Health Literacy Is Associated with Activities of Daily Living of Patients Participating in Cardiac Rehabilitation: A Multicenter Clinical Study
Abstract
1. Introduction
2. Materials and Methods
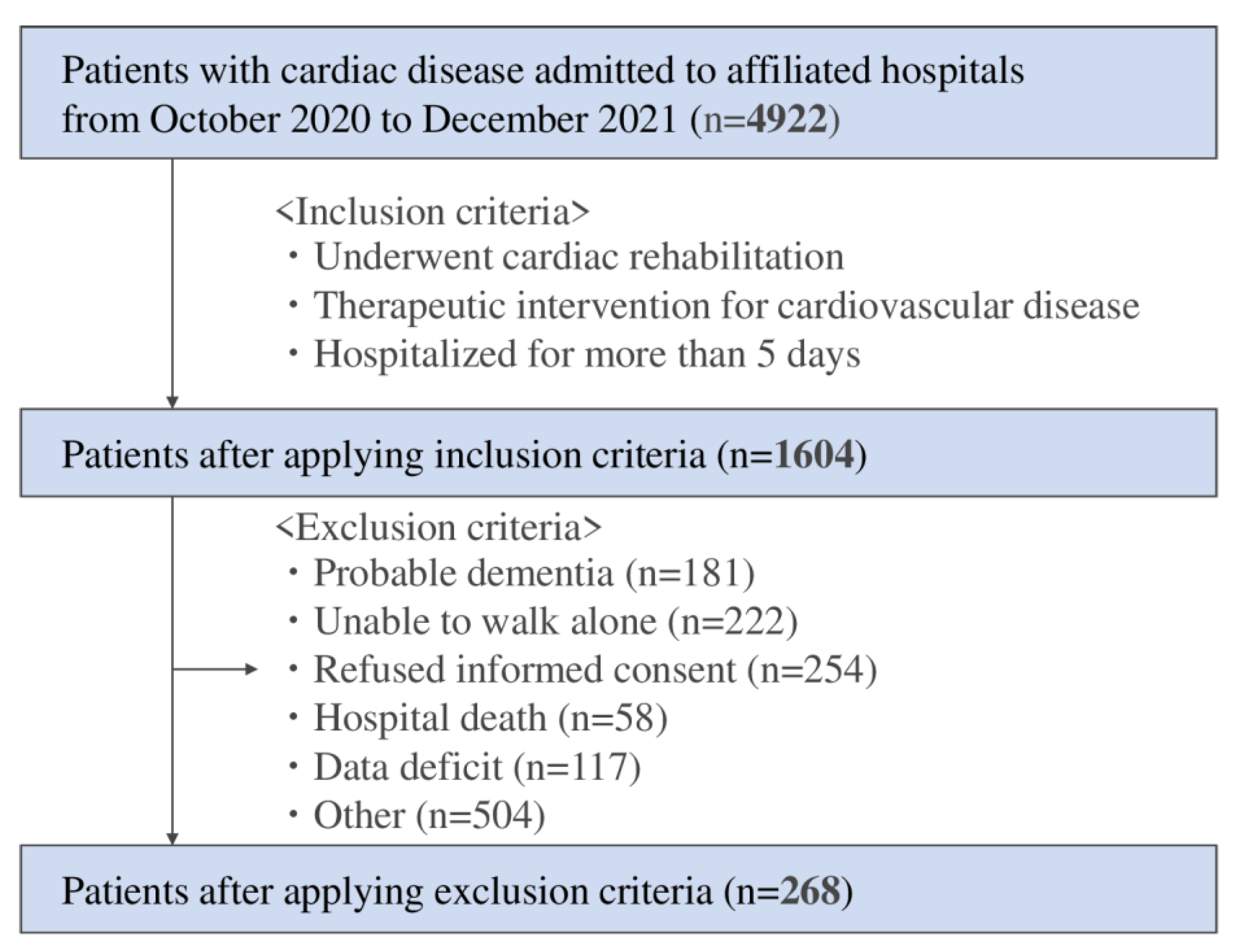
2.1. Study Design and Eligibility Criteria
2.2. Phase 1 Cardiac Rehabilitation
2.3. Patient Characteristics
2.4. Assessment of Health Literacy
2.5. Outcome
2.6. Statistical Analysis
3. Results
3.1. Patient Characteristics
3.2. Comparison between Low HL Group and High HL Group
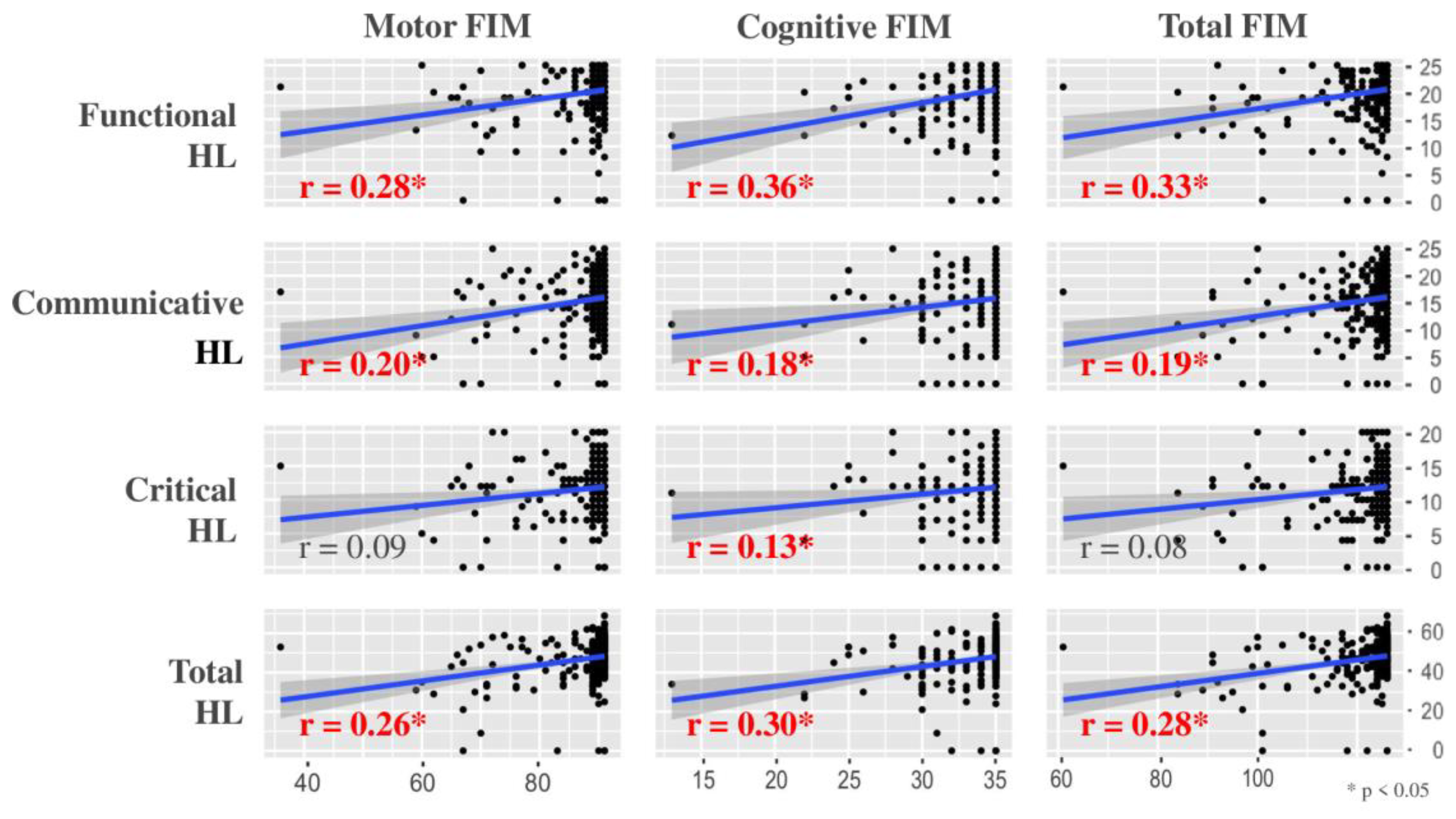
3.3. Correlation Coefficient
3.4. Multiple Linear Regression Analysis
4. Discussion
4.1. Summary
4.2. Comparison with Previous Studies
4.3. Comparison of Analysis Results
4.4. Clinical Implication
4.5. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Nutbeam, D. The evolving concept of health literacy. Soc. Sci. Med. 2008, 67, 2072–2078. [Google Scholar] [CrossRef] [PubMed]
- Jayasinghe, U.W.; Harris, M.F.; Parker, S.M.; Litt, J.; van Driel, M.; Mazza, D.; Del Mar, C.; Lloyd, J.; Smith, J.; Zwar, N.; et al. The impact of health literacy and life style risk factors on health-related quality of life of Australian patients. Health Qual. Life Outcomes 2016, 14, 68. [Google Scholar] [CrossRef] [PubMed]
- Kanejima, Y.; Shimogai, T.; Kitamura, M.; Ishihara, K.; Izawa, K.P. Impact of health literacy in patients with cardiovascular diseases: A systematic review and meta-analysis. Patient Educ. Couns. 2021, 105, 1793–1800. [Google Scholar] [CrossRef] [PubMed]
- JCS Joint Working Group. Guidelines for Rehabilitation in Patients With Cardiovascular Disease (JCS 2012). Circ. J. 2014, 78, 2022–2093. [Google Scholar] [CrossRef] [PubMed]
- Mattson, C.C.; Rawson, K.; Hughes, J.W.; Waechter, N.; Rosneck, J. Health literacy predicts cardiac knowledge gains in cardiac rehabilitation participants. Health Educ. J. 2014, 74, 96–102. [Google Scholar] [CrossRef]
- Mlinac, M.E.; Feng, M.C. Assessment of Activities of Daily Living, Self-Care, and Independence. Arch. Clin. Neuropsychol. 2016, 31, 506–516. [Google Scholar] [CrossRef] [PubMed]
- Dunlay, S.M.; Manemann, S.M.; Chamberlain, A.M.; Cheville, A.L.; Jiang, R.; Weston, S.A.; Roger, V.L. Activities of Daily Living and Outcomes in Heart Failure. Circ. Heart Fail. 2015, 8, 261–267. [Google Scholar] [CrossRef] [PubMed]
