Characteristics of Plantar Pressure with Foot Postures and Lower Limb Pain Profiles in Taiwanese College Elite Rugby League Athletes
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Instruments
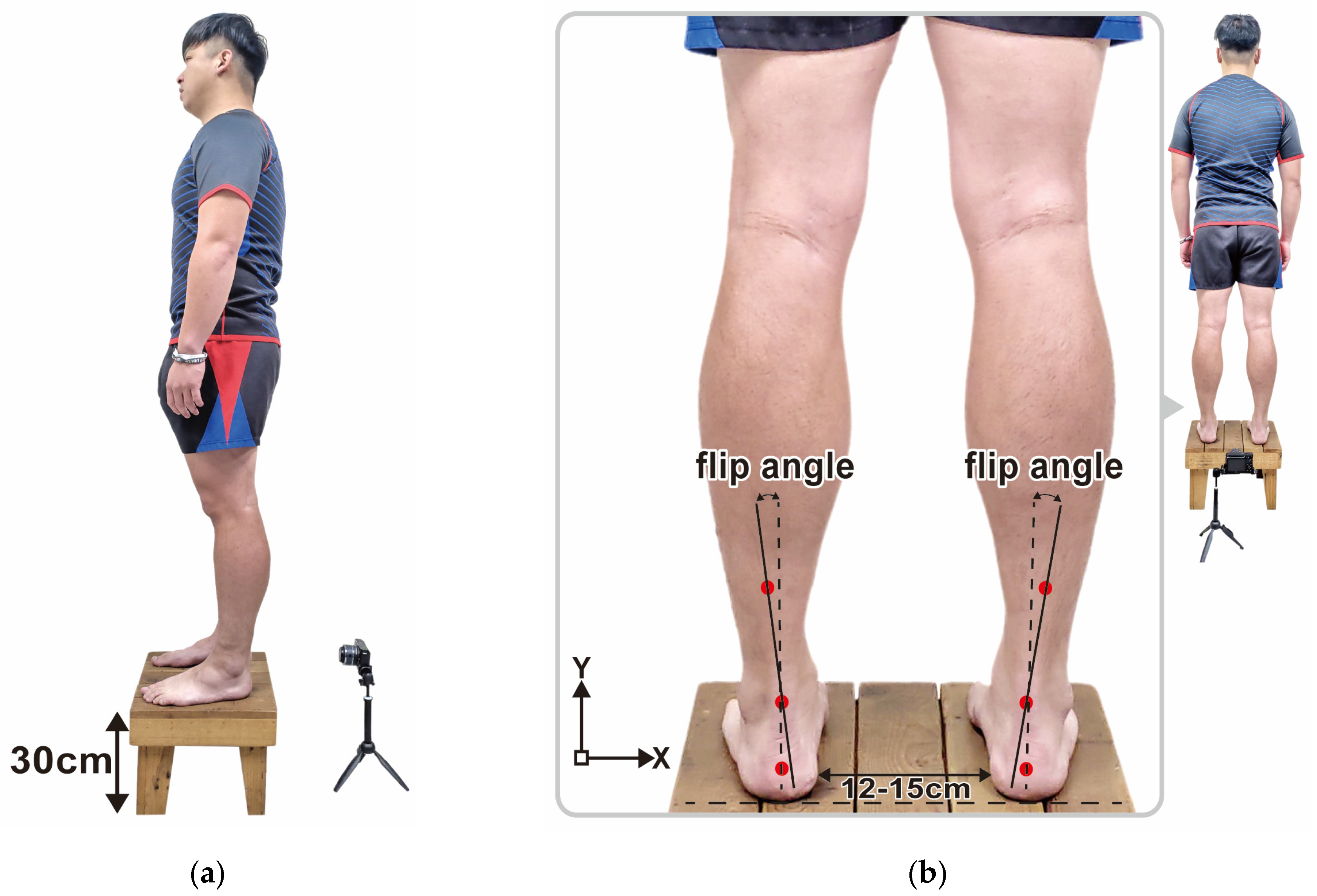
2.3. PPDs Assessment
- Roll the two trouser legs above the knees to avoid clothing restricting the movement of the limbs.
- Stand barefoot on the JC Mat sensor mat with specific markings and measuring range.
- Stand with feet shoulder-width apart and distribute body weight evenly on feet to control and balance the center of gravity.
- Stand in a natural posture, with arms hanging vertically at sides.
- Face the experiment instructor. Look the instructor straight in the eye. Keep the body still and balanced and relax the whole body until the foot pressure measured by JC Mat does not change significantly.
