Paediatric Cutaneous Warts and Verrucae: An Update
Abstract
1. Introduction
Prevalence and Risk Factors for Warts
2. HPV Type and Carriage of Infection
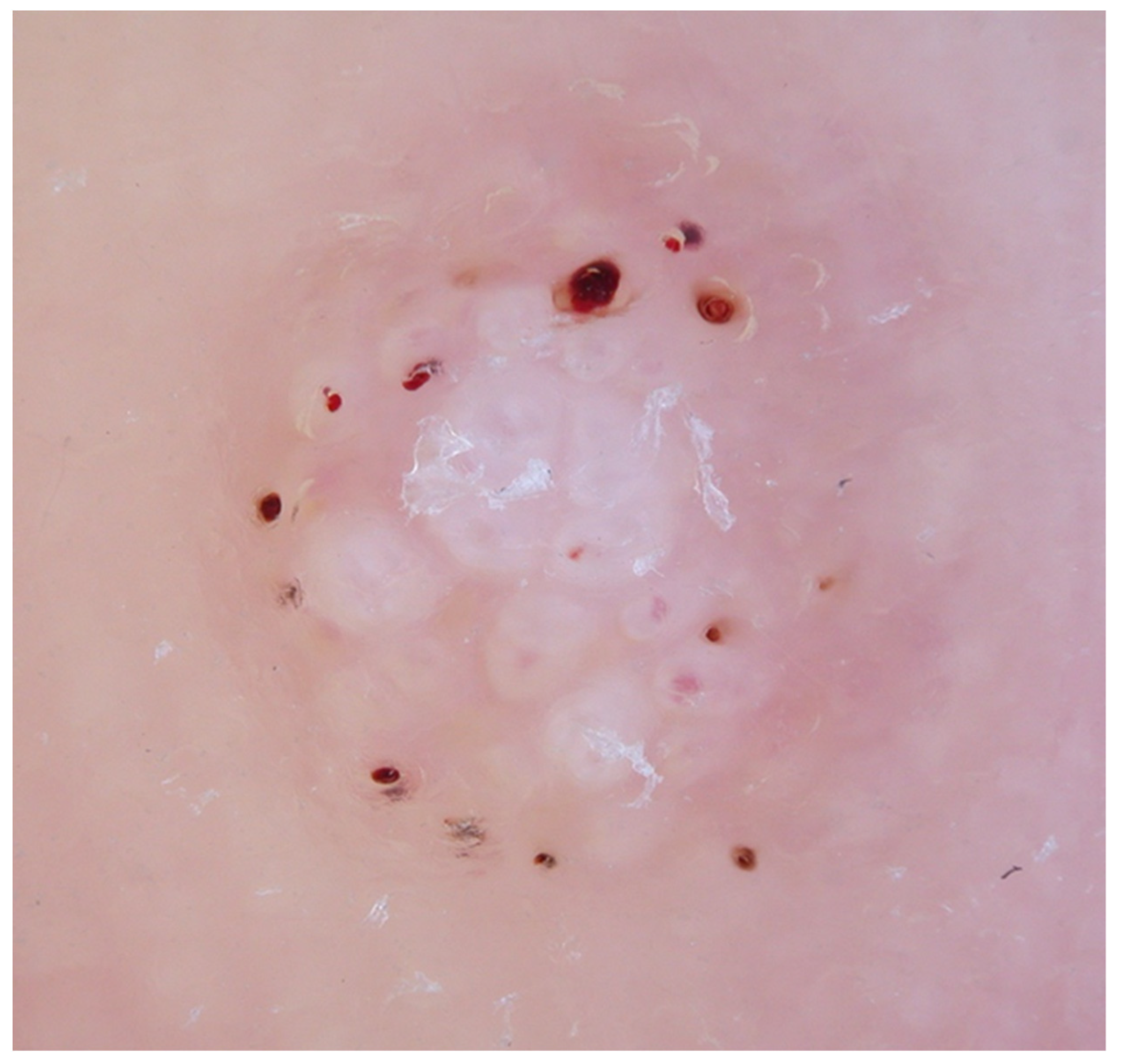
3. Diagnosis
4. Natural Wart Regression
5. Treatment of Warts in Children
6. Treatment of Plantar Warts (Verrucae)
7. Emerging Treatments
8. Summary
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kilkenny, M.; Merlin, K.; Young, R.; Marks, R. The prevalence of common skin conditions in Australian school students: 1. Common, plane and plantar viral warts. Br. J. Dermatol. 1998, 138, 840–845. [Google Scholar] [CrossRef] [PubMed]
- van Haalen, F.M.; Bruggink, S.C.; Gussekloo, J.; Assendelft, W.J.J.; Eekhof, J.A.H. Warts in primary schoolchildren: Prevalence and relation with environmental factors. Br. J. Dermatol. 2009, 161, 148–152. [Google Scholar] [CrossRef] [PubMed]
- Essa, N.; Saleh, M.A.; Mostafa, R.M.; Taha, E.A.; Ismail, T.A. Prevalence and factors associated with warts in primary school children in Tema District, Sohag Governorate, Egypt. J. Egypt. Public Health Assoc. 2019, 94, 6. [Google Scholar] [CrossRef] [PubMed]
- Bruggink, S.C.; Eekhof, J.A.; Egberts, P.F.; van Blijswijk, S.C.; Assendelft, W.J.; Gussekloo, J. Warts transmitted in families and schools: A prospective cohort. Pediatrics 2013, 131, 928–934. [Google Scholar] [CrossRef] [PubMed]
- Williams, H.C.; Pottier, A.; Strachan, D. The descriptive epidemiology of warts in British school children. J. Br. Podiatr. Med. 1994, 49, 171–176. [Google Scholar]
- Liu, J.; Li, H.; Yang, F.; Ren, Y.; Xia, T.; Zhao, Z.; Cao, X.; Wang, Z.; Yin, M.; Lu, S. Epidemiology and clinical profile of cutaneous warts in Chinese college students: A cross-sectional and follow-up study. Sci. Rep. 2018, 8, 15450. [Google Scholar] [CrossRef]
- Ferrari, J. Verrucae pedis in children with juvenile idiopathic arthritis and other paediatric rheumatic diseases: A cross-sectional study. J. Foot Ankle Res. 2022, 15, 29. [Google Scholar] [CrossRef]
- McBride, A.A. Human papillomaviruses: Diversity, infection and host interactions. Nat. Rev. Microbiol. 2022, 20, 95–108. [Google Scholar] [CrossRef]
- de Koning, M.N.C.; Quint, K.D.; Bruggink, S.C.; Gussekloo, J.; Bouwes Bavinck, J.N.; Feltkamp, M.C.W.; Quint, W.G.V.; Eekhof, J.A.H. High prevalence of cutaneous warts in elementary school children and the ubiquitous presence of wart-associated human papillomavirus on clinically normal skin. Br. J. Dermatol. 2015, 172, 196–201. [Google Scholar] [CrossRef]
