Abstract
Background. A growing body of research suggests that financial difficulties could weaken the protective effects of socioeconomic status (SES) indicators, including education and income, on the health status of marginalized communities, such as African Americans. Aim. We investigated the separate and joint effects of education, income, and financial difficulties on mental, physical, and oral self-rated health (SRH) outcomes in African American middle-aged and older adults. Methods. This cross-sectional study enrolled 150 middle-aged and older African Americans residing in South Los Angeles. Data on demographic factors (age and gender), socioeconomic characteristics (education, income, and financial difficulties), and self-rated health (mental, physical, and oral health) were collected. Three linear regression models were used to analyze the data. Results. Higher education and income were associated with a lower level of financial strain in a bivariate analysis. However, according to multivariable models, only financial difficulties were associated with poor mental, physical, and oral health. As similar patterns emerged for all three health outcomes, the risk associated with financial difficulties seems robust. Conclusions. According to our multivariable models, financial strain is a more salient social determinant of health within African American communities than education and income in economically constrained urban environments such as South Los Angeles. While education and income lose some protective effects, financial strain continues to deteriorate the health of African American communities across domains.
1. Background
Oakes and Rossi (2003) define socioeconomic status (SES) as “access to desired resources” [1]. While some measures of SES are objective, other SES indicators are subjective. Some of the pathways that connect SES to health are hypothesized pathways including inadequate money to cover basic needs, access health care, or provide preventive health resources such as acceptable housing or education (Committee on Understanding and Eliminating Racial and Ethnic Disparities in Health Care, 2003).
Although actual income and education are more commonly used as the proxy for SES, financial strain provides additional information about access to SES resources. This is because people with a similar level of education and income may have wide variation in their levels of financial strain. Since inadequacy of income is on the pathway that connects SES to health, it may be preferable to directly measure inadequacy of income to meet an individual’s needs, rather than education and income. To determine inadequacy of income, it is uncommon to have access to the objective data of an individual’s cost of living (e.g., household size, transportation needs) [1,2]. Instead, it is easy to ask for a person’s subjective appraisal of income inadequacy, also known as financial strain [1].
Research has shown that both objective and subjective SES indicators—such as education, income, and financial strain—operate as fundamental causes of health and illness [3,4,5,6,7]. As described by Link, Phelan, Mirowsky, Ross, Hayward, House, Lantz, Williams, and others, these SES indicators protect individuals against a wide range of health problems [3,4,5,6,8,9,10,11,12,13,14,15,16,17]. Education, income, and financial strain are among major social determinants of health in youth [18], adults [19], and middle-aged and older adults [20]. Low education, low income, and severe financial strain partially explain poor health in racial minority groups such as African Americans [21].
Financial strain reflects the economic adversities that individuals experience and report. Perceived financial strain is not addressed with objective and conventional SES indicators, such as education and income, as it is commonly measured as concerns related to a lack of sufficient economic means to afford lifestyle necessities [22,23]. Financial strain is frequently measured using items such as strain in paying for food, clothes, and other bills [24]. Previous research and theoretical work have shown that financial strain is the most salient SES determinant of health among African American individuals [2].
However, the effects of socioeconomic factors such as education, income, and financial strain are not similar across all racial groups [13,14,25]. Financial strain can substantially impact multiple health domains of communities; however, these effects may be more significant for African Americans than White people [24]. The reason for this could be the incredible financial strain experienced by racial/ethnic minorities who reside in communal areas with fewer protective buffers and limited resources [24]. One study suggested that perceived financial strain, not education or income, increased the health vulnerability of African Americans to negative risk factors, such as stress related to discrimination [24]. While SES indicators, such as education and income, reduce perceived discrimination and depression overall [24,26,27,28], these effects are weaker or absent for African Americans who report high perceived discrimination as their education and income increase [28,29,30,31]. Thus, it is essential to study the additive effects of education, income, and financial strain on health among these groups [24].
The gradient and threshold effects of education on mortality risk are shown to be diminished for African Americans compared to White people [13,14]. In the presence of racism and discrimination that impacts the education system and labor market, education may provide more oppor 4tunities, such as low-stress, high-paying jobs for White people than for African Americans. Thus, African American individuals with a high level of education may remain at an increased risk of working in worse jobs with high stress and low pay [32,33]. Therefore, under racism and discrimination, highly educated African Americans have worse health than their White counterparts [32,34,35,36]. As these SES indicators differently shape access to resources and exposure to risk factors among racial groups, [28,29,30,31] future research should test the additive effects of education, income, and financial strain on the African American community.
Research has shown weakened economic and health effects of SES indicators, such as education and income, for racialized and marginalized groups, particularly African Americans—a pattern called Minorities’ or Marginalization-related Diminished Returns (MDRs) [32,33,34,35,36,37]. For example, highly educated and high-income African Americans remain at a high risk of poor health [24,32,36,37,38,39,40]. Although this theory is commonly applied for comparative studies, it is also used by within-race studies that find weaker-than-expected effects of SES without having a White control group [41,42]. As White people are an arbitrary control group and should not be regarded as the norm (considering whiteness as the norm is in itself a reflection of racism), within-racial research has its own major implications [43].
These MDRs are robust as they are observed for African American youth [44,45,46,47,48,49,50,51,52,53,54,55,56,57] and adults [24,32,36,37,38,39,40], as well as middle-aged and older adults [58]. As a result of MDRs, middle- and high- SES African Americans show worse-than-expected health. This is because for African Americans, SES indicators such as education and income may have less-than-expected effects, and their financial strain may remain high, so they report poor well-being and health despite middle--to-high SES levels [24,59]. However, very few studies have simultaneously investigated the additive effects of education, income, and financial strain on various aspects of the health of African American middle-aged and older adults in areas that have been historically underserved and under-resourced.
Aims
In this study, we investigated the associations between three SES indicators (namely education, income, and financial strain) and three health outcomes (namely poor self-rated mental, physical, and oral health) among African American middle-aged and older adults residing in underserved areas of South Los Angeles. Figure 1 presents the study conceptual model. Underserved areas of South Los Angeles include SPA6, with a population of one million individuals, which has the lowest SES, poor access to health resources, and poor health outcomes.
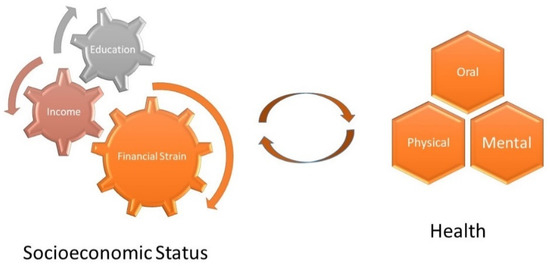
Figure 1.
Study conceptual model.