2.4. PPDs Data Analysis
2.5. Rearfoot Postural Alignment Assessment
2.6. Pain Assessment and Self-Reported Health Status
- The physiotherapist examined the elite rugby athletes’ self-reported health status and pain complaints, and guided them to stand with bare feet and roll their trouser legs up to above the knees.
- The physiotherapist examined the elite rugby athletes’ lower extremities by palpating and pressing their feet (including navicular bones, cuboid bones, phalanges, metatarsals, and calcaneus), ankles, patella, knees, hips, tibias, fibulas and femur according to the participants’ self-reported health status, and re-examined the corresponding position on the other side of the pain areas. The physiotherapist then assessed the skeletal arrangement of the athletes’ lower limbs.
- In order to confirm the athletes’ pain areas precisely, the physiotherapist examined the following specific parts of the athletes’ common pain areas: (1) soft tissues, e.g., the plantar fascia, the Achilles tendon, the gastrocnemius, the tibialis anterior and posterior, the biceps, the quadriceps femoris, the medial and lateral ankle ligaments, the anterior cruciate ligaments, the medial and lateral collateral ligaments, the abductor hallucis and abductor digiti minimi of plantar plate and the lower back; (2) bone tissues of both feet, i.e., navicular bones, cuboid bones, phalanges, metatarsals, and calcaneus; (3) the ankles; (4) the patella; (5) the knees; (6) the hips; and (7) tibias.
2.7. Statistical Analysis
3. Results
3.1. Arch Index
3.2. PPDs of the Three Regions in Static and Dynamic States
3.3. PPDs of the Six Subregions in Static Standing
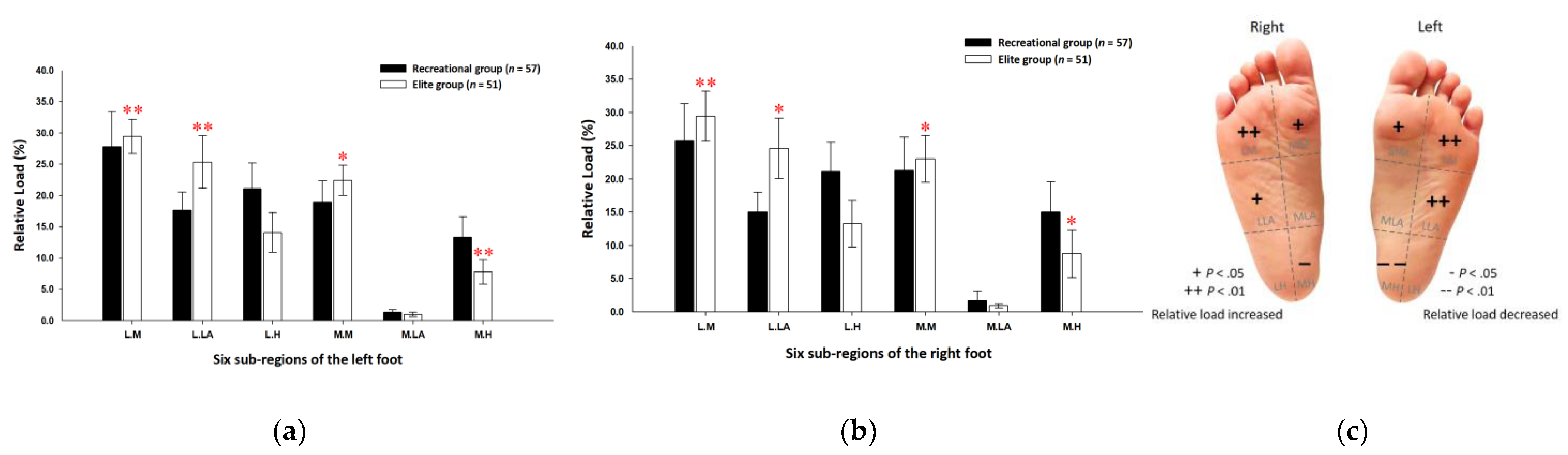
3.4. PPDs of the Six Subregions during the Midstance Phase of Walking
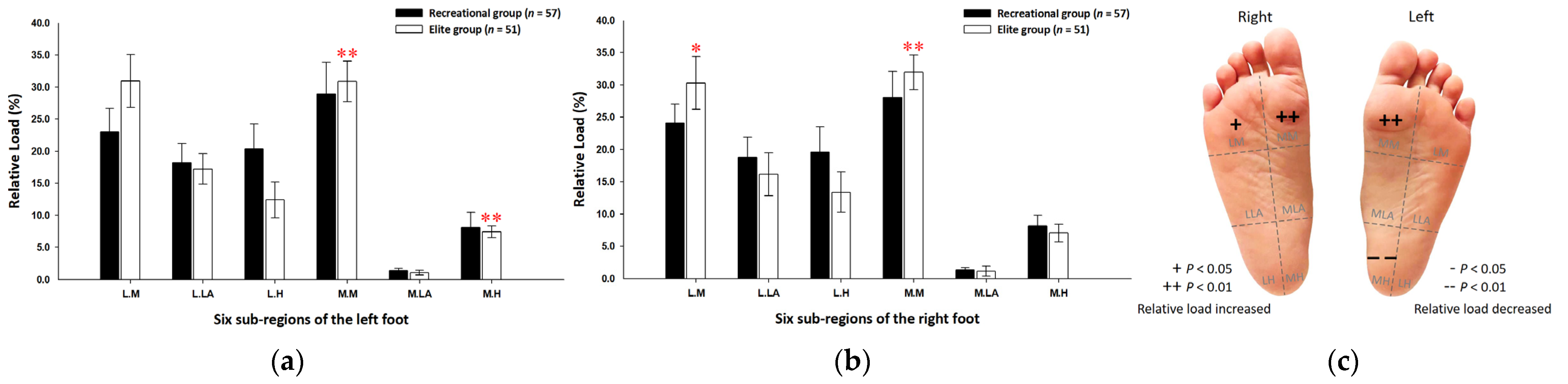
3.5. Footprint Image Characteristics
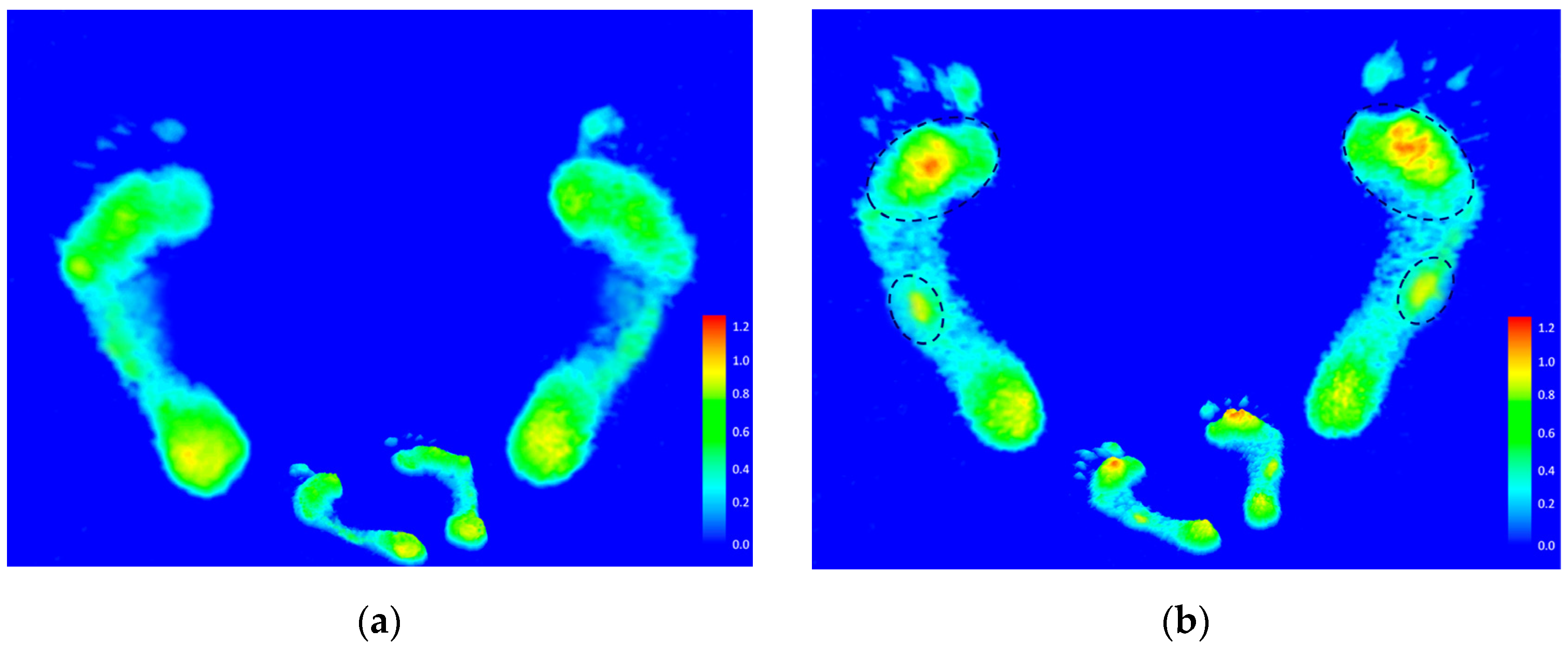
3.6. Rearfoot Postural Alignment Assessment
3.7. Pain Assessment and Self-Reported Health Status of the Participants
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Mickle, K.J.; Steele, J.R.; Munro, B.J. Does excess mass affect plantar pressure in young children? Int. J. Pediatric Obes. 2006, 1, 183–188. [Google Scholar] [CrossRef] [PubMed]
- Yan, S.H.; Zhang, K.; Tan, G.Q.; Liu, Z.C. Effects of obesity on dynamic plantar pressure distribution in Chinese prepubescent children during walking. Gait Posture 2013, 37, 37–42. [Google Scholar] [CrossRef]
- Park, S.-Y.; Park, D.-J. Comparison of Foot Structure, Function, Plantar Pressure and Balance Ability According to the Body Mass Index of Young Adults. Osong Public Heal. Res. Perspect. 2019, 10, 102–107. [Google Scholar] [CrossRef]