- Edemekong, P.F.; Bomgaars, D.L.; Sukumaran, S.; School, C. Activities of daily living. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2022. Available online: https://www.ncbi.nlm.nih.gov/books/NBK470404/ (accessed on 17 February 2022).
- Izawa, K.P.; Watanabe, S.; Oka, K.; Hiraki, K.; Morio, Y.; Kasahara, Y.; Osada, N.; Omiya, K.; Iijima, S. Age-Related Differences in Physiologic and Psychosocial Outcomes After Cardiac Rehabilitation. Am. J. Phys. Med. Rehabil. 2010, 89, 24–33. [Google Scholar] [CrossRef]
- Ishihara, K.; Izawa, K.P.; Kitamura, M.; Shimogai, T.; Kanejima, Y.; Morisawa, T.; Shimizu, I. Influence of mild cognitive impairment on activities of daily living in patients with cardiovascular disease. Heart Vessel. 2019, 34, 1944–1951. [Google Scholar] [CrossRef] [PubMed]
- Wolf, M.S.; Gazmararian, J.A.; Baker, D.W. Health Literacy and Functional Health Status among Older Adults. Arch. Intern. Med. 2005, 165, 1946–1952. [Google Scholar] [CrossRef]
- Chung, K.C.; Song, J.W. A Guide to Organizing a Multicenter Clinical Trial. Plast. Reconstr. Surg. 2010, 126, 515–523. [Google Scholar] [CrossRef] [PubMed]
- Bjarnason-Wehrens, B.; McGee, H.; Zwisler, A.-D.; Piepoli, M.F.; Benzer, W.; Schmid, J.-P.; Dendale, P.; Pogosova, N.-G.V.; Zdrenghea, D.; Niebauer, J.; et al. Cardiac rehabilitation in Europe: Results from the European Cardiac Rehabilitation Inventory Survey. Eur. J. Cardiov. Prev. Rehabil. 2010, 17, 410–418. [Google Scholar] [CrossRef] [PubMed]
- Bouillanne, O.; Morineau, G.; Dupont, C.; Coulombel, I.; Vincent, J.-P.; Nicolis, I.; Benazeth, S.; Cynober, L.; Aussel, C. Geriatric Nutri-tional Risk Index: A new index for evaluating at-risk elderly medical patients. Am. J. Clin. Nutr. 2005, 82, 777–783. [Google Scholar] [CrossRef]
- Charlson, M.E.; Pompei, P.; Ales, K.L.; MacKenzie, C.R. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J. Chronic Dis. 1987, 40, 373–383. [Google Scholar] [CrossRef] [PubMed]
- Suka, M.; Odajima, T.; Kasai, M.; Igarashi, A.; Ishikawa, H.; Kusama, M.; Nakayama, T.; Sumitani, M.; Sugimori, H. The 14-item health literacy scale for Japanese adults (HLS-14). Environ. Health Prev. Med. 2013, 18, 407–415. [Google Scholar] [CrossRef]
