Catch-Up Growth as a Risk Factor for Rapid Weight Gain, Earlier Menarche and Earlier Pubertal Growth Spurt in Girls Born Small for Gestational Age (SGA)—A Longitudinal Study
Abstract
1. Introduction
2. Materials & Methods
2.1. Participants and Study Design
2.2. Size at Birth
2.3. Anthropometric Measurements
2.4. Age at Menarche
2.5. Body Mass Index
2.6. Catch-Up Growth
2.7. Growth Curves and the Assessment of the Specific Parameters of Adolescent Growth Spurt
- t—postnatal age
- Y—height reached at age t
- A—adult height
- E—estimated prenatal duration of growth
- D1, D2, D3—time-scale factors
- C1, C2, C3—dimensionless exponents
2.8. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Battaglia, F.C.; Lubchenco, L.O. A practical classification of newborn infants by weight and gestational age. J. Pediatr. 1967, 71, 159–163. [Google Scholar] [CrossRef]
- Lee, P.A.; Chernausek, S.D.; Hokken-Koelega, A.C.S.; Czernichow, P. For the International SGA Advisory Board International Small for Gestational Age Advisory Board Consensus Development Conference Statement: Management of Short Children Born Small for Gestational Age, April 24–October 1, 2001. Pediatrics 2003, 111, 1253–1261. [Google Scholar] [CrossRef] [PubMed]
- Cho, W.K.; Suh, B.-K. Catch-up growth and catch-up fat in children born small for gestational age. Korean J. Pediatr. 2016, 59, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Albertsson-Wikland, K.; Karlberg, J. Natural Growth in Children Born SGA with and without Catch Up Growth. Horm. Res. Paediatr. 2003, 59, 129. [Google Scholar] [CrossRef] [PubMed]
- Ong, K.K.L.; Ahmed, M.L.; Emmett, P.M.; Preece, M.A.; Dunger, P.D.B. Association between postnatal catch-up growth and obesity in childhood: Prospective cohort study. BMJ 2000, 320, 967–971. [Google Scholar] [CrossRef]
- Karlberg, J.; Kwan, C.-W.; Gelander, L.; Albertsson-Wikland, K. Pubertal Growth Assessment. Horm. Res. Paediatr. 2003, 60, 27–35. [Google Scholar] [CrossRef] [PubMed]
- Prader, A.; Tanner, J.; von Harnack, G. Catch-up growth following illness or starvation: An example of developmental canalization in man. J. Pediatr. 1963, 62, 646–659. [Google Scholar] [CrossRef]
- Wit, J.M.; Boersma, B. Catch-up Growth: Definition, Mechanisms, and Models. J. Pediatr. Endocrinol. Metab. 2002, 15, 1229–1241. [Google Scholar]
- Boersma, B.; Wit, J.M. Catch-up Growth. Endocr. Rev. 1997, 18, 646–661. [Google Scholar] [CrossRef]