- Ripani, M.; Ciccarelli, A.; Morini, S.; Ricciardi, G.; Michielon, G. Evaluation of foot support in rugby players: A baropo-dometric analysis. Sport Sci. Health 2006, 1, 104–108. [Google Scholar] [CrossRef]
- Baumfeld, T.; Rezende, R.F.; Nery, C.; Batista, J.P.; Baumfeld, D. Fifth Metatarsal Fractures in Professional Soccer Players: Case Series. Foot Ankle Spéc. 2020, 14, 213–218. [Google Scholar] [CrossRef]
- Girard, O.; Millet, G.P.; Thomson, A.; Brocherie, F. Is plantar loading altered during repeated sprints on artificial turf in in-ternational? J. Sports Sci. Med. 2018, 17, 359–365. [Google Scholar]
- Porter, D.A.; Klott, J. Proximal fifth metatarsal fractures in athletes: Management of acute and chronic conditions. Foot Ankle Clin. 2021, 26, 35–63. [Google Scholar] [CrossRef] [PubMed]
- Stone, J.A.; Miranda, A.D.; Gerhardt, M.B.; Mandelbaum, B.R.; Giza, E. Outcomes of surgically treated fifth metatarsal frac-tures in major league soccer athletes. Am. J. Sports Med. 2021, 49, 3014–3020. [Google Scholar] [CrossRef]
- Hunt, K.J.; Goeb, Y.; Bartolomei, J. Dynamic Loading Assessment at the Fifth Metatarsal in Elite Athletes With a History of Jones Fracture. Clin. J. Sport Med. 2020, 31, e321–e326. [Google Scholar] [CrossRef]
- Lewson, E.B.; Pulsifer, M.S.E.; Mallette, J.P. Cuboid sling: A novel surgical repair of cuboid syndrome and literature review. Foot Ankle Surg. Tech. Rep. Cases 2021, 1. [Google Scholar] [CrossRef]
- Marshall, P.; Hamilton, W.G. Cuboid subluxation in ballet dancers. Am. J. Sports Med. 1992, 20, 169–175. [Google Scholar] [CrossRef]
- Gabbett, T.J. The training-injury prevention paradox: Should athletes be training smarter and harder? Br. J. Sports Med. 2016, 50, 273–280. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Carl, H.D.; Pauser, J.; Swoboda, B.; Jendrissek, A.; Brem, M. Soccer boots elevate plantar pressures in elite male soccer pro-fessionals. Clin. J. Sport Med. 2014, 24, 58–61. [Google Scholar] [CrossRef]
- Orendurff, M.S.; Rohr, E.S.; Segal, A.D.; Medley, J.W.; Green, J.R., 3rd; Kadel, N.J. Regional foot pressure during running, cutting, jumping, and landing. Am. J. Sports Med. 2008, 36, 566–571. [Google Scholar] [CrossRef] [PubMed]
- Gobbi, G.; Galli, D.; Carubbi, C.; Pelosi, A.; Lillia, M.; Gatti, R.; Queirolo, V.; Costantino, C.; Vitale, M.; Saccavini, M.; et al. Assessment of body plantar pressure in elite athletes: An observational study. Sport Sci. Health 2013, 9, 13–18. [Google Scholar] [CrossRef]
- Zhang, C.; Pan, S.; Qi, Y.; Yang, Y. A Footprint Extraction and Recognition Algorithm Based on Plantar Pressure. Trait. Signal. 2019, 36, 419–424. [Google Scholar] [CrossRef]
