Self-Management of Medication on a Cardiology Ward: Feasibility and Safety of the SelfMED Intervention
Abstract
:1. Introduction
2. Materials and Methods
2.1. Design
2.2. Participants
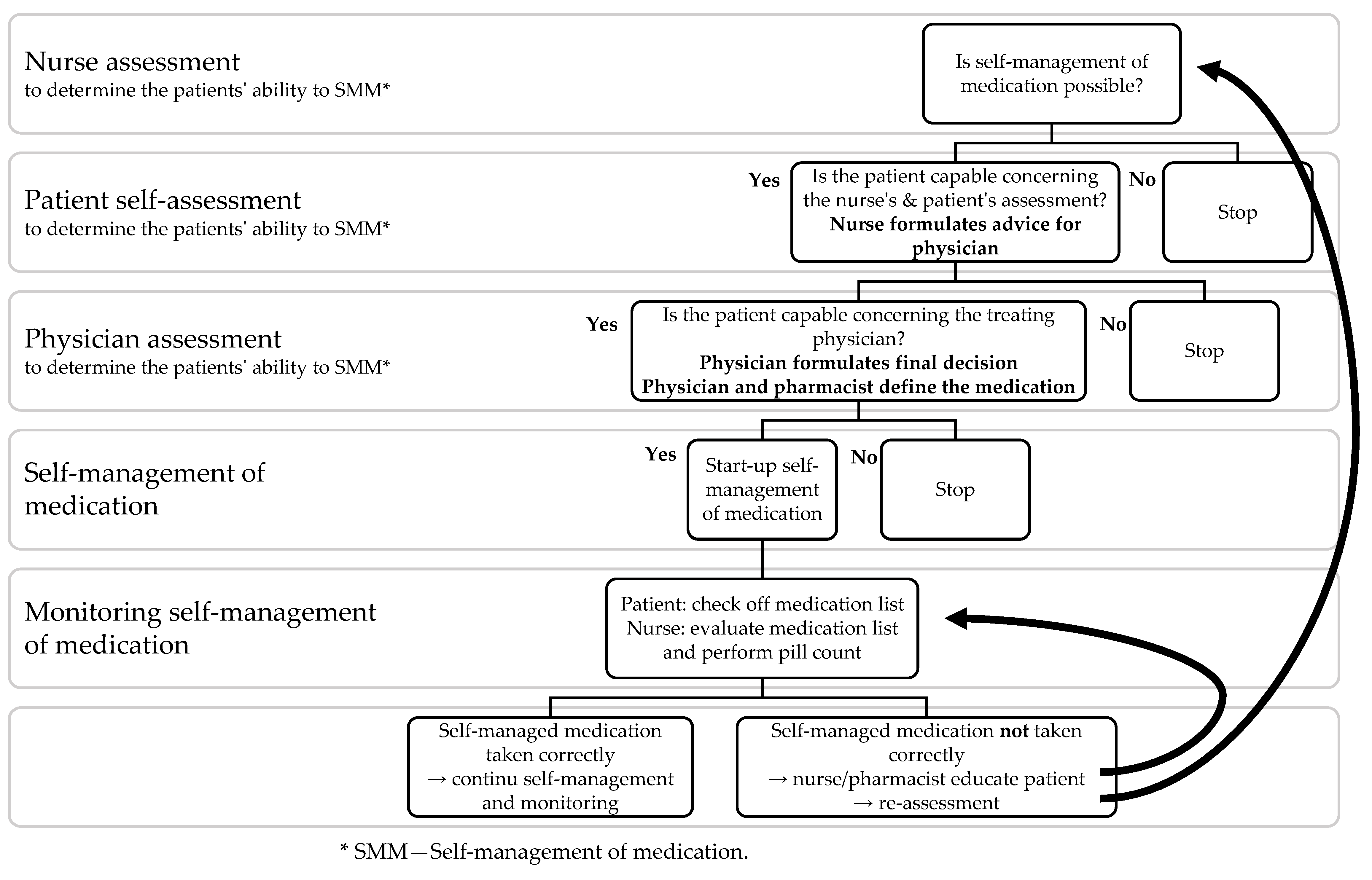
2.3. SelfMED Intervention
2.4. Study Outcomes
2.5. Data Collection
2.6. Data Analysis
3. Results
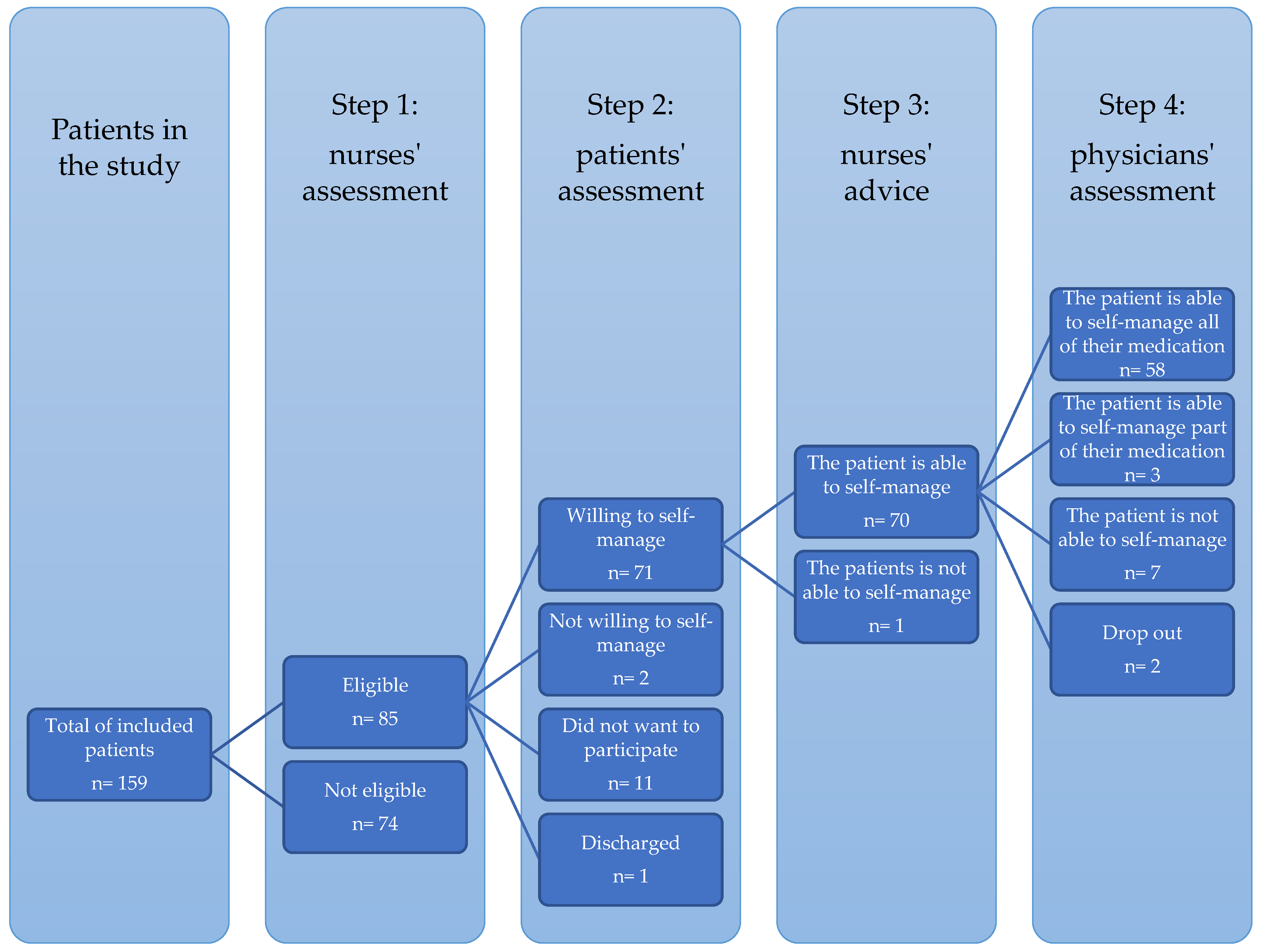
3.1. SelfMED Intervention—Feasibility
3.1.1. Level of Implementation: Assessment
3.1.2. Level of Implementation: Self-Management of Medication
3.1.3. Cross Sectional Evaluation by Cardiologists
3.2. SelfMED Intervention—Safety
3.2.1. Medication Administration Errors
3.2.2. Medication Registration Errors
4. Discussion
4.1. Main Findings
4.2. SelfMED Assessment
4.3. SelfMED Intervention—Feasibility
4.4. SelfMED Intervention—Safety
4.5. Limitations of the Study
4.6. Practice Implications
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Parnell, M.A. Medicines at the Bedside. AJN Am. J. Nurs. 1959, 59, 1417–1418. Available online: https://journals.lww.com/ajnonline/Citation/1959/10000/Medicines_at_the_Bedside.21.aspx (accessed on 15 June 2018). [PubMed]
- Davis, A.; Muir, P.; Allardice, J.-a.; Clark, K.; Groves, J.; Molenaar, M.; Robson, G. SHPA Guidelines for Self-Administration of Medication in Hospitals and Residential Care Facilities. J. Pharm. Pract. Res. 2002, 32, 324–325. [Google Scholar] [CrossRef]
- London Audit Commission. A Spoonful of Sugar: Medicines Management in NHS Hospitals. 2001. Available online: https://www.eprescribingtoolkit.com/wp-content/uploads/2020/06/nrspoonfulsugar1.pdf (accessed on 25 November 2022).
