Effects of Adding an Online Exercise Program on Physical Function in Individuals Hospitalized by COVID-19: A Randomized Controlled Trial
Abstract
1. Introduction
2. Methods
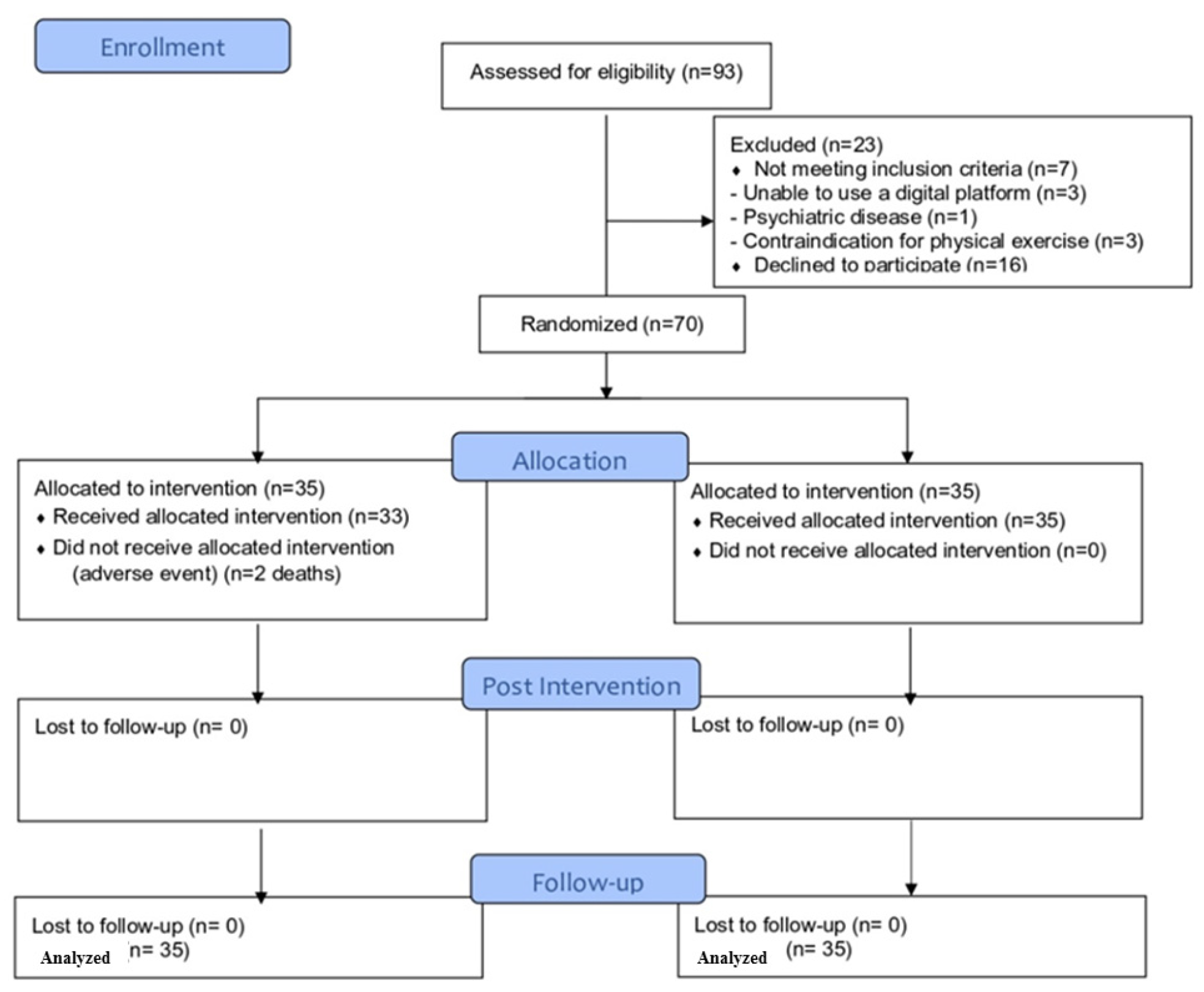
2.1. Study Design
2.2. Participants
2.3. Randomization and Masking