- de Koning, M.N.; ter Schegget, J.; Eekhof, J.A.; Kamp, M.; Kleter, B.; Gussekloo, J.; Feltkamp, M.C.; Bouwes Bavinck, J.N.; Purdie, K.J.; Bunker, C.B.; et al. Evaluation of a novel broad-spectrum PCR-multiplex genotyping assay for identification of cutaneous wart-associated human papillomavirus types. J. Clin. Microbiol. 2010, 48, 1706–1711. [Google Scholar] [CrossRef]
- de Planell-Mas, E.; Martínez-Garriga, B.; Zalacain, A.J.; Vinuesa, T.; Viñas, M. Human papillomaviruses genotyping in plantar warts. J. Med. Virol. 2016, 89, 902–907. [Google Scholar] [CrossRef] [PubMed]
- Tomson, N.; Sterling, J.; Ahmed, I.; Hague, J.; Berth-Jones, J. Human papillomavirus typing of warts and response to cryotherapy. J. Eur. Acad. Dermatol. Venereol. 2011, 25, 1108–1111. [Google Scholar] [CrossRef] [PubMed]
- Hogendoorn, G.K.; Bruggink, S.C.; Hermans, K.E.; Kouwenhoven, S.T.P.; Quint, K.D.; Wolterbeek, R.; Eekhof, J.A.H.; de Koning, M.N.C.; Rissmann, R.; Burggraaf, J.; et al. Developing and validating the Cutaneous WARTS (CWARTS) diagnostic tool: A novel clinical assessment and classification system for cutaneous warts. Br. J. Dermatol. 2018, 178, 527–534. [Google Scholar] [CrossRef]
- Hogendoorn, G.K.; Bruggink, S.C.; de Koning, M.N.C.; Eekhof, J.A.H.; Hermans, K.E.; Rissmann, R.; Burggraaf, J.; Wolterbeek, R.; Quint, K.D.; Kouwenhoven, S.T.P.; et al. Morphological characteristics and HPV genotype predict the treatment response in cutaneous warts. Br. J. Dermatol. 2018, 178, 253–260. [Google Scholar] [CrossRef]
- Bae, J.M.; Kang, H.; Kim, H.O.; Park, Y.M. Differential diagnosis of plantar wart from corn, callus and healed wart with the aid of dermoscopy. Br. J. Dermatol. 2009, 160, 220–222. [Google Scholar] [CrossRef]
- Natsis, N.E.; Gordon, S.C.; Kaushik, A.; Seiverling, E.V. A practical review of dermoscopy for pediatric dermatology part II: Vascular tumors, infections, and inflammatory dermatoses. Pediatr. Dermatol. 2020, 37, 798–803. [Google Scholar] [CrossRef]
- Aqil, N.; Nassiri, A.; Baybay, H.; Gallouj, S.; Sara, E.; Mernissi, F.Z. Warts under the dermoscope. SM Dermatol. J. 2019, 5, 1030. [Google Scholar] [CrossRef]
- Bruggink, S.C.; Eekhof, J.A.; Egberts, P.F.; van Blijswijk, S.C.; Assendelft, W.J.; Gussekloo, J. Natural course of cutaneous warts among primary schoolchildren: A prospective cohort study. Ann. Fam. Med. 2013, 11, 437–441. [Google Scholar] [CrossRef]
- Bruggink, S.C.; Gussekloo, J.; de Koning, M.N.C.; Feltkamp, M.C.W.; Bavinck, J.N.B.; Quint, W.G.V.; Assendelft, W.J.J.; Eekhof, J.A.H. HPV type in plantar warts influences natural course and treatment response: Secondary analysis of a randomised controlled trial. J. Clin. Virol. 2013, 57, 227–232. [Google Scholar] [CrossRef]
- García-Oreja, S.; Álvaro-Afonso, F.J.; García-Álvarez, Y.; García-Morales, E.; Sanz-Corbalán, I.; Lázaro Martínez, J.L. Topical treatment for plantar warts: A systematic review. Dermatol. Ther. 2021, 34, e14621. [Google Scholar] [CrossRef]
