2. Method
The method used in this paper is questionnaire survey, using firsthand data to reveal the inequity in COVID-19. The calculation methods of some core indicators are as follows.
2.1. Measure of Risk of Exposure to COVID-19
In the above formula, the first half of the summation formula calculates the risk of exposure on work days, and the second half represents the risk of exposure on rest days, both of which consist of activity exposure and travel exposure. Among them, : activity venue/coefficient of the environment during travel process, namely indoor/outdoor; : activity venue/coefficient of the number of surrounding people in the travel environment; : coefficient of the mobility of people around the activity venue; represents the length of time residents stay at the activity venue; represents the frequency with which residents engage in a particular activity during work days or rest days; : The mode residents travel to engage in a certain activity; represents the amount of time that residents spend on a certain mode of travel; represents the coefficient of mobility of people in a certain mode of travel; represents the travel frequency, which is the same as the activity frequency in the research.
In the activity section, residents’ exposure risk is measured according to the nature of the environment in the activity, population density, mobility, time of duration, and frequency of activity. According to a study in Korea which compares the COVID-19 risk differences between the indoor activities and the outdoor activities, the risk of becoming COVID-19 infected of indoor activities is 19 times of that of outdoor activities without wearing any masks [
39]. However, the real situation is more complex in Beijing because of the coercive mask-wearing policies. Study have shown that wearing a mask can reduce the risk of COVID-19 infection by 53% [
40]. It is testified that if all the people wear masks, the risk of COVID-19 transmission is only 1.5%, and it rise to 5% when the virus carrier is wearing a mask and other people do not. The risk is 30% if the virus carries does not wear a mask and other people keep wearing the masks [
41]. Due to Beijing’s strict indoor mask-wearing policy, we assume that nearly all people keep wearing masks according to the government’s requirement and only one third of them keep wearing mask outside. Then, in the situation of uncertainty, the weights of the risk of indoor activities and outdoor activities are 1 and 2, respectively. During activity, if mobility of people exists, there is a higher probability of infection, and the value is 2. If there is no mobility of the surrounding people, the risk is low, and the assigned value is 1. Population density and time of duration are assigned by the median value of the option data. In a constantly mobile environment, commuting activity belongs to outdoor environment by default and it has 100% mobility. Based on the actual situation in Beijing, the activity of picking up children belongs to outdoor environment by default, while the dining environment belongs to indoor environment.
In the travel section, residents’ exposure risk is determined by the modes of travel, travel time, nature of the environment, population density, mobility, and frequency. All travel processes are outdoor activities with mobility and are assigned a value of 2. Given the characteristics of COVID-19, the greater the population density, the greater the risk of infection. The number of people gathered around residents varies among different travel modes. About the population density (within a radius of 1.5 m), we conducted field investigation and averaged the data. Under normal circumstances, the population density on the subway is about 4 people; the population density on buses and company shuttle buses is about 3 people. However, commuting activity generally occurs during the morning and evening rush hours. The population density is greater during the ride process compared to other times. At this time, the population density on the subway is 8 people; the population density on buses and company shuttle buses is 6 people. In most cases, there are 2 people in private cars and taxis. The population density is usually 1 person for those who travel by bicycle, on foot, or by electric bicycle. The median value of the option data is directly taken as the calculation criteria for other factors such as travel time and frequency.
2.2. Measure of Inequity
Firstly, a concise statistical table is used to group the amount of COVID-19 exposure by demographic characteristics to present the distribution of the exposure risk of COVID-19 among different populations in the form of mean values, which reveals the characteristics of population differences. Secondly, the coefficient of variation, namely standard deviation/mean value, is used to reveal the specific status of inequity of COVID-19 exposure. In this section, we will calculate the coefficients of variation for the overall population, different demographic characteristics (gender, age), work days/rest days, and different activity types, respectively.
The formula of coefficient of variation is:
2.3. Data Collection
According to the purpose of the study, we designed a structured questionnaire to collect data about daily activities of Beijing residents including those who live, work or study in Beijing.
