Evaluation of Movement Restriction of Spinal Orthoses Using Inertial Measurement Units
Abstract
1. Introduction
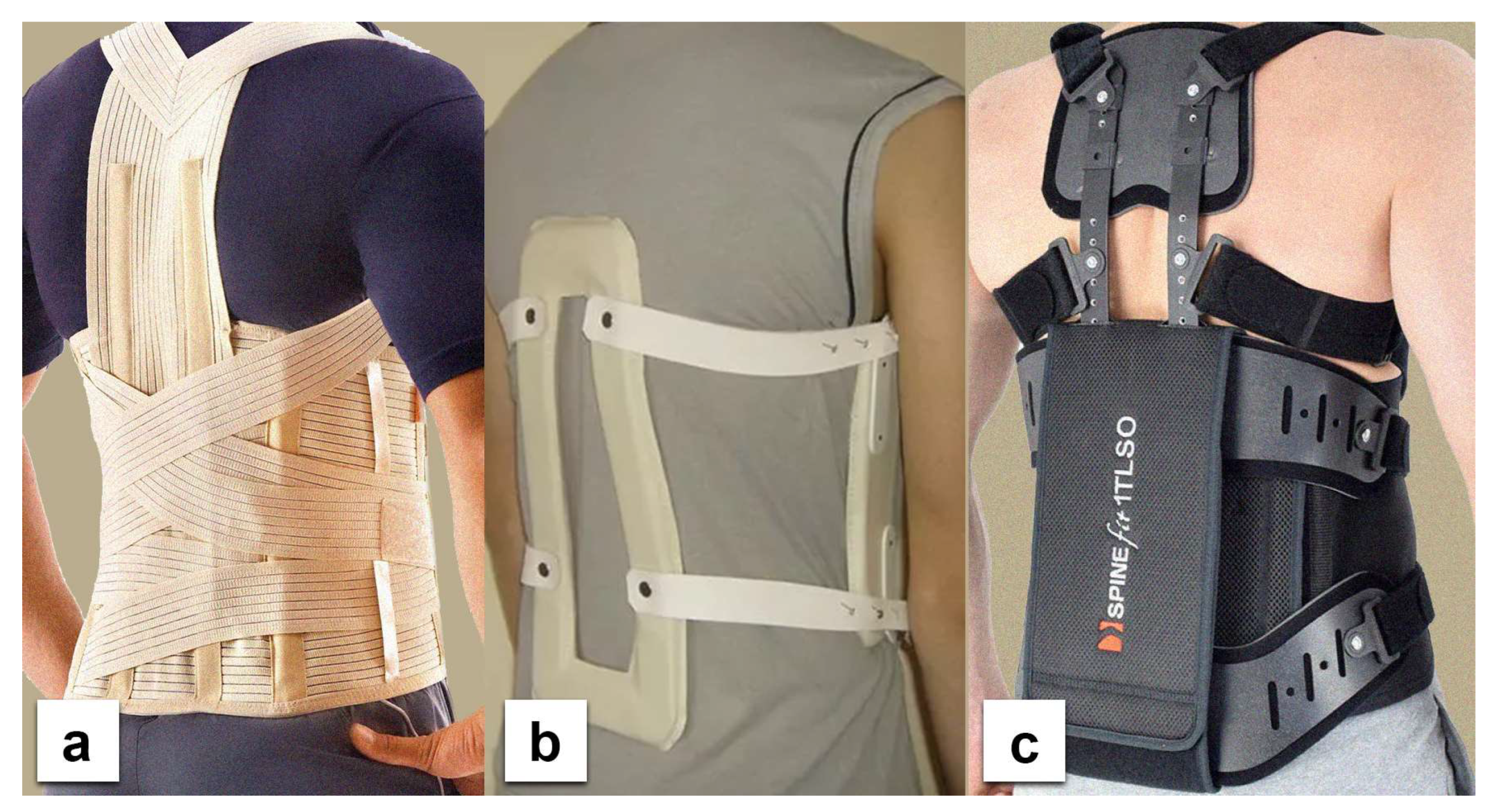
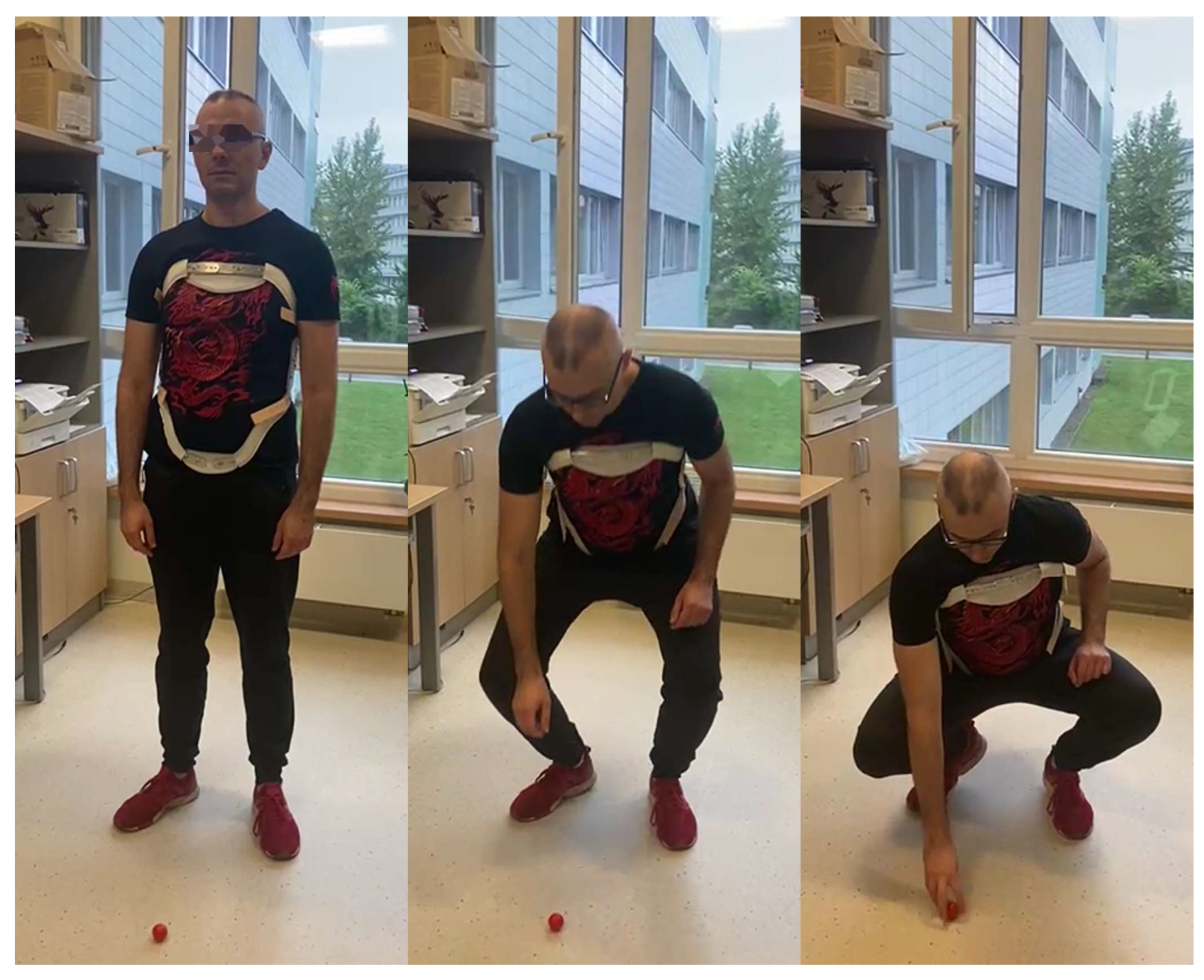
2. Materials and Methods
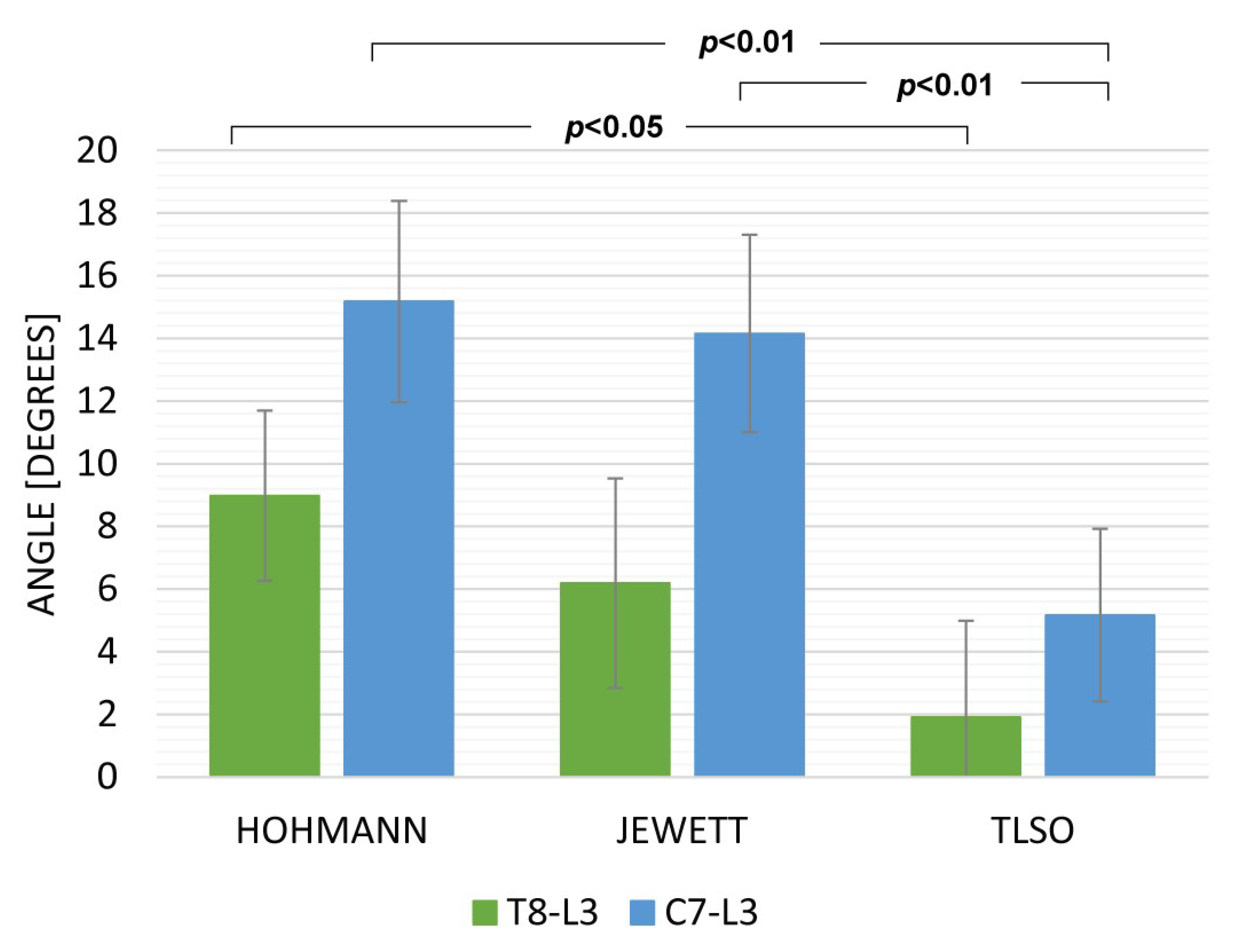
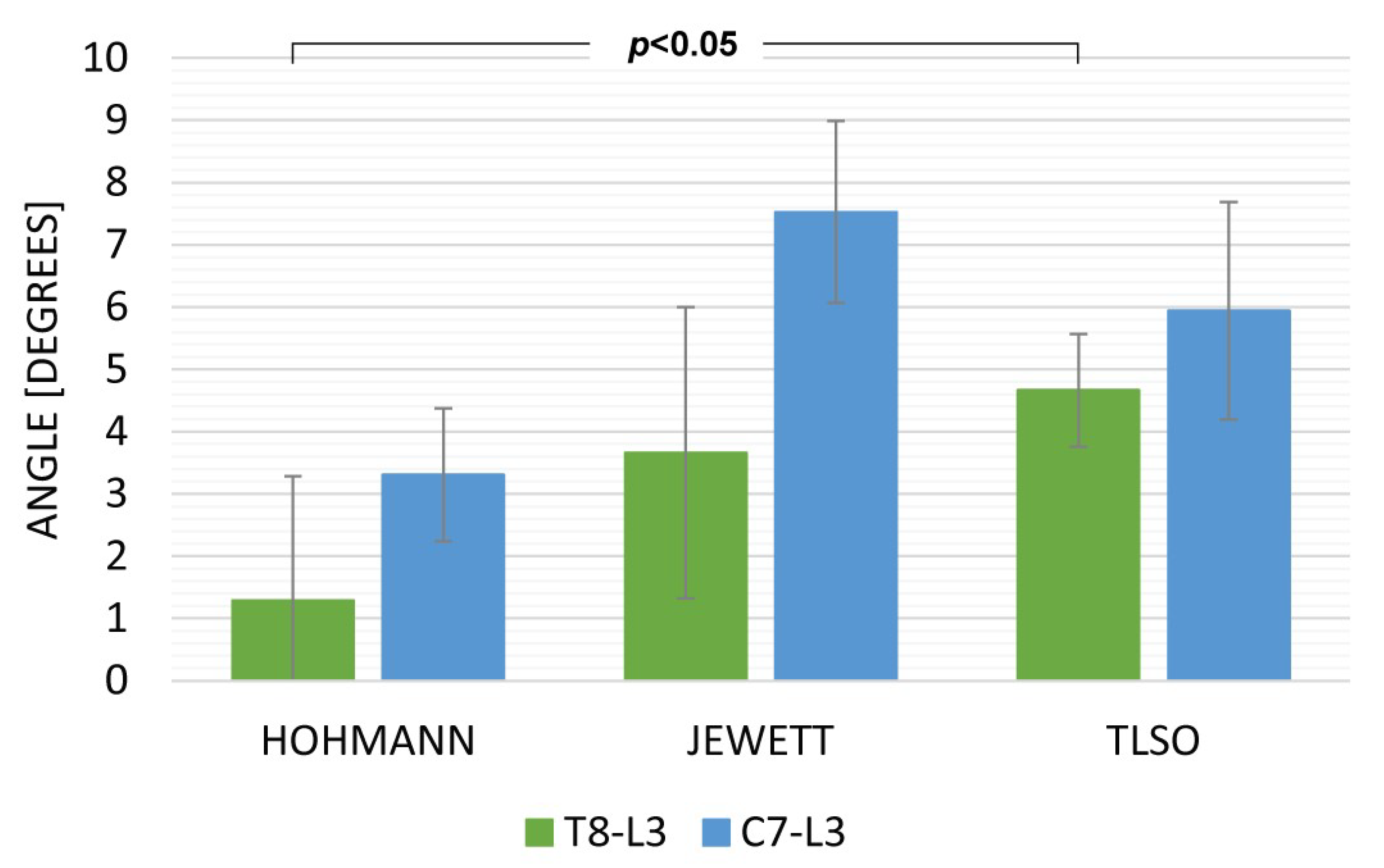
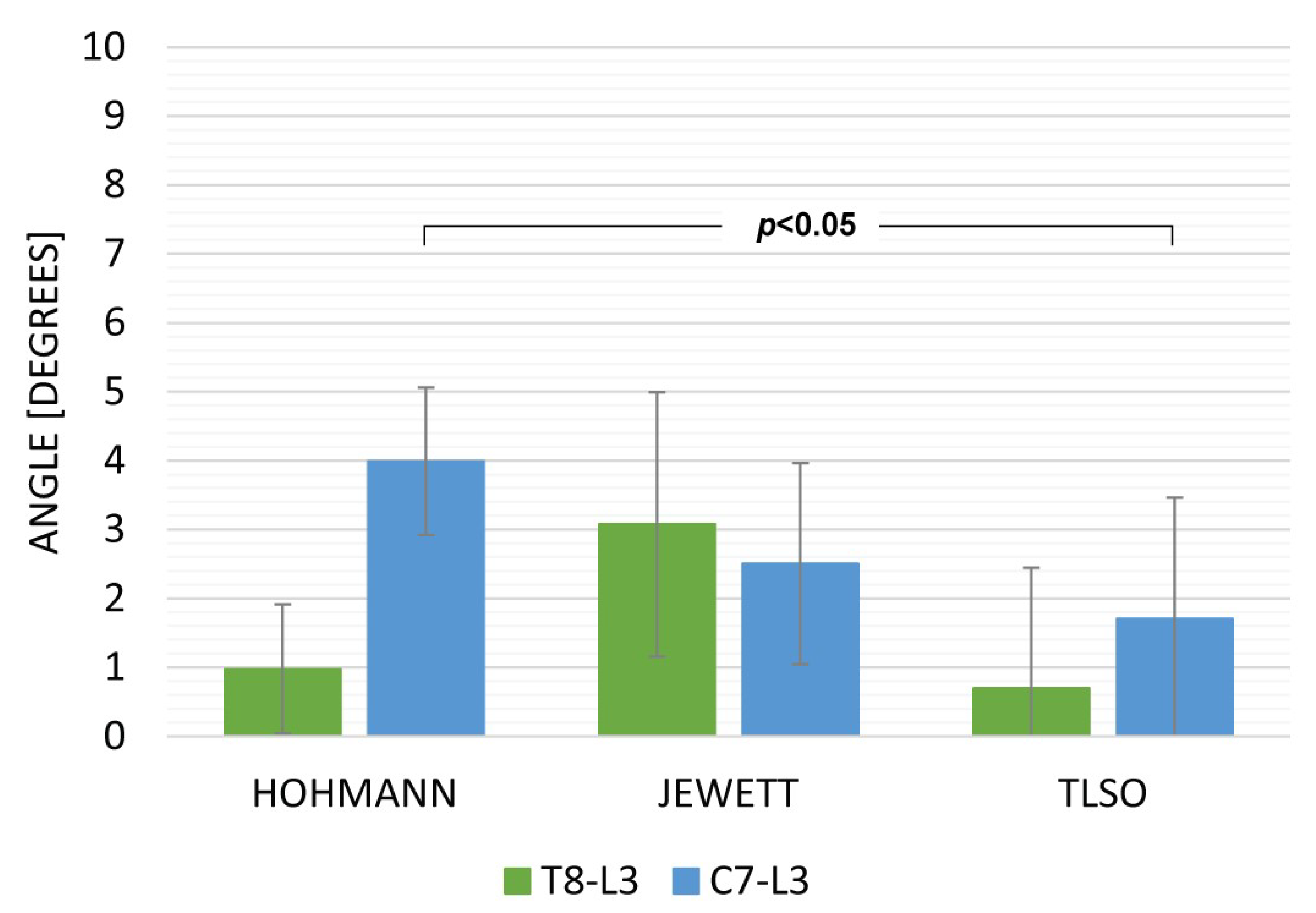
3. Results
4. Discussion
5. Limitations of the Study
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Weppner, J.L.; Alfano, A.P. Principles and Components of Spinal Orthoses. In Atlas of Orthoses and Assistive Devices; Elsevier: Amsterdam, The Netherlands, 2019; pp. 69–89.e2. [Google Scholar] [CrossRef]
- Kaelin, A.J. Adolescent Idiopathic Scoliosis: Indications for Bracing and Conservative Treatments. Ann. Transl. Med. 2020, 8, 28. [Google Scholar] [CrossRef] [PubMed]
- Schwab, F. Treatment with or without an Orthosis Is Equivalent for Thoracolumbar Burst Fracture without Neurologic Injury. J. Bone Jt. Surg.—Am. Vol. 2015, 97, 1374. [Google Scholar] [CrossRef] [PubMed]