- Nam, H.-K.; Lee, K.-H. Small for gestational age and obesity: Epidemiology and general risks. Ann. Pediatr. Endocrinol. Metab. 2018, 23, 9–13. [Google Scholar] [CrossRef]
- Ong, K. Catch-up Growth in Small for Gestational Age Babies: Good or Bad? Curr. Opin. Endocrinol. Diabetes Obes. 2007, 14, 30–34. [Google Scholar] [CrossRef] [PubMed]
- Kryst, Ł.; Żegleń, M.; Woronkowicz, A.; Kowal, M. Body composition of children with different gestation time. Am. J. Hum. Biol. 2021, 34, e23696. [Google Scholar] [CrossRef] [PubMed]
- Sahoo, K.; Sahoo, B.; Choudhury, A.K.; Sofi, N.Y.; Kumar, R.; Bhadoria, A.S. Childhood Obesity: Causes and Consequences. J. Fam. Med. Prim. Care 2015, 4, 187–192. [Google Scholar]
- Durda-Masny, M.; Hanć, T.; Czapla, Z.; Szwed, A. BMI at menarche and timing of growth spurt and puberty in Polish girls—Longitudinal study. Anthr. Anz. 2019, 76, 37–47. [Google Scholar] [CrossRef] [PubMed]
- Shalitin, S.; Kiess, W. Putative Effects of Obesity on Linear Growth and Puberty. Horm. Res. Paediatr. 2017, 88, 101–110. [Google Scholar] [CrossRef] [PubMed]
- Shalitin, S.; Phillip, M. Role of obesity and leptin in the pubertal process and pubertal growth—A review. Int. J. Obes. 2003, 27, 869–874. [Google Scholar] [CrossRef]
- Varvarigou, A.A. Intrauterine Growth Restriction as a Potential Risk Factor for Disease Onset in Adulthood. J. Pediatr. Endocrinol. Metab. 2010, 23, 215–224. [Google Scholar] [CrossRef]
- DeLeonibus, C.; Marcovecchio, M.L.; Chiarelli, F. Update on Natural Growth and Pubertal Development in Obese Children. Pediatr. Rep. 2012, 4, e35. [Google Scholar] [CrossRef]
- Saenger, P.; Czernichow, P.; Hughes, I.; Reiter, E.O. Small for Gestational Age: Short Stature and Beyond. Endocr. Rev. 2007, 28, 219–251. [Google Scholar] [CrossRef]
- Kaneshi, T.; Yoshida, T.; Ohshiro, T.; Nagasaki, H.; Asato, Y.; Ohta, T. Birthweight and risk factors for cardiovascular diseases in Japanese schoolchildren. Pediatr. Int. 2007, 49, 138–143. [Google Scholar] [CrossRef]
- Hales, C.N.; Barker, D.J.P. Type 2 (non-insulin-dependent) diabetes mellitus: The thrifty phenotype hypothesis. Diabetologia 1992, 35, 595–601. [Google Scholar] [CrossRef] [PubMed]
- Barker, D. The Developmental Origins of Adult Disease. J. Am. Coll. Nutr. 2004, 23, 588S–595S. [Google Scholar] [CrossRef] [PubMed]
- Adair, L.S.; Fall, C.H.; Osmond, C.; Stein, A.D.; Martorell, R.; Ramirez-Zea, M.; Sachdev, H.S.; Dahly, D.L.; Bas, I.; Norris, S.A.; et al. Associations of linear growth and relative weight gain during early life with adult health and human capital in countries of low and middle income: Findings from five birth cohort studies. Lancet 2013, 382, 525–534. [Google Scholar] [CrossRef] [PubMed]
