Human Milk for Vulnerable Infants: Breastfeeding and Milk Sharing Practice among Ghanaian Women
Abstract
1. Introduction
2. Materials and Methods
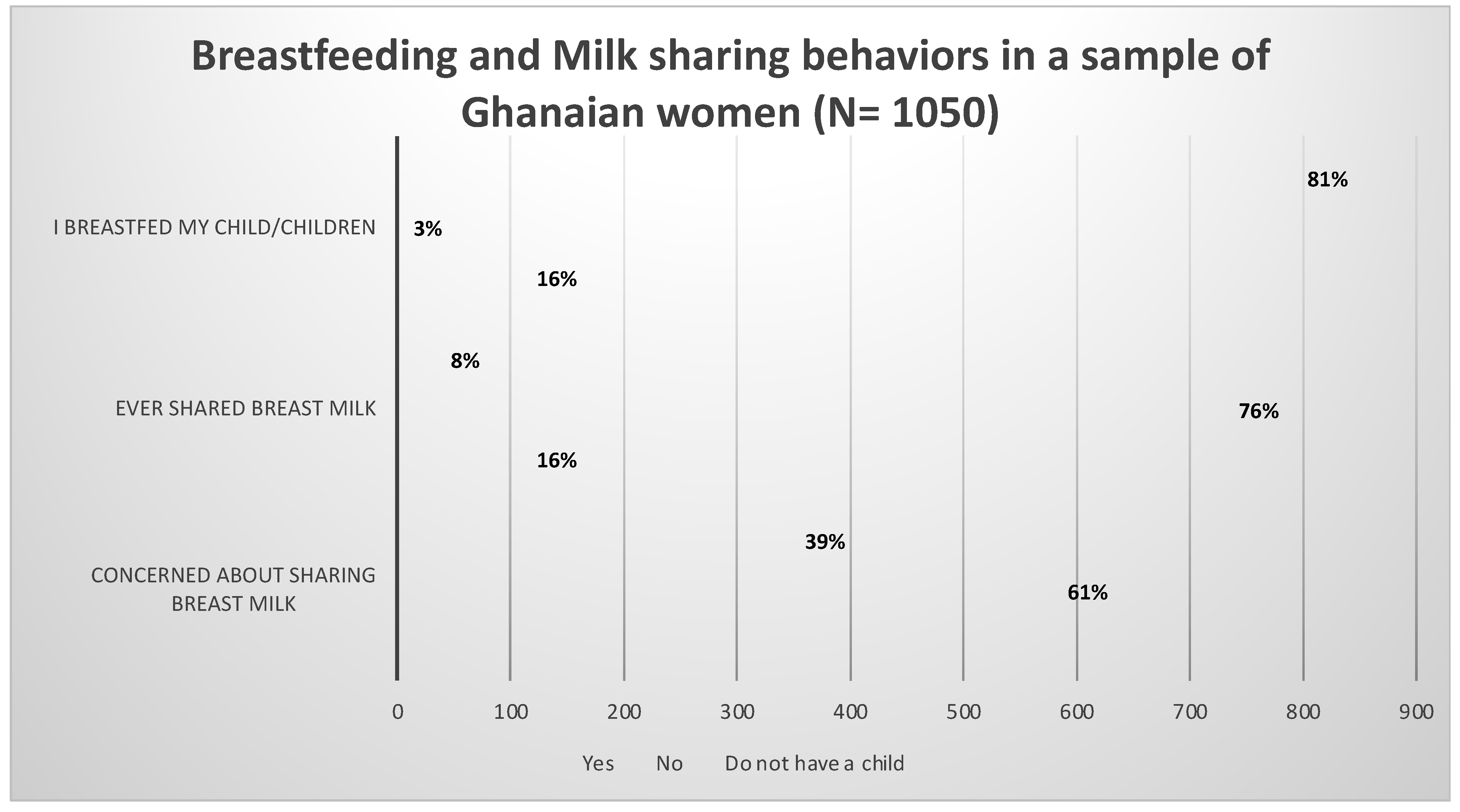
3. Results
3.1. Qualitative Results
- Why mothers breastfeed their children;
- Why mothers chose not to breastfeed their children;
- Mothers motivation for sharing their breast milk with other women/mothers;
- Mothers motivation for not sharing breast milk with other women/mothers;
- Having concerns about sharing breast milk; and
- Having no concerns about sharing breast milk
Reasons for Breastfeeding
- A.
