
- Melamed, S.; Chernet, A.; Labhardt, N.D.; Probst-Hensch, N.; Pfeiffer, C. Social Resilience and Mental Health Among Eritrean Asylum-Seekers in Switzerland. Qual. Health Res. 2019, 29, 222–236. [Google Scholar] [CrossRef]
- Toar, M.; O’Brien, K.K.; Fahey, T. Comparison of self-reported health & healthcare utilisation between asylum seekers and refugees: An observational study. BMC Public Health 2009, 9, 214. [Google Scholar] [CrossRef] [Green Version]
- Gottlieb, N.; Püschmann, C.; Stenzinger, F.; Koelber, J.; Rasch, L.; Koppelow, M.; Al Munjid, R. Health and Healthcare Utilization among Asylum-Seekers from Berlin’s LGBTIQ Shelter: Preliminary Results of a Survey. Int. J. Environ. Res. Public Health 2020, 17, 4514. [Google Scholar] [CrossRef]
- Maier, T.; Schmidt, M.; Mueller, J. Mental health and healthcare utilization in adult asylum seekers. Swiss Med. Wkly. 2010, 140, w13110. [Google Scholar] [CrossRef] [Green Version]
- Bauhoff, S.; Göpffarth, D. Asylum-seekers in Germany differ from regularly insured in their morbidity, utilizations and costs of care. PLoS ONE 2018, 13, e0197881. [Google Scholar] [CrossRef] [Green Version]
- Wenner, J.; Bozorgmehr, K.; Duwendag, S.; Rolke, K.; Razum, O. Differences in realized access to healthcare among newly arrived refugees in Germany: Results from a natural quasi-experiment. BMC Public Health 2020, 20, 846. [Google Scholar] [CrossRef]
- Claassen, K.; Jäger, P. Impact of the Introduction of the Electronic Health Insurance Card on the Use of Medical Services by Asylum Seekers in Germany. Int J. Environ. Res. Public Health 2018, 15, 856. [Google Scholar] [CrossRef] [Green Version]
- Jäger, P.; Claassen, K.; Ott, N.; Brand, A. Does the Electronic Health Card for Asylum Seekers Lead to an Excessive Use of the Health System? Results of a Survey in Two Municipalities of the German Ruhr Area. Int J. Environ. Res. Public Health 2019, 16, 1178. [Google Scholar] [CrossRef] [Green Version]
- Cignacco, E.; Zu Sayn-Wittgenstein, F.; Sénac, C.; Hurni, A.; Wyssmüller, D.; Grand-Guillaume-Perrenoud, J.A.; Berger, A. Sexual and reproductive healthcare for women asylum seekers in Switzerland: A multi-method evaluation. BMC Health Serv. Res. 2018, 18, 712. [Google Scholar] [CrossRef]
- Borgschulte, H.S.; Wiesmüller, G.A.; Bunte, A.; Neuhann, F. Health care provision for refugees in Germany—one-year evaluation of an outpatient clinic in an urban emergency accommodation. BMC Health Serv. Res. 2018, 18, 488. [Google Scholar] [CrossRef] [Green Version]
- Bozorgmehr, K.; Schneider, C.; Joos, S. Equity in access to health care among asylum seekers in Germany: Evidence from an exploratory population-based cross-sectional study. BMC Health Serv. Res. 2015, 15, 502. [Google Scholar] [CrossRef] [Green Version]
- Bianco, A.; Larosa, E.; Pileggi, C.; Nobile, C.G.A.; Pavia, M. Utilization of health-care services among immigrants recruited through non-profit organizations in southern Italy. Int J. Public Health 2016, 61, 673–682. [Google Scholar] [CrossRef]
- Biddle, L.; Menold, N.; Bentner, M.; Nöst, S.; Jahn, R.; Ziegler, S.; Bozorgmehr, K. Health monitoring among asylum seekers and refugees: A state-wide, cross-sectional, population-based study in Germany. Emerg. Themes Epidemiol. 2019, 16, 3. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kohlenberger, J.; Buber-EnnserI, I.; Rengs, B.; Leitner, S.; Landesmann, M. Barriers to health care access and service utilization of refugees in Austria: Evidence from a cross-sectional survey. Health Policy 2019, 123, 833–839. [Google Scholar] [CrossRef] [PubMed]