- Kato, T.; Inose, H.; Ichimura, S.; Tokuhashi, Y.; Nakamura, H.; Hoshino, M.; Togawa, D.; Hirano, T.; Haro, H.; Ohba, T.; et al. Comparison of Rigid and Soft-Brace Treatments for Acute Osteoporotic Vertebral Compression Fracture: A Prospective, Randomized, Multicenter Study. J. Clin. Med. 2019, 8, 198. [Google Scholar] [CrossRef] [PubMed]
- Curfs, I.; van Rooij, W.; Senden, R.; Grimm, B.; van Hemert, W. Evaluating the Immobilization Effect of Spinal Orthoses Using Sensor-Based Motion Analysis. J. Prosthet. Orthot. 2016, 28, 23–29. [Google Scholar] [CrossRef]
- Negrini, S.; Aulisa, A.G.; Aulisa, L.; Circo, A.B.; de Mauroy, J.C.; Durmala, J.; Grivas, T.B.; Knott, P.; Kotwicki, T.; Maruyama, T.; et al. 2011 SOSORT Guidelines: Orthopaedic and Rehabilitation Treatment of Idiopathic Scoliosis during Growth. Scoliosis 2012, 7, 3. [Google Scholar] [CrossRef] [PubMed]
- Agabegi, S.S.; Asghar, F.A.; Herkowitz, H.N. Spinal Orthoses. J. Am. Acad. Orthop. Surg. 2010, 18, 657–667. [Google Scholar] [CrossRef]
- Johnson, D.D.; Ashton-Miller, J.A.; Shih, A.J. Active Spinal Orthosis to Reduce Lumbar Postural Muscle Activity in Flexed Postures. J. Prosthet. Orthot. 2016, 28, 109–113. [Google Scholar] [CrossRef]
