Effects of the COVID-19 Pandemic on Health Behaviors of Higher Education Students in Ghana: A Cross-Sectional Study
Abstract
1. Introduction
2. Materials and Methods
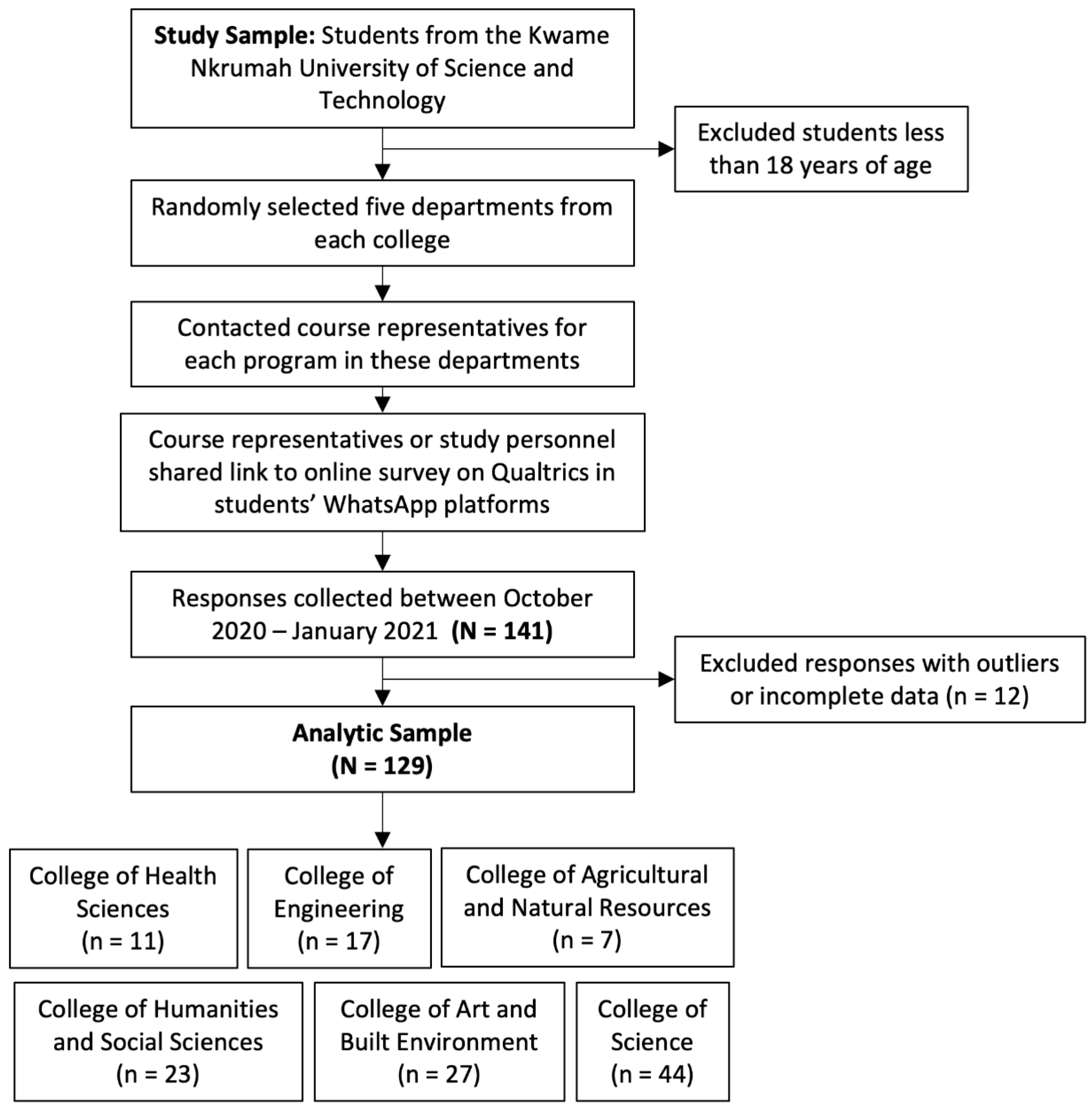
2.1. Study Design
2.2. Demographics
2.3. Evaluation of Quality and Duration of Sleep
2.4. Evaluation of Dietary Risk and Misuse of Alcohol
2.5. Evaluation of Physical Activity and Sitting Time
2.6. Assessment of Financial Stress
2.7. Evaluation of the Impact of the COVID-19 Pandemic on Health Behaviors
2.8. Statistical Analysis
3. Results
3.1. Demographic and Anthropometric Parameters
3.2. Gender Comparisons of Health Behaviors during the COVID-19 Pandemic
3.3. Gender Comparisons of COVID-19 Pandemic-Influenced Health Behaviors
3.4. Association between Quality and Duration of Sleep Changes and Health Behaviors
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Du, C.; Zan, M.C.; Cho, M.J.; Fenton, J.I.; Hsiao, P.Y.; Hsiao, R.; Keaver, L.; Lai, C.-C.; Lee, H.; Ludy, M.-J.; et al. The effects of sleep quality and resilience on perceived stress, dietary behaviors, and alcohol misuse: A mediation-moderation analysis of higher education students from Asia, Europe, and North America during the COVID-19 pandemic. Nutrients 2021, 13, 442. [Google Scholar] [CrossRef] [PubMed]
- Kocevska, D.; Blanken, T.F.; Van Someren, E.J.W.; Rösler, L. Sleep quality during the COVID-19 pandemic: Not one size fits all. Sleep Med. 2020, 76, 86–88. [Google Scholar] [CrossRef] [PubMed]