- Saenger, P.; Reiter, E. Genetic factors associated with small for gestational age birth and the use of human growth hormone in treating the disorder. Int. J. Pediatr. Endocrinol. 2012, 2012, 12. [Google Scholar] [CrossRef] [PubMed]
- Argente, J.; Mehls, O.; Barrios, V. Growth and body composition in very young SGA children. Pediatr. Nephrol. 2010, 25, 679–685. [Google Scholar] [CrossRef]
- Kusuda, S.; Fujimura, M.; Sakuma, I.; Aotani, H.; Kabe, K.; Itani, Y.; Ichiba, H.; Matsunami, K.; Nishida, H. Morbidity and Mortality of Infants With Very Low Birth Weight in Japan: Center Variation. Pediatrics 2006, 118, e1130–e1138. [Google Scholar] [CrossRef]
- Szwed, A.; Kosińska, M. Biological maturity at birth, the course of the subsequent ontogenetic stages and age at menarche. HOMO 2012, 63, 292–300. [Google Scholar] [CrossRef]
- Koziel, S.; Jankowska, E.A. Effect of low versus normal birthweight on menarche in 14-year-old Polish girls. J. Paediatr. Child Health 2002, 38, 268–271. [Google Scholar] [CrossRef]
- Johnston, K.M.; Gooch, K.; Korol, E.; Vo, P.; Eyawo, O.; Bradt, P.; Levy, A. The economic burden of prematurity in Canada. BMC Pediatr. 2014, 14, 1–10. [Google Scholar] [CrossRef]
- Hvidt, J.J.; Brix, N.; Ernst, A.; Lauridsen, L.L.B.; Ramlau-Hansen, C.H. Size at birth, infant growth, and age at pubertal development in boys and girls. Clin. Epidemiol. 2019, 11, 873–883. [Google Scholar] [CrossRef]
- Albertsson-Wikland, K.; Karlberg, J. Natural growth in children born small for gestational age with and without catch-up growth. Acta Paediatr. 1994, 83, 64–70. [Google Scholar] [CrossRef]
- Ibáñez, L.; Ong, K.; Dunger, D.B.; de Zegher, F. Early Development of Adiposity and Insulin Resistance after Catch-Up Weight Gain in Small-for-Gestational-Age Children. J. Clin. Endocrinol. Metab. 2006, 91, 2153–2158. [Google Scholar] [CrossRef]
- Hernández, M.I.; Mericq, V. Impact of being born small for gestational age on onset and progression of puberty. Best Pract. Res. Clin. Endocrinol. Metab. 2008, 22, 463–476. [Google Scholar] [CrossRef] [PubMed]
- Chaudhari, S.; Otiv, M.; Hoge, M.; Pandit, A.; Mote, A. Growth and sexual maturation of low birth weight infants at early adolescence. Indian Pediatr. 2008, 45, 191. [Google Scholar] [PubMed]