2. Methods
2.1. Design
We conducted this cross-sectional survey in South Los Angeles during the COVID-19 pandemic after vaccination became available for the public during 2021–2022. The study recruited African American middle-aged and older adults primarily from churches and other faith-based centers in South Los Angeles. Data were collected through structured face-to-face interviews on demographic factors; SES characteristics (education and financial strain); living arrangement; marital status; and self-rated mental, physical, and oral health.
2.2. Context of the Study
This survey was conducted in faith-based organizations (i.e., churches) in South Los Angeles during the COVID-19 pandemic after COVID-19 vaccines had become available for the public between 2021 and 2022. This is important in multiple regards. First, African American churches and other faith-based centers play a major spiritual and physical role in African American communities. Second, South Los Angeles and SPA6 is a historically underserved, highly segregated, impoverished, and economically disadvantaged area with high rates of poverty and unemployment among the several racial and ethnic minorities.
2.3. Participants and Sampling
The study recruited a convenience sample of middle-aged and older African American adults from faith-based organizations. All participants were Christians, and the faith-based organizations were predominantly Black churches. Eligibility included African American ethnicity, being 55 years or older, and residing in South Los Angeles. Considerable cognitive deficits or participation in a clinical trial were the exclusion criteria in this study. A total number of 150 individuals entered our analysis.
2.4. Study Measures
The variables in this study were demographic factors (i.e., sex/gender and age), socioeconomic status indicators (i.e., educational attainment, income, and financial strain), and health (i.e., self-reported mental, physical, and oral health).
2.4.1. Demographic Factors
Gender was a dichotomous variable, with males coded as 1 and females coded as 0. Age was treated as an interval variable (a continuous measure).
2.4.2. Health Insurance
Only two individuals did not have any health insurance. Thus, we could not include health insurance as a variable. The most common type of health coverage in our sample was Medicare, which was entered as a dichotomous variable in this study as a covariate. This variable was defined as Medicare vs. any other type of insurance or no insurance (n = 2). For the sensitivity analysis and robustness check, we ran our models without Medicare in the models and with Medicare, VA insurance, and Medicaid. The results regarding the significance of the effects of SES indicators did not change, so we reported a model that only controlled for Medicare as the most common insurance. This decision was made to avoid overfitting and over-adjustment, given the low sample size.
2.4.3. Education
Education attainment was self-reported and was measured as one of our SES indicators. Education was treated as an interval variable with five levels, with a higher score indicating more education: (1) no high school diploma, (2) high school diploma, (3) some college, (4) bachelor’s degree, and (5) graduate studies.
2.4.4. Income
Income was the 2nd measure of SES and was measured as an interval variable between 1 and 5: A higher score indicated more income. The categories of income were as follows: (1) <USD 10,000; (2) USD 10,000 to 30,000; (3) USD 30,000 to 50,000 (or <50,000); (4) USD 50,000 to 70,000; and (5) more than USD 70,000. For the sensitivity analysis, we tested our results with income as USD <35,000, 35,000–74,999, and >75,000.
2.4.5. Financial Strain
Financial strain was measured using four items in line with Pearlin’s list of main chronic financial strain as our 3rd measure of SES [60,61,62]. These items assessed whether money was sufficient to meet essential needs to pay for food, rent, clothes, and utility bills. These items measured the frequency of not having enough money to buy enough food, clothing, and pay bills. The responses were on a 0 to 5 scale for ‘never’ to ‘always’. We calculated a mean score with a range between 0 and 5. A higher score indicated greater financial strain. We did not include the item on strain in paying medical bills because that item did not load well on the same construct and reduced the reliability from more than 0.9 to about 0.6.
2.4.6. Self-Rated Mental, Physical, and Oral Health
The participants’ self-rated health (SRH) was measured using the conventional single-item health measure commonly used in the literature. This variable has five options ranging from 1 to 5 [63,64,65,66,67,68,69,70,71]. The item reads as “In general, would you say your …… health is: “very good”, “good”, “fair”, “bad”, or “very bad”. The responses were on an interval variable ranging from one to five, with a high score indicating poor self-rated health. Single-item self-rated health measures predict long-term mortality risk [63,64,65,66,67,68,69,70,71]. These questions were repeated for physical SRH, mental SRH, and oral SRH. Previous work has shown that SRH can be used as a continuous measure. As a result, many previous studies have used SRH as a continuous outcome [41,72,73].
2.5. Statistical Analysis
In this study, we used Statistical Package for the Social Science (SPSS) 23.0 for the data analysis. First, we described the overall sample by reporting the frequency (n) and relative frequency (%) of our categorical variables and reporting mean and standard deviation (SD) for our continuous measures. Then we ran a Spearman correlation to estimate the bivariate correlations between all study variables. Thus, multi-collinearity was ruled out between education, income, and financial strain. We then ran linear regression models with each health outcome as the dependent variable; education, income, and financial strain as the independent variables; and age, gender, marital status, and living arrangements as confounders. We reported b coefficients, standard error (SE), 95% confidence intervals (95% CI), and p values. For the sensitivity analysis, we ran logistic regression with the following coding of SRH: 0 = “very good”, “good”, and 1 = “fair”, “bad”, and “very bad”. As our results did not change between logistic regression and linear regression, and because linear regression was more parsimonious, we only reported the results of the linear regression model.
2.6. Institutional Review Board
The Charles R. Drew University of Medicine and Science institutional review board (IRB) approved the study protocol. All our participants signed the consent form.
3. Results
3.1. Descriptive Data
As shown in Table 1, most participants were female (70%), with an average age of 68.5 (SD = 8.6). Of the participants, 48% were on Medicare and 31.3% were living alone. All demographic variables and health data are summarized in Table 1.

Table 1.
Descriptive Statistics.
3.2. Correlations
Table 2 shows the results of the Spearman correlation test. Higher education and income were correlated with lower financial strain (r ranging 0.271 to 0.430, p < 0.05). Financial strain was positively correlated with self-rated health outcomes that reflected poor health (r ranging between 0.177 and 0.280, p < 0.05). Age and gender were not associated with education, income, or financial strain (p > 0.05).

Table 2.
Bivariate correlations (Spearman correlation).
3.3. Regression Results
Table 3 shows the results of three linear regression models, one for each outcome. These models suggested that financial strain, but not education or income, was associated with poor self-rated mental, physical, and oral health. Similar patterns emerged regardless of health outcome (p < 0.05 for financial strain and p > 0.05 for education and income). The associations were stronger for mental SRH (B = 0.271, p = 0.005) followed by oral (B = 0.212, 0.035) and physical SRH (B = 0.175, p was only marginally significant). Age was only associated with worse oral SRH (B = 0.035, p = 0.005). Gender, living arrangement, and insurance type did not correlate with oral, physical, or mental SRH (p > 0.05 for all).

Table 3.
Summary of three linear regression models with poor self-rated physical, mental, and oral health as outcomes.
4. Discussion
This study showed that while in a bivariate analysis, education, income, and financial strain are all correlated with poor SRH, in a multivariable analysis, financial strain increases the risk of poor health across domains, while education and income fail to show considerable protective effects. This is important and suggests that, at least in this context and this population, the harm associated with financial strain may be larger than the benefit associated with education and income.