2.4. Outcomes
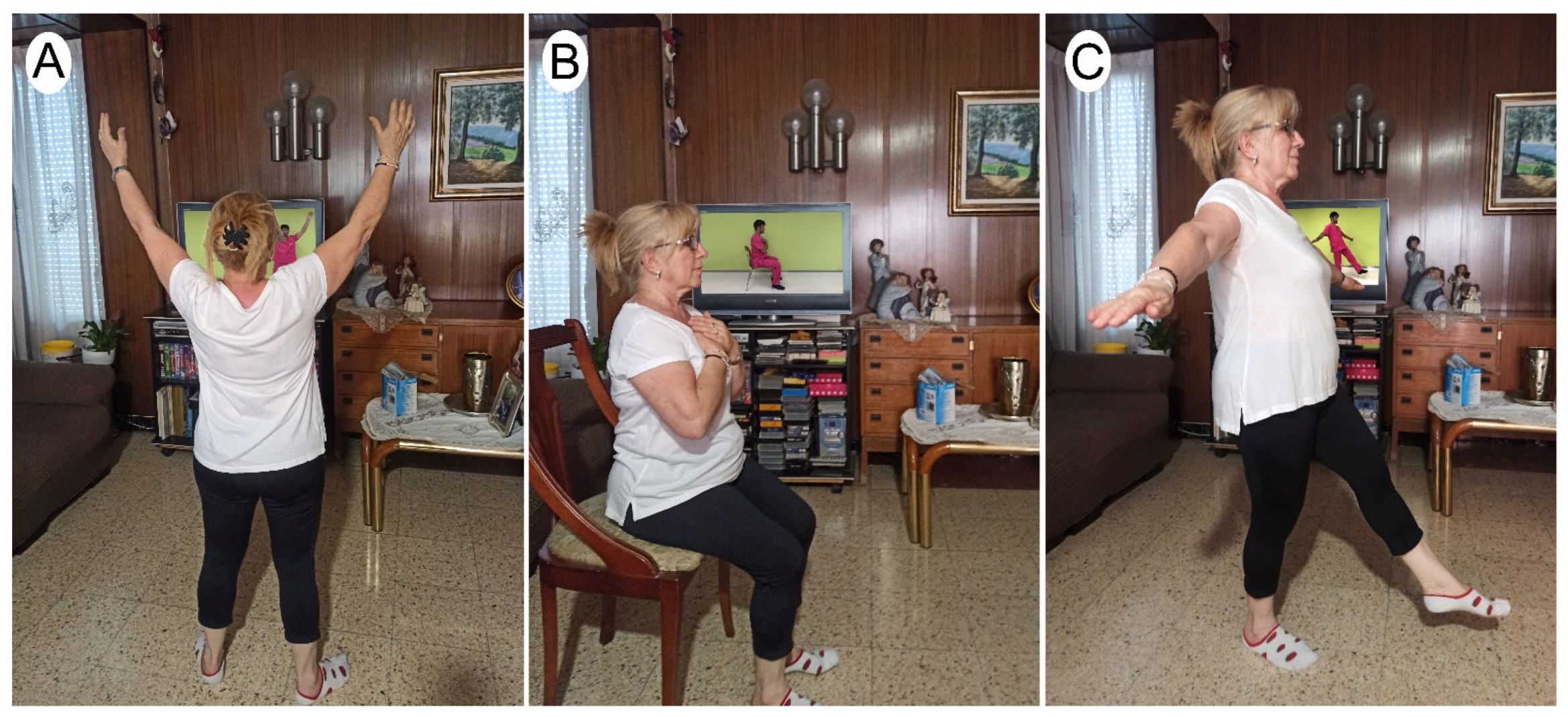
2.5. Interventions
2.6. Study Procedure
- -
- Respiratory frequency < 40 breaths per minute;
- -
- Heart rate < 120 beats/minute in resistance exercises and < 140 beats/minute in intervallic exercises;
- -
- Sp02 < 90%.
