The Impact of Physical Activity at School on Eating Behaviour and Leisure Time of Early Adolescents
Abstract
1. Introduction
2. Materials and Methods
2.1. Subjects
2.2. Procedure
2.3. Questionnaire
2.4. Statistical Analysis
3. Results
3.1. Group Characteristics
3.2. Eating Behaviour
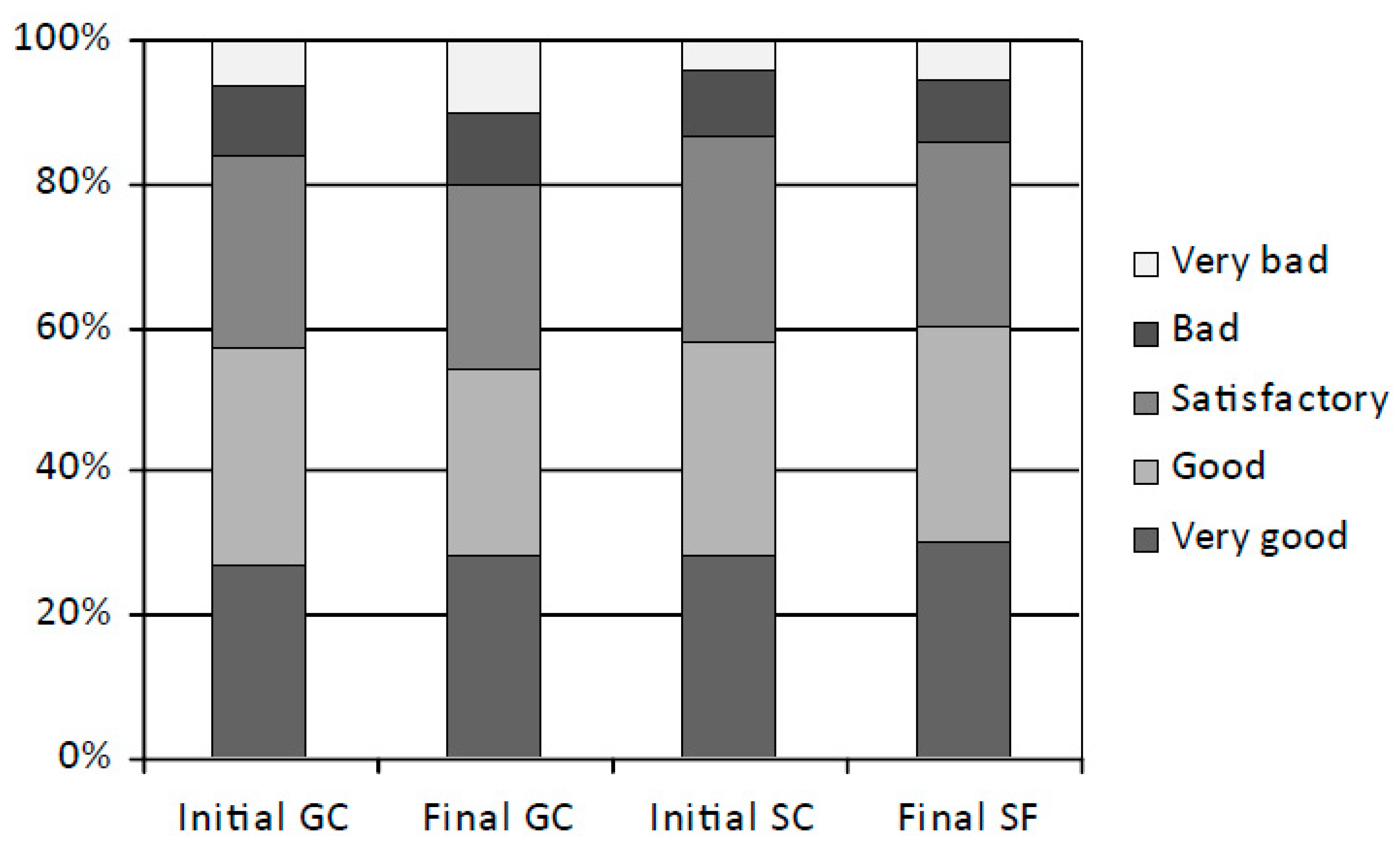
3.2.1. Eating Behaviour in Particular Sessions
3.2.2. Changes in Eating Behaviour over Time
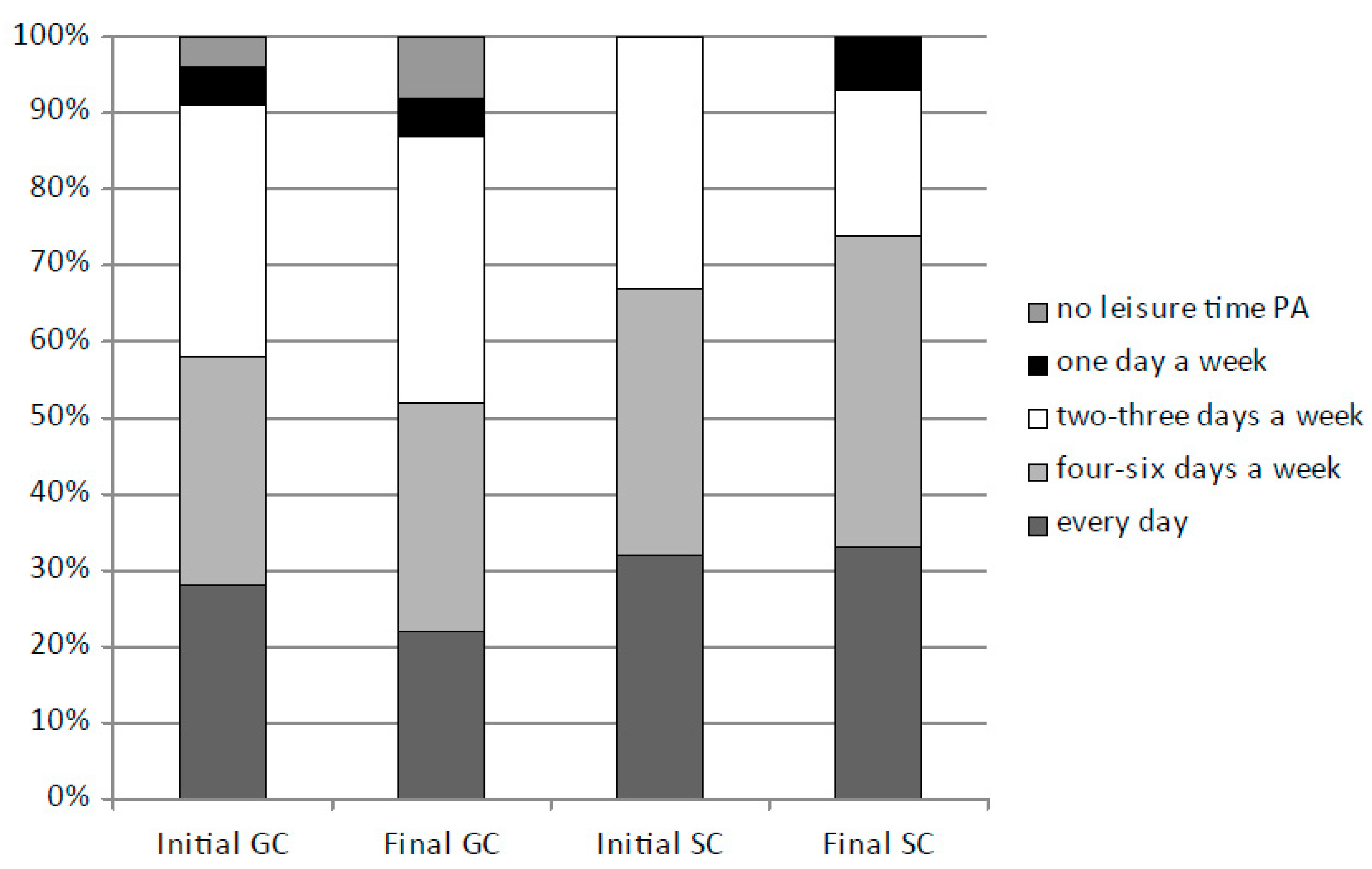
3.3. Frequency of Leisure Time PA
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Bluher, M. Obesity: Global epidemiology and pathogenesis. Nat. Rev. Endocrinol. 2019, 15, 288–298. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. WHO European Regional Obesity Report 2022; WHO Regional Office for Europe: Copenhagen, Denmark, 2022. [Google Scholar]
- Fijałkowska, A.; Dzielska, A.; Mazur, J.; Korzycka, M.; Breda, J.; Oblacińska, A. Childhood Obesity Surveillance Initiative (COSI) in Poland: Implementation of Two Rounds of the Study in the Context of International Methodological Assumptions. J. Mother Child. 2020, 24, 2–12. [Google Scholar] [PubMed]
- Waxman, A. Prevention of chronic diseases: WHO global strategy on diet, physical activity and health. Food Nutr. Bull. 2003, 24, 275–280. [Google Scholar] [CrossRef]
- Di Cesare, M.; Sorić, M.; Bovet, P.; Miranda, J.J.; Bhutta, Z.; Stevens, G.A.; Laxmaiah, A.; Kengne, A.P.; Bentham, J. The epidemiological burden of obesity in childhood: A worldwide epidemic requiring urgent action. BMC Med. 2019, 17, 212. [Google Scholar] [CrossRef]
- Navidad, L.; Padial-Ruz, R.; González, M.C. Nutrition, Physical Activity, and New Technology Programs on Obesity Prevention in Primary Education: A Systematic Review. Int. J. Environ. Res. Public Health 2021, 18, 10187. [Google Scholar] [CrossRef]
- Zeiler, M.; Waldherr, K.; Philipp, J.; Nitsch, M.; Dür, W.; Karwautz, A.; Wagner, G. Prevalence of Eating Disorder Risk and Associations with Health-related Quality of Life: Results from a Large School-based Population Screening. Eur. Eat. Disord. Rev. 2016, 24, 9–18. [Google Scholar] [CrossRef]
- World Health Organization. Noncommunicable Diseases: Childhood Overweight and Obesity. Available online: https://www.who.int/dietphysicalactivity/childhood/en/ (accessed on 23 September 2022).
- Buyuktuncer, Z.; Ayaz, A.; Dedebayraktar, D.; Inan-Eroglu, E.; Ellahi, B.; Besler, H.T. Promoting a Healthy Diet in Young Adults: The Role of Nutrition Labelling. Nutrients 2018, 10, 1335. [Google Scholar] [CrossRef]
- Grace, G.A.; Edward, S.; Gopalakrishnan, S. Dietary Habits and Obesity among Adolescent School Children: A Case Control Study in an Urban Area of Kancheepuram District. Indian J. Community Med. 2021, 46, 637–640. [Google Scholar] [CrossRef]
- Stok, F.M.; Renner, B.; Clarys, P.; Lien, N.; Lakerveld, J.; Deliens, T. Understanding Eating Behavior during the Transition from Adolescence to Young Adulthood: A Literature Review and Perspective on Future Research Directions. Nutrients 2018, 10, 667. [Google Scholar] [CrossRef]