- Du, C.; Zan, M.C.H.; Cho, M.J.; Fenton, J.I.; Hsiao, P.Y.; Hsiao, R.; Keaver, L.; Lai, C.-C.; Lee, H.; Ludy, M.-J.; et al. Health behaviors of higher education students from 7 countries: Poorer sleep quality during the COVID-19 pandemic predicts higher dietary risk. Clocks Sleep 2021, 3, 12–30. [Google Scholar] [CrossRef] [PubMed]
- Ruiz, M.C.; Devonport, T.J.; Chen-Wilson, C.-H.; Nicholls, W.; Cagas, J.Y.; Fernandez-Montalvo, J.; Choi, Y.; Robazza, C. A cross-cultural exploratory study of health behaviors and wellbeing during COVID-19. Front. Psychol. 2021, 11, 608216. [Google Scholar] [CrossRef] [PubMed]
- Knell, G.; Robertson, M.C.; Dooley, E.E.; Burford, K.; Mendez, K.S. Health behavior changes during COVID-19 pandemic and subsequent “stay-at-home” orders. Int. J. Environ. Res. Public Health 2020, 17, 6268. [Google Scholar] [CrossRef]
- Huang, Y.; Zhao, N. Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 outbreak in China: A web-based cross-sectional survey. J. Psychiatr. Res. 2020, 288, 112954. [Google Scholar] [CrossRef]
- Yuan, R.K.; Zitting, K.M.; Maskati, L.; Huang, J. Increased sleep duration and delayed sleep timing during the COVID-19 pandemic. Sci. Rep. 2022, 12, 10937. [Google Scholar] [CrossRef]
- Çıtak, Ş.; Pekdemir, Ü. An analysis on sleep habits and generalized anxiety levels of individuals during the COVİD-19 pandemic. J. Fam. Couns. Educ. 2020, 4, 60–73. [Google Scholar] [CrossRef]
- Simon, C. Insomnia in a Pandemic. Available online: https://news.harvard.edu/gazette/story/2020/04/sleep-problems-becoming-risk-factor-as-pandemic-continues/ (accessed on 30 December 2021).
- Karman, M. Sleep Habits Post Lockdown in the USA. 2020. Available online: https://eachnight.com/sleep/sleep-habits-post-quarantine/ (accessed on 30 December 2021).