2.7. Sample Size Calculation
2.8. Statistical Analysis
3. Results
3.1. Primary Outcome
3.2. Secondary Outcomes
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Karadag, E. Increase in COVID-19 Cases and Case-fatality and Case-recovery Rates in Europe: A Cross-temporal Meta-analysis. J. Med. Virol. 2020, 92, 1511–1517. [Google Scholar] [CrossRef] [PubMed]
- Ito, G.; Rodrigues, V.; Hümmelgen, J.; Meschino, G.; Abou-Rejaile, G.; Brenny, I.; de Castro Júnior, C.; Artigas, R.; Munhoz, J.; Cardoso, G.; et al. COVID-19 Pathophysiology and Ultrasound Imaging: A Multiorgan Review. J. Clin. Ultrasound. 2022, 50, 326–338. [Google Scholar] [CrossRef] [PubMed]
- Diaz Ballve, L.; Da rgains, N.; Inchaustegui, J.; Bratos, A.; Ardariz, C.; Al, E. Weakness Acquired in the Intensive Care Unit. Incidence, Risk Factors and Their Association with Inspiratory Weakness. Observational Cohort Study. Rev. Bras. Ter. Intensiv. 2017, 29, 466. [Google Scholar] [PubMed]
- Hodgson, C.L.; Tipping, C.J. Physiotherapy Management of Intensive Care Unit-Acquired Weakness. J. Physiother. 2017, 63, 4–10. [Google Scholar] [CrossRef] [PubMed]
- Frota, A.X.; Vieira, M.C.; Soares, C.C.S.; da Silva, P.S.; da Silva, G.M.S.; de Souza Nogueira Sardinha Mendes, F.; Mazzoli-Rocha, F.; Veloso, H.H.; da Costa, A.D.; da Cruz Lamas, C.; et al. Functional Capacity and Rehabilitation Strategies in Covid-19 Patients: Current Knowledge and Challenges. Rev. Soc. Bras. Med. Trop 2021, 54, 1–8. [Google Scholar] [CrossRef]
- Torres-Castro, R.; Vasconcello-Castillo, L.; Alsina-Restoy, X.; Solis-Navarro, L.; Burgos, F.; Puppo, H.; Vilaró, J. Respiratory Function in Patients Post-Infection by COVID-19: A Systematic Review and Meta-Analysis. Pulmonology 2021, 27, 328. [Google Scholar] [CrossRef]
- Desai, S.V.; Law, T.J.; Needham, D.M. Long-Term Complications of Critical Care. Crit. Care Med. 2011, 39, 371–379. [Google Scholar] [CrossRef]
- Rooney, S.; Webster, A.; Paul, L. Systematic Review of Changes and Recovery in Physical Function and Fitness After Severe Acute Respiratory Syndrome–Related Coronavirus Infection: Implications for COVID-19 Rehabilitation. Phys. Ther. 2020, 100, 1717–1729. [Google Scholar] [CrossRef]
- Barker, K.; Eickmeyer, S. Therapeutic Exercise. Med. Clin. North. Am. 2020, 104, 189–198. [Google Scholar] [CrossRef]
- Pahor, M.; Guralnik, J.M.; Ambrosius, W.T.; Blair, S.; Bonds, D.E.; Church, T.S.; Espeland, M.A.; Fielding, R.A.; Gill, T.M.; Groessl, E.J.; et al. Effect of Structured Physical Activity on Prevention of Major Mobility Disability in Older Adults. JAMA 2014, 311, 2387. [Google Scholar] [CrossRef]
- Moore, J.L.; Nordvik, J.E.; Erichsen, A.; Rosseland, I.; Bø, E.; Hornby, T.G.; Barkenæs, T.; Bratlie, H.; Byhring, M.; Grimstad, I.; et al. Implementation of High-Intensity Stepping Training During Inpatient Stroke Rehabilitation Improves Functional Outcomes. Stroke 2020, 51, 563–570. [Google Scholar] [CrossRef] [PubMed]
- Billinger, S.A.; Arena, R.; Bernhardt, J.; Eng, J.J.; Franklin, B.A.; Johnson, C.M.; Mackay-Lyons, M.; Macko, R.F.; Mead, G.E.; Roth, E.J.; et al. Physical Activity and Exercise Recommendations for Stroke Survivors: A Statement for Healthcare Professionals from the American Heart Association/American Stroke Association. Stroke 2014, 45, 2532–2553. [Google Scholar] [CrossRef] [PubMed]
- Fiorentino, G.; Esquinas, A.M.; Annunziata, A. Exercise and Chronic Obstructive Pulmonary Disease (COPD). In Advances in Experimental Medicine and Biology; Springer: Berlin/Heidelberg, Germany, 2020; Volume 1228, pp. 355–368. [Google Scholar]
- Zhu, Y.; Wang, Z.; Zhou, Y.; Onoda, K.; Maruyama, H.; Hu, C.; Liu, Z. Summary of Respiratory Rehabilitation and Physical Therapy Guidelines for Patients with COVID-19 Based on Recommendations of World Confederation for Physical Therapy and National Association of Physical Therapy. J. Phys. Ther. Sci. 2020, 32, 545–549. [Google Scholar] [CrossRef] [PubMed]
