Integrative Wellness Approaches to Mitigate Perceived Stress, Increase Vitality, and Build Community during COVID-19: A Pilot Study
Abstract
1. Introduction
Background
2. Materials and Methods
2.1. Pilot Study Methods
2.2. Setting and Sample
2.3. Procedures
2.4. Data Collection
2.5. Subjective Vitality Scale (SVS)
2.6. Perceived Stress Scale (PSS)
2.7. Data Analysis
3. Results
3.1. Sociodemographics
3.2. Quantitative Results
3.3. Qualitative Results
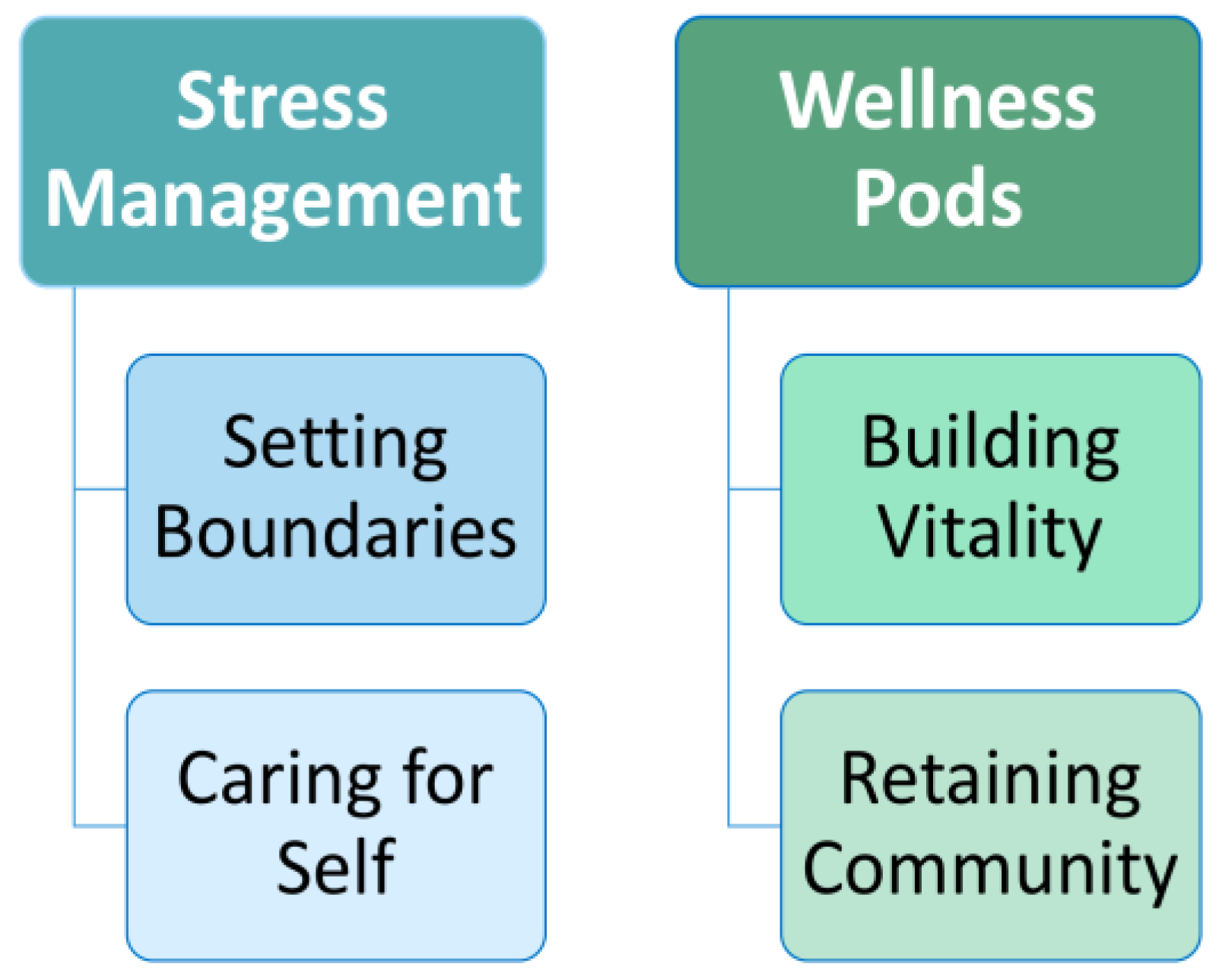
3.4. Stress Management
3.5. Wellness Pods
4. Discussion
4.1. Factors Related to Perceived Stress
4.2. Previous Wellness Interventions to Build Community and Enhance Well-Being
4.3. Moving Forward with Theoretical Considerations
4.4. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Cho, E.-J.; Cho, H.H. Factors Influencing Compassion Fatigue among Hospice and Palliative Care Unit Nurses. Korean J. Hosp. Palliat. Care 2021, 24, 13–25. [Google Scholar] [CrossRef]
- Martin-Cuellar, A.; Lardier, D.T.; Atencio, D.J.; Kelly, R.J.; Montañez, M. Vitality as a Moderator of Clinician History of Trauma and Compassion Fatigue. Contemp. Fam. Ther. 2019, 41, 408–419. [Google Scholar] [CrossRef]
- Figley, C.R. Compassion Fatigue: Coping with Secondary Traumatic Stress Disorder in Those Who Treat the Traumatized; Routledge: London, UK, 2013. [Google Scholar]
- Joinson, C. Coping with Compassion Fatigue. Nursing 1992, 22, 116–121. [Google Scholar] [CrossRef] [PubMed]
- Dall’Ora, C.; Ball, J.; Reinius, M.; Griffiths, P. Burnout in Nursing: A Theoretical Review. Hum. Resour. Health 2020, 18, 41. [Google Scholar] [CrossRef] [PubMed]
- Maslach, C.; Leiter, M.P. Understanding and Preventing Teacher Burnout: A Sourcebook of International Research and Practice; Cambridge University Press: Cambridge, UK, 1999. [Google Scholar]
- Boyle, D. Countering Compassion Fatigue: A Requisite Nursing Agenda. Online J. Issues Nurs. 2011, 16, 2. [Google Scholar] [CrossRef]
- Mudallal, R.H.; Saleh, M.Y.N.; Al-Modallal, H.M.; Abdel-Rahman, R.Y. Quality of Nursing Care: The Influence of Work Conditions, Nurse Characteristics and Burnout. Int. J. Afr. Nurs. Sci. 2017, 7, 24–30. [Google Scholar] [CrossRef]
