Short- and Long-Term Effects of Underemployment on Workers’ Health: Empirical Analysis from the China Labor Force Dynamics Survey
Abstract
1. Introduction
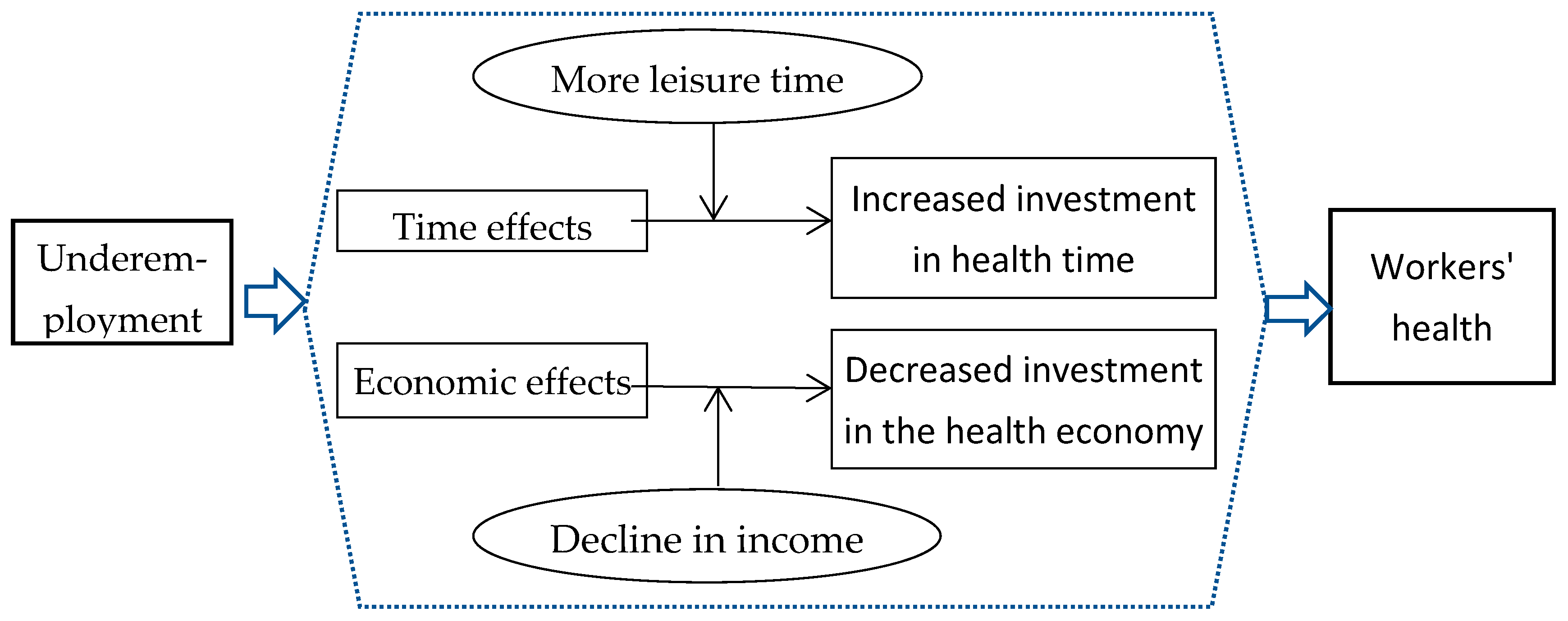
1.1. Health as a Commodity: A Theoretical Analysis
1.2. Underemployment and Health: A Literature Review
2. Materials and Methods
2.1. Data Sources
2.2. Model Setting and Variable Selection
2.2.1. Dependent Variables
2.2.2. Core Variables
2.2.3. Control Variables
3. Results
3.1. Descriptive Statistical Analysis
3.2. Short-Term Effects of Underemployment on Workers’ Health
3.3. Endogenous Processing
3.3.1. Propensity Score Matching
3.3.2. Instrumental Variable Method
3.4. Robustness Test
3.5. Long-Term Effects of Underemployment on Workers’ Self-Rated Health
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Thompson, T.; Shea, T.; Sikora, D.; Perrewé, P.; Ferris, G. Rethinking underemployment and overqualification in organizations: The not so ugly truth. Bus. Horiz. 2013, 56, 113–121. [Google Scholar] [CrossRef]
- Bell, D.N.F.; Blanchflower, D.G. Underemployment in the United States and Europe. ILR Rev. 2019, 74, 56–94. [Google Scholar] [CrossRef]
- Wilkins, R. The consequences of underemployment for the underemployed. J. Ind. Relat. 2007, 49, 247–275. [Google Scholar] [CrossRef]
- McKee-Ryan, F.M.; Harvey, J. “I have a job, but...”: A review of underemployment. J. Manag. 2011, 37, 962–996. [Google Scholar] [CrossRef]
- Barnichon, R.; Zylberberg, Y. Underemployment and the trickle-down of unemployment. Am. Econ. J. Macroecon. 2019, 11, 40–78. [Google Scholar] [CrossRef]
- Mushkin, S.J. Health as an investment. J. Political Econ. 1962, 70, 129–157. [Google Scholar] [CrossRef]
- Qi, X. Where does the time go? Gender differences in time use over the life course in China. J. Chin. Women’s Stud. 2018, 4, 19–32. [Google Scholar]
- Miller, D.L.; Page, M.E.; Stevens, A.H.; Filipski, M. Why are recessions good for your Health? Am. Econ. Rev. 2009, 99, 122–127. [Google Scholar] [CrossRef]
- Berkman, L.F.; Kawachi, I. A historical framework for social epidemiology. In Social Epidemiology; Berkman, L.F., Kawachi, I., Eds.; Oxford University Press: New York, NY, USA, 2000; pp. 3–12. [Google Scholar]
- Porath, C.; Spreitzer, G.; Gibson, C.; Garnett, F.G. Thriving at work: Toward its measurement, construct validation, and theoretical refinement. J. Organ. Behav. 2012, 33, 250–275. [Google Scholar] [CrossRef]
- Lilius, J.M. Recovery at Work: Understanding the restorative side of “depleting” client interactions. Acad. Manag. Rev. 2012, 4, 569–588. [Google Scholar] [CrossRef]
- Grossman, M. On the concept of health capital and the demand for health. J. Political. Econ. 1972, 80, 223–255. [Google Scholar] [CrossRef]
