1000 Days: The “WeCare Generation” Program—The Ultimate Model for Improving Human Mental Health and Economics: The Study Protocol
Abstract
1. Introduction
Background
2. Materials and Methods
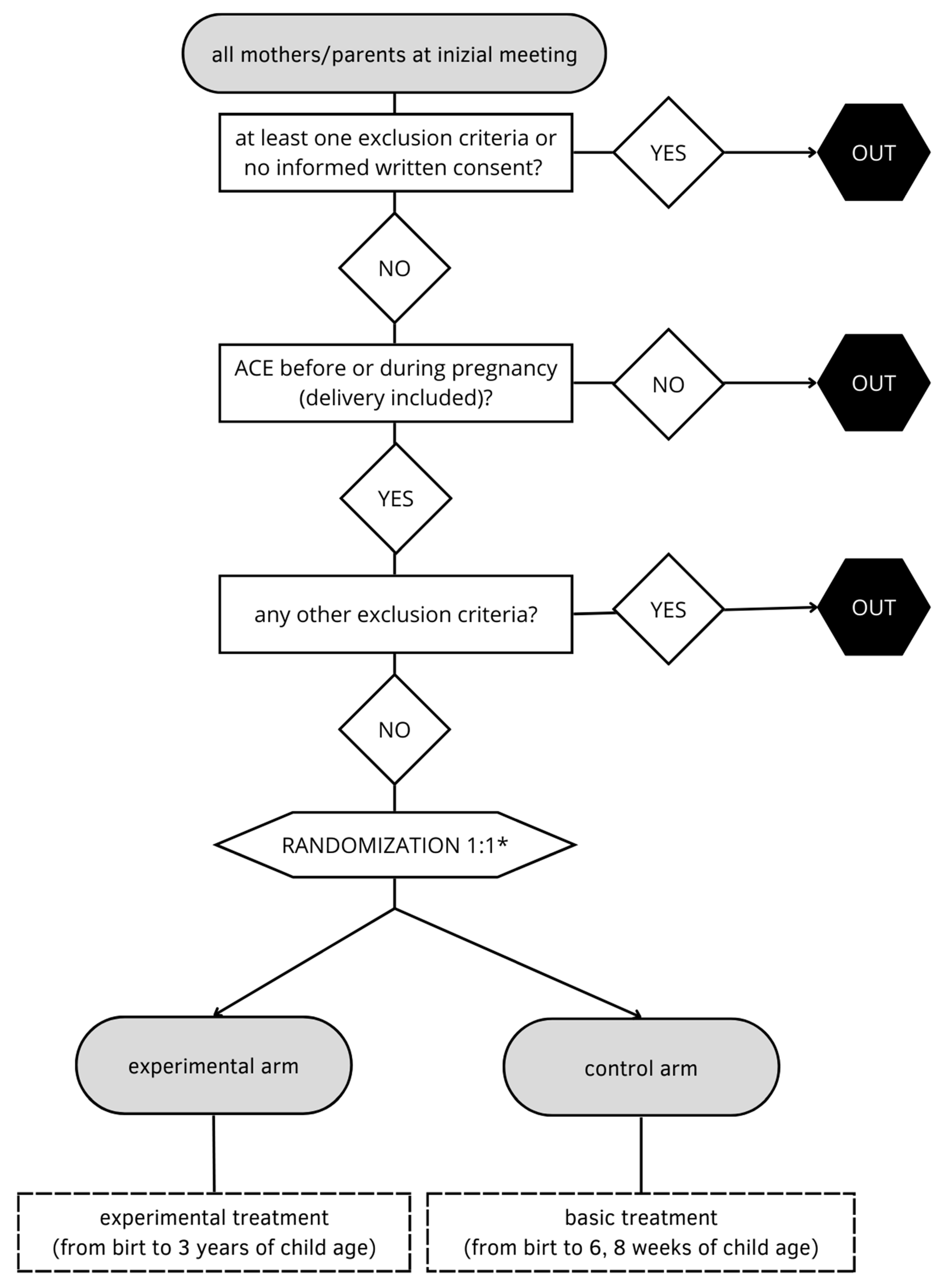
2.1. Inclusion Criteria
2.2. Exclusion Criteria
2.3. Recruitment
2.4. Trauma Detection
2.5. Randomization
2.6. Sample Size
2.7. Monitoring and Data Collection
2.8. Ethical Considerations
2.9. Intervention
2.9.1. Control Arm
2.9.2. Experimental Arm
2.10. Training
2.11. Primary and Secondary Endpoints
- Besides, it will be possible to describe difference concerning the number of children with secure attachment (at 18 months of age) [51]; differences in developmental scales (Bayley scale at 6, 18, 36 months) [52]; social outcome certification for handicap, need educator at school or home, disability certification, social-welfare benefits, skipped daycare days and sick days, how many workdays lost by parents due to parental care, number of accidents (home and non-home), prescription-drug fills, injury-insurance claims, and criminal convictions [53].
3. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Tang, L.; Gao, Y.; Qi, S.; Cui, J.; Zhou, L.; Feng, Y. Prevalence of post-traumatic stress disorder symptoms among patients with mental disorder during the COVID-19 pandemic. BMC Psychiatry 2022, 22, 156–161. [Google Scholar] [CrossRef] [PubMed]
- Brivio, E.; Oliveri, S.; Guiddi, P.; Pravettoni, G. Incidence of PTSD and generalized anxiety symptoms during the first wave of COVID-19 outbreak: An exploratory study of a large sample of the Italian population. BMC Public Health 2021, 21, 1158. [Google Scholar] [CrossRef] [PubMed]
- Bridgland, V.M.E.; Moeck, E.K.; Green, D.M.; Swain, T.L.; Nayda, D.M.; Matson, L.A.; Hutchison, N.P.; Takarangi, M.K.T. Why the COVID-19 pandemic is a traumatic stressor. PLoS ONE 2021, 16, e0240146. [Google Scholar] [CrossRef] [PubMed]
- Schou, T.M.; Joca, S.; Wegener, G.; Bay-Richter, C. Psychiatric and neuropsychiatric sequelae of COVID-19—A systematic review. Brain Behav. Immun. 2021, 97, 328–348. [Google Scholar] [CrossRef]
- Thompson, E.J.; Stafford, J.; Moltrecht, B.; Huggins, C.F.; Kwong, A.S.F.; Shaw, R.J.; Zaninotto, P.; Patel, K.; Silverwood, R.J.; McElroy, E.; et al. Psychological distress, depression, anxiety, and life satisfaction following COVID-19 infection: Evidence from 11 UK longitudinal population studies. Lancet Psychiatry 2022, 9, 894–906. [Google Scholar] [CrossRef]
- Bourmistrova, N.W.; Solomon, T.; Braude, P.; Strawbridge, R.; Carter, B. Long-term effects of COVID-19 on mental health: A systematic review. J. Affect. Disord. 2021, 299, 118–125. [Google Scholar] [CrossRef]
- Horn, M.; Wathelet, M.; Fovet, T.; Amad, A.; Vuotto, F.; Faure, K.; Astier, T.; Noël, H.; Duhem, S.; Vaiva, G.; et al. Is COVID-19 associated with posttraumatic stress disorder? J. Clin. Psychiatry 2020, 82, 20m13641. [Google Scholar] [CrossRef]
- Lotzin, A.; Krause, L.; Acquarini, E.; Ajdukovic, D.; Ardino, V.; Arnberg, F.; Böttche, M.; Bragesjö, M.; Dragan, M.; Figueire-do-Braga, M.; et al. Adjust study consortium. Risk and protective factors, stressors, and symptoms of adjustment disorder during the COVID-19 pandemic—First results of the ESTSS COVID-19 pan-European adjust study. Eur. J. Psychotraumatol. 2021, 12, 1964197. [Google Scholar] [CrossRef]
- Caroppo, E.; Mazza, M.; Sannella, A.; Marano, G.; Avallone, C.; Claro, A.E.; Janiri, D.; Moccia, L.; Janiri, L.; Sani, G. Will nothing be the same again? Changes in lifestyle during COVID-19 pandemic and consequences on mental health. Int. J. Environ. Res. Public Health 2021, 18, 8433. [Google Scholar] [CrossRef]
- Felitti, V.J.; Anda, R.F.; Nordenberg, D.; Williamson, D.F.; Spitz, A.M.; Edwards, V.; Koss, M.P.; Marks, J.S. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: The adverse childhood experiences (ACE) study. Am. J. Prev. Med. 1998, 14, 245–258. [Google Scholar] [CrossRef]
- Hillis, S.D.; Anda, R.F.; Felitti, V.J.; Nordenberg, D.; Marchbanks, P.A. Adverse childhood experiences and sexually transmitted diseases in men and women: A retrospective study. Pediatrics 2000, 106, e11. [Google Scholar] [CrossRef] [PubMed]