- Lazarus, R.S.; Folkman, S. Stress, Appraisal, and Coping; Springer: New York, NY, USA, 1984; ISBN 978-0-8261-4191-0. [Google Scholar]
- Abdul-Raheem, J. Cultural humility in nursing education. J. Cult. Divers. 2018, 25, 66–73. [Google Scholar]
- Akintola, O.; Hlengwa, W.M.; Dageid, W. Perceived Stress and Burnout among Volunteer Caregivers Working in AIDS Care in South Africa. J. Adv. Nurs. 2013, 69, 2738–2749. [Google Scholar] [CrossRef]
- Wingard, J. Higher Ed Must Change or Die 2022. Available online: https://www.insidehighered.com/views/2022/08/16/higher-ed-must-change-or-die-opinion (accessed on 2 September 2022).
- Spurlock, D. The Nursing Shortage and the Future of Nursing Education Is in Our Hands. J. Nurs. Educ. 2020, 59, 303–304. [Google Scholar] [CrossRef]
- Denehy, J. The Future of Nursing: Responding to the Nursing Shortage. J. Sch. Nurs. 2000, 16, 7–8. [Google Scholar] [CrossRef]
- Fischer, K. The Shrinking of Higher Ed in the Past, Colleges Grew Their Way out of Enrollment Crises. This Time Looks Different. Disappearing Stud. 2022. Available online: https://www.chronicle.com/article/the-shrinking-of-higher-ed (accessed on 2 September 2022).
- American Association of Colleges and Nursing Updates on the AACN Essentials. Available online: https://www.aacnnursing.org/Essentials/Latest-Updates (accessed on 2 September 2022).
- Bittner, N.P.; Bechtel, C.F. Identifying and Describing Nurse Faculty Workload Issues: A Looming Faculty Shortage. Nurs. Educ. Perspect. 2017, 38, 171–176. [Google Scholar] [CrossRef] [PubMed]
- Khan, A. Sources and Adverse Effects of Burnout among Academic Staff: A Systematic Review. City Univ. Res. J. 2019, 9, 350–362. [Google Scholar]
- Andrew Weil Center for Integrative Medicine. Integrative Health and Lifestyle Program (IHeLp); Online Education; The University of Arizona: Tucson, AZ, USA, 2015. [Google Scholar]
- Microsoft Microsoft Excel. Available online: https://www.microsoft.com/en-us/microsoft-365/excel (accessed on 15 July 2021).