- Why Mothers Breastfeed Their Children
- Excerpt 1
- Breast milk is very vital and ideal for child development. It contains all the nutrients babies need to grow. (Currently unemployed, 30 years, resident in Southern part of Ghana)
- Excerpt 2
- Because it helps in good child development and also prevent infections. (Public sector worker, 27 years, resident in Southern part of Ghana
- Excerpt 3
- Because it is cheaper and a better option. (Private sector worker, 30 years, resident in Southern part of Ghana)
- Excerpt 4
- Breast milk contains the right nutrients for babies, and it is cheap and readily available. (Public sector worker, 34 years, resident in Southern part of Ghana)
- B.
- Why Mothers Chose Not to Breastfeed Their Children
- Excerpt 5
- I did not have sufficient breast milk (Private sector worker, 27 years, resident in Southern part of Ghana)
- C.
- Motivation for Sharing Breast Milk with Other Women
- Excerpt 6
- My baby refused to suckle, and the other woman saw me expressing and discarding my breast milk so she came, pleading to give it to her instead because she had inverted nipples and also couldn’t produce breast milk and her baby was reducing in weight because she could not afford formula. (Public sector worker, above 35years, resident in Northern part of Ghana)
- Excerpt 7
- I was engorged. And she wasn’t producing enough to feed her child but was determined to stick to the 6 months rule. (Public sector worker, 31years, resident in Southern part of Ghana).
- Excerpt 8
- The baby was same month as mine. His mother had to go somewhere and return quickly but something delayed her, and baby started crying so I breastfed him. (Currently unemployed, 30years, resident in Southern part of Ghana).
- Excerpt 9
- Her breast milk was initially not flowing and later [the mother] was admitted at the hospital because of complications. (Public sector worker, 31 years, resident in Southern part of Ghana).
- D.
- Motivation for Not Sharing Breast Milk with Other Women
- Excerpt 10
- No opportunity to do so.
- (Public sector worker, 27 years, resident in Southern part of Ghana).
- Excerpt 11
- I produce enough and haven’t had the opportunity to share.
- (Public sector worker, 36 years, resident in Southern part of Ghana).
- Excerpt 12
- Well, I know that one need to be screen before and certified before sharing her breast milk to other mothers, so I believe am not fit until I get screened. (Public sector worker, 38 years, resident in Southern part of Ghana)
- Because no screening has been done and we know breast milk can transfer infections.
- (Public sector worker, 40 years, resident in Southern part of Ghana).
- Excerpt 13
- Unfortunate I did not have enough breast milk myself, aside that I do not know any other breastfeeding mom who was in dire need of breast milk.
- (Public sector worker, 36 years, resident in Southern part of Ghana).
- Excerpt 14
- I seldom have enough to spare.
- (Public sector worker, 44 years, resident in Southern part of Ghana).
- Excerpt 15
- Because only my baby needs my breast milk, and I don’t think someone in Ghana will allow her baby to be fed by a person who isn’t even a relative.
- (Public sector worker, 31 years, resident in Southern part of Ghana).
- Excerpt 16
- Because they feel some way when you offer it [breast milk] to them… I have offered it before, but I was turned down.
- (Public sector worker, 27 years, resident in Northern part of Ghana).
- E.
- Concerned about Sharing Breast Milk
- Excerpt 17
- Is everyone’s breast milk good for newborn babies?
- (Currently unemployed, 25 years, resident in Southern part of Ghana).
- Excerpt 18
- Is it safe? Is it a healthy practice?
- (Public sector worker, above 33 years, resident in Southern part of Ghana).