- Wittmer, V.L.; Paro, F.M.; Duarte, H.; Capellini, V.K.; Barbalho-Moulim, M.C. Early Mobilization and Physical Exercise in Patients with COVID-19: A Narrative Literature Review. Complement. Ther. Clin. Pract. 2021, 43, 101364. [Google Scholar] [CrossRef] [PubMed]
- Ahmadi Hekmatikar, A.; Ferreira Júnior, J.; Shahrbanian, S.; Suzuki, K. Functional and Psychological Changes after Exercise Training in Post-COVID-19 Patients Discharged from the Hospital: A PRISMA-Compliant Systematic Review. Int. J. Environ. Res. Public Health 2022, 19, 2290. [Google Scholar] [CrossRef] [PubMed]
- Aytür, Y.K.; Köseoglu, B.F.; Taşkıran, Ö.Ö.; Gökkaya, N.K.O.; Delialioğlu, S.Ü.; Tur, B.S.; Sarıkaya, S.; Şirzai, H.; Tiftik, T.T.; Alemdaroglu, E.; et al. Pulmonary Rehabilitation Principles in SARS-COV-2 Infection (COVID-19): The Revised Guideline for the Acute, Subacute, and Post-COVID-19 Rehabilitation. Turk. J. Phys. Med. Rehabil. 2021, 67, 129–145. [Google Scholar] [CrossRef] [PubMed]
- Huang, C.; Wang, Y.; Li, X.; Ren, L.; Zhao, J.; Hu, Y.; Zhang, L.; Fan, G.; Xu, J.; Gu, X.; et al. Clinical Features of Patients Infected with 2019 Novel Coronavirus in Wuhan, China. Lancet 2020, 395, 497–506. [Google Scholar] [CrossRef]
- Klok, F.A.; Kruip, M.J.H.A.; van der Meer, N.J.M.; Arbous, M.S.; Gommers, D.A.M.P.J.; Kant, K.M.; Kaptein, F.H.J.; van Paassen, J.; Stals, M.A.M.; Huisman, M.V.; et al. Incidence of Thrombotic Complications in Critically Ill ICU Patients with COVID-19. Thromb Res. 2020, 191, 145–147. [Google Scholar] [CrossRef]
- Seid, A.; Aychiluhm, S.; Mohammed, A. Effectiveness and Feasibility of Telerehabilitation in Patients with COVID-19: A Protocol for a Systematic Review and Meta-Analysis. BMJ Open 2022, 12, e058932. [Google Scholar] [CrossRef]
- Thomas, P.; Baldwin, C.; Bissett, B.; Boden, I.; Gosselink, R.; Granger, C.L.; Hodgson, C.; Jones, A.Y.M.; Kho, M.E.; Moses, R.; et al. Physiotherapy Management for COVID-19 in the Acute Hospital Setting: Clinical Practice Recommendations. J. Physiother. 2020, 66, 32–35. [Google Scholar] [CrossRef]
- Ceravolo, M.G.; Arienti, C.; de Sire, A.; Andrenelli, E.; Negrini, F.; Lazzarini, S.G.; Patrini, M.; Negrini, S. Rehabilitation and COVID-19: The Cochrane Rehabilitation 2020 Rapid Living Systematic Review. Eur. J. Phys. Rehabil. Med. 2020, 56, 642–651. [Google Scholar] [CrossRef] [PubMed]
- Iannaccone, S.; Castellazzi, P.; Tettamanti, A.; Houdayer, E.; Brugliera, L.; de Blasio, F.; Cimino, P.; Ripa, M.; Meloni, C.; Alemanno, F.; et al. Role of Rehabilitation Department for Adult Individuals With COVID-19: The Experience of the San Raffaele Hospital of Milan. Arch. Phys. Med. Rehabil. 2020, 101, 1656–1661. [Google Scholar] [CrossRef] [PubMed]
- Bennett, J.; Matthews, A. World Medical Association Declaration of Helsinki. JAMA 2013, 310, 2191. [Google Scholar] [CrossRef]
- Schulz, K.F.; Altman, D.G.; Moher, D. CONSORT 2010 Statement: Updated Guidelines for Reporting Parallel Group Randomized Trials. Ann. Intern. Med. 2010, 152, 726–732. [Google Scholar] [CrossRef] [PubMed]
- Hoffmann, T.C.; Glasziou, P.P.; Boutron, I.; Milne, R.; Perera, R.; Moher, D.; Altman, D.G.; Barbour, V.; Macdonald, H.; Johnston, M.; et al. Better Reporting of Interventions: Template for Intervention Description and Replication (TIDieR) Checklist and Guide. BMJ 2014, 348, g1687. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez-Molinero, A.; Herrero-Larrea, A.; Miñarro, A.; Narvaiza, L.; Gálvez-Barrón, C.; Gonzalo León, N.; Valldosera, E.; de Mingo, E.; Macho, O.; Aivar, D.; et al. The Spatial Parameters of Gait and Their Association with Falls, Functional Decline and Death in Older Adults: A Prospective Study. Sci. Rep. 2019, 9, 8813. [Google Scholar] [CrossRef] [PubMed]
- García-Hermoso, A.; Cavero-Redondo, I.; Ramírez-Vélez, R.; Ruiz, J.R.; Ortega, F.B.; Lee, D.C.; Martínez-Vizcaíno, V. Muscular Strength as a Predictor of All-Cause Mortality in an Apparently Healthy Population: A Systematic Review and Meta-Analysis of Data from Approximately 2 Million Men and Women. Arch. Phys. Med. Rehabil. 2018, 99, 2100–2113.e5. [Google Scholar] [CrossRef]
