The Effects of COVID-19 Lockdown on Glycaemic Control and Lipid Profile in Patients with Type 2 Diabetes: A Systematic Review and Meta-Analysis
Abstract
:1. Introduction
1.1. Description of COVID-19 and Its Lockdown
1.2. How COVID-19 and Its Lockdown May Affect Patients with Diabetes
1.3. Why It Is Important to Do the Review
1.4. Aim
2. Methods
2.1. Types of Studies
2.2. Types of Participants
2.3. Types of Exposure
2.4. The Inclusion Criteria
2.5. The Exclusion Criteria
2.5.1. Types of Outcome Measures
- Blood Glucose Parameters: Glycated haemoglobin (HbA1c, %);
- Lipid parameters: high-density lipoprotein (HDL mg/dL) cholesterol, total cholesterol (mmol/L), low-density lipoprotein (LDL mmol/L) cholesterol, triglycerides (mmol/L);
- Body mass index (BMI) (kg/m2).
2.5.2. Secondary Outcome Measures of Interest
- Fasting Blood Glucose (FBG mg/dL);
- Postprandial Blood Glucose (mg/dL).
2.6. Search Methods for Identification of Studies
3. Data Collection and Analysis
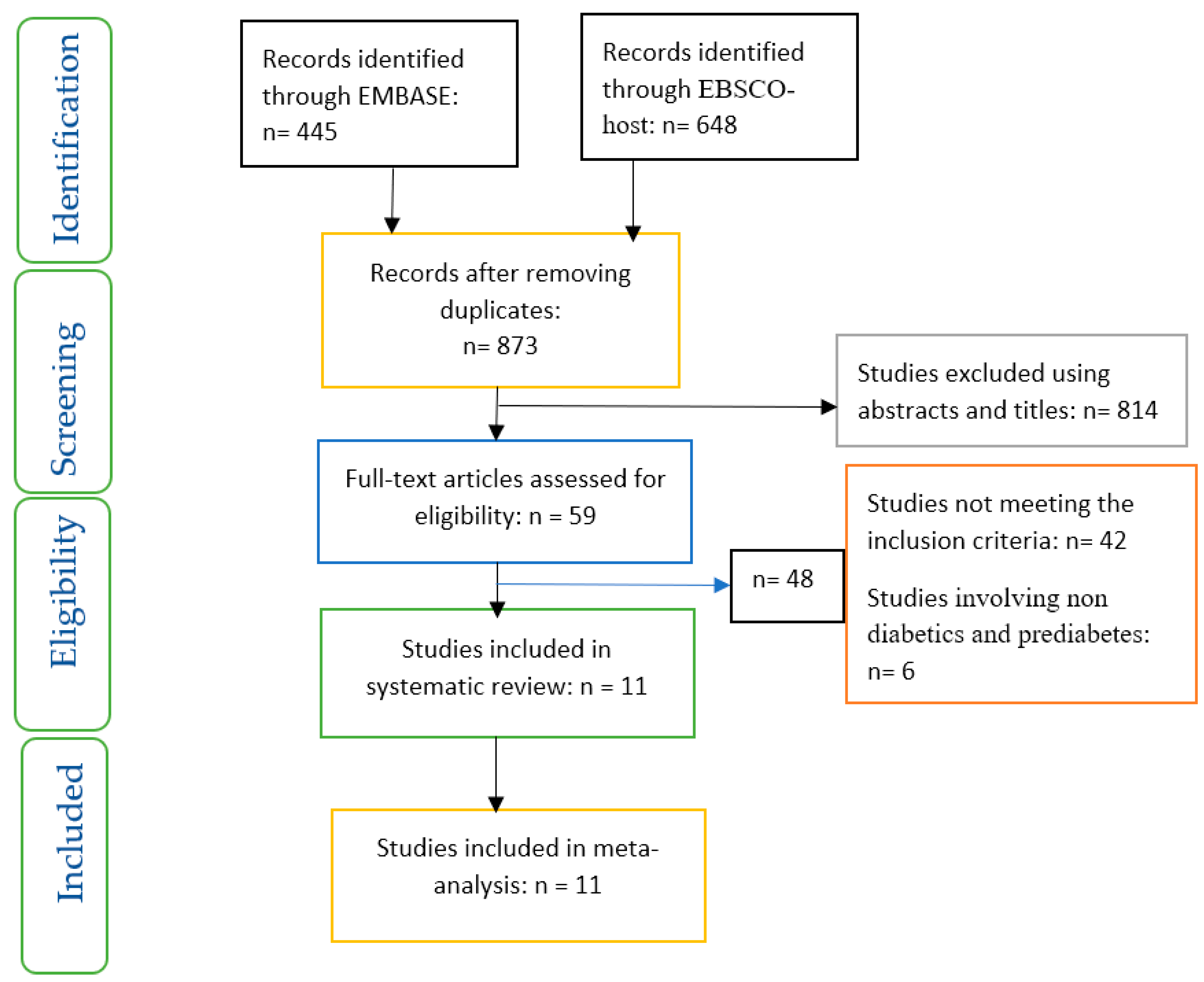
3.1. Selection of Studies
3.2. Data Extraction and Management
3.3. Data Analysis
4. Results
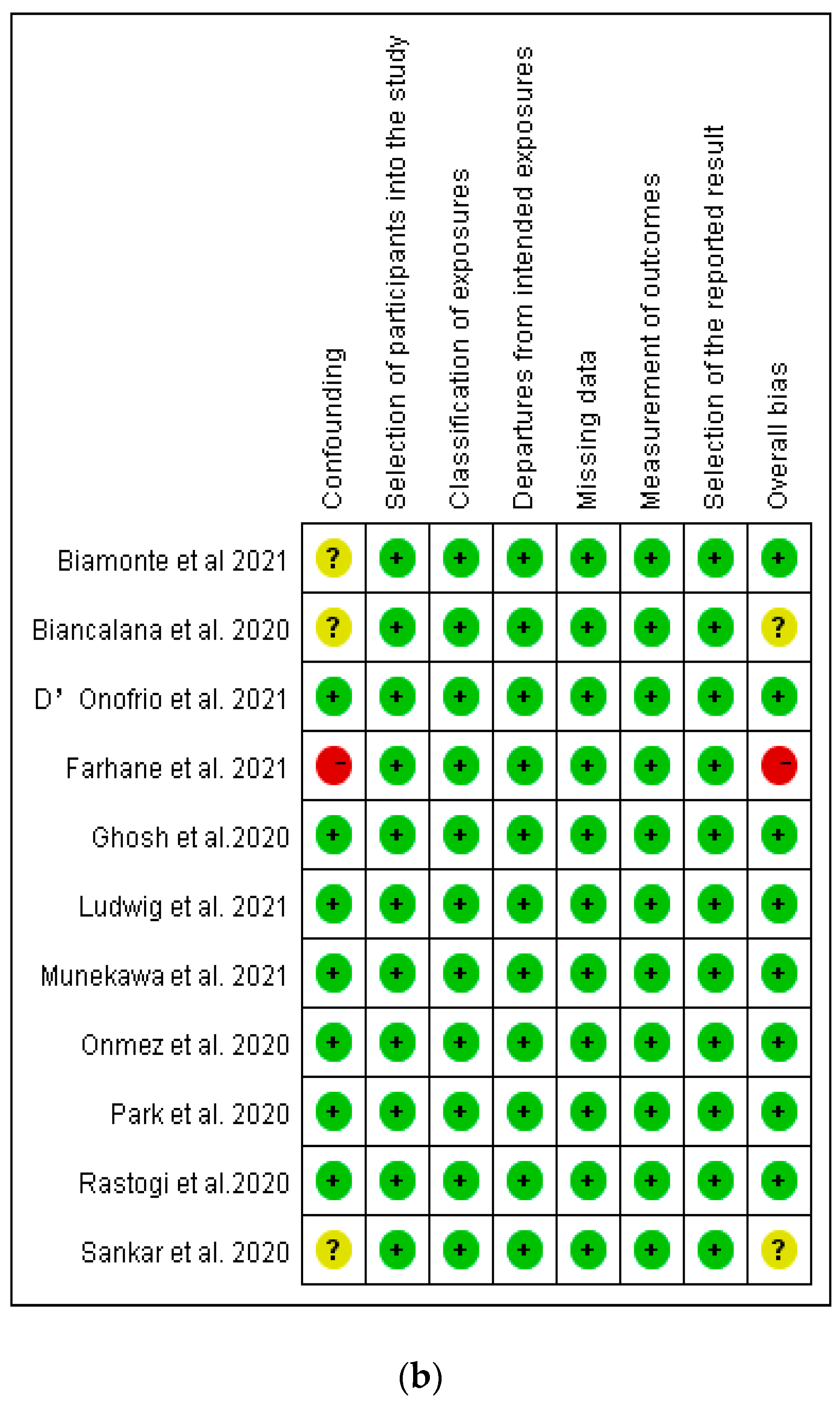
4.1. Assessment of Risk of Bias in Included Studies
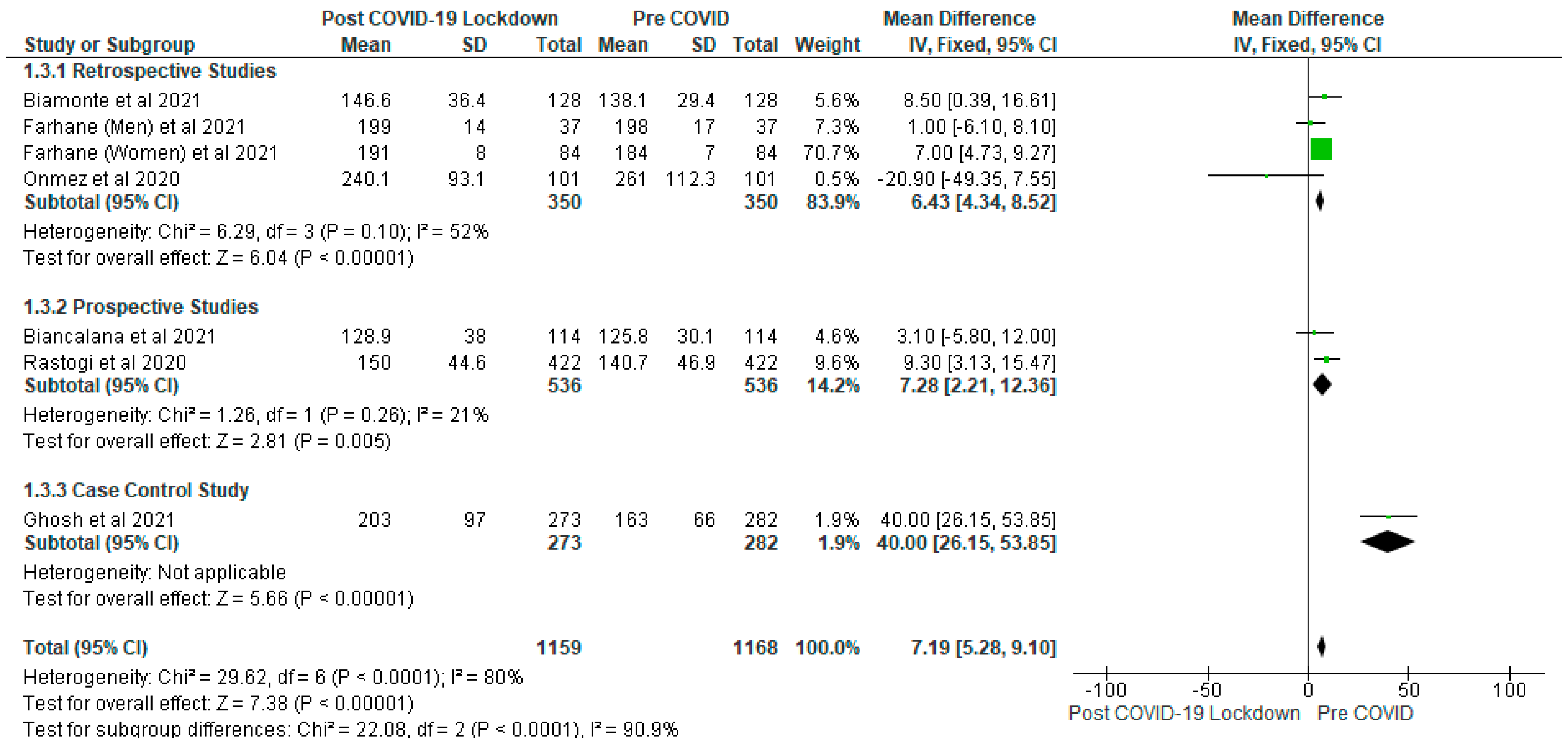
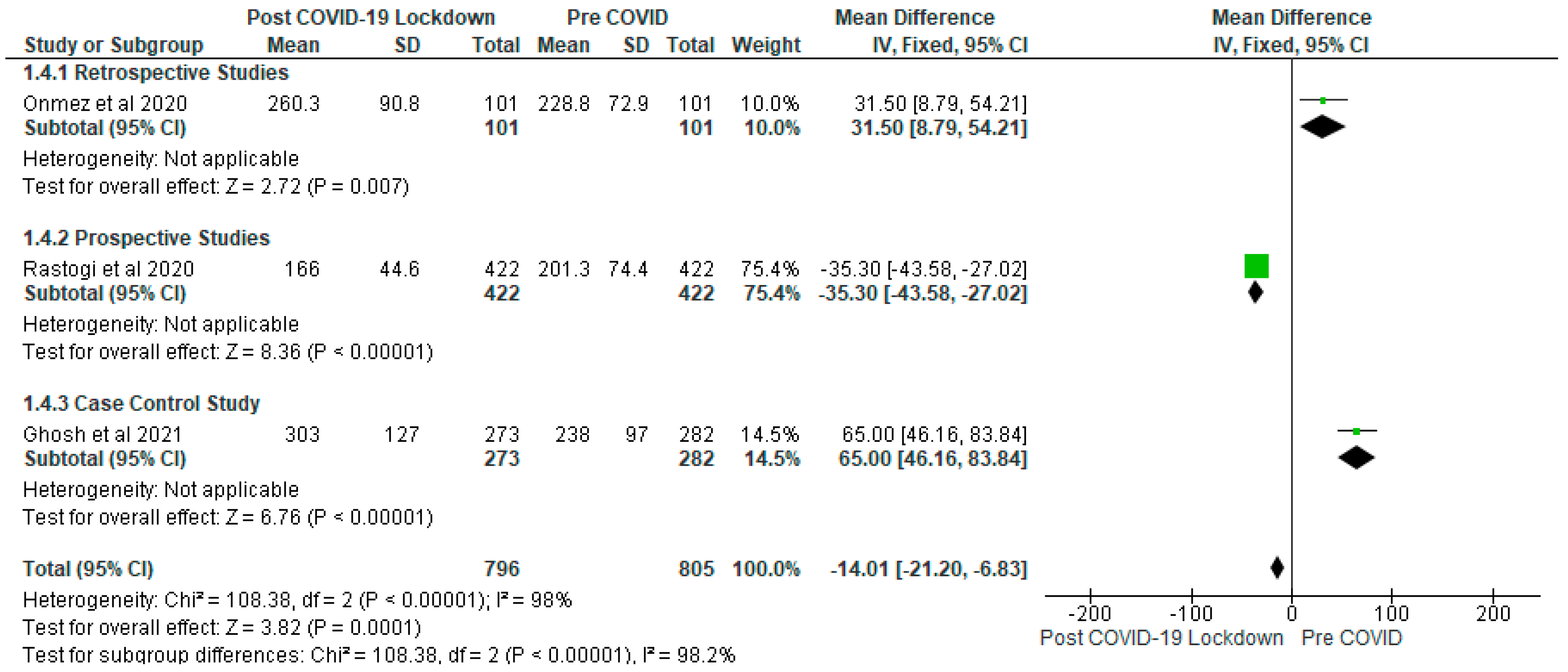