The questionnaire mainly includes four parts: (1) demographic characteristics of residents, including gender, age, education level, marital status, occupation, income, hukou (hukou is a system of household registration used in China. A household registration record officially identifies a person as a permanent resident of an area and includes identifying information such as name, birthplace, gender. There are two types of Hukou: agricultural hukou and non-agricultural hukou), ownership of the house, family structure. (2) Residents’ activity types. In the survey, we divided the time of a week into Monday to Friday (work days) and Saturday to Sunday (rest days), and collected information related to residents’ activities from the above two dimensions. We analyzed the two parts separately. Residents’ daily activities are mainly divided into 8 types, including commuting, dining out, work, personal affairs, shopping, picking up kids, leisure, socializing. In addition, on rest days, home activities were added to the questionnaire to reflect the real-life status of residents. Although home activities can reflect the activity status of residents, they are not outdoor activities and will not be considered in the later calculation. (3) Systematic characteristics of activities. Systematic characteristics of activities include activity time, location, activity environment (indoor or outdoor, population density, personnel mobility), activity duration and activity frequency. (4) Systematic characteristics of travel. In this study, travel originates from activity needs, so travel system belongs to activity system. The systematic characteristics of travel include travel time, travel mode and travel duration. The frequency of travel is consistent with the frequency of activity. It should be noted that travel environment (indoor or outdoor, population density, mobility) and other data were not asked in the questionnaire but were obtained through practical tests and common sense.
We conducted questionnaires in November 2020 by both online interview and onsite interview. There are 756 interviewees, and finally, 754 valid questionnaires were obtained.
In terms of the number of questionnaires issued, we took the proportion of residents’ occupation distribution as a reference standard. From the Beijing Statistical Yearbook, the National Bureau of Statistics and relevant literature, we found information on the number of civil servants, employees in public institutions, employees in state-owned enterprises, employees in private enterprises, employees in foreign enterprises, individual business, freelancer, students, farmers, unemployed in Beijing in 2018 [
42,
43]. Based on the above data, we can obtain the proportion distribution of Beijing residents in these occupations. as According to the reference standard, we found the target population in proportion for targeted distribution and collection of questionnaires.
2.4. Sample Characteristics
Descriptive statistics of the sample are shown in
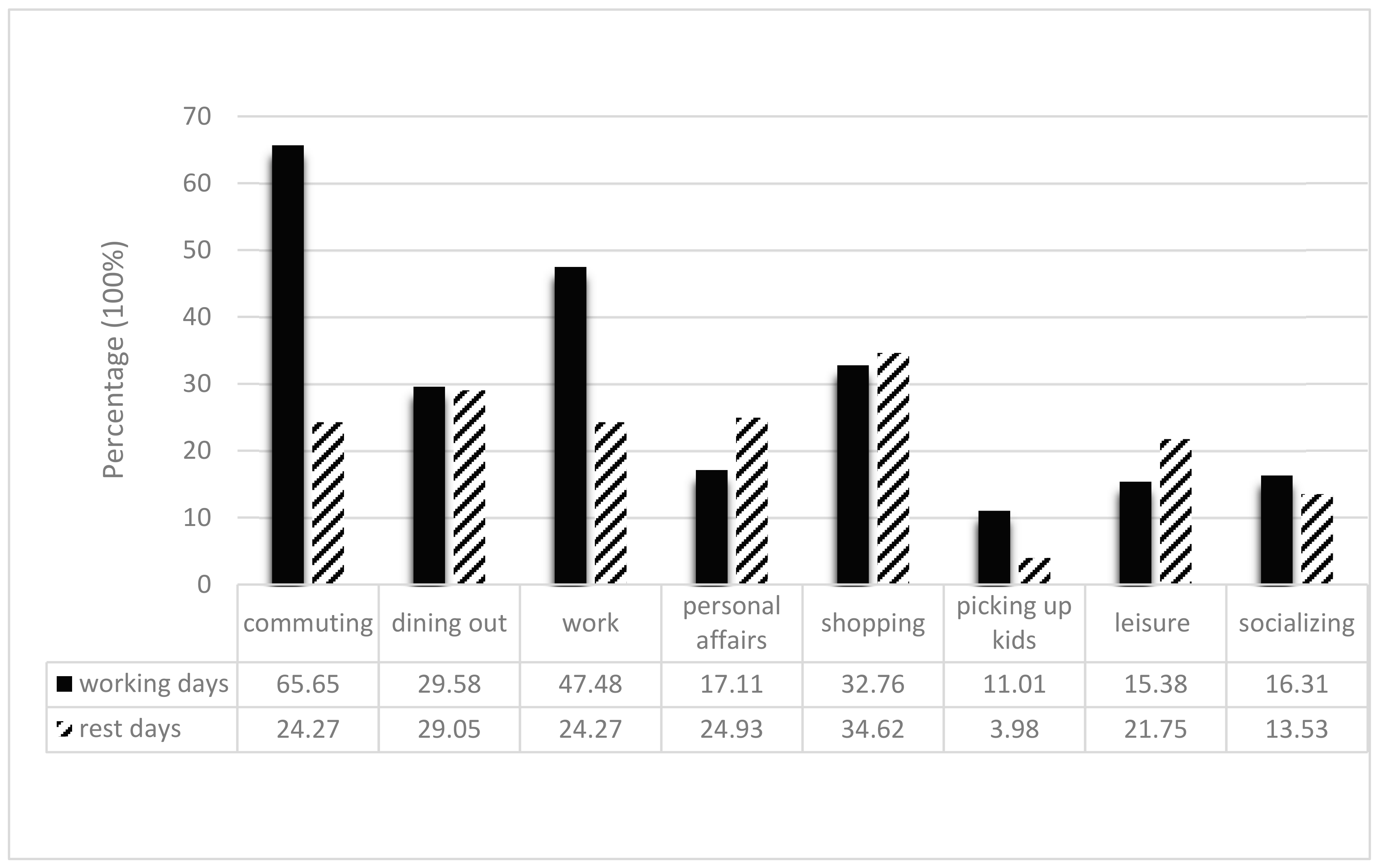
Table 1. The activity types of residents are shown in
Figure 1. Commuting and work are the primary activities of residents on work days. Life activities such as shopping, dining out and personal affairs are the main contents of the rest days.