- Merians, A.N.; Spiller, T.; Harpaz-Rotem, I.; Krystal, J.H.; Pietrzak, R.H. Post-traumatic Stress Disorder. Med. Clin. N. Am. 2023, 107, 85–99. [Google Scholar] [CrossRef] [PubMed]
- Bellis, M.A.; Hughes, K.; Ford, K.; Rodriguez, G.R.; Sethi, D.; Passmore, J. Life course health consequences and associated annual costs of adverse childhood experiences across Europe and North America: A systematic review and meta-analysis. Lancet Public Health 2019, 4, e517–e528. [Google Scholar] [CrossRef]
- Oh, D.L.; Jerman, P.; Marques, S.S.; Koita, K.; Boparai, S.K.P.; Harris, N.B.; Bucci, M. Systematic review of pediatric health outcomes associated with childhood adversity. BMC Pediatr. 2018, 18, 83. [Google Scholar] [CrossRef] [PubMed]
- Hughes, K.; Bellis, M.A.; Hardcastle, K.A.; Sethi, D.; Butchart, A.; Mikton, C.; Jones, L.; Dunne, M.P. The effect of multiple adverse childhood experiences on health: A systematic review and meta-analysis. Lancet Public Health 2017, 2, e356–e366. [Google Scholar] [CrossRef]
- Nelson, C.A.; Scott, R.D.; Bhutta, Z.A.; Harris, N.B.; Danese, A.; Samara, M. Adversity in childhood is linked to mental and physical health throughout life. BMJ 2020, 371, m3048. [Google Scholar] [CrossRef]
- Soares, S.; Rocha, V.; Kelly-Irving, M.; Stringhini, S.; Fraga, S. Adverse childhood events and health biomarkers: A systematic review. Front. Public Health 2021, 9, 649825. [Google Scholar] [CrossRef]
- Hughes, K.; Ford, K.; Bellis, M.A.; Glendinning, F.; Harrison, E.; Passmore, J. Health and financial costs of adverse childhood experiences in 28 European countries: A systematic review and meta-analysis. Lancet Public Health 2021, 6, e848–e857. [Google Scholar] [CrossRef] [PubMed]
- Hughes, K.; Ford, K.; Kadel, R.; Sharp, C.; Bellis, M.A. Health and financial burden of adverse childhood experiences in England and Wales: A combined primary data study of five surveys. BMJ Open 2020, 10, e036374. [Google Scholar] [CrossRef]
- Doyle, O.; Harmon, C.P.; Heckman, J.J.; Tremblay, R.E. Investing in early human development: Timing and economic efficiency. Econ. Hum. Biol. 2009, 7, 1–6. [Google Scholar] [CrossRef]
- Monk, C.; Spicer, J.; Champagne, F. Linking prenatal maternal adversity to developmental outcomes in infants: The role of epigenetic pathways. Dev. Psychopathol. 2012, 24, 1361–1376. [Google Scholar] [CrossRef] [PubMed]
- Cao-Lei, L.; Massart, R.; Suderman, M.J.; Machnes, Z.; Elgbeili, G.; Laplante, D.P.; Szyf, M.; King, S. DNA methylation sig-natures triggered by prenatal maternal stress exposure to a natural disaster: Project ice storm. PLoS ONE 2014, 9, e107653. [Google Scholar] [CrossRef] [PubMed]
- Cao-Lei, L.; de Rooij, S.R.; King, S.; Matthews, S.G.; Metz, G.A.S.; Roseboom, T.J.; Szyf, M. Prenatal stress and epigenetics. Neurosci. Biobehav. Rev. 2020, 117, 198–210. [Google Scholar] [CrossRef]
- Chan, J.C.; Nugent, B.M.; Bale, T.L. Parental advisory: Maternal and paternal stress can impact offspring neurodevelopment. Biol. Psychiatry 2018, 83, 886–894. [Google Scholar] [CrossRef]