- Excerpt 19
- As Africans and Ghanaians, we hold lots of sentiments regarding feeding babies with other woman’s body fluids.
- (Public sector worker, above 35 years, resident in Southern part of Ghana).
- Excerpt 20
- Looking at the way Ghanaians are superstitious; I don’t think parents or relatives will allow their baby share breast milk with anyone.
- (Public sector worker, 31 years, resident in Southern part of Ghana).
- F.
- Not Concerned about Sharing Breast Milk
- Excerpt 21
- Breast milk is good for every child so why should I be worried about sharing. I am willing to share if only the other mother accepts.
- (Currently unemployed, above 35 years, resident in Southern part of Ghana).
- Excerpt 22
- I do not mind so long as I can ascertain that it is being used for a good cause. I have a cousin whose mother died at childbirth. I remember that one of her aunts breastfed her...If it would give a child a good start in life, why not?
- (Private sector worker, above 35 years, resident in Southern part of Ghana).
- Excerpt 23
- Because it will help a baby who really needs it. (Private sector worker, 34 years, resident in Southern part of Ghana).
- Excerpt 24
- I think is a humanitarian duty. (Public sector worker, 34 years, resident in Southern part of Ghana).
4. Discussion
4.1. Limitations
4.2. Recommendations and Future Research
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Research Question | Themes and Subthemes | Participant Quotes |
|---|---|---|
| Why mothers breastfeed their children | Breastmilk being ideal for child development | Breast milk is very vital and ideal for child development. It contains all the nutrients babies need to grow |
| Because it helps in good child development and also prevent infections. | ||
| Breastmilk being affordable | Because it is cheaper and a better option | |
| Breast milk contains the right nutrients for babies, and it is cheap and readily available | ||
| Why Mothers Chose Not to Breastfeed Their Children | Insufficient Breastmilk | I did not have sufficient breast milk |
| Motivation for Sharing Breast Milk with Other Women | Insufficient Breast Milk Production by Infants’ Mothers | My baby refused to suckle, and the other woman saw me expressing and discarding my breast milk so she came, pleading to give it to her instead because she had inverted nipples and also couldn’t produce breast milk and her baby was reducing in weight because she could not afford formula |
| I was engorged. And she wasn’t producing enough to feed her child but was determined to stick to the 6 months rule. | ||
| Mothers Unavailability Prompting mothers to share their Breast Milk | The baby was same month as mine. His mother had to go somewhere and return quickly but something delayed her, and baby started crying so I breastfed him. | |
| Her breast milk was initially not flowing and later [the mother] was admitted at the hospital because of complications. | ||
| Motivation for Not Sharing Breast Milk with Other Women | Absence or Lack of Opportunity to Share Breast Milk | No opportunity to do so. |
| I produce enough and haven’t had the opportunity to share. | ||
| Not Screened | Well, I know that one need to be screen before and certified before sharing her breast milk to other mothers and I, so I believe am not fit until I get screened | |
| Because no screening has been done and we know breast milk can transfer infections. | ||
| Insufficient supply of Breast Milk | Unfortunate I did not have enough breast milk myself, aside that I do not know any other breastfeeding mom who was in dire need of breast milk. | |
| I seldom have enough to spare. | ||
| Personal Perceptions about Breast Milk Sharing | Because only my baby needs my breast milk, and I don’t think someone in Ghana will allow her baby to be fed by a person who isn’t even a relative. | |
| Because they feel some way when you offer it [breast milk] to them… I have offered it before, but I was turned down. | ||
| Concerned about Sharing Breast Milk | Concern about Breast Milk Sharing Being a Healthy Practice | Is everyone’s breast milk good for newborn babies? |
| Is it safe? Is it a healthy practice? | ||
| African Belief System | As Africans and Ghanaians, we hold lots of sentiments regarding feeding babies with other woman’s body fluids. | |
| Looking at the way Ghanaians are superstitious; I don’t think parents or relatives will allow their baby share breast milk with anyone. | ||
| Not Concerned about Sharing Breast Milk | Goodness and Suitability of Breast Milk for Children | Breast milk is good for every child so why should I be worried about sharing. I am willing to share if only the other mother accepts. |
| I do not mind so long as I can ascertain that it is being used for a good cause. I have a cousin whose mother died at childbirth. I remember that one of her aunts breastfed her...If it would give a child a good start in life, why not? | ||
| Breast Milk’s ‘Help’ or Nutritional Benefit to Babies | Because it will help a baby who really needs it | |
| I think is a humanitarian duty. |
References
- World Health Organization. Newborn Mortality. 2022. Available online: https://www.who.int/news-room/fact-sheets/detail/levels-and-trends-in-child-mortality-report-2021 (accessed on 18 July 2022).