- Keng, S.L.; Stanton, M.V.; Haskins, L.B.; Almenara, C.A.; Ickovics, J.; Jones, A.; Grigsby-Toussaint, D.; Agostini, M.; Bélanger, J.J.; Gützkow, B.; et al. COVID-19 stressors and health behaviors: A multilevel longitudinal study across 86 countries. Prev. Med. Rep. 2022, 27, 101764. [Google Scholar] [CrossRef]
- Williams, A.B.; Dzierzewski, J.M.; Griffin, S.C.; Lind, M.J.; Dick, D.; Rybarczyk, B.D. Insomnia disorder and behaviorally induced insufficient sleep syndrome: Prevalence and relationship to depression in college students. Behav. Sleep Med. 2020, 18, 275–286. [Google Scholar] [CrossRef]
- Shankar, A.; Syamala, S.; Kalidindi, S. Insufficient rest or sleep and its relation to cardiovascular disease, diabetes and obesity in a national, multiethnic sample. PLoS ONE 2010, 5, e14189. [Google Scholar] [CrossRef] [PubMed]
- Galambos, N.L.; Howard, A.L.; Maggs, J.L. Rise and fall of sleep quantity and quality with student experiences across the first year of university. J. Adolesc. Res. 2011, 21, 342–349. [Google Scholar] [CrossRef]
- Ghrouz, A.K.; Noohu, M.M.; Dilshad Manzar, M.; Warren Spence, D.; BaHammam, A.S.; Pandi-Perumal, S.R. Physical activity and sleep quality in relation to mental health among college students. Sleep Breath. 2019, 23, 627–634. [Google Scholar] [CrossRef]
- Jansen, E.C.; Prather, A.; Leung, C.W. Associations between sleep duration and dietary quality: Results from a nationally-representative survey of US adults. Appetite 2020, 153, 104748. [Google Scholar] [CrossRef] [PubMed]
- Arora, T.; Grey, I. Health behaviour changes during COVID-19 and the potential consequences: A mini-review. J. Health Psychol. 2020, 25, 1155–1163. [Google Scholar] [CrossRef]
- Liu, C.; Xie, B.; Chou, C.-P.; Koprowski, C.; Zhou, D.; Palmer, P.; Sun, P.; Guo, Q.; Duan, L.; Sun, X.; et al. Perceived stress, depression and food consumption frequency in the college students of China seven cities. Physiol. Behav. 2007, 92, 748–754. [Google Scholar] [CrossRef]
- Evans, T.M.; Bira, L.; Gastelum, J.B.; Weiss, L.T.; Vanderford, N.L. Evidence for a mental health crisis in graduate education. Nat. Biotechnol. 2018, 36, 282–284. [Google Scholar] [CrossRef]
- Murphy, M.H.; Carlin, A.; Woods, C.; Nevill, A.; MacDonncha, C.; Ferguson, K.; Murphy, N. Active students are healthier and happier than their inactive peers: The results of a large representative cross-sectional study of university students in Ireland. J. Phys. Act. Health 2018, 15, 737–746. [Google Scholar] [CrossRef]
- Marelli, S.; Castelnuovo, A.; Somma, A.; Castronovo, V.; Mombelli, S.; Bottoni, D.; Leitner, C.; Fossati, A.; Ferini-Strambi, L. Impact of COVID-19 lockdown on sleep quality in university students and administration staff. J. Neurol. 2021, 268, 8–15. [Google Scholar] [CrossRef]