4. Discussion
It is self-evident that the risks of exposure to COVID-19 are different for different activities and days. However, whether people with different social characteristics are at different risks of exposure to COVID-19 and the health inequities behind these differences are worth discussing.
Studies have shown that vulnerable groups, ethnic minorities and other groups in society have higher infection rates, less medical assistance and higher mortality rates after contracting COVID-19 [
26,
27,
28,
29,
30,
31,
32]. Studies have also shown that these vulnerable and minority groups are hardest hit by COVID-19 [
33,
34]. This inequality is not a matter of chance. This structural inequality has caused widespread concern, and more and more people are calling for attention to these groups. That is, existing studies have focused strongly on pre- and post-infection inequalities. Now, our research shows that going back a step further, there are also some groups that are relatively at higher risk in terms of exposure. However, the groups at higher risk of COVID-19 exposure are different from these studies: they are not traditionally vulnerable groups.
On the whole, different groups of people demonstrate different activity patterns, leading to different exposure levels. However, when it comes to a specific influencing mechanism, the logic behind it needs further explanation.
People with higher education had higher levels of exposure risk than those with less than a junior high school education. Research showed that education level is negatively correlated with fear of being infected, which is consistent with our results to some extent [
45,
46]. The higher the level of education, the lower the fear of infection and the less likely they are to be afraid to go out, leading to a relatively high level of exposure. Coincidentally, some research demonstrates that education level is also positively correlated with the risk of COVID-19 infection [
47]. That is, highly educated people are at a higher risk for both exposure and infection. However, a study pointed out that the higher the education level, the lower the actual infection rate [
48]. A study also pointed out that the lower the education level, the higher the mortality rate of people infected with COVID-19 [
49]. In addition, regarding the “side effects” of COVID-19, people with higher education levels also suffered fewer shocks (such as unemployment) [
50], than people with lower education levels. These studies show that while people with more education are at higher risk of exposure and infection, this risk does not translate into reality impact. It is those with less education who suffer more infections, deaths and unemployment.
In terms of occupation, students are more exposed than civil servants. On the one hand, students are always aggregated in the classrooms with close contacts. On the other hand, it can be seen from our research that students’ frequent outdoor activities are an important reason for their high exposure risk. The reason for the large number of student activities is that students are more flexible in time arrangement and have higher social needs with their peers due to their attributes as young people. Other research points out that an important reason for the high risk of COVID-19 exposure among young people is that they think it will be fine to contact COVID-19 [
51]. A cavalier attitude to the dangers of COVID-19 puts them at higher risk of exposure.
In terms of income, compared with the group with the monthly income ≤2000 yuan, the exposure risk of the group with the monthly income ≥30,001 yuan was higher (p < 0.01). The possible reason lies in the diversity of activities: the number of activities of people with a monthly income of more than 30,001 yuan is much higher than that of people with a monthly income of less than 2000 yuan.
Interestingly, Boyeong et al.’s measurements of COVID-19 exposure in US communities are the exact opposite of our results: Affluent neighborhoods in the United States have the lowest exposure, because in addition to being able to reduce contact by moving to a second home in the suburbs, residents in these neighborhoods have the option of working remotely. Poor minority communities are at greater risk of exposure because they tend to work in basic service jobs where the need to survive prevents them from strictly enforcing government’s stay-at-home orders [
52]. The reason for the completely opposite results of the empirical studies in the two countries may be that the socioeconomic context and the definition of high-income groups are different. Boyeong et al.’s basic analyzing unit is the community, whereas ours is the individual. The American high income groups belongs to wealthy neighborhoods and live far away from the poor ones. The situation is totally different in the megacity in China. In addition, residents’ living habit and activity features of different social groups in China are also different from that of the American residents. We found a robust result even when we applied different weights during the calculations. It may be because most of the respondents’ activities are indoors in the megacity, and the proportion of indoor activities overweight the outdoor activities. Besides, this paper aims to explore the relative differences of exposure risks among respondents, and both CVs of different scenarios are larger than 1, which means great diversity of different social groups. The comparative result is not hampered based on different weights analysis.