- Harvey, N.C.; Odén, A.; Orwoll, E.; Lapidus, J.; Kwok, T.; Karlsson, M.K.; Rosengren, B.E.; Ribom, E.; Cooper, C.; Cawthon, P.M.; et al. Measures of Physical Performance and Muscle Strength as Predictors of Fracture Risk Independent of FRAX, Falls, and ABMD: A Meta-Analysis of the Osteoporotic Fractures in Men (MrOS) Study. J. Bone Miner. Res. 2018, 33, 2150–2157. [Google Scholar] [CrossRef]
- Pavasini, R.; Guralnik, J.; Brown, J.C.; di Bari, M.; Cesari, M.; Landi, F.; Vaes, B.; Legrand, D.; Verghese, J.; Wang, C.; et al. Short Physical Performance Battery and All-Cause Mortality: Systematic Review and Meta-Analysis. BMC Med. 2016, 14, M85–M94. [Google Scholar] [CrossRef] [PubMed]
- Cruz-Jentoft, A.J.; Bahat, G.; Bauer, J.; Boirie, Y.; Bruyère, O.; Cederholm, T.; Cooper, C.; Landi, F.; Rolland, Y.; Sayer, A.A.; et al. Sarcopenia: Revised European Consensus on Definition and Diagnosis. Age Ageing 2019, 48, 16–31. [Google Scholar] [CrossRef]
- Peolsson, A.; Hedlund, R.; Oberg, B. Intra- and Inter-Tester Reliability and Reference Values for Hand Strength. J. Rehabil. Med. 2001, 33, 36–41. [Google Scholar] [CrossRef] [PubMed]
- Rocco, L.L.G.; Fernandes, T.G. Validity of the Short Physical Performance Battery for Screening for Frailty Syndrome among Older People in the Brazilian Amazon Region. A Cross-Sectional Study. Sao Paulo Med. J. 2020, 138, 537–544. [Google Scholar] [CrossRef] [PubMed]
- Gómez, J.F.; Curcio, C.-L.; Alvarado, B.; Zunzunegui, M.V.; Guralnik, J. Validity and Reliability of the Short Physical Performance Battery (SPPB): A Pilot Study on Mobility in the Colombian Andes. Colomb Med. 2013, 44, 165–171. [Google Scholar] [CrossRef]
- Beaudart, C.; Rolland, Y.; Cruz-Jentoft, A.J.; Bauer, J.M.; Sieber, C.; Cooper, C.; Al-Daghri, N.; Araujo de Carvalho, I.; Bautmans, I.; Bernabei, R.; et al. Assessment of Muscle Function and Physical Performance in Daily Clinical Practice: A Position Paper Endorsed by the European Society for Clinical and Economic Aspects of Osteoporosis, Osteoarthritis and Musculoskeletal Diseases (ESCEO). Calcif Tissue Int. 2019, 105, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Ostir, G.V.; Berges, I.M.; Ottenbacher, K.J.; Fisher, S.R.; Barr, E.; Hebel, J.R.; Guralnik, J.M. Gait Speed and Dismobility in Older Adults. Arch. Phys. Med. Rehabil. 2015, 96, 1641–1645. [Google Scholar] [CrossRef]
- Peters, D.M.; Fritz, S.L.; Krotish, D.E. Assessing the Reliability and Validity of a Shorter Walk Test Compared with the 10-Meter Walk Test for Measurements of Gait Speed in Healthy, Older Adults. J. Geriatr. Phys. Ther. 2013, 36, 24–30. [Google Scholar] [CrossRef]
- Aprahamian, I.; de Castro Cezar, N.O.; Izbicki, R.; Lin, S.M.; Paulo, D.L.V.; Fattori, A.; Biella, M.M.; Jacob Filho, W.; Yassuda, M.S. Screening for Frailty With the FRAIL Scale: A Comparison with the Phenotype Criteria. J. Am. Med. Dir. Assoc. 2017, 18, 592–596. [Google Scholar] [CrossRef]
- Susanto, M.; Hubbard, R.E.; Gardiner, P.A. Validity and Responsiveness of the FRAIL Scale in Middle-Aged Women. J. Am. Med. Dir. Assoc. 2018, 19, 65–69. [Google Scholar] [CrossRef]
- Morley, J.E.; Vellas, B.; Abellan van Kan, G.; Anker, S.D.; Bauer, J.M.; Bernabei, R.; Cesari, M.; Chumlea, W.C.; Doehner, W.; Evans, J.; et al. Frailty Consensus: A Call to Action. J. Am. Med. Dir. Assoc. 2013, 14, 392–397. [Google Scholar] [CrossRef]
- World Health Organization. Clinical Management of Severe Acute Respiratory Infection (SARI) When COVID-19 Disease Is Suspected: Interim Guidance, 13 March 2020; World Health Organization: Geneva, Switzerland, 2020. [Google Scholar]
- Izquierdo, M. Multicomponent Physical Exercise Program VIVIFRAIL. Available online: https://vivifrail.com/wp-content/uploads/2019/11/VIVIFRAIL-ENG-Interactivo.pdf (accessed on 1 January 2020).