- Hamułka, J.; Wadolowska, L.; Hoffmann, M.; Kowalkowska, J.; Gutkowska, K. Effect of an Education Program on Nutrition Knowledge, Attitudes toward Nutrition, Diet Quality, Lifestyle, and Body Composition in Polish Teenagers. The ABC of Healthy Eating Project: Design, Protocol, and Methodology. Nutrients 2018, 10, 1439. [Google Scholar] [CrossRef]
- World Health Organization. Healthy Diet. Available online: https://www.who.int/news-room/fact-sheets/detail/healthy-diet (accessed on 23 September 2022).
- Diethelm, K.; Jankovic, N.; Moreno, L.A.; Huybrechts, I.; De Henauw, S.; De Vriendt, T.; González-Gross, M.; Leclercq, C.; Gottrand, F.; Gilbert, C.C. Food intake of European adolescents in the light of different food-based dietary guidelines: Results of the HELENA (Healthy Lifestyle in Europe by Nutrition in Adolescence) Study. Public Health Nutr. 2012, 15, 386–398. [Google Scholar] [CrossRef]
- Bunc, V. Obesity-causes and remedies. Phys. Act. Rev. 2016, 7, 50–56. [Google Scholar] [CrossRef]
- Reilly, J.J.; Kelly, J. Long-term impact of overweight and obesity in childhood and adolescence on morbidity and premature mortality in adulthood: Systematic review. Int. J. Obes. 2011, 35, 891–898. [Google Scholar] [CrossRef] [PubMed]
- Justamente, I.; Raudeniece, J.; Ozolina-Moll, L.; Guadalupe-Grau, A.; Reihmane, D. Comparative Analysis of the Effects of Daily Eating Habits and Physical Activity on Anthropometric Parameters in Elementary School Children in Latvia: Pach Study. Nutrients 2020, 12, 3818. [Google Scholar] [CrossRef]
- Ługowska, K.; Kolanowski, W.; Trafialek, J. Eating Behaviour and Physical Fitness in 10-Year-Old Children Attending General Education and Sports Classes. Int. J. Environ. Res. Public Health 2020, 17, 6467. [Google Scholar] [CrossRef]
- Wells, K.R.; Jeacocke, N.A.; Appaneal, R.; Smith, H.D.; Vlahovich, N.; Burke, L.M.; Hughes, D. The Australian Institute of Sport (AIS) and National Eating Disorders Collaboration (NEDC) Position Statement on Disordered Eating in High Performance Sport. Br. J. Sports Med. 2020, 54, 1247–1258. [Google Scholar] [CrossRef] [PubMed]
- Bonci, C.M.; Bonci, L.J.; Granger, L.R.; Johnson, C.L.; Malina, R.M.; Milne, L.W.; Ryan, R.R.; Vanderbunt, E.M. National Athletic Trainers’ Association Position Statement: Preventing, Detecting, and Managing Disordered Eating in Athletes. J. Athl. Train. 2008, 43, 80–108. [Google Scholar] [CrossRef] [PubMed]
- Gacek, M. Analysis of Dietetary habits among junior and senior soccer players as seen qualitative recommendations for athletes. Probl. Hig. Epidemiol. 2018, 99, 289–293. [Google Scholar]
- Abbey, E.L.; Wright, C.J.; Kirkpatrick, C.M. Nutrition practices and knowledge among NCAA Division III football players. J. Int. Soc. Sports Nutr. 2017, 14, 13. [Google Scholar] [CrossRef]
- Hoch, A.Z.; Goossen, K.; Kretschmer, T. Nutritional requirements of the child and teenage athlete. Phys. Med. Rehabil. Clin. N. Am. 2008, 19, 373–398. [Google Scholar] [CrossRef]
- World Health Organization. Guidelines on Physical Activity and Sedentary Behaviour; WHO: Geneva, Switzerland, 2020. [Google Scholar]
- Physical Activity Guidelines Advisory Committee. 2018 Physical Activity Guidelines Advisory Committee Scientific Report; U.S. Department of Health and Human Services: Washington, DC, USA, 2018.