We hypothesized that a high level of education and income would have protective effects and at the same time, that financial strain would pose a risk to the mental, physical, and oral health of African American middle-aged and older adults who reside in historically underserved, highly segregated, impoverished, and economically disadvantaged areas within South Los Angeles. We expected the same pattern across health outcomes [74] for the effects of education, income, and financial strain [75,76,77]. Our multivariable regression models found that, in South Los Angeles, financial strain increases the risk of poor health across domains, while education and income fail to show considerable protective effects. We explain this observation through the impacts of racism on reducing the health gains of education and income [32,34,35,38,39,40,65,78,79,80,81].
Financial strain reflects an understudied aspect of SES among African American communities [24], as it is a predictor for poor health [82] among the general population [83,84] and individuals with a chronic disease [85]. Understudied financial strain is an overlooked SES indicator [86,87,88,89]. Although different studies name the same construct as financial strain, financial stress, economic distress, or economic hardship [90,91,92,93], they all refer to a scarcity of liquid expendable income. Individuals with chronic financial strain cannot use the services that are essential for maintaining their health [83,94].
Financial strain is shown to be one of the most detrimental social determinants of health that operates as a risk factor for a wide range of health outcomes [82,95,96,97,98,99,100,101,102,103]. Additionally, financial strain impacts the health and well-being of the general population [104] and individuals with chronic disease [85]. In the US, African American middle-aged and older individuals with the highest levels of financial strain experience the worst levels of health. Financial strain deteriorates the health of African American middle-aged and older adults in deprived areas where social support and other potential buffers are scarce [84]. Low access to buffers is precarious for the health of the aging African American population [84].
Financial strain limits access to health resources and services [83] and operates as a type of stress [92]. Thus, financial strain increases the risk of chronic diseases [105], including—but not limited to—heart disease [106], diabetes [85], cancer [107], and hypertension [105]. It also worsens self-rated health [82] by causing anxiety [93,108], depression [59,87], and suicide [109]. Financial strain also predicts poor diet [110], smoking [111], and alcohol use [112]. All these increase the morbidity and mortality of populations [25,88,106,107,113]. Thus, the harm associated with financial strain has been widespread and sustained [114,115,116]. Financial strain also causes biological and social decline [92].
In one study in South Los Angeles [117], financial strain predicted chronic disease, chronic pain, self-rated health, depression, and the usage of sick days. In another study, financial strain was a risk factor for poor self-rated health, chronic pain, sick days, chronic disease, and depression, while education failed to show any protective effect for the same community [41]. Similar to the current study, that study compared the role of financial strain with education and showed similar results [41].
In our South Los Angeles study, education and income did not show any association with mental, physical, or oral self-rated health. While the weak or non-significant effects of education and income may be because these SES indicators are limited by social stratification [80], financial strain negatively impacts various domains of population health. In highly segregated areas, resources are scarce and support is limited, which may be particularly harmful as older adults age [84]. Previous research has established the detrimental effects of financial strain on the health of African Americans [87,118,119] and middle-aged and older adults [91,94,120], such as its impact on future cardiovascular disease [105]. The harm associated with financial strain in low-resource African American communities is exacerbated by chronic poverty due to unemployment, social isolation, and poor urban community infrastructures, including transportation. Thus, the social factors impacted by financial strain operate as risk factors for various chronic diseases.
Our observation that education and income did not correlate with self-rated mental, physical, and oral health, is in line with MDRs reported for self-rated health [32,37], depression [76,79], and chronic diseases [37,38]. These findings are shown not only for middle-aged and older adults [58], but also for children [37,39,40,80] and adults [32,37,78]. Similar findings are reported from national samples [32,38,78] and local studies [37,81]. Thus, regardless of the age, outcome, and design, studies have shown a reduced effect of education and income and an exacerbated effect of financial strain for African American communities.
In historically under-resourced areas, such as South Los Angeles, the potentially protective effects of education and income on the health and well-being of African Americans is weaker because these areas have limited higher income jobs, healthcare systems, transportation, and healthy food locations, as well as recreational parks for exercise. The financial strain becomes a significant threat to the health and well-being of African American [87,118,119] middle-aged and older adults [91,94,120].
Given that financial strain operates as a risk factor, as education and income fail to serve as protective factors, we invite researchers, policymakers, and clinicians to specifically think about the differences across various social determinants of health, from which some may have, and some may not have any effect on the health of African American middle-aged and older adults. As financial necessities operate as a major risk, African American middle-aged and older adults in urban settings may benefit from some cushions that buffer the effects of their financial adversities. Policies that increase the availability of financial supply at the time of need may be a promising strategy to tackle health disparities in African American middle-aged and older adults. We argue that fair lending policies at the time of emergency may be a health policy. Different social determinants have different effects and may not be comparable [121].
This study had some limitations. First, the sampling method was not random. All the participants were recruited from faith-based centers. This particular non-randomized sample can represent a limit. The population that frequents religious places is less heterogeneous than the population itself. Second, the sample size was 150. A larger sample size might show the effect of education and income in our study. However, our previous similar analysis in a larger sample showed similar findings [41]. Third, our study was cross-sectional. In addition, all our study variables were measured at the level of individuals; thus, we cannot claim that education and income do not affect the health of African Americans. We can only claim that these associations were not observed in this sample. We cannot generalize our findings to all African American communities or individuals; thus, we need to interpret the results with caution.
5. Conclusions
Financial strain may be particularly detrimental to the health of African American middle-aged and older adults, even those with a higher level of education and income. Although in the bivariate analysis, we could observe the protective effects of education and income, these effects disappeared in the multivariable analysis that included financial strain. According to our multivariable models, in economically deprived areas and constrained settings, the disadvantages of financial strain outweigh the health advantages of education and income. This finding is in line with the literature on MDRs [44,46,122,123,124,125,126,127,128,129,130] which frequently shows that the disadvantages are stronger than the advantages [131]. Diminishing returns of education and income may be due to structural racism, social stratification, and segregation. Policies that reduce the financial strain of African American middle-aged and older adults are essential and may have considerable health returns. Future research should also test the efficacy of economic policies, such as those that increase the availability of cash in times of need on the health outcomes of African American individuals. Such research is particularly important for contexts that are historically underserved and under-resourced.
Author Contributions
E.A., S.C. and B.N.: conceptualization, data analysis, the first draft of the manuscript, revision, approval of the final draft. All authors: conceptualization, design, funding acquisition, and overseeing the study, revision, and approval of the final draft. All authors have read and agreed to the published version of the manuscript.
Funding
As scholars of the Clinical Research Education and Career Development (CRECD) program at Charles R. Drew University of Medicine and Science (CDU), Drs. Adinkrah’s, Ekwegh’s, and Cobb’s research-related activities were supported by the NIMHD/NIH Award # R25 MD007610.