- Kuhn, A.; Lalive, R.; Zweimüller, J. The public health costs of job loss. J. Health Econ. 2009, 28, 1099–1115. [Google Scholar] [CrossRef] [PubMed]
- Eliason, M.; Storrie, D. Lasting or latent scars? Swedish evidence on the long-term effects of job displacement. J. Labor Econ. 2006, 24, 831–856. [Google Scholar] [CrossRef]
- Feinstein, J.S. The Relationship between socioeconomic status and health: A review of the literature. Milbank Q. 1993, 71, 279–322. [Google Scholar] [CrossRef] [PubMed]
- Nussbaum, M.; Sen, A. The Quality of Life; Oxford University Press: New York, NY, USA, 1993. [Google Scholar]
- Kessler, R.C.; House, J.S.; Turner, J.B. Unemployment and health in a community sample. J. Health Soc. Behav. 1987, 28, 51–59. [Google Scholar] [CrossRef] [PubMed]
- Allan, B.A.; Taewon, K.; Shein, B. Underemployment and mental health: A longitudinal study. J. Couns. Psychol. 2022, 69, 578–588. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.O.; Kapteyn, A.; Clomax, A.; Jin, H. Estimating influences of unemployment and underemployment on mental health during the COVID-19 pandemic: Who suffers the most? Public Health 2021, 201, 48–54. [Google Scholar] [CrossRef]
- Jahoda, M. Work, employment, and unemployment: Values, theories, and approaches in social research. Am. Psychol. 1981, 36, 184–191. [Google Scholar] [CrossRef]
- Wu, W. The effect of working hours on occupational well-being—An empirical analysis based on three typical occupations. China Ind. Econ. 2016, 130–145. [Google Scholar] [CrossRef]
- Siegrist, J. Adverse health effects of high-effort/low-reward conditions. J. Occup. Health Psychol. 1996, 1, 27–41. [Google Scholar] [CrossRef]
- Kim, J.; Golden, L. Inadequacy inequality: The distribution and consequences of part-time underemployment in the US. Community Work Fam. 2022, 25, 84–111. [Google Scholar] [CrossRef]
- Kaur, M.; Goyal, P.; Goyal, M. Individual, interpersonal and economic challenges of underemployment in the wake of COVID-19. Work 2020, 67, 21–28. [Google Scholar] [CrossRef] [PubMed]
- Beiser, M.; Johnson, P.J.; Turner, R.J. Unemployment, underemployment and depressive affect among Southeast Asian refugees. Psychol. Med. 1993, 23, 731–743. [Google Scholar] [CrossRef]
- Becker, S.O.; Ichino, A. Estimation of average treatment effects based on propensity scores. Stata J. 2002, 2, 358–377. [Google Scholar] [CrossRef]
- Chen, Q. Advanced Econometrics and Stata Application; Higher Education Press: Beijing, China, 2014. [Google Scholar]
- Zavodny, M. The effect of the minimum wage on employment and hours. Labour Econ. 2000, 7, 729–750. [Google Scholar] [CrossRef]