- Kolanowski, W.; Ługowska, K.; Trafialek, J. Increased Physical Activity at School Benefits Arterial Blood Pressure in Children—A Prospective Follow-Up Cohort Study. Int. J. Environ. Res. Public Health 2022, 19, 4662. [Google Scholar] [CrossRef] [PubMed]
- Ługowska, K.; Kolanowski, W.; Trafialek, J. The Impact of Physical Activity at School on Children’s Body Mass during 2 Years of Observation. Int. J. Environ. Res. Public Health 2022, 19, 3287. [Google Scholar] [CrossRef] [PubMed]
- Pate, R.R.; Pratt, M.; Blair, S.N.; Haskell, W.L.; Macera, C.A.; Bouchard, C.; Buchner, D.; Ettinger, W.; Heath, G.W.; King, A.C.; et al. Physical activity and public health. A recommendation from the Centers for Disease Control and Prevention and the American College of Sports Medicine. JAMA 1995, 273, 402–407. [Google Scholar] [CrossRef] [PubMed]
- Lang, J.J.; Tremblay, M.S.; Léger, L.; Olds, T.; Tomkinson, G.R. International variability in 20 m shuttle run performance in children and youth: Who are the fittest from a 50-country comparison? A systematic literature review with pooling of aggregate results. Br. J. Sports Med. 2018, 52, 276. [Google Scholar] [CrossRef]
- Guthold, R.; Stevens, G.A.; Riley, L.M.; Bull, F.C. Global trends in insufficient physical activity among adolescents: A pooled analysis of 298 population-based surveys with 1·6 million participants. Lancet Child Adolesc. Health 2020, 4, 23–35. [Google Scholar] [CrossRef]
- Hallal, P.C.; Andersen, L.B.; Bull, F.C.; Guthold, R.; Haskell, W.; Ekelund, U. Physical Activity Series Working Group. Global physical activity levels: Surveillance progress, pitfalls, and prospects. Lancet 2012, 380, 247–257. [Google Scholar] [CrossRef]
- Kovacs, V.A.; Starc, G.; Brandes, M.; Kaj, M.; Blagus, R.; Leskošek, B.; Suesse, T.; Dinya, E.; Guinhouya, B.C.; Zito, V.; et al. Physical activity, screen time and the COVID-19 school closures in Europe—An observational study in 10 countries. Eur. J. Sport Sci. 2022, 22, 1094–1103. [Google Scholar] [CrossRef]
- World Health Organization. Global Action Plan on Physical Activity 2018–2030: More Active People for a Healthier World; WHO: Geneva, Switzerland, 2018. [Google Scholar]
- Messing, S.; Rütten, A.; Abu-Omar, K.; Ungerer-Röhrich, U.; Goodwin, L.; Burlacu, I.; Gediga, G. How Can Physical Activity Be Promoted Among Children and Adolescents? A Systematic Review of Reviews Across Settings. Front. Publ. Health 2019, 7, 55. [Google Scholar] [CrossRef]
- Kerksick, C.M.; Arent, S.; Schoenfeld, B.J.; Stout, J.R.; Campbell, B.; Wilborn, C.D.; Taylor, L.; Kalman, D.; Smith-Ryan, A.E.; Kreider, R.; et al. International society of sports nutrition position stand: Nutrient timing. J. Int. Soc. Sports Nutr. 2017, 14, 33. [Google Scholar] [CrossRef]
- World Health Organization. Commission on Ending Childhood Obesity. Report of the Commission on Ending Childhood Obesity; WHO: Geneva, Switzerland, 2016. [Google Scholar]
- Ortega, F.B.; Cadenas-Sanchez, C.; Migueles, J.H.; Labayen, I.; Ruiz, J.R.; Sui, X.; Blair, S.N.; Martínez-Vizcaino, V.; Lavie, C.J. Role of Physical Activity and Fitness in the Characterization and Prognosis of the Metabolically Healthy Obesity Phenotype: A Systematic Review and Meta-analysis. Prog. Cardiovasc. Dis. 2018, 61, 190–205. [Google Scholar] [CrossRef]
- Bull, F.C.; Al-Ansari, S.S.; Biddle, S.; Borodulin, K.; Buman, M.P.; Cardon, G.; Carty, C.; Chaput, J.P.; Chastin, S.; Chou, R.; et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br. J. Sports Med. 2020, 54, 1451–1462. [Google Scholar] [CrossRef]
- Lipsky, L.M.; Nansel, T.R.; Haynie, D.; Liu, D.; Li, K.; Pratt, C.A.; Iannotti, R.J.; Dempster, K.; Simons-Morton, B. Diet quality of US adolescents during the transition to adulthood: Changes and predictors. Am. J. Clin. Nutr. 2017, 105, 1424–1432. [Google Scholar] [CrossRef] [PubMed]
- Noll, M.; Rodrigues, A.P.; Silveira, E.A. Sport Types and Time Spent Playing Sport Are Associated with Eating Pattern Among Young Brazilian Athletes. Asian J. Sports Med. 2019, 10, 96561. [Google Scholar] [CrossRef]
- Całyniuk, B.; Kiciak, A.; Grochowska-Niedworok, E. Health- and nutrition-related behaviour of pupils attending sports schools in relation to their gender and body mass index—Preliminary report. Med. Og. Nauk. Zdr. 2014, 20, 186–191. [Google Scholar] [CrossRef]
- Dortch, K.S.; Gay, J.; Springer, A.; Kohl, H.W.; Sharma, S.; Saxton, D.; Wilson, K.; Hoelscher, D. The Association between Sport Participation and Dietary Behaviors among Fourth Graders in the School Physical Activity and Nutrition Survey, 2009–2010. Am. J. Heal. Promot. 2014, 29, 99–106. [Google Scholar] [CrossRef]
- Spendlove, J.K.; Heaney, S.E.; Gifford, J.A.; Prvan, T.; Denyer, G.S.; O’Connor, H.T. Evaluation of general nutrition knowledge in elite Australian athletes. Br. J. Nutr. 2012, 107, 1871–1880. [Google Scholar] [CrossRef] [PubMed]
- Spronk, I.; Heaney, S.E.; Prvan, T.; O’Connor, H.T. Relationship between general nutrition knowledge and dietary quality in elite athletes. Int. J. Sport Nutr. Exerc. Metab. 2015, 25, 243–251. [Google Scholar] [CrossRef]
- Manore, M.M.; Patton-Lopez, M.M.; Meng, Y.; Wong, S.S. Sport Nutrition Knowledge, Behaviors and Beliefs of High School Soccer Players. Nutrients 2017, 9, 350. [Google Scholar] [CrossRef]
- Partida, S.; Marshall, A.; Henry, R.; Townsend, J.; Toy, A. Attitudes toward Nutrition and Dietary Habits and Effectiveness of Nutrition Education in Active Adolescents in a Private School Setting: A Pilot Study. Nutrients 2018, 10, 1260. [Google Scholar] [CrossRef]
- Williams, J.; Buoncristiano, M.; Nardone, P.; Rito, A.I.; Spinelli, A.; Hejgaard, T.; Kierkegaard, L.; Nurk, E.; Kunešová, M.; Musić Milanović, S.; et al. A Snapshot of European Children’s Eating Habits: Results from the Fourth Round of the WHO European Childhood Obesity Surveillance Initiative (COSI). Nutrients 2020, 12, 2481. [Google Scholar] [CrossRef]
- Moral-García, J.E.; Agraso-López, A.D.; Ramos-Morcillo, A.J.; Jiménez, A.; Jiménez-Eguizábal, A. The Influence of Physical Activity, Diet, Weight Status and Substance Abuse on Students’ Self-Perceived Health. Int. J. Environ. Res. Public Health 2020, 17, 1387. [Google Scholar] [CrossRef]
- Logan, K.; Cuff, S. Organized Sports for Children, Preadolescents, and Adolescents. Pediatrics 2019, 143, 20190997. [Google Scholar] [CrossRef] [PubMed]
- Faul, F.; Erdfelder, E.; Lang, A.-G.; Buchner, A. G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav. Res. Methods 2007, 39, 175–191. [Google Scholar] [CrossRef] [PubMed]
- Microsoft Excel. Available online: https://www.microsoft.com/pl-pl/microsoft-365/excel (accessed on 4 March 2022).