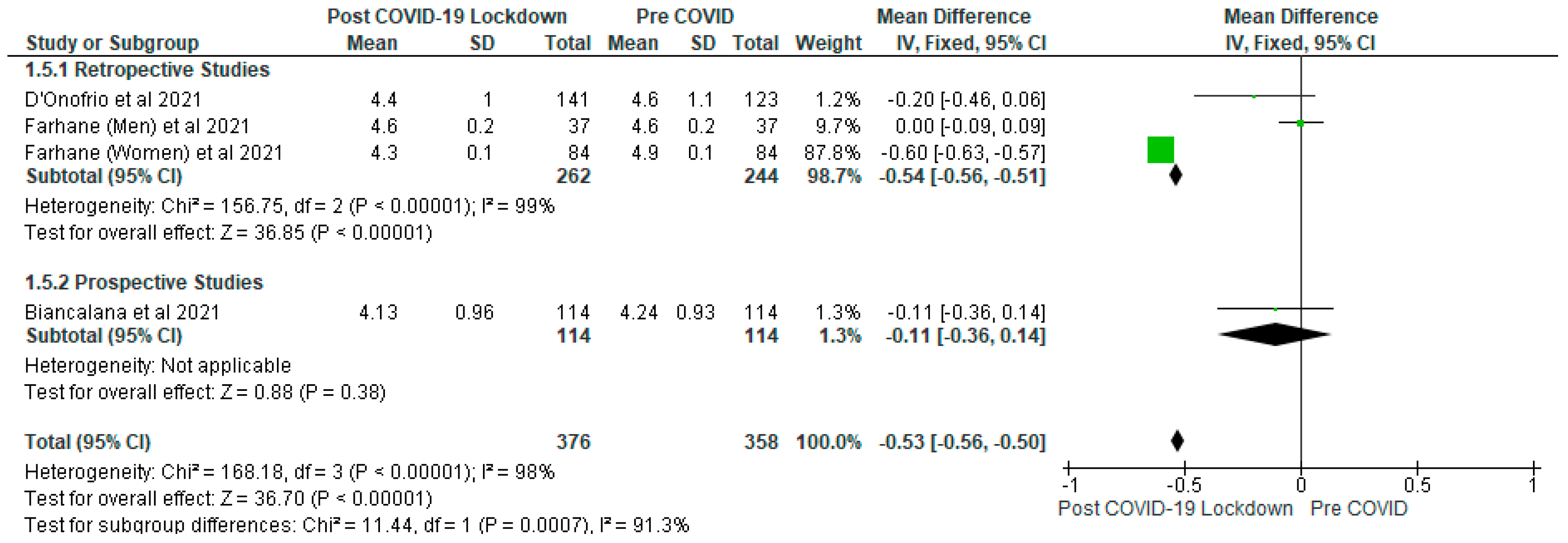
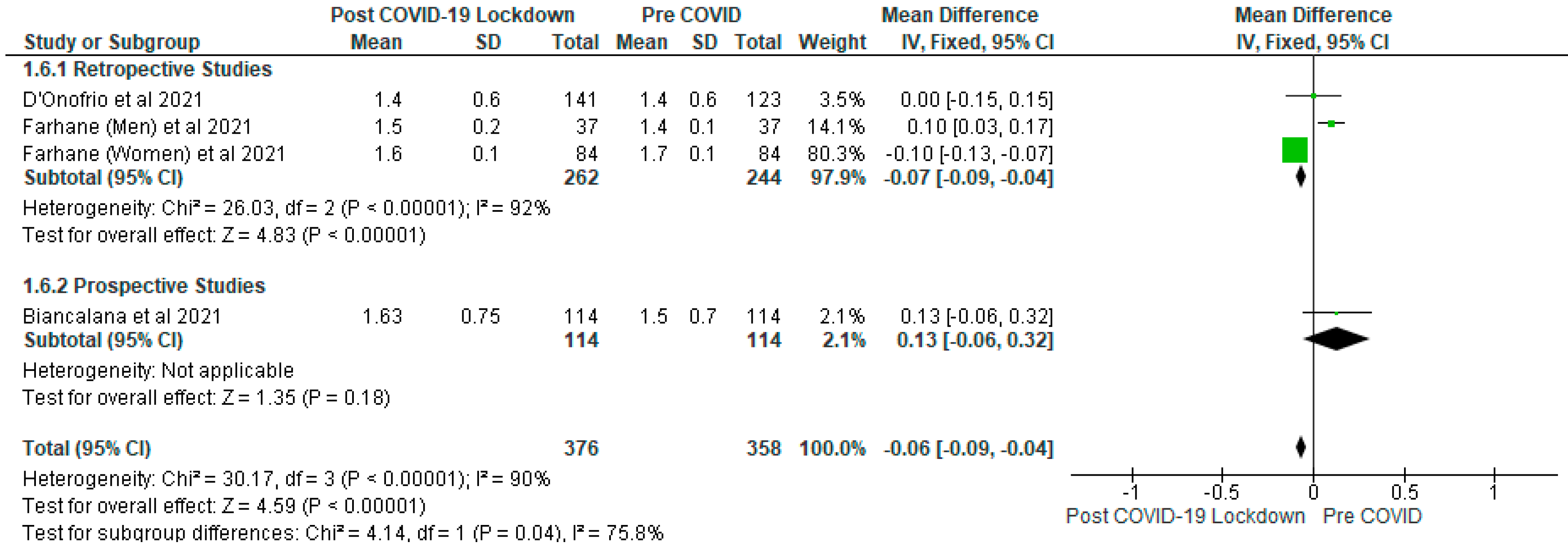
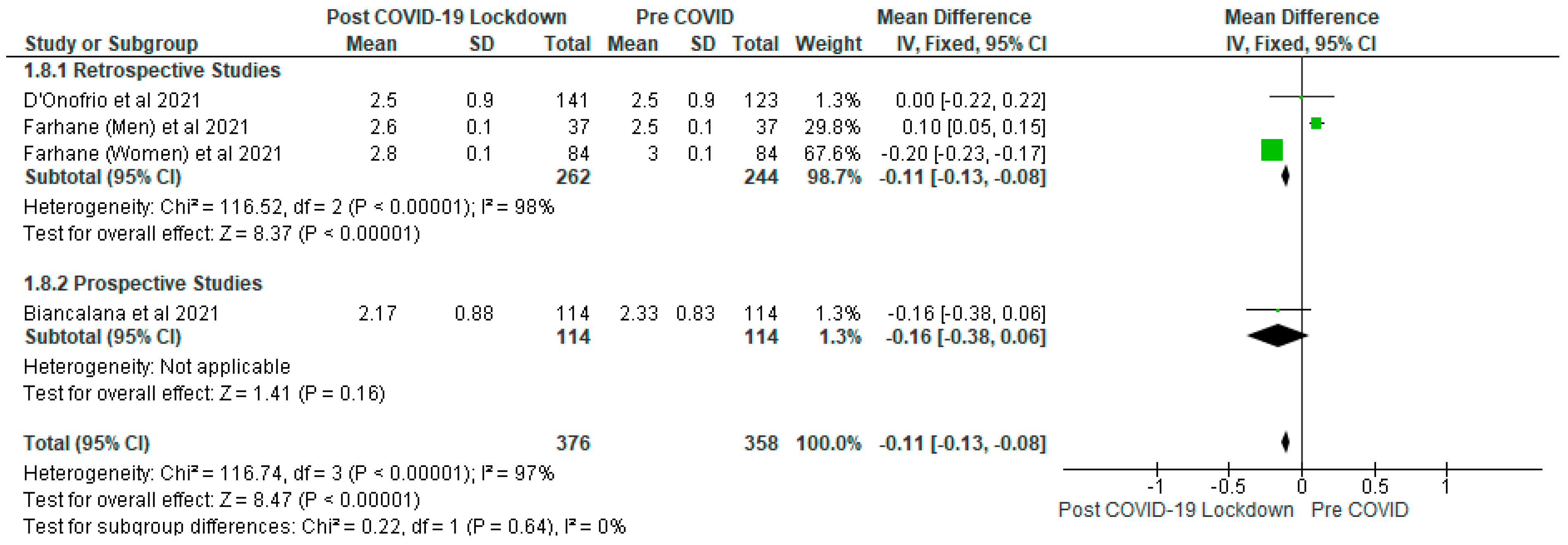
4.2. Glycaemic Control
4.3. Lipid Parameters
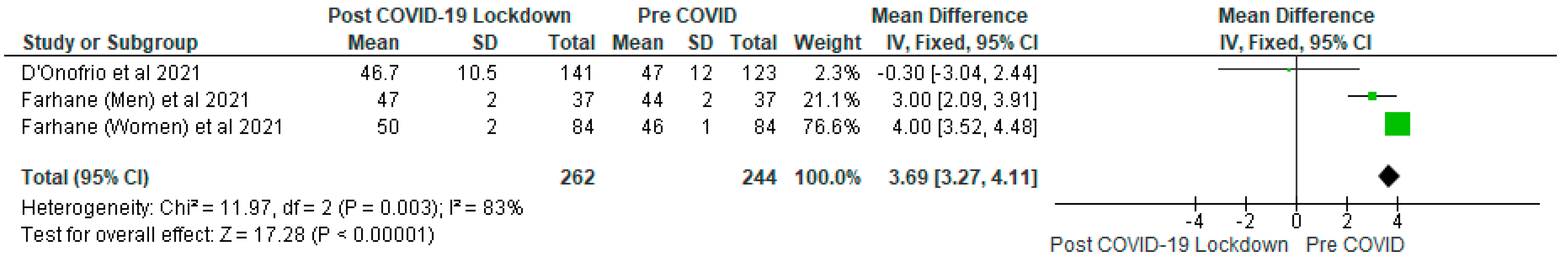
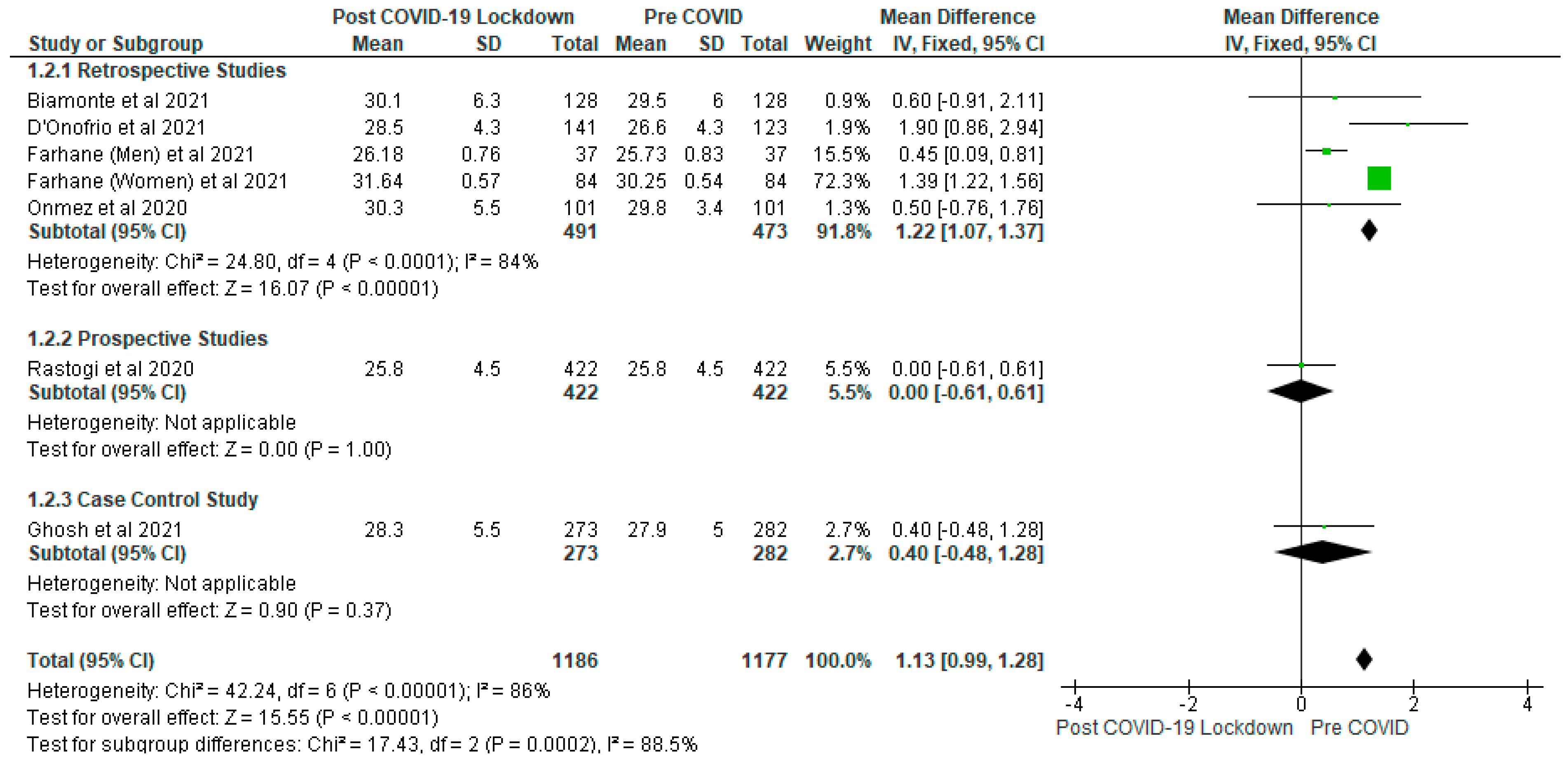
4.4. Body Mass Index (BMI)
5. Discussion
6. Limitations
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Viswanathan, V.; Puvvula, A.; Jamthikar, A.D.; Saba, L.; Johri, A.M.; Kotsis, V.; Khanna, N.N.; Dhanjil, S.K.; Majhail, M.; Misra, D.P.; et al. Bidirectional link between diabetes mellitus and coronavirus disease 2019 leading to cardiovascular disease: A narrative review. World J. Diabetes 2021, 12, 215–237. [Google Scholar] [CrossRef]