- Hekmatjah, J.; Farshchian, M.; Grant-Kels, J.M.; Mehregan, D. The status of treatment for plantar warts in 2021: No definitive advancements in decades for a common dermatology disease. Clin. Dermatol. 2021, 39, 688–694. [Google Scholar] [CrossRef] [PubMed]
- García-Oreja, S.; Álvaro-Afonso, F.J.; Tardáguila-García, A.; López-Moral, M.; García-Madrid, M.; Lázaro-Martínez, J.L. Efficacy of cryotherapy for plantar warts: A systematic review and meta-analysis. Dermatol. Ther. 2022, 35, e15480. [Google Scholar] [CrossRef] [PubMed]
- Sterling, J.C.; Gibbs, S.; Haque Hussain, S.S.; Mohd Mustapa, M.F.; Handfield-Jones, S.E. British association of dermatologists’ guidelines for the management of cutaneous warts 2014. Br. J. Dermatol. 2014, 171, 696–712. [Google Scholar] [CrossRef]
- Loo, S.K.; Tang, W.Y. Warts (non-genital). BMJ Clin. Evid. 2014, 2014, 1710. [Google Scholar] [PubMed]
- Silverberg, N.B. Pediatric warts: Update on interventions. Cutis 2019, 103, 26–30. [Google Scholar]
- Soenjoyo, K.R.; Chua, B.W.B.; Wee, L.W.Y.; Koh, M.J.A.; Ang, S.B. Treatment of cutaneous viral warts in children: A review. Dermatol. Ther. 2020, 33, e14034. [Google Scholar] [CrossRef] [PubMed]
- Daniel, B.S.; Murrell, D.F. Complete resolution of chronic multiple verruca vulgaris treated with quadrivalent human papillomavirus vaccine. JAMA Dermatol. 2013, 149, 370–372. [Google Scholar] [CrossRef]
- Kreuter, A.; Waterboer, T.; Wieland, U. Regression of cutaneous warts in a patient with WILD syndrome following recombinant quadrivalent human papillomavirus vaccination. Arch. Dermatol. 2010, 146, 1196–1197. [Google Scholar] [CrossRef]
- Abeck, D.; Fölster-Holst, R. Quadrivalent human papillomavirus vaccination: A promising treatment for recalcitrant cutaneous warts in children. Acta Derm. Venereol. 2015, 95, 1017–1019. [Google Scholar] [CrossRef]
- Dyall-Smith, D.J. Treatment of warts at the turn of the millennium. Australas. J. Dermatol. 2000, 41, S20–S22. [Google Scholar] [CrossRef]
- Hegyi, G.; Szigeti, G.P. Hyperthermia versus Oncothermia: Cellular effects in complementary cancer therapy. Evid. Based Complement. Alternat. Med. 2013, 2013, 12. [Google Scholar] [CrossRef] [PubMed]
- Fausch, S.C.; Fahey, L.M.; Da Silva, D.M.; Kast, W.M. Human papillomavirus can escape immune recognition through Langerhans cell phosphoinositide 3-kinase activation. J. Immunol. 2005, 174, 7172–7178. [Google Scholar] [CrossRef] [PubMed]
- Xie, Z.; Zhang, M.; Xiong, W.; Wan, H.Y.; Zhao, X.C.; Xie, T.; Lei, H.; Lin, Z.C.; Luo, D.S.; Liang, X.L.; et al. Immunotolerant indoleamine-2,3-dioxygenase is increased in condyloma acuminata. Br. J. Dermatol. 2017, 177, 809–817. [Google Scholar] [CrossRef] [PubMed]