- Granger, C.V.; Hamilton, B.B.; Keith, R.A.; Zielezny, M.; Sherwin, F.S. Advances in functional assessment for medical rehabilitation. Top. Geriatr. Rehabil. 1986, 1, 59–74. [Google Scholar] [CrossRef]
- Ottenbacher, K.J.; Hsu, Y.; Granger, C.V.; Fiedler, R.C. The reliability of the functional independence measure: A quantitative review. Arch. Phys. Med. Rehabil. 1996, 77, 1226–1232. [Google Scholar] [CrossRef]
- Schober, P.; Boer, C.; Schwarte, L.A. Correlation Coefficients. Anesth. Analg. 2018, 126, 1763–1768. [Google Scholar] [CrossRef]
- Stuck, A.E.; Walthert, J.M.; Nikolaus, T.; Büla, C.J.; Hohmann, C.; Beck, J.C. Risk factors for functional status decline in community-living elderly people: A systematic literature review. Soc. Sci. Med. 1999, 48, 445–469. [Google Scholar] [CrossRef]
- de Melo Ghisi, G.L.; da Silva Chaves, G.S.; Britto, R.R.; Oh, P. Health literacy and coronary artery disease: A systematic review. Patient Educ. Couns. 2017, 101, 177–184. [Google Scholar] [CrossRef]
- Nutbeam, D. Health literacy as a public health goal: A challenge for contemporary health education and communication strategies into the 21st century. Health Promot. Int. 2000, 15, 259–267. [Google Scholar] [CrossRef]
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2020; Available online: https://www.R-project.org/ (accessed on 19 July 2011).
- Rickham, P.P. Human Experimentation: Code of Ethics of the World Medical Association. Declaration of Helsinki. Br. Med. J. 1964, 2, 177. [Google Scholar] [PubMed]
- Cajita, M.I.; Cajita, T.R.; Han, H.-R. Health Literacy and Heart Failure. J. Cardiovasc. Nurs. 2016, 31, 121–130. [Google Scholar] [CrossRef] [PubMed]
- Sansone, G.R.; Alba, A.; Frengley, J. Analysis of FIM instrument scores for patients admitted to an inpatient cardiac rehabilitation program. Arch. Phys. Med. Rehabil. 2002, 83, 506–512. [Google Scholar] [CrossRef] [PubMed]
- Kitamura, M.; Izawa, K.P.; Taniue, H.; Mimura, Y.; Imamura, K.; Nagashima, H.; Brubaker, P.H. Relationship between Activities of Daily Living and Readmission within 90 Days in Hospitalized Elderly Patients with Heart Failure. BioMed Res. Int. 2017, 2017, 7420738. [Google Scholar] [CrossRef] [PubMed]