- Izquierdo, M.; Rodriguez-Mañas, L.; Sinclair, A.J. Vivifrail Investigators Group Editorial: What Is New in Exercise Regimes for Frail Older People—How Does the Erasmus Vivifrail Project Take Us Forward? J. Nutr. Health Aging 2016, 20, 736–737. [Google Scholar] [CrossRef]
- Flampouraris, V.; Kalinoglou, S.; Kandreviotou, S.; Raitsiou, B.; Kokolaki, M.; Tsiafaki, X. Assessment of Dyspnoea in Covid 19 Patients Using Modified Borg Scale. Signa Vitae 2021, 17, S37. [Google Scholar] [CrossRef]
- da Silva e Silva, C.M.; Gomes Neto, M.; Saquetto, M.B.; da Conceição, C.S.; Souza-Machado, A. Effects of Upper Limb Resistance Exercise on Aerobic Capacity, Muscle Strength, and Quality of Life in COPD Patients: A Randomized Controlled Trial. Clin. Rehabil. 2018, 32, 1636–1644. [Google Scholar] [CrossRef] [PubMed]
- Mascha, E.J.; Vetter, T.R. Significance, Errors, Power, and Sample Size. Anesth. Analg. 2018, 126, 691–698. [Google Scholar] [CrossRef] [PubMed]
- Pierce, C.; Block, R.; Aguinis, H. Cautionary Note on Reporting Eta-Squared Values from Multifactor ANOVA Designs. Educ. Psychol. Meas. 2004, 64, 916–924. [Google Scholar] [CrossRef]
- Nambi, G.; Kamal Abdelbasset, W.; Alrawaili, S.M.; Elsayed, S.H.; Verma, A.; Vellaiyan, A.; Eid, M.M.; Aldhafian, O.R.; Nwihadh, N.B.; Saleh, A.K. Comparative Effectiveness Study of Low versus High-Intensity Aerobic Training with Resistance Training in Community-Dwelling Older Men with Post-COVID 19 Sarcopenia: A Randomized Controlled Trial. Clin. Rehabil. 2022, 36, 59–68. [Google Scholar] [CrossRef]
- Wiśniowska-Szurlej, A.; Ćwirlej-Sozańska, A.; Wołoszyn, N.; Sozański, B.; Wilmowska-Pietruszyńska, A. Association between Handgrip Strength, Mobility, Leg Strength, Flexibility, and Postural Balance in Older Adults under Long-Term Care Facilities. Biomed. Res. Int. 2019, 2019, 1042834. [Google Scholar] [CrossRef]
- Longobardi, I.; do Prado, D.M.L.; Goessler, K.F.; de Oliveira Júnior, G.N.; de Andrade, D.C.O.; Gualano, B.; Roschel, H. Benefits of Home-Based Exercise Training Following Critical SARS-CoV-2 Infection: A Case Report. Front. Sports Act. Living 2022, 3, 390. [Google Scholar] [CrossRef]
- Ali, N.A.; O’Brien, J.M.; Hoffmann, S.P.; Phillips, G.; Garland, A.; Finley, J.C.W.; Aimoosa, K.; Hejal, R.; Wolf, K.M.; Lemeshow, S.; et al. Acquired Weakness, Handgrip Strength, and Mortality in Critically Ill Patients. Am. J. Respir. Crit. Care Med. 2008, 178, 261–268. [Google Scholar] [CrossRef]
- Casas-Herrero, Á.; Sáez de Asteasu, M.L.; Antón-Rodrigo, I.; Sánchez-Sánchez, J.L.; Montero-Odasso, M.; Marín-Epelde, I.; Ramón-Espinoza, F.; Zambom-Ferraresi, F.; Petidier-Torregrosa, R.; Elexpuru-Estomba, J.; et al. Effects of Vivifrail Multicomponent Intervention on Functional Capacity: A Multicentre, Randomized Controlled Trial. J. Cachexia Sarcopenia Muscle 2022, 13, 884–893. [Google Scholar] [CrossRef]