- Caron, R.M.; Adegboye, A.R.A. COVID-19: A syndemic requiring an integrated approach for marginalized populations. Front. Public Health 2021, 9, 675280. [Google Scholar] [CrossRef]
- Papadokostaki, E.; Tentolouris, N.; Liberopoulos, E. COVID-19 and diabetes: What does the clinician need to know? Prim. Care Diabetes 2020, 14, 558–563. [Google Scholar] [CrossRef]
- Bambra, C.; Riordan, R.; Ford, J.; Matthews, F. The COVID-19 pandemic and health inequalities. J. Epidemiol. Community Health 2020, 74, 964–968. [Google Scholar] [CrossRef] [PubMed]
- Vas, P.; Hopkins, D.; Feher, M.; Rubino, F.; Whyte, M. Diabetes, obesity and COVID-19: A complex interplay. Diabetes Obes. Metab. 2020, 22, 1892–1896. [Google Scholar] [CrossRef]
- Sathish, T.; Tapp, R.J.; Cooper, M.E.; Zimmet, P. Potential metabolic and inflammatory pathways between COVID-19 and new-onset diabetes. Diabetes Metab. 2021, 47, 101204. [Google Scholar] [CrossRef] [PubMed]
- International Diabetes Federation. Promoting Diabetes Care, Prevention and a Cure Worldwide. 2019. Available online: https://www.diabetesatlas.org/upload/resources/material/20200302_133351_IDFATLAS9e-final-web.pdf (accessed on 23 August 2021).