- Beninato, M.; Gill-Body, K.M.; Salles, S.; Stark, P.C.; Black-Schaffer, R.M.; Stein, J. Determination of the Minimal Clinically Important Difference in the FIM Instrument in Patients With Stroke. Arch. Phys. Med. Rehabil. 2006, 87, 32–39. [Google Scholar] [CrossRef] [PubMed]
- Hall, K.M.; Mann, N.; High, W.M.; Wright, J.; Kreutzer, J.S.; Wood, D. Functional Measures After Traumatic Brain Injury: Ceiling Effects of FIM, FIM+FAM, DRS, and CIQ. J. Head Trauma Rehabil. 1996, 11, 27–39. [Google Scholar] [CrossRef]
- Johnson, M. Management of end stage cardiac failure. Postgrad. Med. J. 2007, 83, 395–401. [Google Scholar] [CrossRef]
- Zaben, K.; Khalil, A. Health Literacy, Self-Care Behavior and Quality of Life in Acute Coronary Syndrome Patients: An Inte-grative Review. Open J. Nurs. 2019, 09, 383–395. [Google Scholar] [CrossRef]
- Safeer, R.S.; Cooke, C.E.; Keenan, J. The impact of health literacy on cardiovascular disease. Vasc. Health Risk Manag. 2006, 2, 457–464. [Google Scholar] [CrossRef]
| Characteristic | Low HL (n = 137) | High HL (n = 131) | Z †, χ2 Value | p-Value |
|---|---|---|---|---|
| Age (years) * | 72.0 [61.0–79.0] | 68.0 [58.0–77.0] | 1.02 † | 0.306 |
| Male ratio (%) | 78.1 | 75.6 | 0.24 | 0.623 |
| Body mass index (kg/m2) * | 22.7 [20.3–26.1] | 23.6 [21.1–25.9] | 1.33 † | 0.183 |
| Education (>13 years) (%) | 46.7 | 55 | 1.82 | 0.177 |
| Employment (%) | 53.3 | 58.8 | 0.82 | 0.365 |
| Living together (%) | 76.6 | 82.4 | 1.38 | 0.240 |
| Smoking (%) | 0.01 | 0.728 | ||
| No | 45.3 | 40.5 | ||
| Past | 43.1 | 46.6 | ||
| Current | 11.7 | 13 | ||
| Marriage (%) | 3.25 | 0.197 | ||
| No | 19.0 | 12.2 | ||
| Ex | 18.2 | 15.3 | ||
| Yes | 62.8 | 72.5 | ||
| Admission duration (days) * | 16.0 [12.0–22.0] | 15.0 [12.0–20.0] | 1.27 † | 0.203 |
| Discharge home (%) | 97.1 | 98.5 | 0.59 | 0.684 |
| Main diagnosis (%) | 10.6 | 0.082 | ||
| Heart failure | 40.9 | 29.8 | ||
| Myocardial infarction | 33.6 | 51.1 | ||
| Angina pectoris | 11.7 | 7.6 | ||
| Aortic dissection | 1.5 | 0.8 | ||
| Aortic aneurysm | 0.7 | 2.3 | ||
| Valve diseases | 7.3 | 4.6 | ||
| Others | 4.4 | 3.8 | ||
| Ejection fraction (%) * | 53.0 [38.0–61.3] | 52.0 [41.0–62.0] | 0.38 † | 0.707 |
| Comorbidities (%) | ||||
| Hypertension | 64.2 | 61.8 | 0.17 | 0.684 |
| Diabetes | 35.8 | 35.1 | 0.01 | 0.911 |
| Dyslipidemia | 45.3 | 63.4 | 8.84 | 0.003 |