- Levy, J.; Goldstein, A.; Feldman, R. The neural development of empathy is sensitive to caregiving and early trauma. Nat. Commun. 2019, 10, 1905. [Google Scholar] [CrossRef] [PubMed]
- Morgan, C.A.; Chang, Y.-H.; Choy, O.; Tsai, M.-C.; Hsieh, S. Adverse childhood experiences are associated with reduced psychological resilience in youth: A systematic review and meta-analysis. Children 2021, 9, 27. [Google Scholar] [CrossRef] [PubMed]
- San Cristobal, P.; Santelices, M.P.; Miranda Fuenzalida, D.A. Manifestation of trauma: The effect of early traumatic experiences and adult attachment on parental reflective functioning. Front Psychol. 2017, 8, 449. [Google Scholar] [CrossRef] [PubMed]
- Yehuda, R.; Lehrner, A. Intergenerational transmission of trauma effects: Putative role of epigenetic mechanisms. World Psychiatry 2018, 17, 243–257. [Google Scholar] [CrossRef] [PubMed]
- Scorza, P.; Duarte, C.S.; Hipwell, A.E.; Posner, J.; Ortin, A.; Canino, G.; Monk, C. Program collaborators for environmental influences on child health outcomes research review: Intergenerational transmission of disadvantage: Epigenetics and parents’ childhoods as the first exposure. J. Child Psychol. Psychiatry 2019, 60, 119–132. [Google Scholar] [CrossRef]
- Alhassen, S.; Chen, S.; Alhassen, L.; Phan, A.; Khoudari, M.; De Silva, A.; Barhoosh, H.; Wang, Z.; Parrocha, C.; Shapiro, E.; et al. Intergenerational trauma transmission is associated with brain metabotranscriptome remodeling and mitochondrial dysfunction. Commun. Biol. 2021, 4, 783. [Google Scholar] [CrossRef]
- Richmond-Rakerd, L.S.; D’Souza, S.; Andersen, S.H.; Hogan, S.; Houts, R.M.; Poulton, R.; Ramrakha, S.; Caspi, A.; Milne, B.J.; Moffitt, T.E. Clustering of health, crime and social-welfare inequality in 4 million citizens from two nations. Nat. Hum. Behav. 2020, 4, 255–264. [Google Scholar] [CrossRef] [PubMed]
- Caspi, A.; Houts, R.M.; Belsky, D.W.; Harrington, H.; Hogan, S.; Ramrakha, S.; Poulton, R.; Moffitt, T. Childhood forecasting of a small segment of the population with large economic burden. Nat. Hum. Behav. 2016, 1, 5. [Google Scholar] [CrossRef]
- Gewirtz, A.; Forgatch, M.; Wieling, E. Parenting practices as potential mechanisms for child adjustment following mass trauma. J. Marital. Fam. Ther. 2008, 34, 177–192. [Google Scholar] [CrossRef] [PubMed]
- Gardner, S.; Loya, T.; Hyman, C. FamilyLive: Parental skill building for caregivers with interpersonal trauma exposures. Clin. Soc. Work, J. 2013, 42, 81–89. [Google Scholar] [CrossRef]
- Graf, N.; Zanca, R.M.; Song, W.; Zeldin, E.; Raj, R.; Sullivan, R.M. Neurobiology of parental regulation of the infant and its disruption by trauma within attachment. Front. Behav. Neurosci. 2022, 16, 806323. [Google Scholar] [CrossRef] [PubMed]
- Benoit, D.; Parker, K.C. Stability and transmission of attachment across three generations. Child Dev. 1994, 65, 1444–1456. [Google Scholar] [CrossRef] [PubMed]