- Sadjapong, U.; Yodkeeree, S.; Sungkarat, S.; Siviroj, P. Multicomponent Exercise Program Reduces Frailty and Inflammatory Biomarkers and Improves Physical Performance in Community-Dwelling Older Adults: A Randomized Controlled Trial. Int. J. Environ. Res. Public Health 2020, 17, 3760. [Google Scholar] [CrossRef]
- Suikkanen, S.; Soukkio, P.; Aartolahti, E.; Kääriä, S.; Kautiainen, H.; Hupli, M.T.; Pitkälä, K.; Sipilä, S.; Kukkonen-Harjula, K. Effect of 12-Month Supervised, Home-Based Physical Exercise on Functioning Among Persons With Signs of Frailty: A Randomized Controlled Trial. Arch. Phys. Med. Rehabil. 2021, 102, 2283–2290. [Google Scholar] [CrossRef] [PubMed]
| Experimental Group | Control Group | |
|---|---|---|
| Mean ± SD | Mean ± SD | |
| Age (years) | 49.5 ± 13.7 | 55.1 ± 20.9 |
| Sex | ||
| Men, n (%) | 24 (68.6%) | 23 (65.7%) |
| Women, n (%) | 11 (31.4%) | 12 (34.3%) |
| Height (m) | 1.71 ± 0.1 | 1.7 ± 0.3 |
| Weight (kg) | 87.1 ± 19.2 | 80.1 ± 13.9 |
| BMI (Kg/m2) | 29.7 ± 5.1 | 27.2 ± 4.4 |
| Dominance | ||
| Right, n (%) | 26 (74.3%) | 31 (88.6%) |
| Left, n (%) | 9 (25.7%) | 4 (11.4%) |
| Days of physical activity per week before COVID-19 | 3.0 ± 2.8 | 3.2 ± 3.1 |
| Sitting hours | 5.6 ± 3.1 | 6.5 ± 3.2 |
| Days of hospitalization | 14.3 ± 14.8 | 9.5 ± 8.1 |
| Baseline T0 | Post-Intervention T1 | Follow-up T2 | Difference between T0–T1 | Difference between T1–T2 | Difference between T0–T2 | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| Mean ± SD | Mean ± SD | Mean ± SD | Mean (95% CI) | η2 | Mean (95% CI) | η2 | Mean (95% CI) | η2 | ||
| Control Group | Handgrip (Kg) | |||||||||
| Dominant | 32.1 ± 11.8 | 32.3 ± 15.5 | 32.5 ± 15.5 | 0.2 (−4.4; 4.9) | 0.00 | 0.2 (−1.4; 1.8) | 0.00 | 0.4 (−4.4; 5.2) | 0.00 | |
| Non-dominant | 29.9 ± 10.8 | 28.2 ± 15.0 | 27.7 ± 15.1 | −1.7 (−5.6; 2.3) | 0.00 | −0.5 (−1.9; 1.0) | 0.00 | −2.2 (−6.2; 1.9) | 0.01 | |
| 4 m walk (sg) | 6.6 ± 3.1 | 5.5 ± 3.4 | 5.9 ± 3.4 | −1.1 (−1.9; 0.3) | 0.03 | 0.4 (−0.4; 0.7) | 0.00 | −0.7 (−1.6; 0.0) | 0.01 | |
| 5CRT (sg) | 18.6 ± 13.0 | 15.1 ± 10.4 | 14.8 ± 10.1 | −3.5 (−5.8; −1.3) | 0.02 | −0.3 (−0.9; 0.4) | 0.00 | −3.8 (−6.1; −1.5) | 0.03 | |
| Total SPPB (0–12) | 8.2 ± 2.5 | 8.7 ± 3.4 | 8.6 ± 3.3 | 0.5 (−0.5; 1.5) | 0.01 | −0.1 (−0.5; 0.2) | 0.00 | 0.4 (−0.7; 1.4) | 0.01 | |
| FRAIL scale (5–0) | 2.7 ± 1.4 | 2.1 ± 1.7 | 1.7 ± 1.7 | −0.6 (−1.3; 0.1) | 0.03 | −0.4 (−0.9; 0.8) | 0.03 | −1.0 (−1.7; −0.4) | 0.10 | |