Institutional Review Board Statement
IRB Number = 1663247-4, IRB Date: 10/28/2020, IRB Institute: Charles R Drew University of Medicine and Science, Los Angeles, CA, USA.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare that they have no competing interest.
References
- Oakes, J.M.; Rossi, P.H. The measurement of SES in health research: Current practice and steps toward a new approach. Soc. Sci. Med. 2003, 56, 769–784. [Google Scholar] [CrossRef] [PubMed]
- Szanton, S.L.; Thorpe, R.J.; Whitfield, K. Life-course financial strain and health in African–Americans. Soc. Sci. Med. 2010, 71, 259–265. [Google Scholar] [CrossRef] [PubMed]
- Link, B.G.; Phelan, J. The social shaping of health and smoking. Drug Alcohol Depend. 2009, 104 (Suppl. S1), S6–S10. [Google Scholar] [CrossRef] [PubMed]
- Link, B.G.; Phelan, J. Social conditions as fundamental causes of disease. J. Health Soc. Behav. 1995, 80–94. [Google Scholar] [CrossRef]
- Masters, R.K.; Link, B.G.; Phelan, J.C. Trends in education gradients of ‘preventable’ mortality: A test of fundamental cause theory. Soc. Sci. Med. 2015, 127, 19–28. [Google Scholar] [CrossRef]
- Phelan, J.C.; Link, B.G.; Tehranifar, P. Social conditions as fundamental causes of health inequalities: Theory, evidence, and policy implications. J. Health Soc. Behav. 2010, 51, S28–S40. [Google Scholar] [CrossRef]
- Rodriguez, J.M.; Karlamangla, A.S.; Gruenewald, T.L.; Miller-Martinez, D.; Merkin, S.S.; Seeman, T.E. Social stratification and allostatic load: Shapes of health differences in the MIDUS study in the United States. J. Biosoc. Sci. 2019, 51, 627–644. [Google Scholar] [CrossRef]
- Mirowsky, J.; Ross, C.E. Education, Health, and the Default American Lifestyle. J. Health Soc. Behav. 2015, 56, 297–306. [Google Scholar] [CrossRef]
- Ross, C.E.; Mirowsky, J. Refining the association between education and health: The effects of quantity, credential, and selectivity. Demography 1999, 36, 445–460. [Google Scholar] [CrossRef]
- Chiu, C.T.; Hayward, M.D.; Chan, A.; Matchar, D.B. Educational differences in the compression of disability incidence in the United States. SSM Popul. Health 2019, 7, 100347. [Google Scholar] [CrossRef]
- Crimmins, E.M.; Saito, Y.; Kim, J.K.; Zhang, Y.S.; Sasson, I.; Hayward, M.D. Educational Differences in the Prevalence of Dementia and Life Expectancy with Dementia: Changes from 2000 to 2010. J. Gerontol. B Psychol. Sci. Soc. Sci. 2018, 73, S20–S28. [Google Scholar] [CrossRef]
- Montez, J.K.; Hayward, M.D.; Brown, D.C.; Hummer, R.A. Why is the educational gradient of mortality steeper for men? J. Gerontol. B Psychol. Sci. Soc. Sci. 2009, 64, 625–634. [Google Scholar] [CrossRef] [PubMed]
- Montez, J.K.; Hummer, R.A.; Hayward, M.D. Educational attainment and adult mortality in the United States: A systematic analysis of functional form. Demography 2012, 49, 315–336. [Google Scholar] [CrossRef]
- Montez, J.K.; Hummer, R.A.; Hayward, M.D.; Woo, H.; Rogers, R.G. Trends in the Educational Gradient of U.S. Adult Mortality from 1986 to 2006 by Race, Gender, and Age Group. Res. Aging 2011, 33, 145–171. [Google Scholar] [CrossRef] [PubMed]
- Montez, J.K.; Zajacova, A.; Hayward, M.D. Disparities in Disability by Educational Attainment Across US States. Am. J. Public Health 2017, 107, 1101–1108. [Google Scholar] [CrossRef] [PubMed]
- Montez, J.K.; Zajacova, A.; Hayward, M.D.; Woolf, S.H.; Chapman, D.; Beckfield, J. Educational Disparities in Adult Mortality Across U.S. States: How Do They Differ, and Have They Changed Since the Mid-1980s? Demography 2019, 56, 621–644. [Google Scholar] [CrossRef]
- Williams, D.R.; Yan, Y.; Jackson, J.S.; Anderson, N.B. Racial Differences in Physical and Mental Health: Socio-economic Status, Stress and Discrimination. J. Health Psychol. 1997, 2, 335–351. [Google Scholar] [CrossRef]
- Hill, T.D.; Needham, B.L. Gender-specific trends in educational attainment and self-rated health, 1972–2002. Am. J. Public Health 2006, 96, 1288–1292. [Google Scholar] [CrossRef]
- Zhang, Q.; Wang, Y. Trends in the association between obesity and socioeconomic status in US adults: 1971 to 2000. Obes. Res. 2004, 12, 1622–1632. [Google Scholar] [CrossRef]
- Kubzansky, L.D.; Berkman, L.F.; Glass, T.A.; Seeman, T.E. Is educational attainment associated with shared determinants of health in the elderly? Findings from the MacArthur Studies of Successful Aging. Psychosom. Med. 1998, 60, 578–585. [Google Scholar] [CrossRef]
- Levin, S.; Mayer-Davis, E.J.; Ainsworth, B.E.; Addy, C.L.; Wheeler, F.C. Racial/ethnic health disparities in South Carolina and the role of rural locality and educational attainment. South Med. J. 2001, 94, 711–718. [Google Scholar] [CrossRef] [PubMed]
- Zare, H.; Gaskin, D.D.; Thorpe, R.J., Jr. Income Inequality and Obesity among US Adults 1999–2016: Does Sex Matter? Int. J. Environ. Res. Public Health 2021, 18, 7079. [Google Scholar] [CrossRef] [PubMed]
- Zare, H.; Meyerson, N.S.; Nwankwo, C.A.; Thorpe, R.J., Jr. How Income and Income Inequality Drive Depressive Symptoms in US Adults, Does Sex Matter: 2005–2016. Int. J. Environ. Res. Public Health 2022, 19, 6227. [Google Scholar] [CrossRef] [PubMed]
- Assari, S.; Preiser, B.; Lankarani, M.M.; Caldwell, C.H. Subjective Socioeconomic Status Moderates the Association between Discrimination and Depression in African American Youth. Brain Sci. 2018, 8, 71. [Google Scholar] [CrossRef] [PubMed]
- Bound, J.; Geronimus, A.T.; Rodriguez, J.M.; Waidmann, T.A. Measuring Recent Apparent Declines in Longevity: The Role of Increasing Educational Attainment. Health Aff. 2015, 34, 2167–2173. [Google Scholar] [CrossRef] [PubMed]
- Assari, S.; Gibbons, F.X.; Simons, R. Depression among Black Youth; Interaction of Class and Place. Brain Sci. 2018, 8, 108. [Google Scholar] [CrossRef]