- Deng, X.; Li, W.; Luo, Y.; Liu, S.; Wen, Y.; Liu, Q. Association between Small Fetuses and Puberty Timing: A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2017, 14, 1377. [Google Scholar] [CrossRef] [PubMed]
- Kosińska, M. Two methods for estimating age of newborns in catch-up growth studies. Early Hum. Dev. 2006, 82, 575–582. [Google Scholar] [CrossRef] [PubMed]
- Roggero, P.; Gianni, M.L.; Amato, O.; Orsi, A.; Piemontese, P.; Morlacchi, L.; Mosca, F. Is Term Newborn Body Composition Being Achieved Postnatally in Preterm Infants? Early Hum. Dev. 2009, 85, 349–352. [Google Scholar] [CrossRef] [PubMed]
- Roggero, P.; Gianni, M.L.; Amato, O.; Orsi, A.; Piemontese, P.; Cosma, B.; Morlacchi, L.; Mosca, F. Postnatal Growth Failure in Preterm Infants: Recovery of Growth and Body Composition After Term. Early Hum. Dev. 2008, 24, 555–559. [Google Scholar] [CrossRef] [PubMed]
- Fenton, T.R.; Kim, J.H. A systematic review and meta-analysis to revise the Fenton growth chart for preterm infants. BMC Pediatr. 2013, 13, 59. [Google Scholar] [CrossRef] [PubMed]
- Koyanagi, A.; Zhang, J.; Dagvadorj, A.; Hirayama, F.; Shibuya, K.; Souza, J.P.; Gülmezoglu, A.M. Macrosomia in 23 developing countries: An analysis of a multicountry, facility-based, cross-sectional survey. Lancet 2013, 381, 476–483. [Google Scholar] [CrossRef]
- Cameron, N.; Hiernaux, J.; Jarman, S.; Marshall, W.A.; Tanner, J.M.; Whitehouse, R.H. Anthropometry. In Practical human biology; Weiner, J.S., Lourie, J.A., Eds.; Academic Press: London, UK, 1981. [Google Scholar]
- Daniels, S.R.; Khoury, P.R.; Morrison, J.A. The Utility of Body Mass Index as a Measure of Body Fatness in Children and Adolescents: Differences by Race and Gender. Pediatrics 1997, 99, 804–807. [Google Scholar] [CrossRef] [PubMed]
- WHO Multicentre Growth Reference Study Group. WHO Child Growth Standards based on length/height, weight and age. Acta Paediatr. 2006, 95, 76–85. [Google Scholar]
- Jolicoeur, P.; Pontier, J.; Abidi, H. Asymptotic models for the longitudinal growth of human stature. Am. J. Hum. Biol. 1992, 4, 461–468. [Google Scholar] [CrossRef] [PubMed]
- Jolicoeur, P.; Pontier, J.; Pernin, M.-O.; Sempe, M. A Lifetime Asymptotic Growth Curve for Human Height. Biometrics 1988, 44, 995. [Google Scholar] [CrossRef] [PubMed]
- Molinari, L.; Gasser, T. The Human Growth Curve: Distance, Velocity and Acceleration; Methods in Human Growth Research; Cambridge University Press: Cambridge, UK, 2004. [Google Scholar]
- Kaczmarek, M. Poznańskie Badania Longitudinalne. Rozwój Fizyczny Chłopców i Dziewcząt. Moonografie Inst. Antropol. UAM 2001, 9, 38. [Google Scholar]