- Van der Roer, N.; de Lange, E.S.M.; Bakker, F.C.; de Vet, H.C.W.; van Tulder, M.W. Management of Traumatic Thoracolumbar Fractures: A Systematic Review of the Literature. Eur. Spine J. 2005, 14, 527–534. [Google Scholar] [CrossRef]
- Wallace, N.; McHugh, M.; Patel, R.; Aleem, I.S. Effects of Bracing on Clinical and Radiographic Outcomes Following Thoracolumbar Burst Fractures in Neurologically Intact Patients a Meta-Analysis of Randomized Controlled Trials. JBJS Rev. 2019, 7, e9. [Google Scholar] [CrossRef]
- Hofler, R.C.; Jones, G.A. Bracing for Acute and Subacute Osteoporotic Compression Fractures: A Systematic Review of the Literature. World Neurosurg. 2020, 141, e453–e460. [Google Scholar] [CrossRef]
- Casazza, B.A. Diagnosis and Treatment of Acute Low Back Pain. Am. Fam. Physician 2012, 85, 343–350. [Google Scholar] [PubMed]
- Annaswamy, T.M.; Cunniff, K.J.; Kroll, M.; Yap, L.; Hasley, M.; Lin, C.K.; Petrasic, J. Lumbar Bracing for Chronic Low Back Pain: A Randomized Controlled Trial. Am. J. Phys. Med. Rehabil. 2021, 100, 742–749. [Google Scholar] [CrossRef] [PubMed]
- Mi, J.; Ye, J.; Zhao, X.; Zhao, J. Effects of Lumbosacral Orthoses on Postural Control in Individuals with or without Non-Specific Low Back Pain. Eur. Spine J. 2018, 27, 180–186. [Google Scholar] [CrossRef]