- Truong, P.; You, S.; Ji, S.-H.; Jeong, G.-M. Adaptive Accumulation of Plantar Pressure for Ambulatory Activity Recognition and Pedestrian Identification. Sensors 2021, 21, 3842. [Google Scholar] [CrossRef]
- Monteiro, R.L.; Sartor, C.D.; Ferreira, J.S.S.P.; Dantas, M.G.B.; Bus, S.A.; Sacco, I.C.N. Protocol for evaluating the effects of a foot-ankle therapeutic exercise program on daily activity, foot-ankle functionality, and biomechanics in people with diabetic polyneuropathy: A randomized controlled trial. BMC Musculoskelet. Disord. 2018, 19, 1–12. [Google Scholar] [CrossRef] [Green Version]
- Helili, M.; Geng, X.; Ma, X.; Chen, W.; Zhang, C.; Huang, J.; Wang, X. An investigation of regional plantar soft tissue hard-ness and its potential correlation with plantar pressure distribution in healthy adults. Appl. Bionics Biomech. 2021. [Google Scholar] [CrossRef]
- Chuter, V.H.; Spink, M.J.; David, M.; Lanting, S.; Searle, A. Clinical foot measurements as a proxy for plantar pressure testing in people with diabetes. J. Foot Ankle Res. 2021, 14, 56. [Google Scholar] [CrossRef]
- Zhang, B.; Lu, Q. A Current Review of Foot Disorder and Plantar Pressure Alternation in the Elderly. Phys. Act. Heal. 2020, 4, 95–106. [Google Scholar] [CrossRef]
- Hollander, K.; Zech, A.; Rahlf, A.L.; Orendurff, M.S.; Stebbins, J.; Heidt, C. The relationship between static and dynamic foot posture and running biomechanics: A systematic review and meta-analysis. Gait Posture 2019, 72, 109–122. [Google Scholar] [CrossRef] [PubMed]
- Willems, T.; De Ridder, R.; Roosen, P. The effect of a long-distance run on plantar pressure distribution during running. Gait Posture 2012, 35, 405–409. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Wang, W.; Chen, G.; Ji, A.; Song, Y. Effects of standing and walking on plantar pressure distribution in recrea-tional runners before and after long-distance running. J. Biomech. 2021, 129, 110779. [Google Scholar] [CrossRef] [PubMed]
- Lung, C.W.; Liau, B.Y.; Peters, J.A.; He, L.; Townsend, R.; Jan, Y.K. Effects of various walking intensities on leg muscle fatigue and plantar pressure distributions. BMC Musculoskelet. Disord. 2021, 22, 831. [Google Scholar] [CrossRef]
- Wang, J.-C.; Dommati, H.; Cheng, J. A Turnkey Manufacturing Solution for Customized Insoles Using Material Extrusion Process. In 3D Printing and Additive Manufacturing Technologies; Kumar, L., Pandey, P., Wimpenny, D., Eds.; Springer: Singapore, 2018; pp. 203–216. [Google Scholar]
- Chow, T.H.; Chen, Y.S.; Wang, J.C. Characteristics of plantar pressures and related pain profiles in elite sprinters and recre-ational runners. J. Am. Podiatr. Med. Assoc. 2018, 108, 33–44. [Google Scholar] [CrossRef]