- StatSoft. Elektroniczny Podręcznik Statystyki; StatSoft, Inc.: Kraków, Poland, 2006; Available online: https://www.statsoft.pl/textbook/stathome.html (accessed on 4 March 2022). (In Poland)
- Sullivan, G.M.; Feinn, R. Using Effect Size—Or Why the P Value Is Not Enough. J. Grad. Med. Educ. 2012, 4, 279–282. [Google Scholar] [CrossRef] [PubMed]
- Kansra, A.R.; Lakkunarajah, S.; Jay, M.S. Childhood and Adolescent Obesity: A Review. Front Pediatr. 2021, 8, 581461. [Google Scholar] [CrossRef]
- Grao-Cruces, A.; Fernández-Martínez, A.; Nuviala, A. Association of Fitness With Life Satisfaction, Health Risk Behaviors, and Adherence to the Mediterranean Diet in Spanish Adolescents. J. Strength Cond. Res. 2014, 28, 2164–2172. [Google Scholar] [CrossRef]
- Biddle, S.J.H.; Pearson, N.; Ross, G.M.; Braithwaite, R. Tracking of sedentary behaviours of young people: A systematic review. Prev. Med. 2010, 51, 345–351. [Google Scholar] [CrossRef]
- De Baere, S.; Philippaerts, R.; De Martelaer, K.; Lefevre, J. Associations Between Objectively Assessed Components of Physical Activity and Health-Related Fitness in 10- to 14-Year-Old Children. J. Phys. Act. Health 2016, 13, 993–1001. [Google Scholar] [CrossRef]
- Desbrow, B.; McCormack, J.; Burke, L.M.; Cox, G.R.; Fallon, K.; Hislop, M.; Logan, R.; Marino, N.; Sawyer, S.M.; Shaw, G.; et al. Sports Dietitians Australia Position Statement: Sports Nutrition for the Adolescent Athlete. Int. J. Sport Nutr. Exerc. Metab. 2014, 24, 570–584. [Google Scholar] [CrossRef]
- Rippin, H.L.; Hutchinson, J.; Jewell, J.; Breda, J.J.; Cade, J.E. Child and adolescent nutrient intakes from current national dietary surveys of European populations. Nutr. Res. Rev. 2019, 32, 38–69. [Google Scholar] [CrossRef]
- Comerford, K.B.; Miller, G.D.; Boileau, A.C.; Masiello Schuette, S.M.; Jgiddens, J.C.; Brown, K.A. Global Review of Dairy Recommendations in Food-Based Dietary Guidelines. Front. Nutr. 2021, 8, 671999. [Google Scholar] [CrossRef] [PubMed]
- Basiak-Rasała, A.; Górna, S.; Krajewska, J.; Kolator, M.; Pazdro-Zastawny, K.; Basiak, A.; Zatoński, T. Nutritional habits according to age and BMI of 6-17-year-old children from the urban municipality in Poland. J. Health Popul. Nutr. 2022, 41, 17. [Google Scholar] [CrossRef] [PubMed]
- Dolipska, A.; Majerczyk, M.; Gora, A.; Janion, K.; Szczepanska, E. Eating behaviours of primary school pupils from Slaskie, Malopolskie and Opolskie Voivodeships in Poland. Rocz. Panstw. Zakl. Hig. 2018, 69, 2. [Google Scholar]
- Cooper, S.B.; Bandelow, S.; Nevill, M.E. Breakfast consumption and cognitive function in adolescent schoolchildren. Physiol. Behav. 2011, 103, 431–439. [Google Scholar] [CrossRef] [PubMed]
- Hopkins, L.C.; Sattler, M.; Steeves, E.A.; Jones-Smith, J.C.; Gittelsohn, J. Breakfast consumption frequency and its relationships to overall diet quality, using healthy eating index 2010, and body mass index among adolescents in a low-income urban setting. Ecol. Food Nutr. 2017, 56, 297–311. [Google Scholar] [CrossRef]
- Coulthard, J.D.; Palla, L.; Pot, G.K. Breakfast consumption and nutrient intakes in 4–18-year-olds: UK National Diet and Nutrition Survey Rolling Programme (2008–2012). Br. J. Nutr. 2017, 118, 280–290. [Google Scholar] [CrossRef]
- Timlin, M.T.; Pereira, M.A.; Story, M.; Neumark-Sztainer, D. Breakfast eating and weight change in a 5-year prospective analysis of adolescents: Project EAT (Eating Among Teens). Pediatrics 2008, 121, 638–645. [Google Scholar] [CrossRef]
- Kawalec, A.; Pawlas, K. Breakfast Frequency and Composition in a Group of Polish Children Aged 7–10 Years. Nutrients 2021, 13, 2241. [Google Scholar] [CrossRef]
- Zielińska, M.; Hamułka, J.; Gajda, K. Family influences on breakfast frequency and quality among primary school pupils in Warsaw and its surrounding areas. Rocz. Panstw. Zakl. Hig. 2015, 66, 143–149. [Google Scholar]
- Noll, M.; Rodrigues, A.P.S.; Silveira, E.A. The health-related determinants of eating pattern of high school athletes in Goiás, Brazil. Arch. Public Health 2020, 78, 9. [Google Scholar] [CrossRef]
- Wądołowska, L.; Hamulka, J.; Kowalkowska, J.; Ulewicz, N.; Gornicka, M.; Jeruszka-Bielak, M.; Kostecka, M.; Wawrzyniak, A. Skipping breakfast and a meal at school: Its correlates in adiposity context. report from the ABC of healthy eating study of polish teenagers. Nutrients 2019, 11, 1563. [Google Scholar] [CrossRef] [PubMed]
- Potempa-Jeziorowska, M.; Jonczyk, P.; Swiętochowska, E.; Kucharzewski, M. The Analysis of the Nutritional Status and Dietary Habits among Children Aged 6–10 Years Old Attending Primary Schools in Poland. Int. J. Environ. Res. Public Health 2022, 19, 953. [Google Scholar] [CrossRef] [PubMed]
- Mazur, J.; Małkowska-Szkutnik, A. Zdrowie Uczniów w 2018 Roku na tle Nowego Modelu Badań HBSC; Instytut Matki i Dziecka: Warsaw, Poland, 2018. [Google Scholar]