- Ellakany, P.; Zuñiga, R.A.A.; El Tantawi, M.; Brown, B.; Aly, N.M.; Ezechi, O.; Uzochukwu, B.; Abeldaño, G.F.; Ara, E.; Ayanore, M.A.; et al. Impact of the COVID-19 pandemic on student’ sleep patterns, sexual activity, screen use, and food intake: A global survey. PLoS ONE 2022, 17, e0262617. [Google Scholar] [CrossRef]
- Davy, J.P.; Scheuermaier, K.; Roden, L.C.; Christie, C.J.; Bentley, A.; Gomez-Olive, F.X.; Iacovides, S.; Lewis, R.; Lipinska, G.; Roche, J.; et al. The COVID-19 lockdown and changes in routine-oriented lifestyle behaviors and symptoms of depression, anxiety, and insomnia in South Africa. J. Phys. Act. Health 2021, 18, 1046–1057. [Google Scholar] [CrossRef] [PubMed]
- Williams, P.; Holmbeck, G.; Greenley, R. Adolescent health psychology. J. Consult. Clin. Psychol. 2002, 70, 828–842. [Google Scholar] [CrossRef] [PubMed]
- Buysse Daniel, J.; Hall Martica, L.; Strollo Patrick, J.; Kamarck Thomas, W.; Owens, J.; Lee, L.; Reis Steven, E.; Matthews Karen, A. Relationships between the Pittsburgh Sleep Quality Index (PSQI), Epworth Sleepiness Scale (ESS), and clinical/polysomnographic measures in a community sample. J. Clin. Sleep Med. 2008, 4, 563–571. [Google Scholar] [CrossRef] [PubMed]
- Guo, S.; Sun, W.; Liu, C.; Wu, S. Structural validity of the Pittsburgh Sleep Quality Index in Chinese undergraduate students. Front. Psychol. 2016, 7, 1126. [Google Scholar] [CrossRef] [PubMed]
- Beaudreau, S.A.; Spira, A.P.; Stewart, A.; Kezirian, E.J.; Lui, L.-Y.; Ensrud, K.; Redline, S.; Ancoli-Israel, S.; Stone, K.L. Validation of the Pittsburgh Sleep Quality Index and the Epworth Sleepiness Scale in older Black and White women. Sleep Med. 2012, 13, 36–42. [Google Scholar] [CrossRef]
- Gomes, A.; Marques, D.; Tavares, J.; Azevedo, M. Brief Insomnia and Quality of Sleep Scale (BIQSS): Reliability and validity in higher education students. Sleep Med. 2013, 14, e139–e140. [Google Scholar] [CrossRef]
- Paxton, A.E.; Strycker, L.A.; Toobert, D.J.; Ammerman, A.S.; Glasgow, R.E. Starting the conversation: Performance of a brief dietary assessment and intervention tool for health professionals. Am. J. Prev. Med. 2011, 40, 67–71. [Google Scholar] [CrossRef]
- Bush, K.; Kivlahan, D.R.; McDonell, M.B.; Fihn, S.D.; Bradley, K.A. The AUDIT alcohol consumption questions (AUDIT-C): An effective brief screening test for problem drinking. Arch. Intern. Med. 1998, 158, 1789–1795. [Google Scholar] [CrossRef]
- National Institutes of Health National Institute on Alcohol Abuse and Alcoholism (NIAAA). Available online: https://www.nih.gov/about-nih/what-we-do/nih-almanac/national-institute-alcohol-abuse-alcoholism-niaaa (accessed on 30 December 2021).