- QualtricsXM. Available online: https://www.qualtrics.com (accessed on 15 July 2021).
- Ryan, R.M.; Frederick, C. On Energy, Personality, and Health: Subjective Vitality as a Dynamic Reflection of Well-Being. J. Pers. 1997, 65, 529–565. [Google Scholar] [CrossRef] [PubMed]
- Cohen, S.; Kamarck, T.; Mermelstein, R. A Global Measure of Perceived Stress. J. Health Soc. Behav. 1983, 24, 385. [Google Scholar] [CrossRef]
- Rubio, D.M. A Validation Of The Subjective Vitality Scale Using Structural Equation Modeling. Soc. Indic. Res. 2000, 52, 313–324. [Google Scholar] [CrossRef]
- Ryan, R.M.; Deci, E.L. Self-Determination Theory; Guilford Publishing: New York, NY, USA, 2017. [Google Scholar]
- Lee, E.-H. Review of the Psychometric Evidence of the Perceived Stress Scale. Asian Nurs. Res. 2012, 6, 121–127. [Google Scholar] [CrossRef]
- Elo, S.; Kyngäs, H. The Qualitative Content Analysis Process. J. Adv. Nurs. 2008, 62, 107–115. [Google Scholar] [CrossRef]
- Lincoln, Y.S.; Guba, E.G. Naturalistic Inquiry; Sage: New York, NY, USA, 1985. [Google Scholar]
- Singh, C.; Jackson, D.; Munro, I.; Cross, W. Job Experiences, Challenges, Revelations and Narratives of Nurse Academics. A Qualitative Study. J. Adv. Nurs. 2022, 78, 2622–2633. [Google Scholar] [CrossRef]
- Amaya, M.; Donegan, T.; Conner, D.; Edwards, J.; Gipson, C. Creating a Culture of Wellness: A Call to Action for Higher Education, Igniting Change in Academic Institutions. Build. Healthy Acad. Communities J. 2019, 3, 27. [Google Scholar] [CrossRef]
- Woods-Giscombe, C.L. An Innovative Program to Promote Health Promotion, Quality of Life, and Wellness for School of Nursing Faculty, Staff, and Students: Facilitators, Barriers, and Opportunities for Broad System-Level and Cultural Change. Arch. Psychiatr. Nurs. 2021, 35, 185–188. [Google Scholar] [CrossRef] [PubMed]
- Melnyk, B.M.; Hsieh, A.P.; Tan, A.; Gawlik, K.S.; Hacker, E.D.; Ferrell, D.; Simpson, V.; Burda, C.; Hagerty, B.; Scott, L.D.; et al. The State of Mental Health and Healthy Lifestyle Behaviors in Nursing, Medicine and Health Sciences Faculty and Students at Big 10 Universities with Implications for Action. J. Prof. Nurs. 2021, 37, 1167–1174. [Google Scholar] [CrossRef] [PubMed]
- Ketelaar, S.M.; Gärtner, F.R.; Bolier, L.; Smeets, O.; Nieuwenhuijsen, K.; Sluiter, J.K. Mental Vitality @ Work—A Workers’ Health Surveillance Mental Module for Nurses and Allied Health Care Professionals: Process Evaluation of a Randomized Controlled Trial. J. Occup. Environ. Med. 2013, 55, 563–571. [Google Scholar] [CrossRef] [PubMed]
- Mealer, M.; Conrad, D.; Evans, J.; Jooste, K.; Solyntjes, J.; Rothbaum, B.; Moss, M. Feasibility and Acceptability of a Resilience Training Program for Intensive Care Unit Nurses. Am. J. Crit. Care 2014, 23, e97–e105. [Google Scholar] [CrossRef]
- Querstret, D.; Cropley, M.; Fife-Schaw, C. Internet-Based Instructor-Led Mindfulness for Work-Related Rumination, Fatigue, and Sleep: Assessing Facets of Mindfulness as Mechanisms of Change. A Randomized Waitlist Control Trial. J. Occup. Health Psychol. 2017, 22, 153–169. [Google Scholar] [CrossRef]
- Sampson, M.; Melnyk, B.M.; Hoying, J. The MINDBODYSTRONG Intervention for New Nurse Residents: 6-Month Effects on Mental Health Outcomes, Healthy Lifestyle Behaviors, and Job Satisfaction. Worldviews Evid. Based Nurs. 2020, 17, 16–23. [Google Scholar] [CrossRef]