- Cena, L.; Palumbo, G.; Mirabella, F.; Gigantesco, A.; Stefana, A.; Trainini, A.; Tralli, N.; Imbasciati, A. Perspectives on Early Screening and Prompt Intervention to Identify and Treat Maternal Perinatal Mental Health. Protocol for a Prospective Multicenter Study in Italy. Front. Psychol. 2020, 11, 365. [Google Scholar] [CrossRef]
- González, A.; del Río-Casanova, L.; Justo-Alonso, A. Integrating neurobiology of emotion regulation and trauma therapy: Reflections on EMDR therapy. Rev. Neurosci. 2017, 28, 431–440. [Google Scholar] [CrossRef]
- Jee, S.; Forkey, H. Maximizing the benefit of Screening for adverse childhood experiences. Pediatrics 2022, 149, e2021054624. [Google Scholar] [CrossRef]
- Farina, B.; Liotti, M.; Imperatori, C. The role of attachment trauma and disintegrative pathogenic processes in the traumatic-dissociative dimension. Front Psychol. 2019, 10, 933. [Google Scholar] [CrossRef]
- Van Ijzendoorn, M.H. Intergenerational transmission of parenting: A review of studies in nonclinical populations. Dev. Rev. 1992, 12, 76–99. [Google Scholar] [CrossRef]
- Campbell, F.; Conti, G.; Heckman, J.J.; Moon, S.H.; Pinto, R.; Pungello, E.; Pan, Y. Early childhood investments substantially boost adult health. Science 2014, 343, 1478–1485. [Google Scholar] [CrossRef] [PubMed]
- Scheinost, D.; Sinha, R.; Cross, S.N.; Kwon, S.H.; Sze, G.; Constable, R.T.; Ment, L.R. Does prenatal stress alter the developing connectome? Pediatr. Res. 2017, 81, 214–226. [Google Scholar] [CrossRef] [PubMed]
- Garcia, J.L.; Heckman, J.; Ronda, V. The lasting effects of early childhood education on promoting the skills and social mobility of disadvantaged african americans. NBER Work. Papers 2021. [Google Scholar]
- Shonkoff, J.P.; Boyce, W.T.; Levitt, P.; Martinez, F.D.; McEwen, B. Leveraging the biology of adversity and resilience to transform pediatric practice. Pediatrics 2021, 147, e20193845. [Google Scholar] [CrossRef] [PubMed]
- Houtepen, L.C.; Heron, J.; Suderman, M.J.; Fraser, A.; Chittleborough, C.R.; Howe, L.D. Associations of adverse childhood experiences with educational attainment and adolescent health and the role of family and socioeconomic factors: A prospective cohort study in the UK. PLOS Med. 2020, 17, e1003031. [Google Scholar] [CrossRef]
- Heckman, J.J.; Masterov, D.V. The productivity argument for investing in young children. Rev. Agric. Econ. Am. Agric. Econ. Assoc. 2007, 29, 446–493. [Google Scholar] [CrossRef]
- Heckman, J. The case for investing in disadvantaged young children. Ifo DICE Report 2008, 6, 3–8. [Google Scholar]
- Heckman, J.; Pinto, R.; Savelyev, P. Understanding the mechanisms through which an influential early childhood program boosted adult outcomes. Am. Econ. Rev. 2013, 103, 2052–2086. [Google Scholar] [CrossRef]
- Tracy, M.; Salo, M.; Appleton, A.A. The mitigating effects of maternal social support and paternal involvement on the inter-generational transmission of violence. Child Abuse Negl. 2018, 78, 46–59. [Google Scholar] [CrossRef]
- Sutton, T.E.; Simons, L.G.; Wickrama, K.A.S.; Futris, T. The intergenerational transmission of violence: Examining the mediating roles of insecure attachment and destructive disagreement beliefs. Violence Vict. 2014, 29, 670–687. [Google Scholar] [CrossRef] [PubMed]