- Radloff, L.S. The CES-D Scale: A self-report depression scale for research in the general population. Appl. Psychol. Meas. 1977, 1, 385–401. [Google Scholar] [CrossRef]
- Otterbach, S.; Wooden, M.; Fok, Y.K. Working-Time mismatch and mental health. Melb. Inst. Work. Study 2016, 11, 1–42. [Google Scholar] [CrossRef][Green Version]
- Li, Y.; Zhang, S. “Workplace Tightrope”—The impact of overtime work on the health of employed persons and its gender differences. Popul. Econ. 2020, 1, 16–28. [Google Scholar]
- Stolzenberg, R.M. It’s about time and gender: Spousal employment and health. Am. J. Sociol. 2001, 107, 61–100. [Google Scholar] [CrossRef]
- Jin, S.-H. What makes education therapeutic—And the relationship between education and human health. Educ. Res. 2020, 41, 34–44. [Google Scholar]
- Sun, B.W.; Li, X.; Wu, X. Study on the health promotion effect of social capital. China Popul. Sci. 2016, 6, 98–106. [Google Scholar]
- Ding, S.; Liu, C. The impact of informal employment on residents’ health—An empirical analysis from the China Labor Force Dynamics Survey. J. China Inst. Labor Rel. 2016, 12, 45–55. [Google Scholar]
- Su, Z.; Zhang, Y. The impact of income inequality on rural residents’ health—Validation of a micro perspective based on relative deprivation. Agri. Technol. Econ. 2021, 3, 132–144. [Google Scholar] [CrossRef]
- Wang, W.W.; Fan, C.C. Migrant workers’ integration in urban China: Experiences in employment, social adaptation, and self-identity. Eurasian Geogr. Econ. 2012, 53, 731–749. [Google Scholar] [CrossRef]
- Fein, E.C.; Skinner, N. Clarifying the effect of work hours on health through work-life conflict. Asia Pac. J. Hum. Resour. 2015, 53, 448–470. [Google Scholar] [CrossRef]
- He, M.; Ding, J. Evaluation of health risk smoothing effect of health insurance affordability—A study based on low and middle income insured groups. Dyn. Econ. 2022, 4, 83–102. [Google Scholar]
- Li, S.; Zhu, M.B.; Zhan, P. Income redistribution effect of China’s social security system. Soc. Secur. Rev. 2017, 4, 3–20. [Google Scholar]
- Di Tella, R.; MacCulloch, R.J.; Oswald, A.J. The macroeconomics of happiness. Rev. Econ. Stat. 2003, 85, 809–827. [Google Scholar] [CrossRef]
- Wang, X.J.; Zheng, C. The impact of medical insurance on medical expenditures and health of the elderly. Financ. Res. 2014, 40, 65–75. [Google Scholar] [CrossRef]
- Chang, X.; Su, Q.; Zhou, C. The impact of urban and rural medical insurance coordination on residents’ health. China Popul. Sci. 2018, 6, 103–114. [Google Scholar]
- Wang, Q.F.; Tetiana, L. Immigrant underemployment across US metropolitan areas: From a spatial perspective. Urban Stud. 2014, 51, 2202–2218. [Google Scholar] [CrossRef]
| Type | Variable Name | Variable Interpretation and Assignment | CLDS 2016 | CLDS 2014 | |||