- Sampson, M.; Melnyk, B.M.; Hoying, J. Intervention Effects of the MINDBODYSTRONG Cognitive Behavioral Skills Building Program on Newly Licensed Registered Nurses’ Mental Health, Healthy Lifestyle Behaviors, and Job Satisfaction. J. Nurs. Adm. 2019, 49, 487–495. [Google Scholar] [CrossRef]
- Sood, A.; Prasad, K.; Schroeder, D.; Varkey, P. Stress Management and Resilience Training Among Department of Medicine Faculty: A Pilot Randomized Clinical Trial. J. Gen. Intern. Med. 2011, 26, 858–861. [Google Scholar] [CrossRef]
- Sood, A.; Sharma, V.; Schroeder, D.R.; Gorman, B. Stress Management and Resiliency Training (SMART) Program among Department of Radiology Faculty: A Pilot Randomized Clinical Trial. EXPLORE 2014, 10, 358–363. [Google Scholar] [CrossRef]
- Cheng, S.-T.; Tsui, P.K.; Lam, J.H.M. Improving Mental Health in Health Care Practitioners: Randomized Controlled Trial of a Gratitude Intervention. J. Consult. Clin. Psychol. 2015, 83, 177–186. [Google Scholar] [CrossRef]
- Snyder, C.R. TARGET ARTICLE: Hope Theory: Rainbows in the Mind. Psychol. Inq. 2002, 13, 249–275. [Google Scholar] [CrossRef]
- Vermeesch, A.L.; Garrigues, L.; Rothacker-Peyton, S. Chapter 18: Rewilding Wellness: An Integrated Perspective. In Buttaro Primary Care; Elsevier: Amsterdam, The Netherlands, 2021; in press. [Google Scholar]
| Category | Number of Participants N (%) | |
|---|---|---|
| Gender Identity | Male | 2 (11%) |
| Female | 17 (89%) | |
| Non-Binary | 0 (0%) | |
| Total | 19 (100%) | |
| Age (years) | 20–25 | 0 (0%) |
| 25–30 | 0 (0%) | |
| 30–35 | 2 (11) | |
| 35–40 | 4 (21%) | |
| 40–45 | 3 (16%) | |
| 45–50 | 3 (16%) | |
| 50–55 | 5 (26%) | |
| 55–60 | 1 (5%) | |
| 60–65 | 1 (5%) | |
| 65+ | 0 (0) | |
| Total | 19 (100%) | |
| Academic Appointment | Instructor | 10 (53%) |
| Tenure Track | 7 (37%) | |
| Senior Lecturer | 1 (5%) | |
| Staff | 1 (5%) | |
| Other | 0 (0%) | |
| Total | 19 (100%) | |
| Years of Experience | Less than One Year | 3 (15.7%) |
| 1–2 Years | 3 (15.7%) | |
| 3–5 Years | 3 (15.7%) | |
| 6–9 Years | 3 (15.7%) | |
| 10 + Years | 4 (21.5%) | |
| Missing | 3 (15.7%) | |
| Total | 19 (100%) | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vermeesch, A.L.; Garrigues, L.; Littzen-Brown, C. Integrative Wellness Approaches to Mitigate Perceived Stress, Increase Vitality, and Build Community during COVID-19: A Pilot Study. Int. J. Environ. Res. Public Health 2022, 19, 16463. https://doi.org/10.3390/ijerph192416463
Vermeesch AL, Garrigues L, Littzen-Brown C. Integrative Wellness Approaches to Mitigate Perceived Stress, Increase Vitality, and Build Community during COVID-19: A Pilot Study. International Journal of Environmental Research and Public Health. 2022; 19(24):16463. https://doi.org/10.3390/ijerph192416463
Chicago/Turabian StyleVermeesch, Amber L., Layla Garrigues, and Chloé Littzen-Brown. 2022. "Integrative Wellness Approaches to Mitigate Perceived Stress, Increase Vitality, and Build Community during COVID-19: A Pilot Study" International Journal of Environmental Research and Public Health 19, no. 24: 16463. https://doi.org/10.3390/ijerph192416463
APA StyleVermeesch, A. L., Garrigues, L., & Littzen-Brown, C. (2022). Integrative Wellness Approaches to Mitigate Perceived Stress, Increase Vitality, and Build Community during COVID-19: A Pilot Study. International Journal of Environmental Research and Public Health, 19(24), 16463. https://doi.org/10.3390/ijerph192416463