Compared to existing literature, this study makes contributions in the following aspects: first, most studies aggregated on the research of infection rate and death rate of COVID-19 and other types of epidemics. This research explores the risk of exposure to COVID-19 under the condition of uncertainty and analyzes the impact of different individuals’ activities and social characteristics on their exposure to COVID-19. Second, existing studies usually focus on particular groups of people such as medical staffs and the infected people, and the general public under the risk of becoming infected are paid less attention. This study focuses on the general public and reveals the COVID-19 exposure risk of general public during their different activities at different time. Third, studies on the inequality of COVID-19 or other epidemics are less, this study measures the inequality of the risk of exposure to COVID-19 in and between different social groups, which could enlighten the governments to take effective measures to reduce the infection rate from the perspective of exposure risk.
However, there are still some limitations in this paper. First, although the professional structure of Beijing residents was considered in the design and collection of questionnaires, the questionnaires number was still small in general. Second, based on Beijing’s compulsive “wear a mask” policy, we calculate the exposure risks on the assumption that nearly everyone took strict self-protection measures and wore masks correctly indoors and one third of people also wore masks outside. Different compliance rates of wearing masks indoors and outdoors could lead to different sets of weights which would lead to different values of exposure risks. Although the conclusions of influencing factors of COVID-19 and inequity under uncertainty are robust, there are inevitable value deviations. It needs further and deeper exploration under different circumstances. Lastly, the factors affecting individuals’ exposure risk of COVID-19 in this paper are not fully considered. People with poor immunity and basic diseases are susceptible and have higher chance of becoming infected, when compared with other people, even if they are exposed in the same situation. In the external environment, the spread of the new coronavirus will be affected by meteorological factors such as temperature and humidity [
53]. However, in this study, we did not consider individual health condition and the impact of external environmental factors on the exposure levels. The deficiencies of this study also provide a direction for further research.
5. Conclusions
5.1. Differences in Exposure Risk among Activities
Affected by time and frequency, the exposure risk of each activity is different. First, the exposure risk was always highest for work activities, regardless of the frequency of activity. Second, regardless of the frequency of activity, low-exposure activities, such as dining out, commuting, and picking up kids, did not differ much between weekdays and rest days. Leisure, personal affairs, and socializing are activities with high exposure risk, and the exposure risk is higher on work days than on rest days. Finally, after considering the frequency of activity, dining out, commuting, and picking up kids ranked significantly higher on work days, while leisure, personal affairs and socializing ranked lower.
In terms of the total exposure risk within one week, the exposure risk of subsistence activities was the highest, the exposure risk of living activities was in the middle, and the exposure risk of leisure activities was relatively the lowest. Specifically, the exposure risks of these eight activities in one week, in descending order, are: work, commuting, dining out, picking up children, leisure, personal affairs, life and shopping, and social contact.
5.2. Differences in Exposure Risk among Social Groups
Education level, occupation and income passed the statistical test and showed significant differences of COVID-19 exposure risks. In terms of the education level, residents with master’s degree or above have the highest exposure risk, followed by those with bachelor’s degree. People with a junior high school education or less had the lowest exposure risk. In terms of occupational types, the exposure risk of students is the highest. As for the income level, residents with a monthly income of more than 30,001 yuan had the greatest exposure risk, followed by those with a monthly income of 10,001–15,000 yuan.
5.3. Inequality of Exposure Risk
The coefficients of variation of exposure risk of the whole sample under two scenarios are 1.46 and 1.49, indicating that diversities in exposure risk among residents and health inequity existed. The health inequities are higher on weekdays than on rest days. In terms of activity type, work presents the highest degree of health inequality. This is because each job varies greatly in its working environment, requirements, working hours, population density and mobility. In addition, other activities also present great differences of the exposure risks, expect for the dining out activity.
Health inequalities also exist within groups of different socioeconomic status. The social groups, characterized as male, 31~40 ages, with a high school education degree, married, non-local agricultural hukou, renting houses, farmers, working in private enterprises, income more than 30,001 yuan, are demonstrating higher inequity within the group with larger coefficients of variation of exposure risk. As for people with the same attribute, we have sketched out a portrait of a person who is suffering from the highest level of health inequality within the group: male, 31–40 years old, married, with a rural hukou, rented housing, farmers, three generations of cohabitation.