- Frank, D.; DeBenedetti, A.; Volk, R.; Williams, E.; Kivlahan, D.; Bradley, K. Effectiveness of the AUDIT-C as a screening test for alcohol misuse in three race/ethnic groups. J. Gen. Intern. Med. 2008, 23, 781–787. [Google Scholar] [CrossRef]
- Craig, C.L.; Marshall, A.L.; Sjöström, M.; Bauman, A.E.; Booth, M.L.; Ainsworth, B.E.; Pratt, M.; Ekelund, U.; Yngve, A.; Sallis, J.F.; et al. International physical activity questionnaire: 12-country reliability and validity. Med. Sci. Sports Exerc. 2003, 35, 1381–1395. [Google Scholar] [CrossRef]
- Lim, H.; Heckman, S.J.; Letkiewicz, J.C.; Montalto, C.P. Financial stress, self-efficacy, and financial help-seeking behavior of college students. J. Financ. Couns. Plan. 2014, 25, 148–160. [Google Scholar]
- Buysse, D.J.; Reynolds, C.F.; Monk, T.H.; Berman, S.R.; Kupfer, D.J. The Pittsburgh Sleep Quality Index: A new instrument for psychiatric practice and research. J. Psychiatr. Res. 1989, 28, 193–213. [Google Scholar] [CrossRef] [PubMed]
- Lawson, H.J.; Wellens-Mensah, J.T.; Attah Nantogma, S. Evaluation of sleep patterns and self-reported academic performance among medical students at the university of Ghana school of medicine and dentistry. Sleep Disord. 2019, 2019, 1278579. [Google Scholar] [CrossRef] [PubMed]
- Yeboah, K.; Dodam, K.K.; Agyekum, J.A.; Oblitey, J.N. Association between poor quality of sleep and metabolic syndrome in Ghanaian university students: A cross-sectional study. Sleep Disord. 2022, 2022, 8802757. [Google Scholar] [CrossRef] [PubMed]
- Lankono, C.B. Coronavirus and Food Security: The Plight of Consumers; CUTS International: Accra, Ghana, 2020. [Google Scholar]
- Asante, L.A.; Mills, R.O. Exploring the socio-economic impact of COVID-19 pandemic in marketplaces in urban Ghana. Afr. Spectr. 2020, 55, 170–181. [Google Scholar] [CrossRef]
- Bukari, C.; Aning-Agyei, M.A.; Kyeremeh, C.; Essilfie, G.; Amuquandoh, K.F.; Owusu, A.A.; Otoo, I.C.; Bukari, K.I. Effect of COVID-19 on household food insecurity and poverty: Evidence from Ghana. Soc. Indic. Res. 2022, 159, 991–1015. [Google Scholar] [CrossRef]
- Kanyiri Gaa, P.; Sulley, S.; Boahen, S.; Bogobiri, S.; Mogre, V. Reported dietary habits and lifestyle behaviors of students before and during COVID-19 lockdown: A cross-sectional survey among university students from Ghana. J. Public Health Res. 2022, 11, 22799036221129417. [Google Scholar] [CrossRef]
- Darmon, N.; Lacroix, A.; Muller, L.; Ruffieux, B. Food price policies improve diet quality while increasing socioeconomic inequalities in nutrition. Int. J. Behav. Nutr. Phys. Act. 2014, 11, 66. [Google Scholar] [CrossRef]
- Darmon, N.; Drewnowski, A. Contribution of food prices and diet cost to socioeconomic disparities in diet quality and health: A systematic review and analysis. Nutr. Rev. 2015, 73, 643–660. [Google Scholar] [CrossRef]
- Carpio, C.E.; Kalenkoski, C.M.; Moyeda-Carabaza, A.F.; Murimi, M. The effect of time use and food cost on dietary quality. Public Health Nutr. 2020, 23, 3284–3294. [Google Scholar] [CrossRef]