- Westrich, J.A.; Warren, C.J.; Pyeon, D. Evasion of host immune defenses by human papillomavirus. Virus Res. 2017, 231, 21–33. [Google Scholar] [CrossRef] [PubMed]
- Li, X.D.; Gao, X.H.; Hong, Y.X.; Liu, Y.B.; Zhu, L.L.; Wang, Y.K.; Wang, X.Q.; Huo, W.; Zhang, L.; Chen, H.D. Effects of local hyperthermia on maturation of Langerhans cells in HPV-infected skin. Zhonghua Shi Yan He Lin Chuang Bing Du Xue Za Zhi (Chin. J. Exp. Clin. Virol.) 2010, 24, 122–124. [Google Scholar]
- Zhu, L.-l.; Gao, X.-H.; Qi, R.; Hong, Y.; Li, X.; Wang, X.; McHepange, U.O.; Zhang, L.; Wei, H.; Chen, H.-D. Local hyperthermia could induce antiviral activity by endogenous interferon-dependent pathway in condyloma acuminata. Antiviral Res. 2010, 88, 187–192. [Google Scholar] [CrossRef]
- Huo, W.; Gao, X.H.; Sun, X.P.; Qi, R.Q.; Hong, Y.; McHepange, U.O.; Li, X.D.; Xiao, B.H.; Lin, J.P.; Jiang, Y.; et al. Local hyperthermia at 44 degrees C for the treatment of plantar warts: A randomized, patient-blinded, placebo-controlled trial. J. Infect. Dis. 2010, 201, 1169–1172. [Google Scholar] [CrossRef]
- Stern, P.; Levine, N. Controlled localized heat therapy in cutaneous warts. Arch. Dermatol. 1992, 128, 945–948. [Google Scholar] [CrossRef]
- Ardern-Jones, M.; Lee, A.; Chean, L.W.; Holbrook, D.; Savelyeva, N.; Thomson, P.; Webb, C.; Polak, M.E.; Bristow, I.R. Induction of antihuman papillomavirus immunity by microwave treatment of skin. Br. J. Dermatol. 2016, 175 (Suppl. 1), 151. [Google Scholar]
- Bristow, I.R.; Lim, W.; Lee, A.; Holbrook, D.; Savelyeva, N.; Thomson, P.; Webb, C.; Polak, M.E.; Ardern-Jones, M.R. Microwave therapy for cutaneous human papilloma virus infection. Eur. J. Dermatol. 2017, 27, 511–518. [Google Scholar] [CrossRef]

Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bristow, I. Paediatric Cutaneous Warts and Verrucae: An Update. Int. J. Environ. Res. Public Health 2022, 19, 16400. https://doi.org/10.3390/ijerph192416400
Bristow I. Paediatric Cutaneous Warts and Verrucae: An Update. International Journal of Environmental Research and Public Health. 2022; 19(24):16400. https://doi.org/10.3390/ijerph192416400
Chicago/Turabian StyleBristow, Ivan. 2022. "Paediatric Cutaneous Warts and Verrucae: An Update" International Journal of Environmental Research and Public Health 19, no. 24: 16400. https://doi.org/10.3390/ijerph192416400
APA StyleBristow, I. (2022). Paediatric Cutaneous Warts and Verrucae: An Update. International Journal of Environmental Research and Public Health, 19(24), 16400. https://doi.org/10.3390/ijerph192416400