|---|---|---|---|---|---|---|---|
| Average Value | Standard Deviation | Average Value | Standard Deviation | ||||
| Dependent variable | Health Status | Self-assessment of health | 1 = Very unhealthy; 2 = Rather unhealthy; 3 = Fair; 4 = Healthy; 5 = Very healthy | 3.721 | 0.935 | 3.783 | 0.915 |
| Mental Health | 1 = depressive tendency; 0 = no depressive tendency | 0.153 | 0.360 | 0.456 | 0.498 | ||
| Prevalence of illness over a certain period of time | 1 = Physical pain in the past month; 0 = No physical pain in the past month | 0.304 | 0.460 | 0.285 | 0.452 | ||
| Core Variables | Insufficient Employment | 1 = underemployed; 0 = other | 0.103 | 0.303 | 0.035 | 0.185 | |
| Control Variables | Individuals Features | Gender | 1 = female; 0 = male | 0.453 | 0.498 | 0.441 | 0.497 |
| Age | Actual age (years) | 41.890 | 10.356 | 41.460 | 10.200 | ||
| Education level | 1 = Elementary school and below; 2 = Junior high school; 3 = High School; 4 = College; 5 = Bachelor’s and above | 2.269 | 1.173 | 2.295 | 1.199 | ||
| Appearance | 1–10, 10 is the “highest” value | 6.449 | 1.504 | 6.435 | 1.455 | ||
| Account | 1 = non-farm household; 0 = agricultural household | 0.258 | 0.437 | 0.281 | 0.449 | ||
| Marriage | 1 = first marriage + remarriage; 0 = other | 0.866 | 0.340 | 0.874 | 0.332 | ||
| Economy Status Features | Housing Sources | 1 = owned property; 0 = other | 0.510 | 0.500 | 0.841 | 0.366 | |
| Household income | 10,000 RMB | 6.685 | 10.212 | 6.178 | 8.512 | ||
| Personal income | 10,000 RMB | 3.541 | 6.271 | 3.126 | 4.757 | ||
| Life Habit Features | Smoking | 1 = yes; 0 = no | 0.297 | 0.457 | 0.303 | 0.459 | |
| Drinking | 1 = drinks alcohol every day; 0 = no | 0.075 | 0.263 | 0.230 | 0.421 | ||
| Regular exercise | 1 = yes; 0 = no | 0.287 | 0.452 | 0.197 | 0.398 | ||
| Jobs Features | Occupation Type | 1 = employed by others; 0 = other | 0.467 | 0.499 | 0.476 | 0.499 | |
| Workforce Category | 1 = transitory workforce; 0 = permanent employment | 0.137 | 0.344 | 0.097 | 0.296 | ||
| Workplace | 1 = indoor, workshop, office, home, collectively, and indoor; 0 = other | 0.529 | 0.499 | 0.486 | 0.500 | ||
| Industry Properties | 1 = primary sector; 2 = secondary sector; 3 = tertiary sector | 1.998 | 0.883 | 1.968 | 0.871 | ||
| Enrollment Features | Medical Insurance | 1 = yes; 0 = no | 0.922 | 0.269 | 0.877 | 0.328 | |
| Old-age insurance | 1 = yes; 0 = no | 0.655 | 0.475 | 0.585 | 0.493 | ||
| Unemployment Insurance | 1 = yes; 0 = no | 0.179 | 0.383 | 0.173 | 0.378 | ||
| N | 10,563 | 9703 | |||||
| Variables | Underemployment I | Full Employment II | Overemployment III | I VS. II | I VS. III | II VS. III | |
|---|---|---|---|---|---|---|---|