- Erol, A.; Karpyak, V.M. Sex and gender-related differences in alcohol use and its consequences: Contemporary knowledge and future research considerations. Drug Alcohol Depend. 2015, 156, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Schulte, M.T.; Ramo, D.; Brown, S.A. Gender differences in factors influencing alcohol use and drinking progression among adolescents. Clin. Psychol. Rev. 2009, 29, 535–547. [Google Scholar] [CrossRef] [PubMed]
- Martín-Rodríguez, A.; Tornero-Aguilera, J.F.; López-Pérez, P.J.; Clemente-Suárez, V.J. Gender differences in nutritional, odontological and psychological patterns of adolescent students during COVID-19 pandemic. Appl. Sci. 2021, 11, 8499. [Google Scholar] [CrossRef]
- Baber, I.E. The Relationship between Loneliness, Stress, and Alcohol Consumption among College Students. Master’s Thesis, Abilene Christian University, Abilene, TX, USA, 2018. [Google Scholar]
- Edward, W.A.; Jacob, O.S.; Daniel, A. Physical activity and dietary behaviors: A phenomenological analysis of experiences of Ghanaians during the COVID-19 lockdown. Pan. Afr. Med. J. 2020, 37, 199. [Google Scholar]
- Pandya, A.; Lodha, P. Social connectedness, excessive screen time during COVID-19 and mental health: A review of current evidence. Front. Hum. Dyn. 2021, 3, 684137. [Google Scholar] [CrossRef]
- Agyemang, K.; Banstola, A.; Pokhrel, S.; Anokye, N. Determinants of physical activity and dietary habits among adults in Ghana: A cross-sectional study. Int. J. Environ. Res. Public Health 2022, 19, 4671. [Google Scholar] [CrossRef]
- Lofti, M.; Al-Hosseini, M.K.; Jafarirad, S. The relationship of sleep quality with eating behavior and food intake among male university students. J. Sleep Med. 2015, 2, 1034. [Google Scholar]
- Zuraikat, F.M.; Makarem, N.; Liao, M.; St-Onge, M.P.; Aggarwal, B. Measures of poor sleep quality are associated with higher energy intake and poor diet quality in a diverse sample of women from the Go Red for Women strategically focused research network. J. Am. Heart Assoc. 2020, 9, e014587. [Google Scholar] [CrossRef]
- Jiang, X.; Chen, Y.; Wang, J. Global food security under COVID-19: Comparison and enlightenment of policy responses in different countries. Foods 2021, 10, 2850. [Google Scholar] [CrossRef]
- Davoren, M.P.; Shiely, F.; Byrne, M.; Perry, I.J. Hazardous alcohol consumption among university students in Ireland: A cross-sectional study. BMJ Open 2015, 5, e006045. [Google Scholar] [CrossRef]
- Mekonen, T.; Fekadu, W.; Chane, T.; Bitew, S. Problematic alcohol use among university students. Front. Psychiatry 2017, 8, 86. [Google Scholar] [CrossRef] [PubMed]
- Ji, C.-Y.; Hu, P.-J.; Song, Y. The epidemiology of alcohol consumption and misuse among Chinese college students. Alcohol Alcohol. 2012, 47, 464–472. [Google Scholar] [CrossRef] [PubMed]
- Babor, T.F.; Steinberg, K.; Anton, R.; Del Boca, F. Talk is cheap: Measuring drinking outcomes in clinical trials. J. Stud. Alcohol 2000, 61, 55–63. [Google Scholar] [CrossRef] [PubMed]
- Galambos, N.L.; Dalton, A.L.; Maggs, J.L. Losing sleep over it: Daily variation in sleep quantity and quality in canadian students’ first semester of university. J. Adolesc. Res. 2009, 19, 741–761. [Google Scholar] [CrossRef]
- Lund, H.G.; Reider, B.D.; Whiting, A.B.; Prichard, J.R. Sleep patterns and predictors of disturbed sleep in a large population of college students. J. Adolesc. Health 2010, 46, 124–132. [Google Scholar] [CrossRef] [PubMed]