- Li, H.; Tian, S.; Chen, T.; Cui, Z.; Shi, N.; Zhong, X.; Qiu, K.; Zhang, J.; Zeng, T.; Chen, L.; et al. Newly diagnosed diabetes is associated with a higher risk of mortality than known diabetes in hospitalized patients with COVID-19. Diabetes Obes. Metab. 2020, 22, 1897–1906. [Google Scholar] [CrossRef] [PubMed]
- Farhane, H.; Motrane, M.; Anaibar, F.-E.; Motrane, A.; Abeid, S.N.; Harich, N. COVID-19 pandemic: Effects of national lockdown on the state of health of patients with type 2 diabetes mellitus in a Moroccan population. Prim. Care Diabetes 2021, 15, 772–777. [Google Scholar] [CrossRef]
- Santos, A.; Magro, D.O.; Evangelista-Poderoso, R.; Saad, M.J.A. Diabetes, obesity, and insulin resistance in COVID-19: Molecular interrelationship and therapeutic implications. Diabetol. Metab. Syndr. 2021, 13, 23. [Google Scholar] [CrossRef] [PubMed]
- Ruissen, M.M.; Regeer, H.; Landstra, C.P.; Schroijen, M.; Jazet, I.; Nijhoff, M.F.; Pijl, H.; Ballieux, B.E.P.B.; Dekkers, O.; Huisman, S.D.; et al. Increased stress, weight gain and less exercise in relation to glycemic control in people with type 1 and type 2 diabetes during the COVID-19 pandemic. BMJ Open Diabetes Res. Care 2021, 9, e002035. [Google Scholar] [CrossRef]
- Takahara, M.; Watanabe, H.; Shiraiwa, T.; Maeno, Y.; Yamamoto, K.; Shiraiwa, Y.; Yoshida, Y.; Nishioka, N.; Katakami, N.; Shimomura, I. Lifestyle changes and their impact on glycemic control and weight control in patients with diabetes during the pandemic of coronavirus disease 2019 in Japan. J. Diabetes Investig. 2021, 1. [Google Scholar] [CrossRef] [PubMed]
- Fernández, E.; Cortazar, A.; Bellido, V. Impact of COVID-19 lockdown on glycemic control in patients with type 1 diabetes. Diabetes Res. Clin. Pract. 2020, 166, 108348. [Google Scholar] [CrossRef] [PubMed]
- D’Onofrio, L.; Pieralice, S.; Maddaloni, E.; Mignogna, C.; Sterpetti, S.; Coraggio, L.; Luordi, C.; Guarisco, G.; Leto, G.; Leonetti, F.; et al. Effects of the COVID-19 lockdown on glycaemic control in subjects with type 2 diabetes: The glycalock study. Diabetes Obes. Metab. 2021, 23, 1624–1630. [Google Scholar] [CrossRef]
- Chen, J.; Wu, C.; Wang, X.; Yu, J.; Sun, Z. The impact of COVID-19 on blood glucose: A Systematic review and meta-analysis. Front. Endocrinol. 2020, 11, 574541. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Wang, X.; Chen, J.; Zuo, X.; Zhang, H.; Deng, A. COVID-19 infection may cause ketosis and ketoacidosis. Diabetes Obes. Metab. 2020, 22, 1935–1941. [Google Scholar] [CrossRef]
- Silverii, G.A.; Poggi, C.D.; Dicembrini, I.; Monami, M.; Mannucci, E. Glucose control in diabetes during home confinement for the first pandemic wave of COVID-19: A meta-analysis of observational studies. Acta Diabetol. 2021, 58, 1603–1611. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Ann. Intern. Med. 2009, 151, 264–269. [Google Scholar] [CrossRef] [Green Version]
- Higgins, J.P.T.; Green, S. Cochrane Handbook for Systematic Reviews of Interventions; Wiley-Blackwell: Hoboken, NJ, USA, 2009; p. 31. [Google Scholar]
- The Nordic Cochrane Centre. Review Manager, Version 5.3; The Cochrane Collaboration: Copenhagen, Denmark, 2014. [Google Scholar]
- Ghosh, A.; Anjana, R.M.; Rani, C.S.S.; Rani, S.J.; Gupta, R.; Jha, A.; Gupta, V.; Kuchay, M.S.; Luthra, A.; Durrani, S.; et al. Glycemic parameters in patients with new-onset diabetes during COVID-19 pandemic are more severe than in patients with new-onset diabetes before the pandemic: NOD COVID India Study. Diabetes Metab. Syndr. Clin. Res. Rev. 2021, 15, 215–220. [Google Scholar] [CrossRef]
- Biamonte, E.; Pegoraro, F.; Carrone, F.; Facchi, I.; Favacchio, G.; Lania, A.G.; Mazziotti, G.; Mirani, M. Weight change and glycemic control in type 2 diabetes patients during COVID-19 pandemic: The lockdown effect. Endocrine 2021, 72, 604–610. [Google Scholar] [CrossRef]
- Biancalana, E.; Parolini, F.; Mengozzi, A.; Solini, A. Short-term impact of COVID-19 lockdown on metabolic control of patients with well-controlled type 2 diabetes: A single-centre observational study. Acta Diabetol. 2021, 58, 431–436. [Google Scholar] [CrossRef]
- Ludwig, L.; Scheyer, N.; Remen, T.; Guerci, B. The impact of COVID-19 lockdown on metabolic control and access to healthcare in people with diabetes: The CONFI-DIAB cross-sectional study. Diabetes Ther. 2021, 12, 2207–2221. [Google Scholar] [CrossRef]
- Munekawa, C.; Hosomi, Y.; Hashimoto, Y.; Okamura, T.; Takahashi, F.; Kawano, R.; Nakajima, H.; Osaka, T.; Okada, H.; Majima, S.; et al. Effect of coronavirus disease 2019 pandemic on the lifestyle and glycemic control in patients with type 2 diabetes: A cross-section and retrospective cohort study. Endocr. J. 2021, 68, 201–210. [Google Scholar] [CrossRef]
- Önmez, A.; Gamsızkan, Z.; Özdemir, Ş.; Kesikbaş, E.; Gökosmanoğlu, F.; Torun, S.; Cinemre, H. The effect of COVID-19 lockdown on glycemic control in patients with type 2 diabetes mellitus in Turkey. Diabetes Metab. Syndr. Clin. Res. Rev. 2020, 14, 1963–1966. [Google Scholar] [CrossRef] [PubMed]
- Park, S.-D.; Kim, S.-W.; Moon, J.S.; Lee, Y.Y.; Cho, N.H.; Lee, J.-H.; Jeon, J.-H.; Choi, Y.-K.; Kim, M.K.; Park, K.-G. Impact of social distancing due to coronavirus disease 2019 on the changes in glycosylated hemoglobin level in people with type 2 diabetes mellitus. Diabetes Metab. J. 2021, 45, 109–114. [Google Scholar] [CrossRef] [PubMed]
- Rastogi, A.; Hiteshi, P.; Bhansali, A. Improved glycemic control amongst people with long-standing diabetes during COVID-19 lockdown: A prospective, observational, nested cohort study. Int. J. Diabetes Dev. Ctries. 2020, 40, 476–481. [Google Scholar] [CrossRef] [PubMed]
- Sankar, P.; Ahmed, W.N.; Koshy, V.M.; Jacob, R.; Sasidharan, S. Effects of COVID-19 lockdown on type 2 diabetes, lifestyle and psychosocial health: A hospital-based cross-sectional survey from South India. Diabetes Metab. Syndr. Clin. Res. Rev. 2020, 14, 1815–1819. [Google Scholar] [CrossRef]
- Bristol.ac.uk. Preliminary Tool for Risk of Bias in Exposure Studies. 2021. Available online: https://www.bristol.ac.uk/media-library/sites/social-community-medicine/images/centres/cresyda/Risk_of_bias_preliminary_for_exposures_template_Jul2017.pdf (accessed on 7 December 2021).