- Chow, T.-H.; Chen, Y.-S.; Tsai, W.-C.; Lin, M.-H. Plantar Pressure Profiles and Possible Foot Syndromes of Taiwanese College Elite Basketball Players. J. Am. Podiatr. Med. Assoc. 2020, 111. [Google Scholar] [CrossRef]
- Zhao, Y.; Zheng, D.; Yan, S.; Liu, M.; Yang, L. Children with obesity experience different age-related changes in plantar pres-sure distributions: A follow-up study in China. Int. J. Environ. Res. Public Health 2020, 17, 6602. [Google Scholar] [CrossRef]
- Lee, H.; Ishikawa, H.; Shibuya, T.; Takai, C.; Nemoto, T.; Nomura, Y.; Abe, A.; Otani, H.; Ito, S.; Nakazono, K.; et al. The Combination of Modified Mitchell’s Osteotomy and Shortening Oblique Osteotomy for Patients with Rheumatoid Arthritis: An Analysis of Changes in Plantar Pressure Distribution. Int. J. Environ. Res. Public Health 2021, 18, 9948. [Google Scholar] [CrossRef]
- Hawrylak, A.; Brzeźna, A.; Chromik, K. Distribution of Plantar Pressure in Soccer Players. Int. J. Environ. Res. Public Health 2021, 18, 4173. [Google Scholar] [CrossRef]
- Cavanagh, P.R.; Rodgers, M.M. The arch index: A useful measure from footprints. J. Biomech. 1987, 20, 547–551. [Google Scholar] [CrossRef]
- Ribeiro, A.P.; Sacco, I.C.N.; Dinato, R.C.; João, S.M.A. Relationships between static foot alignment and dynamic plantar loads in runners with acute and chronic stages of plantar fasciitis: A cross-sectional study. Braz. J. Phys. Ther. 2016, 20, 87–95. [Google Scholar] [CrossRef] [Green Version]
- Cornwall, M.W.; McPoil, T.G. Influence of rearfoot postural alignment on rearfoot motion during walking. Foot 2004, 14, 133–138. [Google Scholar] [CrossRef]
- Carolina, R.B.; Pedro, V.M.M.; Teresa, S.P.; María, R.B.; Francisco, A.T.; Sergio, P.G.; Gabriel, D.M. Relationship of body mass index and footprint morphology to the actual height of the medial longitudinal arch of the foot. Int. J. Environ. Res. Public Health 2021, 18, 9815. [Google Scholar]
- Yu, P.; Liang, M.; Ren, F. Locomotion Variations of Arch Index and Interlimb Symmetry in Shod and Barefoot Populations. Appl. Bionics Biomech. 2020, 2020, 1–5. [Google Scholar] [CrossRef]
- Woźniacka, R.; Oleksy, L.; Jankowicz-Szymanska, A.; Mika, A.; Kielnar, R.; Stolarczyk, A. The association between high-arched feet, plantar pressure distribution and body posture in young women. Sci. Rep. 2019, 9, 17187. [Google Scholar] [CrossRef]
- Wong, P.-L.; Chamari, K.; Mao, D.W.; Wisløff, U.; Hong, Y. Higher plantar pressure on the medial side in four soccer-related movements. Br. J. Sports Med. 2007, 41, 93–100. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Queen, R.M.; Haynes, B.B.; Hardaker, W.M.; Garrett, W.E., Jr. Forefoot loading during 3 athletic tasks. Am. J. Sports Med. 2007, 35, 630–636. [Google Scholar] [CrossRef] [PubMed]