- Barbe, M.F.; Massicotte, V.S.; Assari, S.; Monroy, M.A.; Frara, N.; Harris, M.Y.; Amin, M.; King, T.; Cruz, G.E.; Popoff, S.N. Prolonged high force high repetition pulling induces osteocyte apoptosis and trabecular bone loss in distal radius, while low force high repetition pulling induces bone anabolism. Bone 2018, 110, 267–283. [Google Scholar] [CrossRef]
- Assari, S.; Lankarani, M.M.; Caldwell, C.H. Does Discrimination Explain High Risk of Depression among High-Income African American Men? Behav. Sci. 2018, 8, 40. [Google Scholar] [CrossRef]
- Hudson, D.L.; Bullard, K.M.; Neighbors, H.W.; Geronimus, A.T.; Yang, J.; Jackson, J.S. Are benefits conferred with greater socioeconomic position undermined by racial discrimination among African American men? J. Mens. Health 2012, 9, 127–136. [Google Scholar] [CrossRef]
- Hudson, D.L.; Neighbors, H.W.; Geronimus, A.T.; Jackson, J.S. Racial Discrimination, John Henryism, and Depression Among African Americans. J. Black Psychol. 2016, 42, 221–243. [Google Scholar] [CrossRef]
- Hudson, D.L.; Puterman, E.; Bibbins-Domingo, K.; Matthews, K.A.; Adler, N.E. Race, life course socioeconomic position, racial discrimination, depressive symptoms and self-rated health. Soc. Sci. Med. 2013, 97, 7–14. [Google Scholar] [CrossRef] [PubMed]
- Assari, S.; Moghani Lankarani, M. Workplace Racial Composition Explains High Perceived Discrimination of High Socioeconomic Status African American Men. Brain Sci. 2018, 8, 139. [Google Scholar] [CrossRef] [PubMed]
- Assari, S.; Preiser, B.; Kelly, M. Education and Income Predict Future Emotional Well-Being of Whites but Not Blacks: A Ten-Year Cohort. Brain Sci. 2018, 8, 122. [Google Scholar] [CrossRef] [PubMed]
- Assari, S.; Mistry, R.; Caldwell, C.H. Perceived Discrimination and Substance Use among Caribbean Black Youth; Gender Differences. Brain Sci. 2018, 8, 131. [Google Scholar] [CrossRef] [PubMed]
- Assari, S. Parental Educational Attainment and Mental Well-Being of College Students; Diminished Returns of Blacks. Brain Sci. 2018, 8, 193. [Google Scholar] [CrossRef] [PubMed]
- Assari, S.; Mistry, R. Educational Attainment and Smoking Status in a National Sample of American Adults; Evidence for the Blacks’ Diminished Return. Int. J. Environ. Res. Public Health 2018, 15, 763. [Google Scholar] [CrossRef]
- Assari, S.; Thomas, A.; Caldwell, C.H.; Mincy, R.B. Blacks’ Diminished Health Return of Family Structure and Socioeconomic Status; 15 Years of Follow-up of a National Urban Sample of Youth. J. Urban Health 2018, 95, 21–35. [Google Scholar] [CrossRef]
- Assari, S. The Benefits of Higher Income in Protecting against Chronic Medical Conditions Are Smaller for African Americans than Whites. Healthcare 2018, 6, 2. [Google Scholar] [CrossRef]
- Assari, S.; Caldwell, C.H. Family Income at Birth and Risk of Attention Deficit Hyperactivity Disorder at Age 15: Racial Differences. Children 2019, 6, 10. [Google Scholar] [CrossRef]
- Assari, S.; Caldwell, C.H.; Mincy, R. Family Socioeconomic Status at Birth and Youth Impulsivity at Age 15; Blacks’ Diminished Return. Children 2018, 5, 58. [Google Scholar] [CrossRef]
- Assari, S.; Cobb, S.; Saqib, M.; Bazargan, M. Economic Strain Deteriorates While Education Fails to Protect Black Older Adults Against Depressive Symptoms, Pain, Self-rated Health, Chronic Disease, and Sick Days. J. Ment. Health Clin. Psychol. 2020, 4, 49–62. [Google Scholar] [CrossRef] [PubMed]
- Spikes, T.; Murden, R.; McKinnon, I.I.; Bromfield, S.; Van Dyke, M.E.; Moore, R.H.; Rahbari-Oskoui, F.F.; Quyummi, A.; Vaccarino, V.; Lewis, T.T. Association of Net Worth and Ambulatory Blood Pressure in Early Middle-aged African American Women. JAMA Netw. Open 2022, 5, e220331. [Google Scholar] [CrossRef] [PubMed]
- Malat, J.; Mayorga-Gallo, S.; Williams, D.R. The effects of whiteness on the health of whites in the USA. Soc. Sci. Med. 2018, 199, 148–156. [Google Scholar] [CrossRef] [PubMed]
- Assari, S.; Najand, B.; Young-Brinn, A. Racial and Ethnic Differences in the Returns of Family Socioeconomic Status on Peers’ Tobacco Use. Int. J. Travel Med. Glob. Health 2022. [Google Scholar] [CrossRef]
- Assari, S. Youth Social, Emotional, and Behavioral Problems in the ABCD Study: Minorities’ Diminished Returns of Family Income. J. Econ. Public Financ. 2020, 6, 1–19. [Google Scholar] [CrossRef] [PubMed]
- Assari, S. Age-Related Decline in Children’s Reward Sensitivity: Blacks’ Diminished Returns. Res. Health Sci. 2020, 5, 112–128. [Google Scholar] [CrossRef]
- Assari, S. Dimensional Change Card Sorting of American Children: Marginalization-Related Diminished Returns of Age. Child Teenagers 2020, 3, 72–92. [Google Scholar] [CrossRef]
- Assari, S. Parental Education, Household Income, and Cortical Surface Area among 9-10 Years Old Children: Minorities’ Diminished Returns. Brain Sci. 2020, 10, 956. [Google Scholar] [CrossRef]
- Assari, S. Household Income and Children’s Depressive Symptoms: Immigrants’ Diminished Returns. Int. J. Travel Med. Glob. Health 2020, 8, 157–164. [Google Scholar] [CrossRef]
- Assari, S.; Najand, B. Immigration, Educational Attainment, and Happiness in Europe. Int. J. Travel Med. Glob. Health 2022. [Google Scholar]
- Assari, S. American Indian, Alaska Native, Native Hawaiian, and Pacific Islander Children’s Body Mass Index: Diminished Returns of Parental Education and Family Income. Res. Health Sci. 2020, 5, 64–84. [Google Scholar] [CrossRef] [PubMed]
- Assari, S. Parental Education and Nucleus Accumbens Response to Reward Anticipation: Minorities’ Diminished Returns. Adv. Soc. Sci. Cult. 2020, 2, 132–153. [Google Scholar] [CrossRef] [PubMed]