- Eberle, C.; Stichling, S. Impact of COVID-19 lockdown on glycemic control in patients with type 1 and type 2 diabetes mellitus: A systematic review. Diabetol. Metab. Syndr. 2021, 13, 95. [Google Scholar] [CrossRef]
- Hosomi, Y.; Munekawa, C.; Hashimoto, Y.; Okamura, T.; Takahashi, F.; Kawano, R.; Nakajima, H.; Majima, S.; Senmaru, T.; Nakanishi, N.; et al. The effect of COVID-19 pandemic on the lifestyle and glycemic control in patients with type 1 diabetes: A retrospective cohort study. Diabetol. Int. 2021, 13, 85–90. [Google Scholar] [CrossRef] [PubMed]
- Hardy, O.T.; Czech, M.P.; Corvera, S. What causes the insulin resistance underlying obesity? Curr. Opin. Endocrinol. Diabetes Obes. 2012, 19, 81–87. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gulve, E.A. Exercise and glycemic control in diabetes: Benefits, challenges, and adjustments to pharmacotherapy. Phys. Ther. 2008, 88, 1297–1321. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Colberg, S.R.; Sigal, R.J.; Fernhall, B.; Regensteiner, J.G.; Blissmer, B.J.; Rubin, R.R.; Chasan-Taber, L.; Albright, A.L.; Braun, B. Exercise and type 2 diabetes: The American college of sports medicine and the American diabetes association: Joint position statement. Diabetes Care 2010, 33, e147–e167. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dunning, T. Care of People with Diabetes a Manual of Nursing Practice, 4th ed.; Wiley Blackwell: Hoboken, NJ, USA, 2014. [Google Scholar]
- World Health Organisation. Diagnostic Criteria and Classification of Hyperglycaemia First Detected in Pregnancy. 2013. Available online: http://apps.who.int/iris/bitstream/handle/10665/85975/WHO_NMH_MND_13.2_eng.pdf;jsessionid=09A82B923EF7A55CC6AB690976A1A1F3?sequence=1 (accessed on 16 November 2021).
- World Health Organisation. Definition, Diagnosis and Classification of Diabetes Mellitus and Its Complications Report of a WHO Consultation. 1999. Available online: https://www.staff.ncl.ac.uk/philip.home/who_dmg.pdf (accessed on 16 November 2021).
- Chiu, C.-J.; Taylor, A. Dietary hyperglycemia, glycemic index and metabolic retinal diseases. Prog. Retin. Eye Res. 2011, 30, 18–53. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kaminska, H.; Szarpak, L.; Kosior, D.; Wieczorek, W.; Szarpak, A.; Al-Jeabory, M.; Gawel, W.; Gasecka, A.; Jaguszewski, M.J.; Jarosz-Chobot, P. Impact of diabetes mellitus on in-hospital mortality in adult patients with COVID-19: A systematic review and meta-analysis. Acta Diabetol. 2021, 58, 1101–1110. [Google Scholar] [CrossRef]
- Wu, Z.-H.; Tang, Y.; Cheng, Q. Diabetes increases the mortality of patients with COVID-19: A meta-analysis. Acta Diabetol. 2020, 58, 139–144. [Google Scholar] [CrossRef] [PubMed]
- Jung, C.-H.; Choi, K.M. Impact of high-carbohydrate diet on metabolic parameters in patients with type 2 diabetes. Nutrients 2017, 9, 322. [Google Scholar] [CrossRef] [PubMed]


| Patient/Population | Intervention | Outcome (Primary) | Combining Search Terms |
|---|---|---|---|
| Patients with type 2 diabetes | COVID-19 Lockdown | Glycaemic and other metabolic parameters | |
| Patients with diabetes OR Type 2 diabetes OR Diabetes OR Diabetes complications OR diabetes mellitus, type 2 OR diabetes mellitus | Corona virus OR COVID-19 OR COVID-19 testing OR SARS-CoV-2 | Fasting blood glucose OR Glycated haemoglobin OR HbA1c OR Diabetic complications OR diabetic ketoacidosis | Column 1 AND Column 2 AND Column 3 |
| Citation/Country of Study | Type of Study | Sample Details | Mean Age (Years) | Aim | Study Design/Method | Results |
|---|---|---|---|---|---|---|
| Biamonte et al. [22] Italy | Retrospective, observational study | 128 participants with type 2 DM aged 18 yrs and above | 40–91 | To evaluate the impact of COVID-19 lockdown in Italy from 9 March to May 18 2020 on anthropometric parameters and glycaemic control in patients type 2 DM | A retrospective, observational study based on medical records. Evaluation was based on baseline between 15 December 2019 to 1 March 2020 compared to post lockdown between 15 and 30 June 2020 | During lockdown, there were significant increases in the following: body weight from 79.7 ± 18.7 kg to 81.4 ± 19.4 kg, p < 0.001; BMI from 29.5 ± 6 kg/m2 to 30.1 ± 6.3 kg/m2, p < 0.001; Waist circumference from 103.8 ± 13 cm to 105 ± 13.6 cm p < 0.001; Fasting plasma glucose from 138.1 ± 29.4 mg/dl to 146.6 ± 36.4 mg dl and HbA1c from 7 ± 0.8% to 7.3 ± 0.9%, p < 0.001 |
| Biancalana et al. [23] Italy | A single centre, prospective, observational study | 114 participants aged <85 years | 69.4 ± 10.3 | To explore the short-term impact of lockdown on metabolic control in patients with well-controlled type 2 DM. | A prospective observational study which assessed patients who were previously scheduled for follow-up visit during lockdown (9 March–4 May 2020). | After eight weeks of lockdown, an increase of HbA1c > 0.3% was observed in 26% of participants and triglycerides were persistently elevated. |
| D’Onofrio et al. [14] Italy | Observational multicentre retrospective cohort study | 264 participants with T2DM | 61.0–76.0 | To assess the effect of COVID-19 lockdown on glycaemic control in patients type 2 DM | An observational retrospective study consisting of 141 patients (lockdown group) and 123 patients (control group; pre-covid) | No difference in HbA1c was found in both groups (lockdown group: −0.01% [−0.5%, −0.3%] vs. control group −0.1% [−0.4%, −0.2%]; p = 0.482. Glucose (mg/dL) (p = 0.538). BMI (kg/m2) (p = 0.316) |
| Farhane et al. [9] Morocco | Retrospective observational study | 121 patients with T2DM aged 36–85 years | 57.31 ± 0.91 | To analyse the impact of lockdown on monitoring and care of T2DM patients in Morocco | A retrospective observational study. Biochemical, socio-demographic and anthropometric data were collected from each patient pre-lockdown (1 November 2019–19 March 2020) and post-lockdown (6 July–29 December 2020). | Lockdown impacted negatively on health status of T2DM patients, especially women. In women, HbA1c increased from 8.66 ± 0.21% to 9.51 ± 0.25% (p = 0.001) HDL-C (g/L) increased too (p = 0.0132), weight increased from 78.13 ± 1.36 kg to 81.80 ± 1.45 kg with p < 0.000, Systolic blood pressure (mmHg) reduced after lockdown (p = 0.0302). |