- UNICEF. Ghana (GHA)-Demographics, Health & Infant Mortality. UNICEF DATA. Available online: https://data.unicef.org/country/gha/ (accessed on 6 September 2022).
- Nkrumah, J. Maternal work and exclusive breastfeeding practice: A community based cross-sectional study in Efutu Municipal, Ghana. Int. Breastfeed. J. 2016, 12, 10. [Google Scholar] [CrossRef] [PubMed]
- Agbozo, F.; Ocansey, D.; Atitto, P.; Jahn, A. Compliance of a Baby-Friendly Designated Hospital in Ghana With the WHO/UNICEF Baby and Mother-Friendly Care Practices. J. Hum. Lact. 2019, 36, 175–186. [Google Scholar] [CrossRef] [PubMed]
- Ghana Statistical Service. Demographic and Health Survey 2014; Ghana Statistical Service (GSS); Ghana Health Service (GHS) and ICF International: Rockville, MD, USA, 2015. [Google Scholar]
- Ghana Statistical Service. Ghana Multiple indicator Cluster Survey (MISC2017/18); Survey Findings Report; Ghana Statistical Service: Accra, Ghana, 2018. [Google Scholar]
- Appiah, P.K.; Amu, H.; Osei, E.; Konlan, K.D.; Mumuni, I.H.; Verner, O.N.; Maalman, R.S.-E.; Kim, E.; Kim, S.; Bukari, M.; et al. Breastfeeding and weaning practices among mothers in Ghana: A population-based cross-sectional study. PLoS ONE 2021, 16, e0259442. [Google Scholar] [CrossRef] [PubMed]
- Agyekum, M.W.; Codjoe, S.N.A.; Dake, F.A.A.; Abu, M. Is Infant birth weight and mothers perceived birth size associated with the practice of exclusive breastfeeding in Ghana? PLoS ONE 2022, 17, e0267179. [Google Scholar] [CrossRef] [PubMed]
- Haider, R.; Saha, K.K. Breastfeeding and infant growth outcomes in the context of intensive peer counselling support in two communities in Bangladesh. Int. Breastfeed. J. 2016, 11, 1–10. [Google Scholar] [CrossRef]
- Khanal, V.; Da Cruz, J.L.N.B.; Karkee, R.; Lee, A.H. Factors Associated with Exclusive Breastfeeding in Timor-Leste: Findings from Demographic and Health Survey 2009–2010. Nutrients 2014, 6, 1691–1700. [Google Scholar] [CrossRef]
- Tampah-Naah, A.M.; Kumi-Kyereme, A.; Amo-Adjei, J. Maternal challenges of exclusive breastfeeding and complementary feeding in Ghana. PLoS ONE 2019, 14, e0215285. [Google Scholar] [CrossRef]
- Hobbs, A.J.; Mannion, C.A.; McDonald, S.W.; Brockway, M.; Tough, S.C. The impact of caesarean section on breastfeeding initiation, duration and difficulties in the first four months postpartum. BMC Pregnancy Childbirth 2016, 16, 1–9. [Google Scholar] [CrossRef]
- Yisma, E.; Mol, B.W.; Lynch, J.W.; Smithers, L.G. Impact of caesarean section on breastfeeding indicators: Within-country and meta-analyses of nationally representative data from 33 countries in sub-Saharan Africa. BMJ Open 2019, 9, e027497. [Google Scholar] [CrossRef]
- Murad, S.A.B.; Mohammed, A.K. Impact Mode of Delivery on Breastfeeding Practice Among Women Delivering in Maternity Teaching Hospital Sulaimani City. Mosul J. Nurs. 2021, 9, 315–332. [Google Scholar] [CrossRef]