| Self-assessment of health | 1 = unhealthy, 0 = healthy | 0.161 (0.007) | 0.073 (0.005) | 0.095 (0.004) | −0.088 *** | −0.066 *** | 0.021 *** |
| Depressive tendencies | 1 = yes, 0 = no | 0.166 (0.004) | 0.122 (0.006) | 0.138 (0.012) | −0.044 *** | −0.028 ** | 0.016 |
| Prevalence of illness over a certain period of time | 1 = yes, 0 = no | 0.361 (0.010) | 0.255 (0.008) | 0.302 (0.006) | −0.106 *** | −0.058 *** | 0.047 ** |
| Variables | Self-Assessment of Health | Mental Health | Prevalence of Illness over a Certain Period of Time |
|---|---|---|---|
| Underemployment | 0.244 ** (0.096) | 0.284 *** (0.083) | 0.291 *** (0.071) |
| Gender | 0.120 (0.088) | 0.443 *** (0.071) | 0.428 *** (0.057) |
| Age | 0.604 *** (0.044) | 0.106 *** (0.033) | 0.381 *** (0.027) |
| Education level | −0.191 *** (0.051) | −0.030 (0.036) | −0.074 ** (0.029) |
| Account | 0.096 (0.126) | 0.093 (0.089) | 0.043 (0.072) |
| Appearance | −0.125 *** (0.024) | −0.099 *** (0.020) | −0.042 *** (0.016) |
| Marital Status | −0.097 (0.128) | −0.408 *** (0.086) | −0.181 ** (0.075) |
| Personal Income | −0.127 *** (0.021) | −0.007 (0.008) | −0.003 (0.005) |
| Household Income | −0.036 *** (0.010) | −0.007 (0.005) | −0.002 (0.003) |
| Housing | 0.024 (0.071) | 0.089 (0.058) | 0.030 (0.047) |
| Smoking | −0.183 * (0.094) | 0.076 (0.078) | −0.046 (0.061) |
| Drinking | −0.155 (0.125) | −0.065 (0.113) | −0.054 (0.086) |
| Regular Exercise | 0.001 (0.089) | −0.178 *** (0.069) | −0.039 (0.054) |
| Occupation Type | −0.313 *** (0.114) | 0.014 (0.082) | −0.171 *** (0.064) |
| Workplace | 0.115 (0.109) | 0.015 (0.080) | 0.163 *** (0.063) |
| Industry Type | −0.203 *** (0.067) | −0.103 ** (0.050) | −0.088 ** (0.039) |
| Workforce Type | −0.026 (0.131) | 0.187 ** (0.090) | 0.016 (0.073) |
| Medical Insurance | −0.045 (0.132) | −0.091 (0.103) | −0.168 * (0.086) |
| Old-age Insurance | −0.054 (0.077) | −0.132 ** (0.064) | 0.170 *** (0.052) |
| Unemployment Insurance | 0.208 (0.159) | 0.002 (0.102) | −0.062 (0.080) |
| Regional Fixed Effects | Controlled | Controlled | Controlled |
| Constant term | 0.652 (0.487) | 0.335 (0.344) | 0.794 *** (0.286) |
| pseudo R2 | 0.157 | 0.035 | 0.070 |
| N | 10563 | 10563 | 10563 |
| Health Status | Matching Method | Processing Group | Control Group | ATT Estimate | Bootstrap Standard Error | T-Value |
|---|---|---|---|---|---|---|
| Self-rated health (1 = unhealthy, 0 = healthy) | Nuclear matching | 0.169 | 0.140 | 0.029 | 0.012 | 2.42 ** |
| K-Nearest Neighbor Matching | 0.169 | 0.148 | 0.021 | 0.013 | 1.74 * | |
| Mental health (1 = depressive tendency, 0 = no depressive tendency) | Nuclear matching | 0.213 | 0.166 | 0.048 | 0.013 | 3.63 *** |
| K-Nearest Neighbor Matching | 0.213 | 0.160 | 0.053 | 0.017 | 3.07 *** | |