| Experimental Group | Handgrip (Kg) | |||||||||
| Dominant | 25.2 ± 13.3 | 35.5 ± 9.3 | 37.1 ± 10.2 | 10.3 (−5.7; 15.0) | 0.17 | 1.6 (0.1; 3.1) | 0.01 | 11.9 (7.1; 16.7) | 0.20 | |
| Non-dominant | 26.6 ± 13.2 | 36.7 ± 11.1 | 37.9 ± 11.4 | 10.1 (6.2; 14.0) | 0.15 | 1.2 (−0.3; 2.6) | 0.00 | 11.3 (7.2; 15.3) | 0.18 | |
| 4 m walk (sg) | 6.5 ± 1.8 | 4.4 ± 1.5 | 4.0 ± 1.2 | −2.2 (−2.9; −1.4) | 0.26 | −0.4 (−0.7; 0.0) | 0.02 | −2.5 (−3.2; −1.6) | 0.32 | |
| 5CRT (sg) | 19.5 ± 7.5 | 13.1 ± 6.0 | 12.4 ± 5.8 | −6.4 (−8.7; −4.2) | 0.15 | −0.7 (−1.3; −0.1) | 0.00 | −7.1 (−9,5; −4.8) | 0.18 | |
| Total SPPB (0–12) | 7.5 ± 1.6 | 10.6 ± 1.8 | 10.9 ± 1.7 | 3.2 (2.2; 4.2) | 0.26 | 0.3 (−0.1; 0.7) | 0.00 | 3.4 (2.4; 4.4) | 0.30 | |
| FRAIL scale (5–0) | 2.9 ± 1.0 | 2.0 ± 1.2 | 0.6 ± 0.8 | −0.9 (−1.6; −0.2) | 0.14 | −1.4 (−1.9; 0.9) | 0.18 | −2.3 (−2.9; −1.6) | 0.46 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Llurda-Almuzara, L.; Rodríguez-Sanz, J.; López-de-Celis, C.; Aiguadé-Aiguadé, R.; Arán-Jové, R.; Labata-Lezaun, N.; Fernández-de-las-Peñas, C.; Bosch, J.; Pérez-Bellmunt, A. Effects of Adding an Online Exercise Program on Physical Function in Individuals Hospitalized by COVID-19: A Randomized Controlled Trial. Int. J. Environ. Res. Public Health 2022, 19, 16619. https://doi.org/10.3390/ijerph192416619
Llurda-Almuzara L, Rodríguez-Sanz J, López-de-Celis C, Aiguadé-Aiguadé R, Arán-Jové R, Labata-Lezaun N, Fernández-de-las-Peñas C, Bosch J, Pérez-Bellmunt A. Effects of Adding an Online Exercise Program on Physical Function in Individuals Hospitalized by COVID-19: A Randomized Controlled Trial. International Journal of Environmental Research and Public Health. 2022; 19(24):16619. https://doi.org/10.3390/ijerph192416619
Chicago/Turabian StyleLlurda-Almuzara, Luis, Jacobo Rodríguez-Sanz, Carlos López-de-Celis, Ramón Aiguadé-Aiguadé, Raúl Arán-Jové, Noé Labata-Lezaun, César Fernández-de-las-Peñas, Joan Bosch, and Albert Pérez-Bellmunt. 2022. "Effects of Adding an Online Exercise Program on Physical Function in Individuals Hospitalized by COVID-19: A Randomized Controlled Trial" International Journal of Environmental Research and Public Health 19, no. 24: 16619. https://doi.org/10.3390/ijerph192416619
APA StyleLlurda-Almuzara, L., Rodríguez-Sanz, J., López-de-Celis, C., Aiguadé-Aiguadé, R., Arán-Jové, R., Labata-Lezaun, N., Fernández-de-las-Peñas, C., Bosch, J., & Pérez-Bellmunt, A. (2022). Effects of Adding an Online Exercise Program on Physical Function in Individuals Hospitalized by COVID-19: A Randomized Controlled Trial. International Journal of Environmental Research and Public Health, 19(24), 16619. https://doi.org/10.3390/ijerph192416619