- Royal Pharmaceutical Society. The Safe and Secure Handling of Medicines: A Team Approach. 2005. Available online: https://www.rpharms.com/resources/professional-standards/safe-andsecure-handling-of-medicines (accessed on 25 November 2022).
- United Kingdom Central Council for Nursing Midwifery and Health Visiting [UKCC]. Standards for the Administration of Medicines: UKCC for Nursing Midwifery and Health Visitors; UKCC: London, UK, 2002. [Google Scholar]
- Vanwesemael, T.; Van Rompaey, B.; Petrovic, M.; Boussery, K.; Dilles, T. SelfMED: Self-Administration of Medication in Hospital: A Prevalence Study in Flanders, Belgium. J. Nurs. Scholarsh. Off. Publ. Sigma Tau Int. Honor Soc. Nurs. 2017, 49, 277–285. [Google Scholar] [CrossRef] [PubMed]
- Vanwesemael, T.; Boussery, K.; Manias, E.; Petrovic, M.; Fraeyman, J.; Dilles, T. Self-management of medication during hospitalisation: Healthcare providers’ and patients’ perspectives. J. Clin. Nurs. 2018, 27, 753–768. [Google Scholar] [CrossRef]
- Wright, J.; Emerson, A.; Stephens, M.; Lennan, E. Hospital inpatient self-administration of medicine programmes: A critical literature review. Pharm. World Sci. PWS 2006, 28, 140–151. [Google Scholar] [CrossRef]
- Richardson, S.J.; Brooks, H.L.; Bramley, G.; Coleman, J.J. Evaluating the effectiveness of self-administration of medication (SAM) schemes in the hospital setting: A systematic review of the literature. PLoS ONE 2014, 9, e113912. [Google Scholar] [CrossRef] [Green Version]
- Manias, E.; Beanland, C.J.; Riley, R.G.; Hutchinson, A.M. Development and validation of the self-administration of medication tool. Ann. Pharmacother. 2006, 40, 1064–1073. [Google Scholar] [CrossRef] [PubMed]