- Assari, S.; Islam, S. Diminished Protective Effects of Household Income on Internalizing Symptoms among African American than European American Pre-Adolescents. J. Econ. Trade Mark. Manag. 2020, 2, 38–56. [Google Scholar] [CrossRef] [PubMed]
- Assari, S. Parental Education and Children’s Sleep Disturbance: Minorities’ Diminished Returns. Int. J. Epidemiol. Res. 2021, 8, 31–39. [Google Scholar] [CrossRef] [PubMed]
- Ayoubian, A.; Najand, B.; Assari, S. Black Americans’ Diminished Health Returns of Employment During COVID-19 Pandemic. Int. J. Travel Med. Glob. Health 2022, 10, 114–121. [Google Scholar]
- Assari, S.; Boyce, S.; Bazargan, M.; Thomas, A.; Cobb, R.J.; Hudson, D.; Curry, T.J.; Nicholson, H.L., Jr.; Cuevas, A.G.; Mistry, R.; et al. Parental Educational Attainment, the Superior Temporal Cortical Surface Area, and Reading Ability among American Children: A Test of Marginalization-Related Diminished Returns. Children 2021, 8, 412. [Google Scholar] [CrossRef]
- Assari, S.; Caldwell, C.H. Racism, Diminished Returns of Socioeconomic Resources, and Black Middle-Income Children’s Health Paradox. JAMA Pediatr. 2021, 175, 1287–1288. [Google Scholar] [CrossRef]
- Assari, S.; Lankarani, M.M. Education and Alcohol Consumption among Older Americans; Black-White Differences. Front. Public Health 2016, 4, 67. [Google Scholar] [CrossRef]
- Assari, S. Race, Depression, and Financial Distress in a Nationally Representative Sample of American Adults. Brain Sci. 2019, 9, 29. [Google Scholar] [CrossRef]
- Laaksonen, E.; Lallukka, T.; Lahelma, E.; Ferrie, J.E.; Rahkonen, O.; Head, J.; Marmot, M.G.; Martikainen, P. Economic difficulties and physical functioning in Finnish and British employees: Contribution of social and behavioural factors. Eur. J. Public Health 2011, 21, 456–462. [Google Scholar] [CrossRef]
- Lallukka, T.; Ferrie, J.E.; Kivimaki, M.; Shipley, M.J.; Rahkonen, O.; Lahelma, E. Economic difficulties and subsequent sleep problems: Evidence from British and Finnish occupational cohorts. Sleep Med. 2012, 13, 680–685. [Google Scholar] [CrossRef] [PubMed]
- Conklin, A.I.; Forouhi, N.G.; Suhrcke, M.; Surtees, P.; Wareham, N.J.; Monsivais, P. Socioeconomic status, financial hardship and measured obesity in older adults: A cross-sectional study of the EPIC-Norfolk cohort. BMC Public Health 2013, 13, 1039. [Google Scholar] [CrossRef] [PubMed]
- Coman, E.N.; Wu, H.Z.; Assari, S. Exploring Causes of Depression and Anxiety Health Disparities (HD) by Examining Differences between 1:1 Matched Individuals. Brain Sci. 2018, 8, 207. [Google Scholar] [CrossRef] [PubMed]
- Assari, S. Self-rated Health and Mortality due to Kidney Diseases: Racial Differences in the United States. Adv. Biomed. Res. 2018, 7, 4. [Google Scholar] [CrossRef]
- Assari, S. Life Expectancy Gain Due to Employment Status Depends on Race, Gender, Education, and Their Intersections. J. Racial. Ethn. Health Disparities 2018, 5, 375–386. [Google Scholar] [CrossRef]
- DeSalvo, K.B.; Bloser, N.; Reynolds, K.; He, J.; Muntner, P. Mortality prediction with a single general self-rated health question. A meta-analysis. J. Gen. Intern. Med. 2006, 21, 267–275. [Google Scholar] [CrossRef]
- Franks, P.; Gold, M.R.; Fiscella, K. Sociodemographics, self-rated health, and mortality in the US. Soc. Sci. Med. 2003, 56, 2505–2514. [Google Scholar] [CrossRef]
- Haga, H.; Shibata, H.; Ueno, M.; Nagai, H.; Yasumura, S.; Suyama, Y.; Matsuzaki, T.; Suzuki, K.; Iwasaki, K.; Sawaguchi, S. Relationship of self-rated health to mortality among the community elderly. Nihon Koshu Eisei Zasshi 1991, 38, 783–789. [Google Scholar]
- Idler, E.L.; Angel, R.J. Self-rated health and mortality in the NHANES-I Epidemiologic Follow-up Study. Am. J. Public Health 1990, 80, 446–452. [Google Scholar] [CrossRef]
- Mossey, J.M.; Shapiro, E. Self-rated health: A predictor of mortality among the elderly. Am. J. Public Health 1982, 72, 800–808. [Google Scholar] [CrossRef]
- Schoenfeld, D.E.; Malmrose, L.C.; Blazer, D.G.; Gold, D.T.; Seeman, T.E. Self-rated health and mortality in the high-functioning elderly—A closer look at healthy individuals: MacArthur field study of successful aging. J. Gerontol. 1994, 49, M109–M115. [Google Scholar] [CrossRef] [PubMed]
- Cobb, S.; Assari, S. Investigation of the Predictors of Self-rated Health of Economically Disadvantaged African American Men and Women: Evidence for Sponge Hypothesis. Int. J. Epidemiol. Res. 2020, 7, 25–34. [Google Scholar] [CrossRef] [PubMed]
- Pikhart, H.; Bobak, M.; Siegrist, J.; Pajak, A.; Rywik, S.; Kyshegyi, J.; Gostautas, A.; Skodova, Z.; Marmot, M. Psychosocial work characteristics and self rated health in four post-communist countries. J. Epidemiol. Community Health 2001, 55, 624–630. [Google Scholar] [CrossRef] [PubMed]
- Carter, J.D.; Assari, S. Sustained Obesity and Depressive Symptoms over 6 Years: Race by Gender Differences in the Health and Retirement Study. Front. Aging Neurosci. 2016, 8, 312. [Google Scholar] [CrossRef] [PubMed]
- Assari, S.; Khoshpouri, P.; Chalian, H. Combined Effects of Race and Socioeconomic Status on Cancer Beliefs, Cognitions, and Emotions. Healthcare 2019, 7, 17. [Google Scholar] [CrossRef]
- Assari, S. Combined Racial and Gender Differences in the Long-Term Predictive Role of Education on Depressive Symptoms and Chronic Medical Conditions. J. Racial. Ethn. Health Disparities 2017, 4, 385–396. [Google Scholar] [CrossRef]
- Assari, S. Separate and Combined Effects of Anxiety, Depression and Problem Drinking on Subjective Health among Black, Hispanic and Non-Hispanic White Men. Int. J. Prev. Med. 2014, 5, 269–279. [Google Scholar]
- Assari, S. Socioeconomic Status and Self-Rated Oral Health; Diminished Return among Hispanic Whites. Dent. J. 2018, 6, 11. [Google Scholar] [CrossRef]