| Congestive heart failure | 46.7 | 38.2 | 2.00 | 0.157 |
| Stroke | 10.9 | 9.2 | 0.24 | 0.627 |
| Renal dysfunction | 27 | 18.3 | 2.87 | 0.090 |
| Peripheral artery disease | 8.8 | 4.6 | 1.87 | 0.172 |
| Chronic lung disease | 6.6 | 8.4 | 0.32 | 0.569 |
| Mild cognitive impairment | 21.9 | 10.7 | 6.13 | 0.013 |
| Charlson Comorbidity Index * | 2.0 [1.0–3.0] | 1.0 [0.0–3.0] | 1.68 † | 0.094 |
| Hemoglobin (g/dL) * | 13.0 [11.4–14.6] | 13.5 [12.0–14.5] | 1.49 † | 0.137 |
| Creatinine (mg/dL) * | 1.0 [0.8–1.3] | 0.9 [0.8–1.1] | 1.44 † | 0.150 |
| eGFR (mL/min/1.73 m2)* | 55.4 [39.2–69.8] | 59.2 [47.1–70.4] | 1.68 † | 0.093 |
| GNRI * | 100.5 [91.5–107.0] | 101.9 [92.7–109.2] | 0.51 † | 0.608 |
| Medications (%) | ||||
| Beta blocker (%) | 73 | 75.6 | 0.23 | 0.629 |
| ACE-I (%) | 25.5 | 35.1 | 2.91 | 0.088 |
| ARB (%) | 22.6 | 29.0 | 1.43 | 0.232 |
| Diuretic (%) | 55.5 | 54.2 | 0.04 | 0.834 |
| Statin (%) | 51.8 | 73.3 | 13.1 | <0.001 |
| FIM/Motor * | 90.0 [88.0–91.0] | 91.0 [89.0–91.0] | 3.16 † | 0.002 |
| FIM/Cognitive * | 35.0 [33.0–35.0] | 35.0 [35.0–35.0] | 3.78 † | <0.001 |
| FIM/Total * | 124.0 [120.0–126.0] | 125.0 [124.0–126.0] | 3.39 † | <0.001 |
| HLS-14/Functional * | 19.0 [16.0–22.0] | 23.0 [21.0–25.0] | 7.46 † | <0.001 |
| HLS-14/Communicative * | 13.0 [10.0–15.0] | 20.0 [17.0–21.0] | 15.3 † | <0.001 |
| HLS-14/Critical * | 10.0 [8.0–12.0] | 14.0 [12.0–16.0] | 8.21 † | <0.001 |
| HLS14/Total * | 43.0 [38.0–46.0] | 54.0 [52.0–57.5] | 23.3 † | <0.001 |
| Characteristic | Univariable Model | Multivariable Model | ||
|---|---|---|---|---|
| Beta (95% CI) | p-Value | Beta (95% CI) | p-Value | |
| Age | −0.29 (−0.36 to −0.22) | <0.001 | −0.18 (−0.27 to −0.10) | <0.001 |
| Sex | 4.87 (2.57 to 7.18) | <0.001 | 0.98 (−1.24 to 3.20) | 0.39 |
| Body mass index | 0.32 (0.09 to 0.54) | 0.005 | −0.11 (−0.37 to 0.15) | 0.40 |
| Education | 3.12 (1.16 to 5.09) | 0.002 | −0.21 (−1.97 to 1.55) | 0.82 |
| Employment | 5.58 (3.67 to 7.48) | <0.001 | −0.18 (−2.36 to 2.00) | 0.87 |
| Living together | −0.98 (−3.46 to 1.50) | 0.44 | −3.82 (−6.22 to −1.42) | 0.002 |
| Smoking | 2.30 (−0.73 to 5.34) | 0.14 | −0.63 (−3.10 to 1.83) | 0.61 |
| Marriage | 2.28 (1.50 to 3.06) | <0.001 | 2.07 (1.22 to 2.91) | <0.001 |