- Myszkowska-Ryciak, J.; Harton, A.; Lange, E.; Laskowski, W.; Gajewska, D. Nutritional behaviors of Polish adolescents: Results of the wise nutrition—Healthy generation project. Nutrients 2019, 11, 1592. [Google Scholar] [CrossRef]
- Kim, S.Y.; Sim, S.; Park, B.; Kong, I.G.; Kim, J.-H.; Choi, H.G. Dietary habits are associated with school performance in adolescents. Medicine 2016, 95, 3096. [Google Scholar] [CrossRef] [PubMed]
- Inchley, J.; Currie, D.; Budisavljevic, S.; Torsheim, T.; Jastad, A.; Cosma, A. Spotlight on Adolescent Health and Well-Being: Findings from the 2017/2018 Health Behaviour in School-Aged Children (HBSC) Survey in Europe and Canada; World Health Organization Regional Office for Europe: Copenhagen, Denmark, 2020. [Google Scholar]
- Coutinho, L.A.A.; Porto, C.P.M.; Pierucci, A.P.T.R. Critical evaluation of food intake and energy balance in young modern pentathlon athletes: A cross-sectional study. J. Int. Soc. Sports Nutr. 2016, 13, 15. [Google Scholar] [CrossRef]
- Stefańska, E.; Falkowska, A.; Ostrowska, L. Selected nutritional habits children and teenagers aged 10–15 years. Rocz. Panstw. Zakl. Hig. 2012, 63, 91–97. [Google Scholar]
- World Health Organization, Food and Agriculture Organization. Diet, Nutrition and the Prevention of Chronic Diseases. Report of a Joint WHO/FAO Expert Consultation; WHO Technical Report Series No. 916; World Health Organization: Geneva, Switzerland, 2003. [Google Scholar]
- Zadka, K.; Pałkowska-Goździk, E.; Rosołowska-Huszcz, D. Relation between environmental factors and children’s health behaviors contributing to the occurrence of diet-related diseases in central Poland. Int. J. Environ. Res. Public Health 2019, 16, 541. [Google Scholar] [CrossRef]
- Jonczyk, P.; Potempa-Jeziorowska, M.; Świętochowska, E.; Kucharzewski, M. The analysis of the degree of 10–13-yearold children’s nutrition, dietary habits and physical activity in the selected rural and urban areas of Silesian Province (Poland). Egypt. Pediatr. Assoc. Gaz. 2021, 69, 14. [Google Scholar] [CrossRef]
- Lynch, C.; Kristjansdottir, A.G.; Te Velde, S.J.; Lien, N.; Roos, E.; Thorsdottir, I.; Krawinkel, M.; de Almeida, M.D.V.; Papadaki, A.; Ribic, C.H.; et al. Fruit and vegetable consumption in a sample of 11-year-old children in ten European countries—The PRO GREENS cross-sectional survey. Public Health Nutr. 2014, 17, 2436–2444. [Google Scholar] [CrossRef]
- Taliaferro, L.A.; Rienzo, B.A.; Donovan, K.A. Relationships between youth sport participation and selected health risk behaviors from 1999 to 2007. J. Sch. Health 2010, 80, 399–410. [Google Scholar] [CrossRef]
- Pate, R.R.; Trost, S.G.; Levin, S.; Dowda, M. Sports participation and health-related behaviors among US youth. Arch. Pediatr. Adolesc. Med. 2000, 154, 904–911. [Google Scholar] [CrossRef] [PubMed]
- Papanikolaou, Y.; Jonesm, J.M.; Fulgoni, V.L. Several grain dietary patterns are associated with better diet quality and improved shortfall nutrient intakes in US children and adolescents: A study focusing on the 2015–2020 Dietary Guidelines for Americans. Nutr. J. 2017, 16, 266. [Google Scholar] [CrossRef]
- Kamar, M.; Evans, C.; Hugh-Jones, S. Factors Influencing British Adolescents’ Intake of Whole Grains: A Pilot Feasibility Study Using SenseCam Assisted Interviews. Nutrients 2019, 11, 2620. [Google Scholar] [CrossRef] [PubMed]
- García-Munoz, S.; Barlinska, J.; Wojtkowska, K.; Da Quinta, N.; Baranda, A.; Alfaro, B.; Santa Cruz, E. Is it possible to improve healthy food habits in schoolchildren? A cross cultural study among Spain and Poland. Food Qual. Prefer. 2022, 90, 104534. [Google Scholar] [CrossRef]
- Ruiz, L.D. Zuelch, M.L.; Dimitratos, S.M.; Scherr, R.E. Adolescent Obesity: Diet Quality, Psychosocial Health, and Cardiometabolic Risk Factors. Nutrients 2020, 12, 43. [Google Scholar] [CrossRef]
- Ojeda-Rodríguez, A.; Zazpe, I.; Morell-Azanza, L.; Chueca, M.J.; Azcona-Sanjulian, M.C.; Marti, A. Improved Diet Quality and Nutrient Adequacy in Children and Adolescents with Abdominal Obesity after a Lifestyle Intervention. Nutrients 2018, 10, 1500. [Google Scholar] [CrossRef] [PubMed]
- Mendyk, K.; Antos-Latek, K.; Kowalik, M.; Pagacz, K.; Lewicki, M.; Obel, E. Zachowania prozdrowotne w zakresie odżywiania i aktywności fizycznej u dzieci i młodzieży szkolnej w wieku do 18. roku życia Pro-health behavior in adolescents in regard to nourishment and physical activity. Piel Zdr. Publ. 2017, 26, 13–17. [Google Scholar] [CrossRef]
- Roura, E.; Mila-Villarroel, R.; Lucia Pareja, S.; Adot Caballero, A. Assessment of Eating Habits and Physical Activity among Spanish Adolescents. The “Cooking and Active Leisure” TAS Program. PLoS ONE 2016, 11, e0159962. [Google Scholar] [CrossRef][Green Version]
- American Academy of Pediatrics. American Public Health Association. Caring for Our Children, National Health and Safety Performance Standards; American Academy of Pediatrics: Washington, DC, USA, 2019. [Google Scholar]