| Prevalence of illness over a certain period of time (1 = sick, 0 = not sick) | Nuclear matching | 0.398 | 0.340 | 0.058 | 0.016 | 3.65 *** |
| K-Nearest Neighbor Matching | 0.398 | 0.341 | 0.057 | 0.021 | 2.67 *** |
| Variables | Self-Assessment of Health | Mental Health | Prevalence of Illness over a Certain Period of Time |
|---|---|---|---|
| Underemployment | 3.193 *** (0.186) | 2.847 *** (0.681) | 2.690 *** (0.520) |
| Control variables | Controlled | Controlled | Controlled |
| Regional fixed effects | Controlled | Controlled | Controlled |
| Constant term | 0.360 (0.239) | −1.000 *** (0.117) | −1.099 *** (0.108) |
| N | 10,563 | 10,563 | 10,430 |
| Variables | Self-Assessment of Health | Mental Health | Prevalence of Illness over a Certain Period of Time |
|---|---|---|---|
| Underemployment | 0.783 *** (0.154) | 0.789 *** (0.118) | 0.423 *** (0.121) |
| Control variables | Controlled | Controlled | Controlled |
| Regional fixed effects | Controlled | Controlled | Controlled |
| pseudo R2 | 0.153 | 0.039 | 0.075 |
| N | 9703 | 9703 | 9703 |
| Variables | Self-Assessment of Health | Mental Health | Prevalence of Illness over a Certain Period of Time |
|---|---|---|---|
| Underemployment | −0.186 (0.272) | 0.410 * (0.213) | −0.134 (0.195) |
| Control variables | Controlled | Controlled | Controlled |
| Regional fixed effects | Controlled | Controlled | Controlled |
| pseudo R2 | 0.159 | 0.045 | 0.073 |
| Sample size | 4713 | 4713 | 4713 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Li, N.; Liang, H.; Gao, Y.; Wu, D. Short- and Long-Term Effects of Underemployment on Workers’ Health: Empirical Analysis from the China Labor Force Dynamics Survey. Int. J. Environ. Res. Public Health 2022, 19, 16695. https://doi.org/10.3390/ijerph192416695
Li N, Liang H, Gao Y, Wu D. Short- and Long-Term Effects of Underemployment on Workers’ Health: Empirical Analysis from the China Labor Force Dynamics Survey. International Journal of Environmental Research and Public Health. 2022; 19(24):16695. https://doi.org/10.3390/ijerph192416695
Chicago/Turabian StyleLi, Nan, Huanhuan Liang, Yi Gao, and Dan Wu. 2022. "Short- and Long-Term Effects of Underemployment on Workers’ Health: Empirical Analysis from the China Labor Force Dynamics Survey" International Journal of Environmental Research and Public Health 19, no. 24: 16695. https://doi.org/10.3390/ijerph192416695
APA StyleLi, N., Liang, H., Gao, Y., & Wu, D. (2022). Short- and Long-Term Effects of Underemployment on Workers’ Health: Empirical Analysis from the China Labor Force Dynamics Survey. International Journal of Environmental Research and Public Health, 19(24), 16695. https://doi.org/10.3390/ijerph192416695