- Getaneh, T.; Negesse, A.; Dessie, G.; Desta, M.; Temesgen, H.; Getu, T.; Gelaye, K. Impact of cesarean section on timely initiation of breastfeeding in Ethiopia: A systematic review and meta-analysis. Int. Breastfeed. J. 2021, 16, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Babchuk, W.A. Fundamentals of qualitative analysis in family medicine. Fam. Med. Community Health 2019, 7, e000040. [Google Scholar] [CrossRef] [PubMed]
- Chowdhury, R.; Sinha, B.; Sankar, M.J.; Taneja, S.; Bhandari, N.; Rollins, N.; Bahl, R.; Martines, J. Breastfeeding and maternal health outcomes: A systematic review and meta-analysis. Acta Paediatr. 2015, 104, 96–113. [Google Scholar] [CrossRef] [PubMed]
- Eidelman, A.I.; Schanler, R.J.; Johnston, M.; Landers, S.; Noble, L.; Szucs, K.; Viehmann, L. Breastfeeding and the Use of Human Milk. Pediatrics 2012, 129, e827–e841. [Google Scholar]
- Otoo, G.E.; Lartey, A.A.; Pérez-Escamilla, R. Perceived Incentives and Barriers to Exclusive Breastfeeding Among Periurban Ghanaian Women. J. Hum. Lact. 2009, 25, 34–41. [Google Scholar] [CrossRef] [PubMed]
- West, E.; Knight, R.J. Mothers’ Milk: Slavery, Wet-Nursing, and Black and White Women in the Antebellum South. J. South. Hist. 2017, 83, 37–68. [Google Scholar] [CrossRef]
- Can, H.; Yesil, Y.; Eksioglu, A.; Ceber, E. Women’s Views on Wet Nursing and Milk Siblinghood: An Example from Turkey. Breastfeed. Med. 2014, 9, 559–560. [Google Scholar]
- Golden, J. A Social History of Wet Nursing in America: From Breast to Bottle; Ohio State University Press: Columbus, OH, USA, 2001; 236p. [Google Scholar]
- Kimani-Murage, E.W.; Wanjohi, M.N.; Kamande, E.W.; Macharia, T.N.; Mwaniki, E.; Zerfu, T.; Ziraba, A.; Muiruri, J.W.; Samburu, B.; Govoga, A.; et al. Perceptions on donated human milk and human milk banking in Nairobi, Kenya. Matern. Child Nutr. 2019, 15, e12842. [Google Scholar] [CrossRef]
- Coutsoudis, I.; Petrites, A.; Coutsoudis, A. Acceptability of donated breast milk in a resource limited South African setting. Int. Breastfeed. J. 2011, 6, 3. [Google Scholar] [CrossRef]
- Chagwena, D.T.; Mugariri, F.; Sithole, B.; Mataga, S.F.; Danda, R.; Matsungo, T.M.; Maponga, C.C. Acceptability of donor breastmilk banking among health workers: A cross-sectional survey in Zimbabwean urban settings. Int. Breastfeed. J. 2020, 15, 1–11. [Google Scholar] [CrossRef]
- Joseph, F.; Earland, J. A qualitative exploration of the sociocultural determinants of exclusive breastfeeding practices among rural mothers, North West Nigeria. Int. Breastfeed. J. 2019, 14, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Yeo, E.A.; Béquet, L.; Ekouévi, D.K.; Krawinkel, M. Attitudes Towards Exclusive Breastfeeding and Other Infant Feeding Options—A Study from Abidjan, Côte d’Ivoire. J. Trop. Pediatr. 2005, 51, 223–226. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Nacro, B.; Barro, M.; Gaudreault, S.; Dao, B. Prevention of Mother to Child Transmission of HIV in Burkina Faso: Breastfeeding and Wet Nursing. J. Trop. Pediatr. 2009, 56, 183–186. [Google Scholar] [CrossRef] [PubMed]
- Emergency Nutrition Network (ENN). A Review of Wet Nursing Experiences, Motivations, facilitators and Barriers. Field Exch. 2019, 59. Available online: https://www.ennonline.net/fex/59/www.ennonline.net/fex/59/wetnursing (accessed on 19 October 2022).