- Cvetković, B.; Cvetković, M.; Petrušič, T.; Đorđić, V.; Bubanj, S.; Popović, B.; Andrašić, S.; Buišić, S.; Bogataj, Š. Nutrition and Physical Activity Behavior in 11–14-Year-Old Schoolchildren in Serbia. Children 2021, 8, 625. [Google Scholar] [CrossRef]
| No. | Questions | SC | GC | Statistical Measures * | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Ranks | ||||||||||||
| 1 | 2 | 3 | 4 | 5 | 1 | 2 | 3 | 4 | 5 | |||
| 1. | Number of meals per day | 0.00 | 0.00 | 14.33 | 52.00 | 33.66 | 0.00 | 0.00 | 18.67 | 50.67 | 30.66 | χ2 = 1.592, df − 4; p = 0.810, VC = 0.127 |
| 2. | Eating of breakfast | 6.67 | 7.67 | 9.00 | 13.33 | 63.33 | 10.00 | 7.00 | 10.00 | 11.00 | 62.00 | χ2 = 12.220, df = 4; p = 0.020 VC = 0.072 |
| 3. | Eating of lunch at school | 4.00 | 13.33 | 6.67 | 24.00 | 52.00 | 6.67 | 16.00 | 6.67 | 21.33 | 49.33 | χ2 = 1.138, df = 4; p = 0.888, VC = 0.125 |
| 4. | Type of snacks eaten during the day | 21.00 | 22.33 | 5.33 | 40.00 | 11.34 | 24.00 | 26.33 | 4.67 | 37.00 | 8.00 | χ2 = 13.547, df − 4; p = 0.040, VC = 0.189 |
| 5. | Eating of milk and dairy products | 2.33 | 6.00 | 17.00 | 36.00 | 38.67 | 3.33 | 1.67 | 21.00 | 38.66 | 35.33 | χ2 = 8.243, df = 4; p = 0.043, VC = 0.289 |
| 6. | Eating of vegetables | 0.00 | 0.00 | 12.33 | 41.67 | 46.00 | 7.66 | 0.66 | 17.00 | 36.02 | 38.66 | χ2 = 10.042, df = 4; p = 0.039, VC = 0.319 |
| 7. | Eating of fruit | 0.00 | 0.00 | 13.66 | 37.34 | 49.00 | 2.00 | 1.00 | 16.67 | 35.33 | 45.00 | χ2 = 8.997, df = 4; p = 0.041, VC = 0.302 |
| 8. | Eating of white bread | 0.67 | 1.00 | 12.67 | 60.33 | 25.33 | 2.33 | 1.33 | 6.33 | 64.68 | 25.33 | χ2 = 9.535, df − 4; p = 0.038, VC = 0.160 |
| 9. | Eating of wholemeal bread | 5.67 | 7.00 | 42.00 | 28.33 | 17.00 | 10.67 | 14.33 | 42.67 | 23.33 | 9.00 | χ2 = 31.026, df − 4; p = 0.025, VC = 0.175 |
| 10. | Eating of coarse groats, wholemeal pasta, flakes, etc. | 3.67 | 6.67 | 54.33 | 27.00 | 8.33 | 8.67 | 9.67 | 54.33 | 20.66 | 6.67 | χ2 = 11.737, df − 4; p = 0.028, VC = 0.132 |
| 11. | Eating of fine groats, pasta, standard flakes | 2.33 | 7.67 | 58.00 | 23.67 | 8.33 | 2.33 | 5.33 | 49.34 | 32.00 | 11.00 | χ2 = 9.255, df − 2; p = 0.035, VC = 0.306 |
| 12. | Eating of eggs | 6.33 | 9.67 | 55.00 | 23.67 | 5.33 | 6.33 | 5.00 | 56.33 | 23.67 | 8.67 | χ2 = 1.667 df = 4; p = 0.794, VC = 0.130 |
| 13. | Eating of processed meat products | 3.67 | 8.00 | 28.33 | 23.33 | 36.67 | 6.00 | 4.67 | 29.33 | 28.00 | 32.00 | χ2 = 16.402, df = 4; p = 0.002, VC = 0.408 |
| 14. | Eating of poultry meat | 0.00 | 6.67 | 29.33 | 20.00 | 44.00 | 1.66 | 9.67 | 32.67 | 14.00 | 42.00 | χ2 = 12.570, df = 4; p = 0.036, VC = 0.126 |
| 15. | Eating of red meat | 3.00 | 12.00 | 30.00 | 16.33 | 38.67 | 6.67 | 15.33 | 25.33 | 12.33 | 40.34 | χ2 = 4.279, df − 4; p = 0.014 VC = 0.208 |
| 16. | Eating of fish | 11.67 | 30.33 | 53.33 | 3.67 | 1.00 | 25.33 | 26.34 | 46.00 | 2.33 | 0.00 | χ2 = 11.951, df − 4; p = 0.020, VC = 0.245 |
| 17. | Eating of fast foods | 0.00 | 0.00 | 19.33 | 68.67 | 12.00 | 0.67 | 1.67 | 28.33 | 63.00 | 6.33 | χ2 = 1.512, df = 4; p = 0.824, VC = 0.123 |
| 18. | Drinking beverages | 6.33 | 17.00 | 17.00 | 4.67 | 55.00 | 11.67 | 15.33 | 10.00 | 6.33 | 56.67 | χ2 = 13.547, df − 4; p= 0.047, VC = 0.189 |
| Mean | 4.30 | 8.63 | 26.53 | 30.22 | 30.32 | 7.55 | 8.97 | 26.41 | 28.90 | 28.17 | χ2 = 10.952, df = 4; p = 0.016 VC = 0.098 | |
| No. | Questions | SC | GC | Statistical Measures * | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Ranks | ||||||||||||
| 1 | 2 | 3 | 4 | 5 | 1 | 2 | 3 | 4 | 5 | |||
| 1. | Number of meals per day | 0.00 | 0.00 | 21.00 | 38.00 | 41.00 | 0.00 | 0.00 | 17.00 | 46.00 | 37.00 | χ2 = 1.338, df = 4; p = 0.846 VC = 0.116 |
| 2. | Eating of breakfast | 2.00 | 5.00 | 6.00 | 18.00 | 69.00 | 3.00 | 5.00 | 7.00 | 14.00 | 71.00 | χ2 = 1.805, df = 4; p = 0.937 VC = 0.182 |
| 3. | Eating of lunch at school | 5.00 | 9.00 | 9.00 | 28.00 | 49.00 | 5.00 | 13.00 | 9.00 | 24.00 | 49.00 | χ2 = 5.571, df = 4; p = 0.233 VC = 0.192 |
| 4. | Type of snacks eaten during the day | 19.00 | 29.00 | 3.00 | 43.00 | 6.00 | 23.00 | 32.00 | 0.00 | 41.00 | 4.00 | χ2 = 3.679, df = 4; p = 0.409 VC = 0.193 |
| 5. | Eating of milk and dairy products | 4.00 | 13.00 | 20.00 | 32.00 | 31.00 | 4.00 | 0.00 | 26.00 | 39.00 | 31.00 | χ2 = 14.472, df = 4; p = 0.005 VC = 0.383 |
| 6. | Eating of vegetables | 0.00 | 0.00 | 9.00 | 51.00 | 40.00 | 6.00 | 0.00 | 24.00 | 39.00 | 31.00 | χ2 = 15.559, df = 4; p = 0.003 VC = 0.397 |
| 7. | Eating of fruit | 0.00 | 0.00 | 17.00 | 40.00 | 43.00 | 0.00 | 1.00 | 18.00 | 39.00 | 42.00 | χ2 = 1.053, df = 4; p = 0.901 VC = 0.103 |
| 8. | Eating of white bread | 0.00 | 0.00 | 12.00 | 71.00 | 17.00 | 0.00 | 0.00 | 3.00 | 71.00 | 26.00 | χ2 = 7.283, df = 4; p = 0.121 VC = 0.271 |