- Jackson, B.J.; Needelman, H.; Roberts, H.; Willet, S.; McMorris, C. Bayley scales of infant development screening test-gross motor subtest: Efficacy in determining need for services. Pediatr. Phys. Ther. 2012, 24, 58–62. [Google Scholar] [CrossRef] [PubMed]
- Chudasama, Y.V.; Khunti, K.; Davies, M.J. Clustering of comorbidities. Futur. Health J. 2021, 8, e224–e229. [Google Scholar] [CrossRef] [PubMed]
- Garca, J.L.; Heckman, J.J.; Leaf, D.E.; Prados, M.J. Quantifying the life-cycle benefits of an influential early-childhood program. J. Polit. Econ. 2020, 128, 2502–2541. [Google Scholar] [CrossRef]
- Lotzin, A.; Acquarini, E.; Ajdukovic, D.; Ardino, V.; Böttche, M.; Bondjers, K.; Bragesjö, M.; Dragan, M.; Grajewski, P.; Figueiredo-Braga, M.; et al. Stressors, coping and symptoms of adjustment disorder in the course of the COVID-19 pandemic—study protocol of the European Society for Traumatic Stress Studies (ESTSS) pan-European study. Eur. J. Psychotraumatol. 2020, 11, 1780832. [Google Scholar] [CrossRef]
- Roubinov, D.S.; Luecken, L.J.; Curci, S.G.; Somers, J.A.; Winstone, L.K. A prenatal programming perspective on the inter-generational transmission of maternal adverse childhood experiences to offspring health problems. Am. Psychol. 2021, 76, 337–349. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Uccellini, O.; Benlodi, A.; Caroppo, E.; Cena, L.; Esposito, G.; Fernandez, I.; Ghazanfar, M.; Imbasciati, A.; Longo, F.; Mazza, M.; et al. 1000 Days: The “WeCare Generation” Program—The Ultimate Model for Improving Human Mental Health and Economics: The Study Protocol. Int. J. Environ. Res. Public Health 2022, 19, 16741. https://doi.org/10.3390/ijerph192416741
Uccellini O, Benlodi A, Caroppo E, Cena L, Esposito G, Fernandez I, Ghazanfar M, Imbasciati A, Longo F, Mazza M, et al. 1000 Days: The “WeCare Generation” Program—The Ultimate Model for Improving Human Mental Health and Economics: The Study Protocol. International Journal of Environmental Research and Public Health. 2022; 19(24):16741. https://doi.org/10.3390/ijerph192416741
Chicago/Turabian StyleUccellini, Orlando, Andrea Benlodi, Emanuele Caroppo, Loredana Cena, Gianluca Esposito, Isabel Fernandez, Maria Ghazanfar, Antonio Imbasciati, Francesco Longo, Marianna Mazza, and et al. 2022. "1000 Days: The “WeCare Generation” Program—The Ultimate Model for Improving Human Mental Health and Economics: The Study Protocol" International Journal of Environmental Research and Public Health 19, no. 24: 16741. https://doi.org/10.3390/ijerph192416741
APA StyleUccellini, O., Benlodi, A., Caroppo, E., Cena, L., Esposito, G., Fernandez, I., Ghazanfar, M., Imbasciati, A., Longo, F., Mazza, M., Marano, G., Nacinovich, R., Pignatto, A., Rolnick, A., Trivelli, M., Spada, E., & Vanzini, C. (2022). 1000 Days: The “WeCare Generation” Program—The Ultimate Model for Improving Human Mental Health and Economics: The Study Protocol. International Journal of Environmental Research and Public Health, 19(24), 16741. https://doi.org/10.3390/ijerph192416741