- Ibáñez, L.; Potau, N.; Marcos, M.V.; De Zegher, F. Exaggerated Adrenarche and Hyperinsulinism in Adolescent Girls Born Small for Gestational Age. J. Clin. Endocrinol. Metab. 1999, 84, 4739–4741. [Google Scholar] [CrossRef]
- Ibáñez, L.; Potau, N.; Francois, I.; De Zegher, F. Precocious Pubarche, Hyperinsulinism, and Ovarian Hyperandrogenism in Girls: Relation to Reduced Fetal Growth. J. Clin. Endocrinol. Metab. 1998, 83, 3558–3562. [Google Scholar] [CrossRef]
- Yadav, S.; Rustogi, D. Small for gestational age: Growth and puberty issues. Indian Pediatr. 2015, 52, 135–140. [Google Scholar] [CrossRef] [PubMed]
- Ong, K.K.; Potau, N.; Petry, C.J.; Jones, R.; Ness, A.R.; Honour, J.W.; De Zegher, F.; Ibáñez, L.; Dunger, D.B. Opposing Influences of Prenatal and Postnatal Weight Gain on Adrenarche in Normal Boys and Girls. J. Clin. Endocrinol. Metab. 2004, 89, 2647–2651. [Google Scholar] [CrossRef]
- Francois, I.; De Zegher, F. Adrenarche and Fetal Growth. Pediatr. Res. 1997, 41, 440–442. [Google Scholar] [CrossRef][Green Version]
- Kimber-Trojnar, Ż.; Marciniak, A.; Patro-Małysza, J.; Marciniak, B.; Mielnik-Niedzielska, G.; Leszczyńska-Gorzelak, B. Programowanie Płodowe. Ginekol. Perinatol. Prakt. 2018, 3, 58–63. [Google Scholar]
- Hales, C.N.; Barker, D. The Thrifty Phenotype Hypothesis: Type 2 Diabetes. Br. Med. Bull. 2001, 60, 5–20. [Google Scholar] [CrossRef]
- Clayton, P.E.; Cianfarani, P.; Czernichow, G.; Johannsson, R.; Rogol, R.A. Management of the Child Born Small for Gestational Age through to Adulthood: A Consensus Statement of the International Societies of Pediatric Endocrinology and the Growth Hormone Research Society. J. Clin. Endocrinol. Metab. 2007, 92, 804–810. [Google Scholar] [CrossRef]
- Kaplowitz, P.B. Link Between Body Fat and the Timing of Puberty. Pediatrics 2008, 121, S208–S217. [Google Scholar] [CrossRef] [PubMed]
- Cortés, M.E.; Carrera, B.; Rioseco, H.; del Río, J.P.; Vigil, P. The Role of Kisspeptin in the Onset of Puberty and in the Ovulatory Mechanism: A Mini-review. J. Pediatr. Adolesc. Gynecol. 2015, 28, 286–291. [Google Scholar] [CrossRef] [PubMed]
- Martos-Moreno, G.; Chowen, J.; Argente, J. Metabolic signals in human puberty: Effects of over and undernutrition. Mol. Cell. Endocrinol. 2010, 324, 70–81. [Google Scholar] [CrossRef] [PubMed]
- Solorzano, C.M.B.; McCartney, C.R. Obesity and the pubertal transition in girls and boys. Reproduction 2010, 140, 399–410. [Google Scholar] [CrossRef]