- Van Duijvenbode, I.C.D.; Jellema, P.; van Poppel, M.N.M.; van Tulder, M.W. Lumbar Supports for Prevention and Treatment of Low Back Pain. Cochrane Database Syst. Rev. 2008, 2008, CD001823. [Google Scholar] [CrossRef] [PubMed]
- Takasaki, H.; Miki, T. The Impact of Continuous Use of Lumbosacral Orthoses on Trunk Motor Performance: A Systematic Review with Meta-Analysis. Spine J. 2017, 17, 889–900. [Google Scholar] [CrossRef] [PubMed]
- Azadinia, F.; Ebrahimi, E.; Kamyab, M.; Parnianpour, M.; Cholewicki, J.; Maroufi, N. Can Lumbosacral Orthoses Cause Trunk Muscle Weakness? A Systematic Review of Literature. Spine J. 2017, 17, 589–602. [Google Scholar] [CrossRef] [PubMed]
- Lang, G.; Hirschmüller, A.; Patermann, S.; Eichelberger, P.; Strohm, P.; Baur, H.; Südkamp, N.P.; Herget, G.W. Efficacy of Thoracolumbar Bracing in Spinal Immobilization: Precise Assessment of Gross, Intersegmental, and Segmental Spinal Motion Restriction by a 3D Kinematic System. World Neurosurg. 2018, 116, e128–e146. [Google Scholar] [CrossRef]