- Chalian, H.; Khoshpouri, P.; Assari, S. Demographic, Social, and Behavioral Determinants of Lung Cancer Perceived Risk and Worries in a National Sample of American Adults; Does Lung Cancer Risk Matter? Medicina 2018, 54, 97. [Google Scholar] [CrossRef]
- Assari, S.; Caldwell, C.H.; Zimmerman, M.A. Family Structure and Subsequent Anxiety Symptoms; Minorities’ Diminished Return. Brain Sci. 2018, 8, 97. [Google Scholar] [CrossRef]
- Assari, S.; Farokhnia, M.; Mistry, R. Education Attainment and Alcohol Binge Drinking: Diminished Returns of Hispanics in Los Angeles. Behav Sci. 2019, 9, 9. [Google Scholar] [CrossRef] [PubMed]
- Berry, B. Does money buy better health? Unpacking the income to health association after midlife. Health 2007, 11, 199–226. [Google Scholar] [CrossRef] [PubMed]
- Pasco, B. Impact of financial difficulty on health and aged care choices. Aust. Nurs. Midwifery J. 2016, 23, 30. [Google Scholar] [PubMed]
- Aslund, C.; Larm, P.; Starrin, B.; Nilsson, K.W. The buffering effect of tangible social support on financial stress: Influence on psychological well-being and psychosomatic symptoms in a large sample of the adult general population. Int. J. Equity Health 2014, 13, 85. [Google Scholar] [CrossRef] [PubMed]
- Morris, J.L.; Chasens, E.R. Financial Difficulty: A Barrier to Self-care in Patients With Diabetes. Diabetes Educ. 2017, 43, 247–248. [Google Scholar] [CrossRef]
- Financial stress linked to periodontal disease. J. Am. Dent. Assoc. 1995, 126, 1346. [CrossRef]
- Andrade, F.C.D.; Kramer, K.Z.; Monk, J.K.; Greenlee, A.J.; Mendenhall, R. Financial stress and depressive symptoms: The impact of an intervention of the Chicago Earned Income Tax Periodic Payment. Public Health 2017, 153, 99–102. [Google Scholar] [CrossRef]
- Carlsson, A.C.; Starrin, B.; Gigante, B.; Leander, K.; Hellenius, M.L.; de Faire, U. Financial stress in late adulthood and diverse risks of incident cardiovascular disease and all-cause mortality in women and men. BMC Public Health 2014, 14, 17. [Google Scholar] [CrossRef]
- Datta, B.K.; Husain, M.J.; Husain, M.M.; Kostova, D. Noncommunicable disease-attributable medical expenditures, household financial stress and impoverishment in Bangladesh. SSM Popul. Health 2018, 6, 252–258. [Google Scholar] [CrossRef]
- Adams, D.R.; Meyers, S.A.; Beidas, R.S. The relationship between financial strain, perceived stress, psychological symptoms, and academic and social integration in undergraduate students. J. Am. Coll. Health 2016, 64, 362–370. [Google Scholar] [CrossRef]
- Francoeur, R.B. Cumulative financial stress and strain in palliative radiation outpatients: The role of age and disability. Acta Oncol. 2005, 44, 369–381. [Google Scholar] [CrossRef] [PubMed]
- Palta, P.; Szanton, S.L.; Semba, R.D.; Thorpe, R.J.; Varadhan, R.; Fried, L.P. Financial strain is associated with increased oxidative stress levels: The Women’s Health and Aging Studies. Geriatr. Nurs. 2015, 36, S33–S37. [Google Scholar] [CrossRef] [PubMed]
- Sharp, L.; Carsin, A.E.; Timmons, A. Associations between cancer-related financial stress and strain and psychological well-being among individuals living with cancer. Psychooncology 2013, 22, 745–755. [Google Scholar] [CrossRef] [PubMed]
- Hanratty, B.; Holland, P.; Jacoby, A.; Whitehead, M. Financial stress and strain associated with terminal cancer—A review of the evidence. Palliat. Med. 2007, 21, 595–607. [Google Scholar] [CrossRef]
- Daly, M.; Boyce, C.; Wood, A. A social rank explanation of how money influences health. Health Psychol. 2015, 34, 222–230. [Google Scholar] [CrossRef]
- Dassah, E.; Aldersey, H.M.; McColl, M.A.; Davison, C. ‘When I don’t have money to buy the drugs, I just manage.’—Exploring the lived experience of persons with physical disabilities in accessing primary health care services in rural Ghana. Soc. Sci. Med. 2018, 214, 83–90. [Google Scholar] [CrossRef]
- Gee, S.; Vargas, J.; Foster, A.M. “We need good nutrition but we have no money to buy food”: Sociocultural context, care experiences, and newborn health in two UNHCR-supported camps in South Sudan. BMC Int. Health Hum. Rights 2018, 18, 40. [Google Scholar] [CrossRef]
- Margolis, R.; Myrskyla, M. Family, money, and health: Regional differences in the determinants of life satisfaction over the life course. Adv. Life Course Res. 2013, 18, 115–126. [Google Scholar] [CrossRef]
- Mirvis, D.M.; Klesges, L.M. Poverty and health: A simple matter of money? Tenn. Med. 1999, 92, 258–260. [Google Scholar]
- Plagerson, S.; Patel, V.; Harpham, T.; Kielmann, K.; Mathee, A. Does money matter for mental health? Evidence from the Child Support Grants in Johannesburg, South Africa. Glob. Public Health 2011, 6, 760–776. [Google Scholar] [CrossRef]
- Sinclair, R.R.; Cheung, J.H. Money Matters: Recommendations for Financial Stress Research in Occupational Health Psychology. Stress Health 2016, 32, 181–193. [Google Scholar] [CrossRef]
- Tezoquipa, I.H.; Monreal, L.A.; Trevino-Siller, S. “Without money you’re nothing”: Poverty and health in Mexico from women’s perspective. Rev. Lat. Am. Enferm. 2005, 13, 626–633. [Google Scholar] [CrossRef] [PubMed]
- Warr, D.J.; Tacticos, T.; Kelaher, M.; Klein, H. ‘Money, stress, jobs’: Residents’ perceptions of health-impairing factors in ‘poor’ neighbourhoods. Health Place 2007, 13, 743–756. [Google Scholar] [CrossRef] [PubMed]
- Siahpush, M.; Spittal, M.; Singh, G.K. Smoking cessation and financial stress. J. Public Health 2007, 29, 338–342. [Google Scholar] [CrossRef] [PubMed]
- Medical Electronics Buyers Guide Part 6. CAT scanners, electrical safety & test equipment, financial management, neonatal & pediatric equipment, pulmonary/respiratory equipment, simulators, stress test systems/ergometers. Med. Electron. 1984, 15, 116–192.