| Heart failure | −5.85 (−7.82 to −3.87) | <0.001 | −3.20 (−5.62 to −0.78) | 0.010 |
| Myocardial infarction | 4.30 (2.34 to 6.26) | <0.001 | −0.39 (−2.61 to 1.82) | 0.73 |
| Ejection fraction | 0.001 (−0.07 to 0.07) | 0.97 | 0.005 (−0.06 to 0.06) | 0.88 |
| Stroke | −5.03 (−8.31 to −1.76) | 0.003 | −2.86 (−5.58 to −0.13) | 0.040 |
| Renal disease | −5.00 (−7.31 to −2.68) | <0.001 | −0.80 (−2.90 to 1.30) | 0.45 |
| MCI | −8.99 (−11.5 to −6.52) | <0.001 | −3.98 (−6.44 to −1.51) | 0.002 |
| GNRI | 0.10 (0.02 to 0.18) | 0.012 | 0.00 (−0.09 to 0.09) | >0.99 |
| HLS-14 | 0.28 (0.17 to 0.40) | <0.001 | 0.16 (0.06 to 0.26) | 0.002 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kanejima, Y.; Izawa, K.P.; Kitamura, M.; Ishihara, K.; Ogura, A.; Kubo, I.; Nagashima, H.; Tawa, H.; Matsumoto, D.; Shimizu, I. Health Literacy Is Associated with Activities of Daily Living of Patients Participating in Cardiac Rehabilitation: A Multicenter Clinical Study. Int. J. Environ. Res. Public Health 2022, 19, 16550. https://doi.org/10.3390/ijerph192416550
Kanejima Y, Izawa KP, Kitamura M, Ishihara K, Ogura A, Kubo I, Nagashima H, Tawa H, Matsumoto D, Shimizu I. Health Literacy Is Associated with Activities of Daily Living of Patients Participating in Cardiac Rehabilitation: A Multicenter Clinical Study. International Journal of Environmental Research and Public Health. 2022; 19(24):16550. https://doi.org/10.3390/ijerph192416550
Chicago/Turabian StyleKanejima, Yuji, Kazuhiro P. Izawa, Masahiro Kitamura, Kodai Ishihara, Asami Ogura, Ikko Kubo, Hitomi Nagashima, Hideto Tawa, Daisuke Matsumoto, and Ikki Shimizu. 2022. "Health Literacy Is Associated with Activities of Daily Living of Patients Participating in Cardiac Rehabilitation: A Multicenter Clinical Study" International Journal of Environmental Research and Public Health 19, no. 24: 16550. https://doi.org/10.3390/ijerph192416550
APA StyleKanejima, Y., Izawa, K. P., Kitamura, M., Ishihara, K., Ogura, A., Kubo, I., Nagashima, H., Tawa, H., Matsumoto, D., & Shimizu, I. (2022). Health Literacy Is Associated with Activities of Daily Living of Patients Participating in Cardiac Rehabilitation: A Multicenter Clinical Study. International Journal of Environmental Research and Public Health, 19(24), 16550. https://doi.org/10.3390/ijerph192416550