- Gerritsen, A.A.M.; Bramsen, I.; Devillé, W.; van Willigen, L.H.M.; Hovens, J.-E.; van der Ploeg, H.M. Use of health services by Afghan, Iranian, and Somali refugees and asylum seekers living in the Netherlands. Eur. J. Public Health 2016, 16, 394–399. [Google Scholar] [CrossRef] [Green Version]
- Klingberg, K.; Stoller, A.; Müller, M.; Jegerlehner, S.; Brown, A.D.; Exadaktylos, A.; Jachmann, A.; Srivastava, D. Asylum Seekers and Swiss Nationals with Low-Acuity Complaints: Disparities in the Perceived level of Urgency, Health Literacy and Ability to Communicate:A Cross-Sectional Survey at a Tertiary Emergency Department. Int. J. Environ. Res. Public Health 2020, 17, 2769. [Google Scholar] [CrossRef] [PubMed]
- Wångdahl, J.; Lytsy, P.; Mårtensson, L.; Westerling, R. Poor health and refraining from seeking healthcare are associated with comprehensive health literacy among refugees: A Swedish cross-sectional study. Int. J. Public Health 2018, 63, 409–419. [Google Scholar] [CrossRef] [Green Version]
- Riza, E.; Karnaki, P.; Gil-Salmerón, A.; Zota, K.; Ho, M.; Petropoulou, M.; Katsas, K.; Garcés-Ferrer, J.; Linos, A. Determinants of Refugee and Migrant Health Status in 10 European Countries: The Mig-HealthCare Project. Int J. Environ. Res. Public Health 2020, 17, 6353. [Google Scholar] [CrossRef]
- Lamkaddem, M.; Stronks, K.; Devillé, W.D.; Olff, M.; Gerritsen, A.A.; Essink-Bot, M.L. Course of post-traumatic stress disorder and health care utilisation among resettled refugees in the Netherlands. BMC Psychiatry 2014, 14, 90. [Google Scholar] [CrossRef] [Green Version]
- O’Donnell, C.A.; Higgins, M.; Chauhan, R.; Mullen, K. “They think we’re OK and we know we’re not”. A qualitative study of asylum seekers’ access, knowledge and views to health care in the UK. BMC Health Serv. Res. 2007, 7, 75. [Google Scholar] [CrossRef] [Green Version]
- Bischoff, A.; Bovier, P.A.; Rrustemi, I.; Gariazzo, F.; Eytan, A.; Loutan, L. Language barriers between nurses and asylum seekers: Their impact on symptom reporting and referral. Soc. Sci. Med. 2003, 57, 503–512. [Google Scholar] [CrossRef]
- Zander, V.; Müllersdorf, M.; Christensson, K.; Eriksson, H. Struggling for sense of control: Everyday life with chronic pain for women of the Iraqi diaspora in Sweden. Scand. J. Public Health 2013, 41, 799–807. [Google Scholar] [CrossRef]
- Schein, Y.L.; Winje, B.A.; Myhre, S.L.; Nordstoga, I.; Straiton, M.L. A qualitative study of health experiences of Ethiopian asylum seekers in Norway. BMC Health Serv. Res. 2019, 19, 958. [Google Scholar] [CrossRef]
- Mangrio, E.; Carlson, E.; Zdravkovic, S. Understanding experiences of the Swedish health care system from the perspective of newly arrived refugees. BMC Res. Notes 2018, 11, 616. [Google Scholar] [CrossRef] [Green Version]
- Mårtensson, L.; Lytsy, P.; Westerling, R.; Wångdahl, J. Experiences and needs concerning health related information for newly arrived refugees in Sweden. BMC Public Health 2020, 20, 1044. [Google Scholar] [CrossRef]
- Razavi, M.F.; Falk, L.; Björn, Å.; Wilhelmsson, S. Experiences of the Swedish healthcare system: An interview study with refugees in need of long-term health care. Scand. J. Public Health 2011, 39, 319–325. [Google Scholar] [CrossRef]
- Jensen, N.K.; Johansen, K.S.; Kastrup, M.; Krasnik, A.; Norredam, M. Patient experienced continuity of care in the psychiatric healthcare system-a study including immigrants, refugees and ethnic danes. Int J. Environ. Res. Public Health 2014, 11, 9739–9759. [Google Scholar] [CrossRef] [Green Version]
- Feldmann, C.T.; Bensing, J.M.; de Ruijter, A. Worries are the mother of many diseases: General practitioners and refugees in the Netherlands on stress, being ill and prejudice. Patient Educ. Couns. 2007, 65, 369–380. [Google Scholar] [CrossRef] [Green Version]