| 9. | Eating of wholemeal bread | 8.00 | 9.00 | 49.00 | 21.00 | 13.00 | 19.00 | 21.00 | 43.00 | 10.00 | 7.00 | χ2 = 15.376, df = 4; p = 0.004 VC = 0.395 |
| 10. | Eating of coarse groats, wholemeal pasta, flakes, etc. | 2.00 | 6.00 | 61.00 | 27.00 | 4.00 | 8.00 | 10.00 | 57.00 | 18.00 | 7.00 | χ2 = 7.353, df= 4; p = 0.118 VC = 0.273 |
| 11. | Eating of fine groats, pasta, standard flakes | 3.00 | 7.00 | 57.00 | 22.00 | 11.00 | 1.00 | 2.00 | 46.00 | 37.00 | 14.00 | χ2 = 9.126, df = 4; p = 0.058 VC = 0.304 |
| 12. | Eating of eggs | 6.00 | 11.00 | 61.00 | 22.00 | 0.00 | 0.00 | 2.00 | 66.00 | 30.00 | 2.00 | χ2 = 15.658, df = 4; p = 0.003 VC = 0.398 |
| 13. | Eating of processed meat products | 0.00 | 16.00 | 34.00 | 16.00 | 34.00 | 0.00 | 12.00 | 30.00 | 28.00 | 30.00 | χ2 = 4.344, df = 4; p = 0.361 VC = 0.210 |
| 14. | Eating of poultry meat | 0.00 | 12.00 | 31.00 | 15.00 | 42.00 | 0.00 | 14.00 | 33.00 | 11.00 | 42.00 | χ2 = 1.740 df = 4; p = 0.783 VC = 0.132 |
| 15. | Eating of red meat | 5.00 | 16.00 | 24.00 | 15.00 | 40.00 | 5.00 | 16.00 | 23.00 | 14.00 | 42.00 | χ2 = 2.016, df = 4; p = 0.732 VC = 0.143 |
| 16. | Eating of fish | 9.00 | 18.00 | 64.00 | 6.00 | 3.00 | 26.00 | 18.00 | 53.00 | 3.00 | 0.00 | χ2 = 13.291, df = 4; p = 0.009 VC = 0.367 |
| 17. | Eating of fast foods | 0.00 | 0.00 | 22.00 | 68.00 | 10.00 | 0.00 | 0.00 | 26.00 | 70.00 | 4.00 | χ2 = 2.933, df = 4; p = 0.569 VC = 0.172 |
| 18. | Drinking beverages | 9.00 | 18.00 | 14.00 | 5.00 | 54.00 | 16.00 | 23.00 | 10.00 | 7.00 | 44.00 | χ2 = 4.590, df = 4; p = 0.331 VC = 0.215 |
| Mean | 4.00 | 9.39 | 28.55 | 29.89 | 28.17 | 6.44 | 9.39 | 27.28 | 30.06 | 26.83 | χ2 = 0.871, df = 4; p = 0.927 VC = 0.194 | |
| No. | Questions | SC | GC | Statistical Measures * | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Ranks | ||||||||||||
| 1 | 2 | 3 | 4 | 5 | 1 | 2 | 3 | 4 | 5 | |||
| 1. | Number of meals per day | 0.00 | 0.00 | 12.00 | 53.00 | 35.00 | 0.00 | 0.00 | 18.00 | 53.00 | 29.00 | χ2 = 11.762, df = 4; p = 0.009 VC = 0.133 |
| 2. | Eating of breakfast | 8.00 | 10.00 | 8.00 | 12.00 | 62.00 | 13.00 | 6.00 | 11.00 | 10.00 | 60.00 | χ2 = 5.874, df = 4; p = 0.048 VC = 0.021 |
| 3. | Eating of lunch at school | 4.00 | 15.00 | 7.00 | 22.00 | 5200 | 7.00 | 17.00 | 6.00 | 21.00 | 49.00 | χ2 = 1.132, df = 4; p = 0.029 VC = 0.182 |
| 4. | Type of snacks eaten during the day | 21.00 | 19.00 | 5.00 | 42.00 | 13.00 | 23.00 | 24.00 | 6.00 | 37.00 | 10.00 | χ2 = 1.471, df = 4; p = 0.831 VC = 0.122 |
| 5. | Eating of milk and dairy products | 0.00 | 3.00 | 12.00 | 40.00 | 45.00 | 4.00 | 0.00 | 13.00 | 43.00 | 40.00 | χ2 = 7.442, df = 4; p = 0.114 VC = 0.274 |
| 6. | Eating of vegetables | 0.00 | 0.00 | 11.00 | 42.00 | 47.00 | 4.00 | 0.00 | 11.00 | 41.00 | 44.00 | χ2 = 10.110, df = 4; p = 0.031 VC = 0.024 |
| 7. | Eating of fruit | 0.00 | 0.00 | 6.00 | 37.00 | 57.00 | 1.00 | 0.00 | 12.00 | 36.00 | 51.00 | χ2 = 3.347, df = 4; p = 0.501 VC = 0.184 |
| 8. | Eating of white bread | 0.00 | 0.00 | 12.00 | 56.00 | 32.00 | 2.00 | 2.00 | 6.00 | 64.00 | 26.00 | χ2 = 17.154, df = 4; p = 0.028 VC = 0.269 |
| 9. | Eating of wholemeal bread | 5.00 | 6.00 | 42.00 | 27.00 | 20.00 | 7.00 | 9.00 | 49.00 | 24.00 | 11.00 | χ 2 = 4.261, df = 4; p = 0.371 VC = 0.207 |
| 10. | Eating of coarse groats, wholemeal pasta, flakes, etc. | 2.00 | 4.00 | 55.00 | 29.00 | 10.00 | 4.00 | 7.00 | 59.00 | 26.00 | 4.00 | χ2 = 4.360, df = 4; p = 0.359 VC = 0.210 |
| 11. | Eating of fine groats, pasta, standard flakes | 2.00 | 4.00 | 57.00 | 27.00 | 10.00 | 1.00 | 4.00 | 45.00 | 38.00 | 12.00 | χ2 = 3.788, df = 4; p = 0.453 VC = 0.195 |
| 12. | Eating of eggs | 0.00 | 0.00 | 59.00 | 26.00 | 15.00 | 0.00 | 0.00 | 61.00 | 20.00 | 19.00 | χ2 = 1.286, df = 4; p = 0.863 VC = 0.114 |
| 13. | Eating of processed meat products | 0.00 | 0.00 | 30.00 | 26.00 | 44.00 | 0.00 | 0.00 | 34.00 | 30.00 | 36.00 | χ2 = 1.335, df = 4; p = 0.855 VC = 0.116 |
| 14. | Eating of poultry meat | 0.00 | 2.00 | 29.00 | 25.00 | 44.00 | 0.00 | 5.00 | 35.00 | 17.00 | 43.00 | χ2 = 13.585, df = 4; p = 0.035 VC = 0.190 |
| 15. | Eating of red meat | 0.00 | 11.00 | 34.00 | 16.00 | 39.00 | 7.00 | 15.00 | 25.00 | 13.00 | 40.00 | χ2 = 6.896, df = 4; p = 0.141 VC = 0.264 |
| 16. | Eating of fish | 17.00 | 38.00 | 45.00 | 0.00 | 0.00 | 21.00 | 33.00 | 46.00 | 0.00 | 0.00 | χ2 = 0.784, df = 4; p = 0.940 VC = 0.007 |
| 17. | Eating of fast foods | 0.00 | 0.00 | 20.00 | 66.00 | 14.00 | 0.00 | 0.00 | 27.00 | 66.00 | 7.00 | χ2 = 3.375 df = 4; p = 0.490 VC = 0.185 |
| 18. | Drinking beverages | 6.00 | 24.00 | 16.00 | 6.00 | 48.00 | 10.00 | 16.00 | 9.00 | 10.00 | 55.00 | χ2 = 9.035, df = 4; p = 0.006 VC = 0.247 |
| Mean | 3.60 | 7.56 | 25.56 | 30.67 | 32.61 | 5.78 | 7.67 | 26.27 | 30.50 | 29.78 | χ2 = 10.468, df = 4; p = 0.023 VC = 0.068 | |
| No. | Questions | SC | GC | Statistical Measures * | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Ranks | ||||||||||||