- Lowe, C.J.; Raynor, D.K.; Courtney, E.A.; Purvis, J.; Teale, C. Effects Of Self Medication Programme On Knowledge Of Drugs And Compliance With Treatment In Elderly Patients. BMJ: Br. Med. J. 1995, 310, 1229–1231. [Google Scholar] [CrossRef] [Green Version]
- Wood, S.I.; Calvert, R.T.; Acomb, C.; Kay, E.A. A self medication scheme for elderly patients improves compliance with their medication regimens. Int. J. Pharm. Pract. 1992, 1, 240–241. [Google Scholar] [CrossRef]
- Pereles, L.; Romonko, L.; Murzyn, T.; Hogan, D.; Silvius, J.; Stokes, E.; Long, S.; Fung, T. Evaluation of a self-medication program. J. Am. Geriatr. Soc. 1996, 44, 161–165. [Google Scholar] [CrossRef]
- Hajialibeigloo, R.; Mazlum, S.R.; Mohajer, S.; Morisky, D.E. Effect of self-administration of medication programme on cardiovascular inpatients’ medication adherence and nurses’ satisfaction: A randomized clinical trial. Nurs. Open 2021, 8, 1947–1957. [Google Scholar] [CrossRef] [PubMed]
- Kaday, R.; Ratanajamit, C. Inpatient self-administered medication under the supervision of a multidisciplinary team: A randomized, controlled, blinded parallel trial. Pharm. Pract. 2020, 18, 1766. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yang, C.; Lee, D.T.F.; Wang, X.; Chair, S.Y. Effects of a nurse-led medication self-management intervention on medication adherence and health outcomes in older people with multimorbidity: A randomised controlled trial. Int. J. Nurs. Stud. 2022, 134, 104314. [Google Scholar] [CrossRef]
- Jensen, L. Self-administered cardiac medication program evaluation. Can. J. Cardiovasc. Nurs. J. Can. En Soins Infirm. Cardio-Vasc. 2003, 13, 35–44. Available online: https://pubmed.ncbi.nlm.nih.gov/12802837/ (accessed on 22 November 2022).