| Ghosh et al. [21] India | Case control | 555 participants aged 18 and above with new onset of diabetes | 46.2 ± 12.3 | To investigate if new onset diabetes during COVID-19 is phenotypically or biochemically different from new onset diabetes before COVID-19 | Patient diagnosed from 1 April 20–30 October 20 (Covid group) from two hospitals were in one group and patients diagnosed from 1 September 19–29 February 20 (pre-covid) from same hospital were in comparator group.Data were collected and compared. | There was no significant difference in symptomatology, phenotype and C-peptide levels between the pre-covid and Covid groups but the Covid group had more hyperglycaemia probably due to delayed diagnosis. |
| Ludwig et al. [24] France | Observational cross-sectional single-centre study | 870 adults living with type 1 or type 2 diabetes | 65.0 (57.0, 72.0) | To evaluate the impact of the COVID-19 lockdown on metabolic control and access to healthcare in patients with diabetes. | Data were collected from existing medical records and self-administered questionnaire from patients pre (18 September 2019 to 24 March 2020) and post (11 May 2020 to 20 June 2020) lockdown. These data were compared. | Despite the lockdown and disruption in healthcare, there was improvement in metabolic control in a large sample of patients.HbA1c pre-lock was 7.7% (7.1, 8.4) and post-lockdown was 7.4% (6.8, 8.2) (p < 0.0001). |
| Munekawa et al. [25] Japan | cross-sectional and retrospective cohort study | 203 patients with T2DM | 67.4 (11.3) | To investigate the acute effects of the COVID-19 pandemic on the lifestyle changes in patients with T2DM | Data regarding the body weight and HbA1c levels were collected from medical records and questionnaire was administered to the patients with type 2 diabetes mellitus who visited the clinic from 16 April to 1 May 2020 | Results showed increased stress levels and changes in life-style factors during the COVID-19 pandemic. These lifestyle changes were associated with increased body weight and HbA1c levels. [57.9 (±10.6) to 59.7 (±12.0) mmol/mol] (p = 0.001). |
| Onmez et al. [26] Turkey | Single-centre retrospective, observational study. | 101 type 2 DM patients aged 18–80 years | 55 ± 13 years | To investigate how type 2 DM patients were affected by the lockdown | A retrospective, observational study was conducted between 16 March and 1 June 2020 with patients unable to attend follow-ups due to lockdown, but who attended follow-ups in July and August post lockdown | Glycaemic parameters, HbA1c increased from 7.67 ± 1.76% to 8.11 ± 2.48%, fasting glucose from 157.9 (83–645) mg/dL to 163.2 (84–550) mg/dl, postprandial glucose from 228.8 ± 72.9 mg/dl to 260.3 ±90.8 mg/dL.The changes between pre and post lockdown were not statistically significant (p = 0.253, p = 0.678 and p = 0.079, respectively). |
| Park et al. [27] South Korea | Retrospective cohort study | 20,087 adult patients with T2DM. Aged 19 and over | (62.8 years) [19 to 95 years] | To determine the effects of social distancing due to COVID-19 on the changes in HbA1c level in people with T2DM. | Data were collected from the COVID-19 cohort (2019 to 2020), non-COVID-19 cohort 1 (2018 to 2019) and cohort 2 (2017 to 2018), and categorized into Periods 1 and 2. The HbA1c values for each patient were collected from their electronic medical records. The changes in HbA1c between Periods 1 and 2 in the COVID-19 cohort were compared with those in the non-COVID-19 cohorts as control groups. | Social distancing due to COVID-19 negatively impacted glycaemic control in people with T2DM |
| Rastogi et al. [28] India | prospective, observational, cohort study | 422 patients living with T2DM | 58.0 (52.0 to 64.0) | To examine the effect of lockdown on physical activity and glycaemic control in T2DM | Data relating to changes in glycaemic control (HbA1c) with the modification of weight, BMI, and physical activity during the lockdown period were collected. The pre- and post-lockdown glycaemic variables were compared using Wilcoxon signed-rank t test | Result showed that there is an overall improvement of glycaemic control during COVID-19 lockdown independent of increase in physical activity in people with long duration of T2DM. HbA1c pre lockdown was 7.8% (6.9 to 9.4%) compared with 7.4% (6.6 to 8.7) after 3 months of lockdown (p = 0.005) |
| Sankar et al. [29] India | Hospital-based cross-sectional survey | 110 Adult participants with T2DM | 58.67 ± 10.8 years. | To identify the effects of lockdown on glycaemic status, lifestyle changes and psychosocial health. | The pre- and post-lockdown data of 110 adults with T2D who were under regular follow up was collected by direct interview during their visit to the diabetes clinic. The variables analysed included demographic data, HbA1c, body weight, lifestyle changes, psychosocial factors and use of technology | Lockdown did not cause a major change in the overall glycaemic control.There was no statistically significant difference in the mean HbA1c before (8.2 ± 1.3%) and after (8.12 ± 1.6%) lockdown. The mean body weight after the lockdown was numerically higher (71.8 ± 13.6 kg) compared to that before lockdown (71.5 ± 14.8 kg), but could not achieve statistical significance. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ojo, O.; Wang, X.-H.; Ojo, O.O.; Orjih, E.; Pavithran, N.; Adegboye, A.R.A.; Feng, Q.-Q.; McCrone, P. The Effects of COVID-19 Lockdown on Glycaemic Control and Lipid Profile in Patients with Type 2 Diabetes: A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2022, 19, 1095. https://doi.org/10.3390/ijerph19031095
Ojo O, Wang X-H, Ojo OO, Orjih E, Pavithran N, Adegboye ARA, Feng Q-Q, McCrone P. The Effects of COVID-19 Lockdown on Glycaemic Control and Lipid Profile in Patients with Type 2 Diabetes: A Systematic Review and Meta-Analysis. International Journal of Environmental Research and Public Health. 2022; 19(3):1095. https://doi.org/10.3390/ijerph19031095
Chicago/Turabian StyleOjo, Omorogieva, Xiao-Hua Wang, Osarhumwese Osaretin Ojo, Edith Orjih, Nivedita Pavithran, Amanda Rodrigues Amorim Adegboye, Qian-Qian Feng, and Paul McCrone. 2022. "The Effects of COVID-19 Lockdown on Glycaemic Control and Lipid Profile in Patients with Type 2 Diabetes: A Systematic Review and Meta-Analysis" International Journal of Environmental Research and Public Health 19, no. 3: 1095. https://doi.org/10.3390/ijerph19031095
APA StyleOjo, O., Wang, X.-H., Ojo, O. O., Orjih, E., Pavithran, N., Adegboye, A. R. A., Feng, Q.-Q., & McCrone, P. (2022). The Effects of COVID-19 Lockdown on Glycaemic Control and Lipid Profile in Patients with Type 2 Diabetes: A Systematic Review and Meta-Analysis. International Journal of Environmental Research and Public Health, 19(3), 1095. https://doi.org/10.3390/ijerph19031095