| 1 | 2 | 3 | 4 | 5 | 1 | 2 | 3 | 4 | 5 | |||
| 1. | Number of meals per day | 0.00 | 0.00 | 10.00 | 65.00 | 25.00 | 0.00 | 0.00 | 21.00 | 53.00 | 26.00 | χ2 = 9.143, df = 4; p = 0.020 VC = 0.228 |
| 2. | Eating of breakfast | 10.00 | 8.00 | 13.00 | 10.00 | 59.00 | 10.00 | 7.00 | 10.00 | 11.00 | 62.00 | χ2 = 13.215, df = 4; p = 0.010 VC= 0.386 |
| 3. | Eating of lunch at school | 3.00 | 16.00 | 4.00 | 22.00 | 55.00 | 8.00 | 18.00 | 5.00 | 19.00 | 50.00 | χ2 = 11.425, df = 4; p = 0.042 VC = 0.002 |
| 4. | Type of snacks eaten during the day | 23.00 | 19.00 | 8.00 | 35.00 | 15.00 | 26.00 | 23.00 | 8.00 | 33.00 | 10.00 | χ2 = 1.623, df = 4; p = 0.804 VC = 0.128 |
| 5. | Eating of milk and dairy products | 3.00 | 2.00 | 19.00 | 36.00 | 40.00 | 2.00 | 5.00 | 24.00 | 34.00 | 35.00 | χ2 = 12.457, df = 4; p = 0.052 VC = 0.150 |
| 6. | Eating of vegetables | 0.00 | 0.00 | 17.00 | 32.00 | 51.00 | 13.00 | 2.00 | 16.00 | 29.00 | 41.00 | χ2 = 16.260, df = 4; p = 0.002 VC = 0.406 |
| 7. | Eating of fruit | 0.00 | 0.00 | 18.00 | 35.00 | 47.00 | 5.00 | 2.00 | 20.00 | 31.00 | 42.00 | χ2 = 12.628, df = 4; p = 0.006 VC = 0.278 |
| 8. | Eating of white bread | 2.00 | 3.00 | 14.00 | 54.00 | 27.00 | 5.00 | 2.00 | 10.00 | 59.00 | 24.00 | χ2 = 2.550, df = 4; p = 0.635 VC = 0.160 |
| 9. | Eating of wholemeal bread | 4.00 | 6.00 | 35.00 | 37.00 | 18.00 | 6.00 | 13.00 | 36.00 | 36.00 | 9.00 | χ2 = 9.006, df = 4; p = 0.028 VC = 0.246 |
| 10. | Eating of coarse groats, wholemeal pasta, flakes, etc. | 7.00 | 10.00 | 47.00 | 25.00 | 11.00 | 14.00 | 12.00 | 47.00 | 18.00 | 9.00 | χ2 = 3.854, df = 4; p = 0.426 VC = 0.197 |
| 11. | Eating of fine groats, pasta, standard flakes | 2.00 | 12.00 | 60.00 | 22.00 | 4.00 | 5.00 | 10.00 | 57.00 | 21.00 | 7.00 | χ2 = 2.385, df = 4; p = 0.665 VC = 0.155 |
| 12. | Eating of eggs | 13.00 | 18.00 | 45.00 | 23.00 | 1.00 | 19.00 | 13.00 | 42.00 | 21.00 | 5.00 | χ2 = 4.792, df = 4; p = 0.309 VC = 0.220 |
| 13. | Eating of processed meat products | 11.00 | 8.00 | 21.00 | 28.00 | 32.00 | 18.00 | 2.00 | 24.00 | 26.00 | 30.00 | χ2 = 5.268, df = 4; p = 0.228 VC = 0.231 |
| 14. | Eating of poultry meat | 0.00 | 6.00 | 28.00 | 20.00 | 46.00 | 5.00 | 10.00 | 30.00 | 14.00 | 41.00 | χ2 = 8.303, df = 4; p = 0.021 VC = 0.290 |
| 15. | Eating of red meat | 4.00 | 9.00 | 32.00 | 18.00 | 37.00 | 8.00 | 15.00 | 28.00 | 10.00 | 39.00 | χ2 = 3.136, df = 4; p = 0.535 VC = 0.178 |
| 16. | Eating of fish | 9.00 | 35.00 | 51.00 | 5.00 | 0.00 | 29.00 | 28.00 | 39.00 | 4.00 | 0.00 | χ2 = 13.015, df = 4; p = 0.011 VC = 0.363 |
| 17. | Eating of fast foods | 0.00 | 0.00 | 16.00 | 72.00 | 12.00 | 2.00 | 5.00 | 32.00 | 53.00 | 8.00 | χ2 = 16.021, df = 4; p = 0.003 VC = 0.403 |
| 18. | Drinking beverages | 4.00 | 9.00 | 21.00 | 3.00 | 63.00 | 9.00 | 7.00 | 11.00 | 2.00 | 71.00 | χ2 = 9.975, df = 4; p = 0.038 VC = 0.246 |
| Mean | 5.27 | 8.94 | 25.50 | 30.11 | 30.18 | 10.23 | 9.67 | 25.56 | 26.33 | 28.21 | χ2 = 12.772, df = 4; p = 0.055 VC = 0.134 | |
| Average Age (Years) | SC | GC | Statistical Measures * | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Ranks | |||||||||||
| 1 | 2 | 3 | 4 | 5 | 1 | 2 | 3 | 4 | 5 | ||
| 10.27 | 0.00 | 0.00 | 33.00 | 35.00 | 32.00 | 4.00 | 5.00 | 10.27 | 30.00 | 28.00 | χ2 = 9.651; df = 4; p = 0.040 VC = 0.258 |
| 11.27 | 0.00 | 0.00 | 12.00 | 49.00 | 39.00 | 2.00 | 2.00 | 11.27 | 38.00 | 25.00 | χ2 = 18.253; df = 4; p = 0.011 VC = 0.143 |
| 12.27 | 0.00 | 7.00 | 19.00 | 41.00 | 33.00 | 8.00 | 5.00 | 12.27 | 30.00 | 22.00 | χ2 = 16.978; df = 4; p = 0.002 VC = 0.138 |
| Mean | 0.00 | 2.33 | 21.33 | 41.67 | 34.67 | 4.66 | 4.00 | 33.67 | 32.67 | 25.00 | χ2 = 2.612; df − 4; p = 0.013; VC = 0.128 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kolanowski, W.; Ługowska, K.; Trafialek, J. The Impact of Physical Activity at School on Eating Behaviour and Leisure Time of Early Adolescents. Int. J. Environ. Res. Public Health 2022, 19, 16490. https://doi.org/10.3390/ijerph192416490
Kolanowski W, Ługowska K, Trafialek J. The Impact of Physical Activity at School on Eating Behaviour and Leisure Time of Early Adolescents. International Journal of Environmental Research and Public Health. 2022; 19(24):16490. https://doi.org/10.3390/ijerph192416490
Chicago/Turabian StyleKolanowski, Wojciech, Katarzyna Ługowska, and Joanna Trafialek. 2022. "The Impact of Physical Activity at School on Eating Behaviour and Leisure Time of Early Adolescents" International Journal of Environmental Research and Public Health 19, no. 24: 16490. https://doi.org/10.3390/ijerph192416490
APA StyleKolanowski, W., Ługowska, K., & Trafialek, J. (2022). The Impact of Physical Activity at School on Eating Behaviour and Leisure Time of Early Adolescents. International Journal of Environmental Research and Public Health, 19(24), 16490. https://doi.org/10.3390/ijerph192416490