- Lueprasitsakul, P.; Latour, D.; Longcope, C. Aromatase activity in human adipose tissue stromal cells: Effect of growth factors. Steroids 1990, 55, 540–544. [Google Scholar] [CrossRef] [PubMed]
- Blank, S.K.; McCartney, C.R.; Chhabra, S.; Helm, K.D.; Eagleson, C.A.; Chang, R.J.; Marshall, J.C. Modulation of Gonadotropin-Releasing Hormone Pulse Generator Sensitivity to Progesterone Inhibition in Hyperandrogenic Adolescent Girls—Implications for Regulation of Pubertal Maturation. J. Clin. Endocrinol. Metab. 2009, 94, 2360–2366. [Google Scholar] [CrossRef] [PubMed]
- Frisch, R.E.; Revelle, R. Height and weight at menarche and a hypothesis of menarche. Arch. Dis. Child. 1971, 46, 695–701. [Google Scholar] [CrossRef] [PubMed]
- Forbes, G.B. Nutrition and Growth. J. Pediatr. 1977, 91, 40–42. [Google Scholar] [CrossRef] [PubMed]
- Vignolo, M.; Naselli, A.; Di Battista, E.; Mostert, M.; Aicardi, G. Growth and development in simple obesity. Eur. J. Pediatr. 1988, 147, 242–244. [Google Scholar] [CrossRef]
- Postel-Vinay, M.-C.; Saab, C.; Gourmelen, M. Nutritional Status and Growth Hormone-Binding Protein. Horm. Res. 1995, 44, 177–181. [Google Scholar] [CrossRef]
- Bideci, A.; Cinaz, P.; Hasanoglu, A.; Elbeg, S. Serum levels of insulin-like growth factor-I and insulin-like growth factor binding protein-3 in obese children. J. Pediatr. Endocrinol. Metab. 1997, 10, 295–300. [Google Scholar] [CrossRef] [PubMed]
- Malendowicz, L.K.; Rucinski, M.; Belloni, A.S.; Ziolkowska, A.; Nussdorfer, G.G. Leptin and the Regulation of the Hypothalamic–Pituitary–Adrenal Axis. Int. Rev. Cytol. 2007, 263, 63–102. [Google Scholar] [PubMed]
- Meinhardt, U.J.; Ho, K.K.Y. Modulation of growth hormone action by sex steroids. Clin. Endocrinol. 2006, 65, 413–422. [Google Scholar] [CrossRef]
- Maor, G.; Rochwerger, M.; Segev, Y.; Phillip, M. Leptin Acts as a Growth Factor on the Chondrocytes of Skeletal Growth Centers. J. Bone Miner. Res. 2002, 17, 1034–1043. [Google Scholar] [CrossRef]
- Graber, J.A.; Seeley, J.R.; Brooks-Gunn, J.; Lewinsohn, P.M. Is pubertal timing associated with psychopathology in young adulthood. J. Am. Acad. Child Adolesc. Psychiatry 2004, 43, 718–726. [Google Scholar] [CrossRef]
- Mendle, J.; Turkheimer, E.; Emery, R.E. Detrimental psychological outcomes associated with early pubertal timing in adolescent girls. Dev. Rev. 2007, 27, 151–171. [Google Scholar] [CrossRef]