- Shah, S.J.; Krumholz, H.M.; Reid, K.J.; Rathore, S.S.; Mandawat, A.; Spertus, J.A.; Ross, J.S. Financial stress and outcomes after acute myocardial infarction. PLoS ONE 2012, 7, e47420. [Google Scholar] [CrossRef]
- Goncalves, A. Financial stress: A prognostic factor for cancer survival! Bull. Cancer 2016, 103, 318. [Google Scholar] [CrossRef]
- Eisenberg, D.; Gollust, S.E.; Golberstein, E.; Hefner, J.L. Prevalence and correlates of depression, anxiety, and suicidality among university students. Am. J. Orthopsychiatry 2007, 77, 534–542. [Google Scholar] [CrossRef]
- Carr, M.M.; Ellis, J.D.; Ledgerwood, D.M. Suicidality among gambling helpline callers: A consideration of the role of financial stress and conflict. Am. J. Addict. 2018, 27, 531–537. [Google Scholar] [CrossRef]
- Klesges, L.M.; Pahor, M.; Shorr, R.I.; Wan, J.Y.; Williamson, J.D.; Guralnik, J.M. Financial difficulty in acquiring food among elderly disabled women: Results from the Women’s Health and Aging Study. Am. J. Public Health 2001, 91, 68–75. [Google Scholar]
- Guillaumier, A.; Twyman, L.; Paul, C.; Siahpush, M.; Palazzi, K.; Bonevski, B. Financial Stress and Smoking within a Large Sample of Socially Disadvantaged Australians. Int. J. Environ. Res. Public Health 2017, 14, 231. [Google Scholar] [CrossRef] [PubMed]
- Peirce, R.S.; Frone, M.R.; Russell, M.; Cooper, M.L. Financial stress, social support, and alcohol involvement: A longitudinal test of the buffering hypothesis in a general population survey. Health Psychol. 1996, 15, 38–47. [Google Scholar] [CrossRef] [PubMed]
- Rodriguez, J.M. Health disparities, politics, and the maintenance of the status quo: A new theory of inequality. Soc. Sci. Med. 2018, 200, 36–43. [Google Scholar] [CrossRef] [PubMed]
- Simons, R.L.; Ong, M.L.; Lei, M.-K.; Klopack, E.; Berg, M.; Zhang, Y.; Philibert, R.; Beach, S.S. Unstable childhood, adult adversity, and smoking accelerate biological aging among middle-age African Americans: Similar findings for GrimAge and PoAm. J. Aging Health 2022, 34, 487–498. [Google Scholar] [CrossRef]
- Hastert, T.A.; Ruterbusch, J.J.; Abrams, J.; Nair, M.; Wenzlaff, A.S.; Beebe-Dimmer, J.L.; Pandolfi, S.S.; Schwartz, A.G. Financial hardship by age at diagnosis including in young adulthood among African American cancer survivors. Cancer Epidemiol. Biomark. Prev. 2022, 31, 876–884. [Google Scholar] [CrossRef]
- Marshall, G.L.; Bayaz-Ozturk, G.; Kahana, E.; Gallo, W.T.; Seghal, A. Dynamics of financial hardship in the United States: Health and Retirement Study 2006–2016. J. Gerontol. Soc. Work 2022, 65, 241–251. [Google Scholar] [CrossRef]
- Evans, M.C.; Bazargan, M.; Cobb, S.; Assari, S. Mental and Physical Health Correlates of Financial Difficulties Among African-American Older Adults in Low-Income Areas of Los Angeles. Front. Public Health 2020, 8, 21. [Google Scholar] [CrossRef]
- Gyamfi, P.; Brooks-Gunn, J.; Jackson, A.P. Associations between employment and financial and parental stress in low-income single black mothers. Women Health 2001, 32, 119–135. [Google Scholar] [CrossRef]
- Moran, K.E.; Ommerborn, M.J.; Blackshear, C.T.; Sims, M.; Clark, C.R. Financial Stress and Risk of Coronary Heart Disease in the Jackson Heart Study. Am. J. Prev. Med. 2019, 56, 224–231. [Google Scholar] [CrossRef]
- Logue, B.J. Women at risk: Predictors of financial stress for retired women workers. Gerontologist 1991, 31, 657–665. [Google Scholar] [CrossRef]
- Assari, S.; Boyce, S.; Bazargan, M.; Caldwell, C.H. Family Income Mediates the Effect of Parental Education on Adolescents’ Hippocampus Activation During an N-Back Memory Task. Brain Sci. 2020, 10, 520. [Google Scholar] [CrossRef] [PubMed]
- Assari, S. Parental Educational Attainment and Academic Performance of American College Students; Blacks’ Diminished Returns. J. Health Econ. Dev. 2019, 1, 21–31. [Google Scholar] [PubMed]
- Chalian, H.; Khoshpouri, P.; Assari, S. Patients’ age and discussion with doctors about lung cancer screening: Diminished returns of Blacks. Aging Med. 2019, 2, 35–41. [Google Scholar] [CrossRef] [PubMed]
- Assari, S. Parental Education and Youth Inhibitory Control in the Adolescent Brain Cognitive Development (ABCD) Study: Blacks’ Diminished Returns. Brain Sci. 2020, 10, 312. [Google Scholar] [CrossRef] [PubMed]
- Assari, S. College Graduation and Wealth Accumulation: Blacks’ Diminished Returns. World J. Educ. Res. 2020, 7, 1–18. [Google Scholar] [CrossRef] [PubMed]
- Assari, S. Parental Education and Spanking of American Children: Blacks’ Diminished Returns. World J. Educ. Res. 2020, 7, 19–44. [Google Scholar] [CrossRef] [PubMed]
- Assari, S. American Children’s Screen Time: Diminished Returns of Household Income in Black Families. Information 2020, 11, 538. [Google Scholar] [CrossRef]
- Assari, S. Mental Rotation in American Children: Diminished Returns of Parental Education in Black Families. Pediatr. Rep. 2020, 12, 130–141. [Google Scholar] [CrossRef]
- Assari, S. Protective Effects of Maternal Education against Low Birth Weight Deliveries: Blacks’ Diminished Returns. Res. Health Sci 2020, 5, 1–17. [Google Scholar] [CrossRef]
- Assari, S.; Boyce, S. Family’s Subjective Economic Status and Children’s Matrix Reasoning: Blacks’ Diminished Returns. Res. Health Sci. 2020, 6, 1–23. [Google Scholar] [CrossRef]
- Baumeister, R.F.; Bratslavsky, E.; Finkenauer, C.; Vohs, K.D. Bad is stronger than good. Rev. Gen. Psychol. 2001, 5, 323–370. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).