- Sims, E.L.; Hardaker, W.M.; Queen, R.M. Gender differences in plantar loading during three soccer-specific tasks. Br. J. Sports Med. 2008, 42, 272–277. [Google Scholar] [CrossRef] [Green Version]
- Lee, K.T.; Kim, K.C.; Park, Y.U.; Kim, T.W.; Lee, Y.K. Radiographic Evaluation of Foot Structure following Fifth Metatarsal Stress Fracture. Foot Ankle Int. 2011, 32, 796–801. [Google Scholar] [CrossRef] [PubMed]
- Klem, N.-R.; Wild, C.Y.; Williams, S.; Ng, L. Effect of External Ankle Support on Ankle and Knee Biomechanics During the Cutting Maneuver in Basketball Players. Am. J. Sports Med. 2016, 45, 685–691. [Google Scholar] [CrossRef]
- Czerniecki, J.M. Foot and ankle biomechanics in walking and running. A review. Am. J. Phys. Med. Rehabil. 1988, 67, 246–252. [Google Scholar] [PubMed]
- Hasegawa, H.; Yamauchi, T.; Kraemer, W.J. Foot strike patterns of runners at the 15-km point during an elite-level half marathon. J. Strength Cond. Res. 2007, 21, 888–893. [Google Scholar] [PubMed]
- Tourillon, R.; Gojanovic, B.; Fourchet, F. How to Evaluate and Improve Foot Strength in Athletes: An Update. Front. Sports Act. Living 2019, 1. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hughes, R.; Cross, M.; Stokes, K.; Tobin, D.; Power, E.; McNally, S.; Pamment, J. Novel biomechanical injury risk score demonstrates correlation with lower limb posterior chain injury in 50 elite-level rugby union athletes. BMJ Open Sport Exerc. Med. 2021, 7, e001062. [Google Scholar] [CrossRef] [PubMed]
- Hislop, M.D.; Stokes, K.A.; Williams, S.; McKay, C.; England, M.E.; Kemp, S.; Trewartha, G. Reducing musculoskeletal injury and concussion risk in schoolboy rugby players with a pre-activity movement control exercise programme: A cluster randomised controlled trial. Br. J. Sports Med. 2017, 51, 1140–1146. [Google Scholar] [CrossRef]
- Takahashi, S.; Nagano, Y.; Ito, W.; Kido, Y.; Okuwaki, T. A retrospective study of mechanisms of anterior cruciate ligament injuries in high school basketball, handball, judo, soccer, and volleyball. Medicine 2019, 98, e16030. [Google Scholar] [CrossRef]
- Tummala, S.V.; Hartigan, D.E.; Makovicka, J.L.; Patel, K.A.; Chhabra, A. 10-Year Epidemiology of Ankle Injuries in Men’s and Women’s Collegiate Basketball. Orthop. J. Sports Med. 2018, 6. [Google Scholar] [CrossRef] [Green Version]
- Jenkins, W.L.; Killian, C.B.; Williams, D.S., 3rd; Loudon, J.; Raedeke, S.G. Anterior cruciate ligament injury in female and male athletes: The relationship between foot structure and injury. J. Am. Podiatr. Med. Assoc. 2007, 97, 371–376. [Google Scholar] [CrossRef]