- Poitras, I.; Dupuis, F.; Bielmann, M.; Campeau-Lecours, A.; Mercier, C.; Bouyer, L.J.; Roy, J.S. Validity and Reliability of Wearable Sensors for Joint Angle Estimation: A Systematic Review. Sensors 2019, 19, 1555. [Google Scholar] [CrossRef]
- Al-Amri, M.; Nicholas, K.; Button, K.; Sparkes, V.; Sheeran, L.; Davies, J.L. Inertial Measurement Units for Clinical Movement Analysis: Reliability and Concurrent Validity. Sensors 2018, 18, 719. [Google Scholar] [CrossRef]
- Beange, K.H.E.; Chan, A.D.C.; Beaudette, S.M.; Graham, R.B. Concurrent Validity of a Wearable IMU for Objective Assessments of Functional Movement Quality and Control of the Lumbar Spine. J. Biomech. 2019, 97, 109356. [Google Scholar] [CrossRef]
- Pfeifer, M.; Gehlen, M.; Hinz, C. Spinal Orthoses in the Treatment of Vertebral Fractures with Osteoporosis: A Systematic Review Article. Z. Rheumatol. 2017, 76, 860–868. [Google Scholar] [CrossRef] [PubMed]
- Meccariello, L.; Muzii, V.F.; Falzarano, G.; Medici, A.; Carta, S.; Fortina, M.; Ferrata, P. Dynamic Corset versus Three-Point Brace in the Treatment of Osteoporotic Compression Fractures of the Thoracic and Lumbar Spine: A Prospective, Comparative Study. Aging Clin. Exp. Res. 2016, 29, 443–449. [Google Scholar] [CrossRef] [PubMed]