- Proos, M.; Reiley, P.; Eagan, J.; Stengrevics, S.; Castile, J.; Arian, D. A study of the effects of self-medication on patients’ knowledge of and compliance with their medication regimen. J. Nurs. Care Qual. 1992, 6, 18–26. [Google Scholar] [CrossRef]
- Manias, E.; Beanland, C.; Riley, R.; Baker, L. Self-administration of medication in hospital: Patients’ perspectives. J. Adv. Nurs. 2004, 46, 194–203. [Google Scholar] [CrossRef]
- Sørensen, C.A.; Lisby, M.; Olesen, C.; Enemark, U.; Sørensen, S.B.; de Thurah, A. Self-administration of medication: A pragmatic randomized controlled trial of the impact on dispensing errors, perceptions, and satisfaction. Ther. Adv. Drug Saf. 2020, 11, 2042098620904616. [Google Scholar] [CrossRef] [PubMed]
- Glinn, J. Policy For Self Administration of Medicines (SAM) By Competent Patients. Available online: https://www.google.be/url?sa=t&rct=j&q=&esrc=s&source=web&cd=10&ved=2ahUKEwja-52P1zoAhUBDewKHfAoDSUQFjAJegQIBRAB&url=http%3A%2F%2Fwk.ixueshu.com%2Ffile%2F82cc9cf167564b1b.html&usg=AOvVaw13a1w65Dq2QTUqWqI8ikAK (accessed on 25 November 2022).
- Palmer, R.; Finnegan, T.; Darko, A. Guidelines for Patient Self-Administration of Medication (SAM). 2014. Available online: http://studylib.net/doc/8439031/patient-self-administration-ofmedicine–sam (accessed on 25 November 2022).
- Nursing and Midwifery Council. NMC Standards for Medicines Management. Available online: http://carewisesuffolk.co.uk/uploads/files/nmc-standards-for-medicines-management.pdf (accessed on 25 November 2022).