- Zedde, P.; Mela, F.; Del Prete, F.; Masia, F.; Manunta, A.F. Meniscal injuries in basketball players. Joints 2015, 2, 192–196. [Google Scholar] [CrossRef]
- Schilaty, N.; Bates, N.; Krych, A.; Hewett, T. How Anterior Cruciate Ligament Injury was averted during Knee Collapse in a NBA Point Guard. Ann. Musculoskelet. Med. 2017, 1, 008–012. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wright, I.; Neptune, R.; Bogert, A.V.D.; Nigg, B. The influence of foot positioning on ankle sprains. J. Biomech. 2000, 33, 513–519. [Google Scholar] [CrossRef] [Green Version]
- Stovitz, S.D.; Coetzee, J.C. Hyperpronation and foot pain: Steps toward pain-free feet. Physician Sportsmed. 2004, 32, 19–26. [Google Scholar] [CrossRef] [PubMed]
- Brockett, C.L.; Chapman, G.J. Biomechanics of the ankle. Orthop. Trauma 2016, 30, 232–238. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jennings, J.; Davies, G.J. Treatment of Cuboid Syndrome Secondary to Lateral Ankle Sprains: A Case Series. J. Orthop. Sports Phys. Ther. 2005, 35, 409–415. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Usgu, S.; Ramazanoğlu, E.; Yakut, Y. The Relation of Body Mass Index to Muscular Viscoelastic Properties in Normal and Overweight Individuals. Medicine 2021, 57, 1022. [Google Scholar] [CrossRef]
| Characteristic | Recreational Group 1 (n = 57) | Elite Group 2 (n = 51) |
|---|---|---|
| Age (years) | 19.6 ± 1.1 | 20.4 ± 1.3 |
| Height (cm) | 172.3 ± 4.4 | 179.0 ± 4.7 * |
| Mass (kg) | 72.1 ± 3.7 | 86.0 ± 5.8 * |
| BMI (m/kg) | 24.3 ± 0.8 | 26.9 ± 1.6 * |
| Rugby training experience (years) | 4.3 ± 1.0 | 5.3 ± 0.9 |
| Recreational Group | Elite Group | p Value 1 | |
|---|---|---|---|
| Left foot | 0.21 ± 0.04 | 0.30 ± 0.05 | 0.039 |
| Right foot | 0.21 ± 0.04 | 0.31 ± 0.05 | 0.033 |
| Region | Recreational Group | Elite Group | p Value 1 |
|---|---|---|---|
| Left foot | |||
| Forefoot (%) | 23.34 ± 6.40 | 25.91 ± 4.37 | <0.01 |
| Midfoot (%) | 9.49 ± 8.43 | 13.16 ± 12.59 | <0.01 |
| Rearfoot (%) | 17.17 ± 5.39 | 10.93 ± 4.10 | 0.058 |
| Right foot | |||
| Forefoot (%) | 23.50 ± 5.74 | 26.23 ± 4.84 | <0.05 |
| Midfoot (%) | 8.34 ± 7.09 | 12.77 ± 12.31 | <0.01 |
| Rearfoot (%) | 18.07 ± 5.41 | 11.00 ± 4.22 | 0.074 |
| Region | Recreational Group | Elite Group | p Value 1 |
|---|---|---|---|
| Left foot | |||
| Forefoot (%) | 25.98 ± 5.24 | 30.91 ± 3.65 | <0.01 |
| Midfoot (%) | 9.82 ± 8.72 | 9.16 ± 8.28 | 0.154 |
| Rearfoot (%) | 14.22 ± 6.95 | 9.94 ± 3.25 | <0.01 |
| Right foot | |||
| Forefoot (%) | 26.04 ± 4.05 | 31.13 ± 3.55 | <0.01 |
| Midfoot (%) | 10.06 ± 9.03 | 8.64 ± 7.92 | 0.200 |
| Rearfoot (%) | 13.91 ± 6.47 | 10.23 ± 3.99 | <0.01 |