- Copeland, W.; Shanahan, L.; Miller, S.; Costello, E.J.; Angold, A.; Maughan, B. Outcomes of Early Pubertal Timing in Young Women: A Prospective Population-Based Study. Am. J. Psychiatry 2010, 167, 1218–1225. [Google Scholar] [CrossRef]
- Olivieri, D.J.; Massingham, L.J.; Schwab, J.L.; Quintos, J.B. Lack of Catch-Up Growth with Growth Hormone Treatment in a Child Born Small for Gestational Age Leading to a Diagnosis of Noonan Syndrome with a Pathogenic PTPN11 Variant. Case Rep. Endocrinol. 2021, 2021, 5571524. [Google Scholar] [CrossRef] [PubMed]
- Stróżewska, W.; Durda-Masny, M.; Szwed, A. Mutations in GHR and IGF1R Genes as a Potential Reason for the Lack of Catch-Up Growth in SGA Children. Genes 2022, 13, 856. [Google Scholar] [CrossRef] [PubMed]
- Finken, M.; van der Steen, M.; Smeetrs, C.; Walenkamp, M.; de Bruin, C.; Hokken-Koelega, A.; Wit, J.M. Children Born Small for Gestational Age: Differential Diagnosis, Molecular Genetic Evaluation, and Implications. Endocr. Rev. 2018, 39, 851–894. [Google Scholar] [CrossRef] [PubMed]
- Netchine, I.; van der Steen, M.; López-Bermejo, A.; Koledova, E.; Maghnie, M. New Horizons in Short Children Born Small for Gestational Age. Front. Pediatr. 2021, 9, 655931. [Google Scholar] [CrossRef]
- Renes, J.; van Doorn, J.; Breukhoven, P.; Lem, A.; de Ridder, M.; Hokken-Koelega, A. Acid-Labile Subunit Levels and the Association with Response to Growth Hormone Treatment in Short Children Born Small for Gestational Age. Horm. Res. Paediatr. 2014, 81, 126–132. [Google Scholar] [CrossRef]
- de Zegher, F.; Ong, K.; Ibáñez, L.; Dunger, D. Growth Hormone Therapy in Short Children Born Small for Gestational Age. Horm. Res. Paediatr. 2006, 65, 145–152. [Google Scholar] [CrossRef]
- Caliebe, J.; Broekman, S.; Boogaard, M.; Bosch, C.A.; Ruivenkamp, C.A.; Oostdijk, W.; Kant, S.; Binder, G.; Ranke, M.B.; Wit, J.M.; et al. IGF1, IGF1R and SHOX Mutation Analysis in Short Children Born Small for Gestational Age and Short Children with Normal Birth Size (Idiopathic Short Stature). Horm. Res. Paediatr. 2012, 77, 250–260. [Google Scholar] [CrossRef]
- Giabicani, E.; Willems, M.; Steunou, V.; Chantot-Bastaraud, S.; Thibaud, N.; Habib, W.A.; Azzi, S.; Lam, B.; Bérard, L.; Bony-Trifunovic, H.; et al. Increasing knowledge in IGF1R defects: Lessons from 35 new patients. J. Med. Genet. 2019, 57, 160–168. [Google Scholar] [CrossRef]
- Zhu, J.; Chan, Y.-M. Adult Consequences of Self-Limited Delayed Puberty. Pediatrics 2017, 139, e20163177. [Google Scholar] [CrossRef]


| N | % | |
|---|---|---|
| Mother’s education | ||
| Primary/vocational | 78 | 26.26 |