- McLeod, M.; Ahmed, Z.; Barber, N.; Franklin, B.D. A national survey of inpatient medication systems in English NHS hospitals. BMC Health Serv. Res. 2014, 14, 93. [Google Scholar] [CrossRef] [Green Version]
- Vanwesemael, T.; Dilles, T.; Van Rompaey, B.; Boussery, K. An Evidence-Based Procedure for Self-Management of Medication in Hospital: Development and Validation of the SelfMED Procedure. Pharmacy 2018, 6, 77. [Google Scholar] [CrossRef] [Green Version]
- National Coordinating Council for Medication Error Reporting and Prevention. Taxonomy of Medication Errors. Available online: https://www.nccmerp.org/taxonomy-medication-errors-now-available (accessed on 22 November 2015).
- Kim, H.Y. Statistical notes for clinical researchers: Assessing normal distribution (2) using skewness and kurtosis. Restor. Dent. Endod. 2013, 38, 52–54. [Google Scholar] [CrossRef]
- WHO. WHO Collaboration Centre for Drug Statistics Methodology. Available online: http://www.whocc.no/atc/structure_and_principles/ (accessed on 22 November 2015).
- Eibergen, L.; Janssen, M.J.A.; Blom, L.; Karapinar-Çarkit, F. Informational needs and recall of in-hospital medication changes of recently discharged patients. Res. Soc. Adm. Pharm. RSAP 2018, 14, 146–152. [Google Scholar] [CrossRef] [PubMed]
- Pollack, A.H.; Backonja, U.; Miller, A.D.; Mishra, S.R.; Khelifi, M.; Kendall, L.; Pratt, W. Closing the Gap: Supporting Patients’ Transition to Self-Management after Hospitalization. Proc. SIGCHI Conf. Hum. Factors Comput. Syst. CHI Conf. 2016, 2016, 5324–5336. [Google Scholar] [CrossRef]
| Questions in the Assessment | Positive Assessment a n = 61 % (n) | Negative Assessment b n = 98 % (n) | ||||
|---|---|---|---|---|---|---|
| Agree | Dis- Agree | Un- Known | Agree | Dis- Agree | Un- Known | |
| 98.3 (59) | 1.7 (1) | 0.0 | 51.1 (48) | 46.8 (44) | 2.1 (2) |
| 100 (61) | 0.0 | 0.0 | 78.7 (74) | 19.1 (18) | 2.1 (2) |
| 98.3 (60) | 1.7 (1) | 0.0 | 54.3 (51) | 44.7 (42) | 1.1 (1) |
| 98.4 (60) | 1.6 (1) | 0.0 | 67.3 (66) | 32.7 (32) | 0.0 |
| 100.0 (61) | 0.0 | 0.0 | 52.0 (51) | 48.0 (47) | 0.0 |
| 88.5 (54) | 9.8 (6) | 1.6 (1) | 43.3 (42) | 7.2 (7) | 49.5 (48) |
| 96.7 (59) | 3.3 (2) | 0.0 | 48.0 (47) | 49.0 (48) | 3.1 (3) |
| 96.7 (59) | 0.0 | 3.3 (2) | 86.6 (84) | 3.1 (3) | 10.3 (10) |
| 98.4 (60) | 1.6 (1) | 0 | 76.3 (74) | 18.6 (18) | 5.2 (5) |
| 100.0 (61) | 0 | 0 | 91.8 (89) | 4.1 (4) | 4.1 (4) |
| All Screened Patients (n = 158) | Self-Management Not Allowed (n = 97) | Self-Management Allowed (n = 61) | Test Statistic | p-Value | |
| Age (years) | U = 2065 | 0.001 | |||
| mean ± SD | 72.8 ± 13.6 | 75.0 ± 14.1 | 69.5 ± 12.0 | ||
| median (min–max) | 75.0 (23–95) | 79.0 (23–95) | 71.0 (45–89) | ||
| Gender (%) | X² = 0.936 | 0.333 | |||
| Female | 47.5 | 50.5 | 42.6 | ||
| Male | 52.5 | 49.5 | 57.4 | ||
| Level of education (%) | X² = 3.885 | 0.422 | |||
| None | 12.3 | 15.4 | 11.7 | ||
| Primary school | 17.8 | 15.4 | 18.3 | ||
| Secondary school | 52.1 | 69.2 | 48.3 | ||
| Bachelor level degree | 15.1 | 0.0 | 18.3 | ||
| Master level degree | 2.7 | 0.0 | 3.4 | ||
| Number of long-term medicines taken at home a | - | - | |||
| mean ± SD | 4.5 ± 3.2 | ||||
| Medication management at home (%) a | - | - | |||
| Self-management | 96.7 | ||||
| Aids used for preparation | 3.3 | ||||