| Recreational Group | Elite Group | p Value 1 | |
|---|---|---|---|
| Left foot | 2.48 ± 4.57 | −1.30 ± 5.45 | 0.042 |
| Right foot | 2.25 ± 3.52 | −2.45 ± 5.78 | <0.01 |
| Pain Area | Elite Group (No. [%]) | Pain Area | Elite Group (No. [%]) |
|---|---|---|---|
| Bone pain | Soft-tissue pain | ||
| Foot (Plantar phalanx 1st) | 47 (92.2) | Plantar plate (Abductor hallucis) | 47 (92.2) |
| Foot (Metatarsophalangeal joint 1st & 2nd) | 46 (90.2) | Plantar plate (Abductor digiti minimi) | 47 (92.2) |
| Foot (Plantar metatarsal bone 1st & 2nd) | 46 (90.2) | Medial collateral ligament (MCL) | 36 (70.6) |
| Foot (Metatarsophalangeal joint 4th & 5th) | 43 (84.3) | Lateral collateral ligament (LCL) | 32 (62.7) |
| Foot (Plantar metatarsal bone 4th & 5th) | 43 (84.3) | Anterior cruciate ligament (ACL) | 31 (60.8) |
| Foot (Calcaneus) | 37 (72.5) | Lateral ankle ligament | 27 (52.9) |
| Medial knee joint | 36 (70.6) | Medial ankle ligament | 25 (49.0) |
| Lateral knee joint | 32 (62.7) | Quadriceps femoris | 23 (45.1) |
| Lateral ankle joint | 32 (62.7) | Biceps femoris | 21 (41.2) |
| Patella | 31 (60.8) | Tibialis anterior | 19 (37.3) |
| Medial ankle joint | 25 (49.0) | Gastrocnemius | 19 (37.3) |
| Tibia | 19 (37.3) | Achilles tendon | 18 (35.3) |
| Hip joint | 13 (25.5) | Plantar fascia | 15 (29.4) |
| Others | 6 (11.8) | Lower back | 15 (29.4) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chow, T.-H.; Chen, Y.-S.; Hsu, C.-C.; Hsu, C.-H. Characteristics of Plantar Pressure with Foot Postures and Lower Limb Pain Profiles in Taiwanese College Elite Rugby League Athletes. Int. J. Environ. Res. Public Health 2022, 19, 1158. https://doi.org/10.3390/ijerph19031158
Chow T-H, Chen Y-S, Hsu C-C, Hsu C-H. Characteristics of Plantar Pressure with Foot Postures and Lower Limb Pain Profiles in Taiwanese College Elite Rugby League Athletes. International Journal of Environmental Research and Public Health. 2022; 19(3):1158. https://doi.org/10.3390/ijerph19031158
Chicago/Turabian StyleChow, Tong-Hsien, Yih-Shyuan Chen, Chin-Chia Hsu, and Chin-Hsien Hsu. 2022. "Characteristics of Plantar Pressure with Foot Postures and Lower Limb Pain Profiles in Taiwanese College Elite Rugby League Athletes" International Journal of Environmental Research and Public Health 19, no. 3: 1158. https://doi.org/10.3390/ijerph19031158
APA StyleChow, T.-H., Chen, Y.-S., Hsu, C.-C., & Hsu, C.-H. (2022). Characteristics of Plantar Pressure with Foot Postures and Lower Limb Pain Profiles in Taiwanese College Elite Rugby League Athletes. International Journal of Environmental Research and Public Health, 19(3), 1158. https://doi.org/10.3390/ijerph19031158