- O’Donnell, C.A.; Higgins, M.; Chauhan, R.; Mullen, K. Asylum seekers’ expectations of and trust in general practice: A qualitative study. Br. J. Gen. Pract. 2008, 58, e1–e11. [Google Scholar] [CrossRef] [Green Version]
- Feldmann, C.T.; Bensing, J.M.; de Ruijter, A.; Boeije, H.R. Afghan refugees and their general practitioners in The Netherlands: To trust or not to trust. Sociol. Health Illn. 2007, 29, 515–535. [Google Scholar] [CrossRef] [Green Version]
- Blöchliger, C.; Osterwalder, J.; Hatz, C.; Tanner, M.; Junghanss, T. Asylum seekers and refugees in the emergency department. Soz. Prav. 1998, 43, 39–48. [Google Scholar] [CrossRef]
- Pollard, T.; Howard, N. Mental healthcare for asylum-seekers and refugees residing in the United Kingdom: A scoping review of policies, barriers, and enablers. Int. J. Ment. Health Syst. 2021, 15, 60. [Google Scholar] [CrossRef]
- Munz, D.; Melcop, N. The psychotherapeutic care of refugees in Europe: Treatment needs, delivery reality and recommendations for action. Eur. J. Psychotraumatol. 2018, 9, 1476436. [Google Scholar] [CrossRef]
- Karliner, L.S.; Jacobs, E.A.; Chen, A.H.; Mutha, S. Do professional interpreters improve clinical care for patients with limited English proficiency? A systematic review of the literature. Health Serv. Res. 2007, 42, 727–754. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Griswold, K.S.; Pottie, K.; Kim, I.; Kim, W.; Lin, L. Strengthening effective preventive services for refugee populations: Toward communities of solution. Public Health Rev. 2018, 39, 3. [Google Scholar] [CrossRef] [Green Version]
- Smith Jervelund, S.; Maltesen, T.; Wimmelmann, C.L.; Petersen, J.H.; Krasnik, A. Ignorance is not bliss: The effect of systematic information on immigrants’ knowledge of and satisfaction with the Danish healthcare system. Scand. J. Public Health 2017, 45, 161–174. [Google Scholar] [CrossRef] [PubMed]
- Marmot, M.; Friel, S.; Bell, R.; Houweling, T.A.; Taylor, S. Closing the gap in a generation: Health equity through action on the social determinants of health. Lancet 2008, 372, 1661–1669. [Google Scholar] [CrossRef]
- Rechel, B.; Mladovsky, P.; Ingleby, D.; Mackenbach, J.P.; McKee, M. Migration and health in an increasingly diverse Europe. Lancet 2013, 381, 1235–1245. [Google Scholar] [CrossRef]
- Chen, W.; Hall, B.J.; Ling, L.; Renzaho, A.M. Pre-migration and post-migration factors associated with mental health in humanitarian migrants in Australia and the moderation effect of post-migration stressors: Findings from the first wave data of the BNLA cohort study. Lancet Psychiatry 2017, 4, 218–229. [Google Scholar] [CrossRef]
| Inclusion Criteria | Exclusion Criteria |
|---|---|
|
|
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nowak, A.C.; Namer, Y.; Hornberg, C. Health Care for Refugees in Europe: A Scoping Review. Int. J. Environ. Res. Public Health 2022, 19, 1278. https://doi.org/10.3390/ijerph19031278
Nowak AC, Namer Y, Hornberg C. Health Care for Refugees in Europe: A Scoping Review. International Journal of Environmental Research and Public Health. 2022; 19(3):1278. https://doi.org/10.3390/ijerph19031278
Chicago/Turabian StyleNowak, Anna Christina, Yudit Namer, and Claudia Hornberg. 2022. "Health Care for Refugees in Europe: A Scoping Review" International Journal of Environmental Research and Public Health 19, no. 3: 1278. https://doi.org/10.3390/ijerph19031278
APA StyleNowak, A. C., Namer, Y., & Hornberg, C. (2022). Health Care for Refugees in Europe: A Scoping Review. International Journal of Environmental Research and Public Health, 19(3), 1278. https://doi.org/10.3390/ijerph19031278