- Stein, M.D.; Friedmann, P.D. Disturbed sleep and its relationship to alcohol use. Subst. Abuse 2006, 26, 1–13. [Google Scholar] [CrossRef]
- Dzierzewski, J.M.; Buman, M.P.; Giacobbi, P.R., Jr.; Roberts, B.L.; Aiken-Morgan, A.T.; Marsiske, M.; McCrae, C.S. Exercise and sleep in community-dwelling older adults: Evidence for a reciprocal relationship. J. Sleep Res. 2014, 23, 61–68. [Google Scholar] [CrossRef]
- Kline, C.E. The bidirectional relationship between exercise and sleep: Implications for exercise adherence and sleep improvement. Am. J. Lifestyle Med. 2014, 8, 375–379. [Google Scholar] [CrossRef]
- Lin, P.-H.; Lin, C.-Y.; Wang, P.-Y.; Yang, S.-Y. Association between sleeping duration and health-related behaviors in college student. J. Health Soc. Behav. 2018, 1, 31–36. [Google Scholar]
- Sherrill, D.L.; Kotchou, K.; Quan, S.F. Association of physical activity and human sleep disorders. Arch. Intern. Med. 1998, 158, 1894–1898. [Google Scholar] [CrossRef]
- Dolezal, B.A.; Neufeld, E.V.; Boland, D.M.; Martin, J.L.; Cooper, C.B. Interrelationship between sleep and exercise: A systematic review. Adv. Prev. Med. 2017, 2017, 1364387. [Google Scholar] [PubMed]
| Parameters | Males | Females | p-Value | t/z-Value | df |
|---|---|---|---|---|---|
| n (%) | 72 (55.8) | 57 (44.2) | 0.060 | 1.868 | 1 |
| Age (years) (mean ± SD) | 21.1 ± 1.7 | 20.9 ± 1.7 | 0.501 | 0.674 | 124 |
| BMI (kg/m2) (mean ± SD) | 19.0 ± 4.2 | 19.7 ± 4.6 | 0.375 | −0.891 | 106 |
| College | % of Students (n = 129) |
|---|---|
| College of Science (CoS) | 34.1 (44) |
| College of Art and Built Environment (CABES) | 20.9 (27) |
| College of Engineering (CoE) | 17.8 (23) |
| College of Humanities and Social Sciences (CoHSS) | 13.2 (17) |
| College of Health Sciences (CoH) | 8.5 (11) |
| College of Agriculture and Natural Resources (CANR) | 5.4 (7) |
| Males | Females | Overall | p-Value | t/z/χ2-Value | df | |
|---|---|---|---|---|---|---|
| PSQI scores (mean ± SD) | 5.72 ± 2.67 | 6.14 ± 3.58 | 5.91 ± 3.10 | 0.448 | −0.761 | 126 |
| Average sleep (h/d) (mean ± SD) | 6.72 ± 1.32 | 6.75 ± 1.40 | 6.73 ± 1.35 | 0.899 | −0.128 | 123 |
| Weekday sleep (h/d) (mean ± SD) | 6.57 ± 1.34 | 6.68 ± 1.38 | 6.62 ± 1.35 | 0.642 | −0.465 | 123 |
| Weekend sleep (h/d) (mean ± SD) | 7.16 ± 1.70 | 6.82 ± 1.89 | 7.01 ± 1.780 | 0.289 | 1.071 | 125 |
| Poor sleep quality (%) | 48.61 | 49.12 | 48.84 | 0.982 | 0 | 1 |
| Short sleep duration (%) | 48.61 | 56.14 | 51.94 | 0.465 | 0.532 | 1 |
| Financial stress (mean ± SD) | 16.33 ± 4.68 | 14.63 ± 4.98 | 15.58 ± 4.87 | 0.048 | 1.993 | 127 |
| Dietary risk (mean ± SD) | 6.24 ± 2.46 | 6.89 ± 2.72 | 6.47 ± 2.61 | 0.153 | −1.439 | 127 |
| Alcohol misuse score (mean ± SD) | 0.33 ± 0.65 | 0.28 ± 0.65 | 0.31 ± 0.65 | 0.653 | 1.417 | 127 |
| Classified as alcohol misuser (%) | 4.20 | 1.80 | 0.75 | 0.432 | 0.785 | 1 |
| METs (min/wk) | 4022.49 ± 4351.39 | 3392.79 ± 4597.26 | 3727.14 ± 4459.45 | 0.456 | 0.748 | 111 |
| Sitting time (min/d) | 266.82 ± 138.85 | 290.5 ± 196.08 | 277.27 ± 166.23 | 0.427 | −0.796 | 125 |
| Health Behavior | Direction of Change | Males (%) | Females (%) | Overall | p-Value | z-Value |
|---|---|---|---|---|---|---|
| Diet | Less healthy | 19.44 | 21.05 | 20.16 | 0.821 | −0.226 |