- La Leche League. Sharing Breastmilk. La Leche League GB. 2016. Available online: https://www.laleche.org.uk/sharing-breastmilk/ (accessed on 2 December 2022).
- Geraghty, S.R.; Heier, J.E.; Rasmussen, K.M. Got Milk? Sharing Human Milk via the Internet. Public Health Rep. 2011, 126, 161–164. [Google Scholar] [CrossRef]
- Biggs, C. Talking the Talk but not Walking the Walk: Donating to Human Milk Banks in South Africa. J. Hum. Lact. 2020, 37, 105–113. [Google Scholar] [CrossRef]
| Frequency (F) | Percentage (%) | |
|---|---|---|
| Country of Origin | ||
| Ghanaian | 1050 | 100 |
| Residence | ||
| Southern Part of Ghana | 921 | 87 |
| Northern Part of Ghana | 121 | 12 |
| Outside Ghana (Diaspora) | 8 | 1 |
| Age | ||
| Below 35 | 748 | 71 |
| Above 35 | 302 | 29 |
| Occupation | ||
| Public Sector | 708 | 68 |
| Private sector | 287 | 27 |
| Currently Unemployed | 55 | 5 |
| Educational level | ||
| Junior High school or less | 140 | 13 |
| Senior High School | 137 | 13 |
| Some College | 129 | 12 |
| Bachelor’s Degree | 418 | 40 |
| Master’s Degree | 174 | 16 |
| Some Doctoral Level Courses | 8 | 1 |
| Doctoral Degree | 16 | 2 |
| No Formal Education | 28 | 3 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Obeng, C.; Jackson, F.; Nsiah-Asamoah, C.; Amissah-Essel, S.; Obeng-Gyasi, B.; Perry, C.A.; Gonzalez Casanova, I. Human Milk for Vulnerable Infants: Breastfeeding and Milk Sharing Practice among Ghanaian Women. Int. J. Environ. Res. Public Health 2022, 19, 16560. https://doi.org/10.3390/ijerph192416560
Obeng C, Jackson F, Nsiah-Asamoah C, Amissah-Essel S, Obeng-Gyasi B, Perry CA, Gonzalez Casanova I. Human Milk for Vulnerable Infants: Breastfeeding and Milk Sharing Practice among Ghanaian Women. International Journal of Environmental Research and Public Health. 2022; 19(24):16560. https://doi.org/10.3390/ijerph192416560
Chicago/Turabian StyleObeng, Cecilia, Frederica Jackson, Christiana Nsiah-Asamoah, Salome Amissah-Essel, Barnabas Obeng-Gyasi, Cydne A. Perry, and Ines Gonzalez Casanova. 2022. "Human Milk for Vulnerable Infants: Breastfeeding and Milk Sharing Practice among Ghanaian Women" International Journal of Environmental Research and Public Health 19, no. 24: 16560. https://doi.org/10.3390/ijerph192416560
APA StyleObeng, C., Jackson, F., Nsiah-Asamoah, C., Amissah-Essel, S., Obeng-Gyasi, B., Perry, C. A., & Gonzalez Casanova, I. (2022). Human Milk for Vulnerable Infants: Breastfeeding and Milk Sharing Practice among Ghanaian Women. International Journal of Environmental Research and Public Health, 19(24), 16560. https://doi.org/10.3390/ijerph192416560