- Ehrenhofer, A.; Wallmersperger, T. Shell-Forming Stimulus-Active Hydrogel Composite Membranes: Concept and Modeling. Micromachines 2020, 11, 541. [Google Scholar] [CrossRef] [PubMed]
- Sadeghian, F.; Zakerzadeh, M.R.; Karimpour, M.; Baghani, M. Compliant Orthoses for Repositioning of Knee Joint Based on Super-Elasticity of Shape Memory Alloys. J. Intell. Mater. Syst. Struct. 2018, 29, 3136–3150. [Google Scholar] [CrossRef]
- Zhou, L.; Fischer, E.; Tunca, C.; Brahms, C.M.; Ersoy, C.; Granacher, U.; Arnrich, B. How We Found Our IMU: Guidelines to IMU Selection and a Comparison of Seven IMUs for Pervasive Healthcare Applications. Sensors 2020, 20, 4090. [Google Scholar] [CrossRef] [PubMed]

| Sl. No. | Criteria | Rating |
|---|---|---|
| 1. | …is comfortable | 1 2 3 4 5 |
| 2. | …causes no pain | 1 2 3 4 5 |
| 3. | …does not pinch | 1 2 3 4 5 |
| 4. | …can easily be worn under clothes | 1 2 3 4 5 |
| 5. | …is easy and quick to use | 1 2 3 4 5 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fercho, J.; Krakowiak, M.; Yuser, R.; Szmuda, T.; Zieliński, P.; Szarek, D.; Pettersson, S.D.; Miękisiak, G. Evaluation of Movement Restriction of Spinal Orthoses Using Inertial Measurement Units. Int. J. Environ. Res. Public Health 2022, 19, 16515. https://doi.org/10.3390/ijerph192416515
Fercho J, Krakowiak M, Yuser R, Szmuda T, Zieliński P, Szarek D, Pettersson SD, Miękisiak G. Evaluation of Movement Restriction of Spinal Orthoses Using Inertial Measurement Units. International Journal of Environmental Research and Public Health. 2022; 19(24):16515. https://doi.org/10.3390/ijerph192416515
Chicago/Turabian StyleFercho, Justyna, Michał Krakowiak, Rami Yuser, Tomasz Szmuda, Piotr Zieliński, Dariusz Szarek, Samuel D. Pettersson, and Grzegorz Miękisiak. 2022. "Evaluation of Movement Restriction of Spinal Orthoses Using Inertial Measurement Units" International Journal of Environmental Research and Public Health 19, no. 24: 16515. https://doi.org/10.3390/ijerph192416515
APA StyleFercho, J., Krakowiak, M., Yuser, R., Szmuda, T., Zieliński, P., Szarek, D., Pettersson, S. D., & Miękisiak, G. (2022). Evaluation of Movement Restriction of Spinal Orthoses Using Inertial Measurement Units. International Journal of Environmental Research and Public Health, 19(24), 16515. https://doi.org/10.3390/ijerph192416515