| Aid for preparation and self-administration | 0.0 | ||||
| Self-management of medication during previous admission a | - | - | |||
| Yes (%) | 24.6 |
| Characteristics | Mean ± SD | Median (Min–Max) | % |
|---|---|---|---|
| Duration of patient self-management of medication (days) (n = 61) | 3.7 (1.4) | 3.0 (2–9) | |
| Number of self-managed medicines per patient during hospital stay (n= 367 a) | 5.0 (2.9) | 4.0 (1–11) | |
| Main ATC group of self-managed medicines (n = 367 a) b | |||
| A: Alimentary tract and metabolism | 6.0 | ||
| B: Blood and blood forming organs | 8.9 | ||
| C: Cardiovascular system | 21.2 | ||
| D: Dermatologicals | 0.0 | ||
| G: Genitourinary system and reproductive hormones | 0.9 | ||
| H: Systemic hormonal preparations, excluding reproductive hormones and insulins | 1.0 | ||
| J: Anti-infectives for systemic use | 0.6 | ||
| L: Antineoplastic and immunomodulating agents | 0.1 | ||
| M: Musculoskeletal system | 1.0 | ||
| N: Nervous system | 3.3 | ||
| P: Antiparasitic products, insecticides, and repellents | 0.0 | ||
| R: Respiratory system | 0.9 | ||
| S: Sensory organs | 0.6 |
| Median (Range) c | |
|---|---|
| Question on the satisfaction of …a | |
| the SelfMED procedure | 6.0 (3–7) |
| the content of the questions in the nurses’ assessment | 6.5 (6–7) |
| the content of the questions in the patient self-assessment | 6.5 (6–8) |
| the number of questions in the nurses’ assessment | 7.0 (7–8) |
| the number of questions in the patient self-assessment | 7.0 (7–8) |
| the user-friendliness of the SelfMED procedure | 6.0 (5–7) |
| the time investment to facilitate self-management of medication | 4.0 (3–5) |
| The SelfMED procedure contributes to … b | |
| better self-management of the patients’ prescribed medical therapy | 6.5 (5–8) |
| better communication between patients, nurses, and physicians concerning the prescribed medical therapy | 4.0 (3–5) |
| better understanding of patients’ competences to self-manage medication after hospital discharge | 7.0 (6,7) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vanwesemael, T.; Mortelmans, L.; Boussery, K.; Jordan, S.; Dilles, T. Self-Management of Medication on a Cardiology Ward: Feasibility and Safety of the SelfMED Intervention. Int. J. Environ. Res. Public Health 2022, 19, 16715. https://doi.org/10.3390/ijerph192416715
Vanwesemael T, Mortelmans L, Boussery K, Jordan S, Dilles T. Self-Management of Medication on a Cardiology Ward: Feasibility and Safety of the SelfMED Intervention. International Journal of Environmental Research and Public Health. 2022; 19(24):16715. https://doi.org/10.3390/ijerph192416715
Chicago/Turabian StyleVanwesemael, Toke, Laura Mortelmans, Koen Boussery, Sue Jordan, and Tinne Dilles. 2022. "Self-Management of Medication on a Cardiology Ward: Feasibility and Safety of the SelfMED Intervention" International Journal of Environmental Research and Public Health 19, no. 24: 16715. https://doi.org/10.3390/ijerph192416715
APA StyleVanwesemael, T., Mortelmans, L., Boussery, K., Jordan, S., & Dilles, T. (2022). Self-Management of Medication on a Cardiology Ward: Feasibility and Safety of the SelfMED Intervention. International Journal of Environmental Research and Public Health, 19(24), 16715. https://doi.org/10.3390/ijerph192416715