| Alcohol consumption | Drinking more | 4.17 | 1.75 | 3.10 | 0.432 | 0.785 |
| Sleep quality | Worse | 16.67 | 24.56 | 20.16 | 0.267 | −1.110 |
| Sleep duration | Less | 22.22 | 22.81 | 20.48 | 0.937 | −0.079 |
| Exercise frequency | Exercising less | 43.06 | 40.35 | 41.86 | 0.757 | 0.309 |
| Exercise intensity | Less intense | 38.89 | 36.84 | 37.98 | 0.812 | 0.238 |
| Groups | n (%) | PSQI (Mean ± SD) | Average Duration of Sleep (Mean ± SD) |
|---|---|---|---|
| Change in quality of sleep | |||
| Worse | 26 (20.16) | 8.12 ± 3.18 a | 6.40 ± 1.20 a |
| Better | 57 (44.19) | 5.11 ± 2.65 b,c | 7.03 ± 1.31 a |
| Did not change | 46 (35.66) | 5.63 ± 3.03 c | 6.55 ± 1.43 a |
| Change in duration of sleep | |||
| Less | 29 (22.48) | 8.48 ± 2.9 a | 5.95 ± 1.40 a |
| More | 70 (54.26) | 4.96 ± 2.64 b,c | 7.25 ± 1.17 a |
| Did not change | 30 (23.26) | 5.60 ± 2.91 c | 6.31 ± 1.22 a |
| Predictors | Dietary Risk B (p-Value) | Alcohol Misuse Scores B (p-Value) | Physical Activity (METs/wk) B (p-Value) | Sitting Time (min/d) B (p-Value) |
|---|---|---|---|---|
| R-square | 0.06 | 0.06 | 0.04 | 0.03 |
| Constant | 10.45 (0.001) | 0.52 (0.504) | 4103.41 (0.45) | 470.94 (0.021) |
| Change in quality of sleep | ||||
| Worse | 0.76 (0.327) | −0.17 (0.396) | −740.59 (0.589) | 28.20 (0.578) |
| Better | 0.94 (0.116) | 0.11 (0.498) | 1159.87 (0.281) | −4.14 (0.916) |
| Did not change (reference) | - | - | - | - |
| Change in duration of sleep | ||||
| Less | −0.85 (0.303) | 0.50 (0.021) | 672.25 (0.659) | −74.16 (0.173) |
| More | −0.98 (0.142) | 0.14 (0.431) | 598.23 (0.625) | −14.61 (0.738) |
| Did not change (reference) | - | - | - | - |
| Gender | ||||
| Male | - | - | - | - |
| Female | 0.83 (0.077) | −0.15 (0.363) | −316.19 (0.713) | 18.64 (0.549) |
| Age | −0.19 (0.159) | 0.02 (0.668) | −54.02 (0.831) | −8.69 (0.347) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Amoako, M.; Amoah-Agyei, F.; Mensah, G.O.; Du, C.; Sergin, S.; Fenton, J.I.; Tucker, R.M. Effects of the COVID-19 Pandemic on Health Behaviors of Higher Education Students in Ghana: A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2022, 19, 16442. https://doi.org/10.3390/ijerph192416442
Amoako M, Amoah-Agyei F, Mensah GO, Du C, Sergin S, Fenton JI, Tucker RM. Effects of the COVID-19 Pandemic on Health Behaviors of Higher Education Students in Ghana: A Cross-Sectional Study. International Journal of Environmental Research and Public Health. 2022; 19(24):16442. https://doi.org/10.3390/ijerph192416442
Chicago/Turabian StyleAmoako, Mary, Felicity Amoah-Agyei, Gideon Okyere Mensah, Chen Du, Selin Sergin, Jenifer I. Fenton, and Robin M. Tucker. 2022. "Effects of the COVID-19 Pandemic on Health Behaviors of Higher Education Students in Ghana: A Cross-Sectional Study" International Journal of Environmental Research and Public Health 19, no. 24: 16442. https://doi.org/10.3390/ijerph192416442
APA StyleAmoako, M., Amoah-Agyei, F., Mensah, G. O., Du, C., Sergin, S., Fenton, J. I., & Tucker, R. M. (2022). Effects of the COVID-19 Pandemic on Health Behaviors of Higher Education Students in Ghana: A Cross-Sectional Study. International Journal of Environmental Research and Public Health, 19(24), 16442. https://doi.org/10.3390/ijerph192416442