| Secondary | 134 | 45.12 |
| University | 85 | 28.62 |
| Father’s education | ||
| Primary/vocational | 134 | 45.12 |
| Secondary | 102 | 34.34 |
| University | 61 | 20.54 |
| Number of children in the family | ||
| One | 107 | 36.03 |
| Two | 104 | 35.02 |
| Three or more | 86 | 28.95 |
| Economic status of the family | ||
| Good | 109 | 36.70 |
| Middle (average) | 156 | 52.53 |
| Bad | 32 | 10.77 |
| Variable | SGA, Catch-Up Growth | SD | AGA | SD | SGA, No-Catch-Up Growth | SD | H | p |
|---|---|---|---|---|---|---|---|---|
| BMI at 8 ya (z-scores) | 1.49 | 1.19 | 0.31 | 0.95 | −1.95 | 0.41 | 94.22 | <0.001 |
| BMI at menarche (z-scores) | 1.47 | 1.10 | 0.45 | 0.97 | −0.98 | 1.07 | 58.21 | <0.001 |
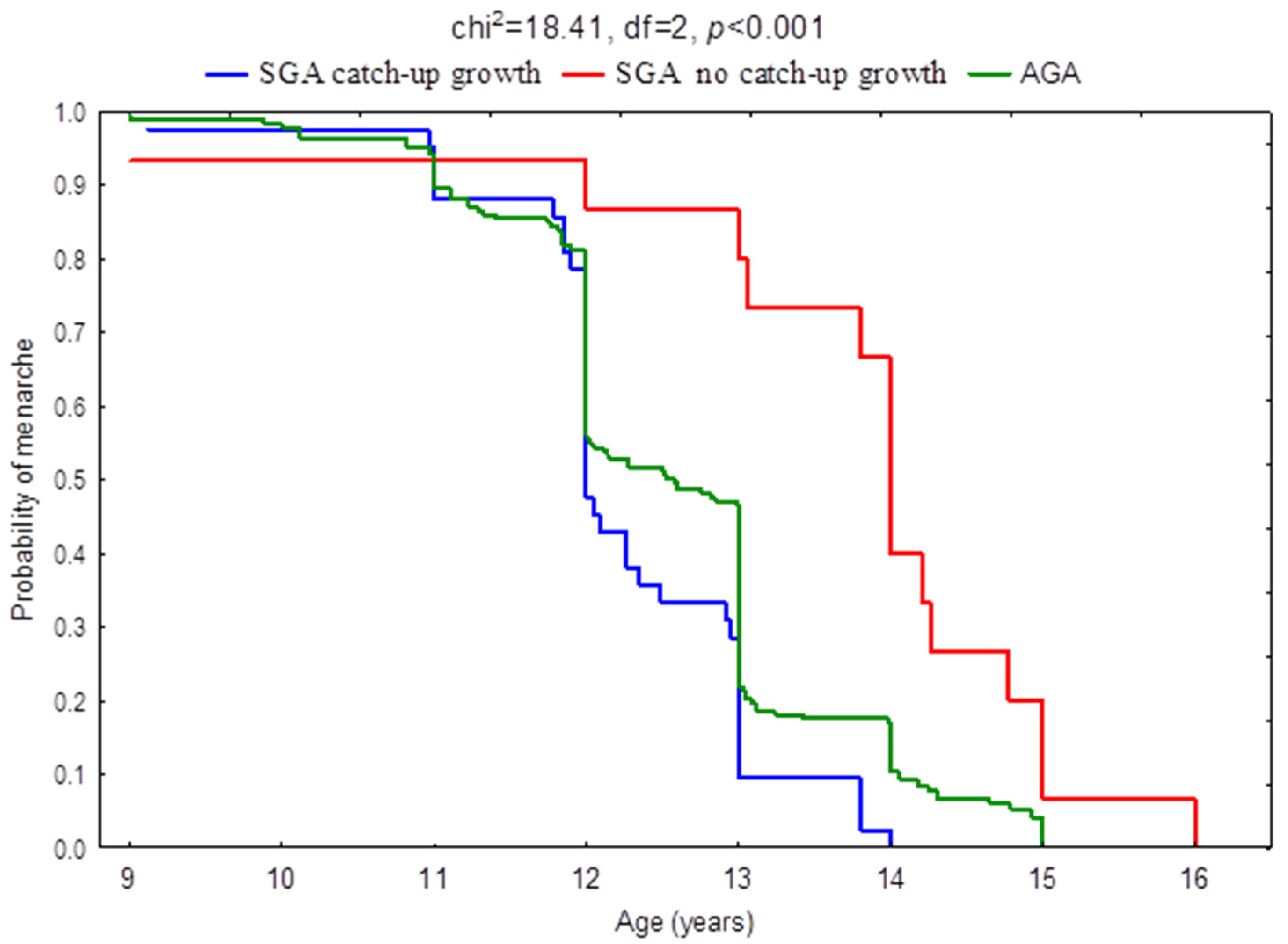
| Age at menarche (years) | 12.25 | 0.88 | 12.57 | 1.16 | 13.86 | 1.60 | 21.77 | <0.001 |
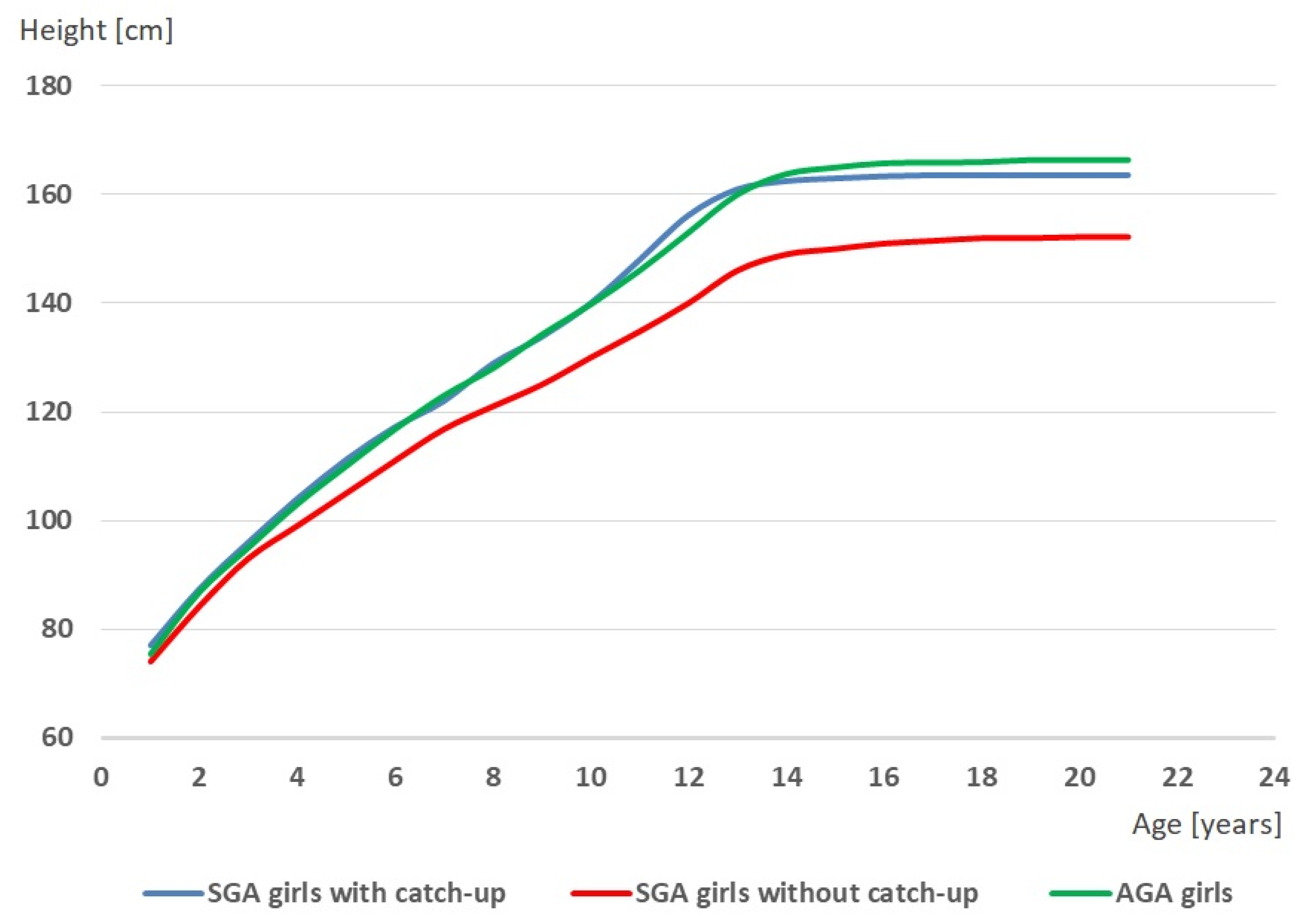
| Age at TO (years) | 8.28 | 0.77 | 8.57 | 0.63 | 8.72 | 0.79 | 8.85 | 0.012 |
| Age at PHV (years) | 11.36 | 0.77 | 11.55 | 0.72 | 11.89 | 0.85 | 11.71 | 0.003 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Durda-Masny, M.; Stróżewska, W.; Szwed, A. Catch-Up Growth as a Risk Factor for Rapid Weight Gain, Earlier Menarche and Earlier Pubertal Growth Spurt in Girls Born Small for Gestational Age (SGA)—A Longitudinal Study. Int. J. Environ. Res. Public Health 2022, 19, 16808. https://doi.org/10.3390/ijerph192416808
Durda-Masny M, Stróżewska W, Szwed A. Catch-Up Growth as a Risk Factor for Rapid Weight Gain, Earlier Menarche and Earlier Pubertal Growth Spurt in Girls Born Small for Gestational Age (SGA)—A Longitudinal Study. International Journal of Environmental Research and Public Health. 2022; 19(24):16808. https://doi.org/10.3390/ijerph192416808
Chicago/Turabian StyleDurda-Masny, Magdalena, Weronika Stróżewska, and Anita Szwed. 2022. "Catch-Up Growth as a Risk Factor for Rapid Weight Gain, Earlier Menarche and Earlier Pubertal Growth Spurt in Girls Born Small for Gestational Age (SGA)—A Longitudinal Study" International Journal of Environmental Research and Public Health 19, no. 24: 16808. https://doi.org/10.3390/ijerph192416808
APA StyleDurda-Masny, M., Stróżewska, W., & Szwed, A. (2022). Catch-Up Growth as a Risk Factor for Rapid Weight Gain, Earlier Menarche and Earlier Pubertal Growth Spurt in Girls Born Small for Gestational Age (SGA)—A Longitudinal Study. International Journal of Environmental Research and Public Health, 19(24), 16808. https://doi.org/10.3390/ijerph192416808





