Residential Environment Assessment by Older Adults in Nursing Homes during COVID-19 Outbreak
Abstract
1. Introduction
2. Materials and Methods
2.1. Data Source and Selected Variables
2.2. Statistical Analysis
3. Results
3.1. Overall Residential Assessment Characteristics
3.2. The Assessment of Residential Environment Scale Properties
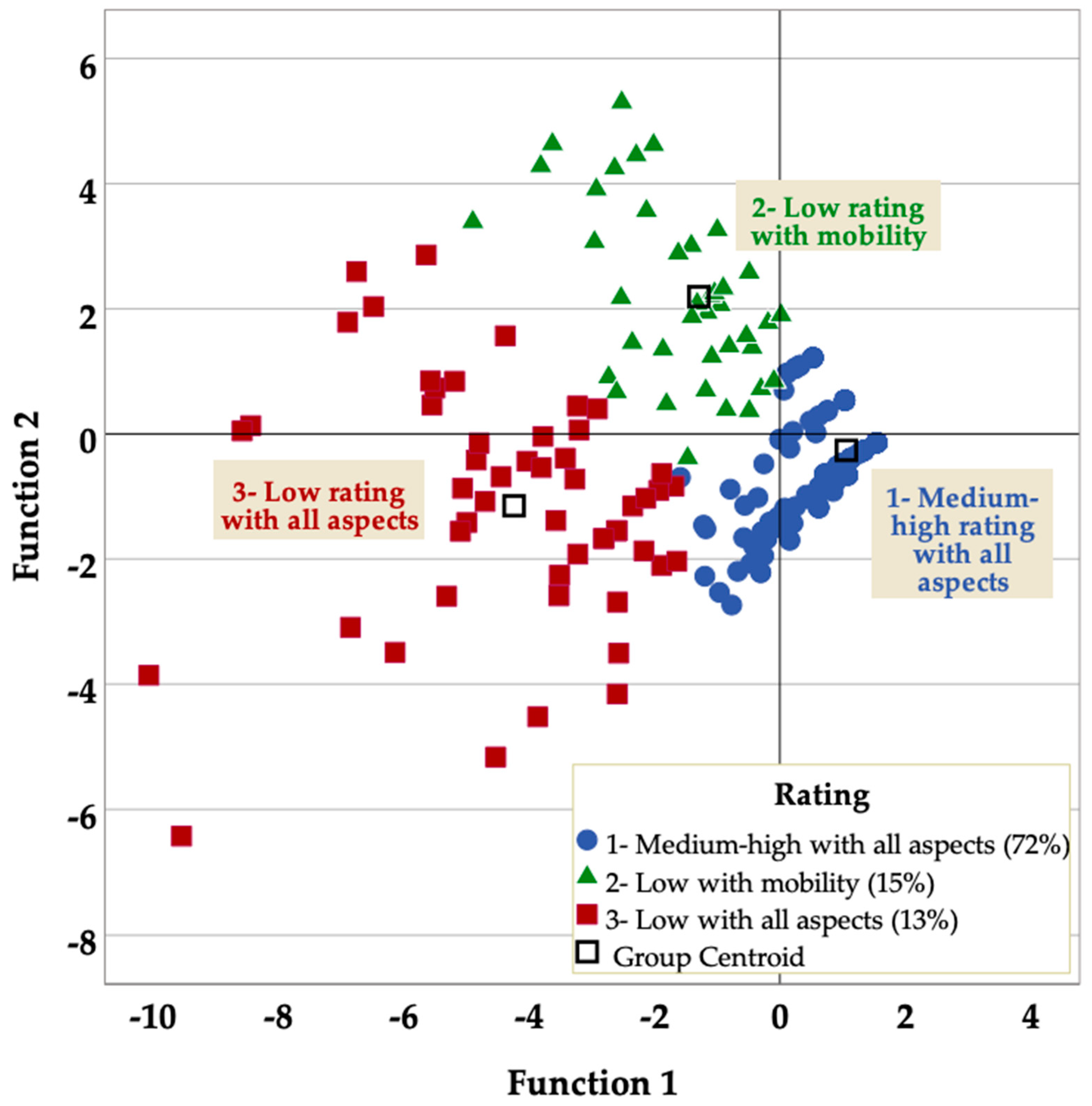
3.3. Grouping of Subjects According to Residential Assessment
3.4. Explaining Membership of Each Residential Value Cluster
3.4.1. Prediction of Medium-High Rating with All Aspects of the Residential Environment
3.4.2. Prediction of Low Rating with Mobility in the Residential Environment
3.4.3. Prediction of Low Rating wih All Aspects of the Residential Environment
4. Discussion
5. Concluding Remarks and Future Research
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- INE—Instituto Nacional de Estadística. Censos de Población y Viviendas 2011. Población Residente en Establecimientos Colectivos; Instituto Nacional de Estadística: Madrid, Spain, 2013. [Google Scholar]
- Pérez Díaz, J.; Ramiro Fariñas, D.; Aceituno Nieto, P.; Muñoz Díaz, C.; Bueno López, C.; Ruiz-Santacruz, J.S.; Fernández Morales, I.; Castillo Belmonte, A.B.; de las Obras-Loscertales Sampériz, J.; Villuendas Hijosa, B. Un perfil de las personas mayores en España 2022. Indicadores Demográficos Básicos; Informes Envejecimiento en Red: Madrid, Spain, 2022; pp. 1–40. [Google Scholar]
- Abellán García, A.; Aceituno Nieto, M.P.; Ramiro Fariñas, D.; Castillo Belmonte, A.B. Estadísticas Sobre Residencias. Distribución de Centros y Plazas Residenciales por Provincia. Datos de Septiembre de 2020; Informes Envejecimiento en Red, nº 27: Madrid, Spain, 2021; p. 24. [Google Scholar]
- Lu, P.; Kong, D.; Shelley, M. Making the Decision to Move to a Nursing Home: Longitudinal Evidence from the Health and Retirement Study. J. Appl. Gerontol. 2020, 40, 1197–1205. [Google Scholar] [CrossRef]
- Green, O.; Ayalon, L. “Home Is Where My Couch Is”: The Role of Possessions in the Process of Moving and Adjusting to Continuing Care Retirement Communities. Qual. Health Res. 2019, 29, 577–588. [Google Scholar] [CrossRef]
- Abrahamson, K.; Hass, Z.; Arling, G. Shall I Stay or Shall I Go? The Choice to Remain in the Nursing Home Among Residents With High Potential for Discharge. J. Appl. Gerontol. 2020, 39, 863–870. [Google Scholar] [CrossRef] [PubMed]
- Fernández-Mayoralas, G.; Rojo-Pérez, F.; Martínez-Martín, P.; Prieto-Flores, M.-E.; Rodríguez-Blázquez, C.; Martín-García, S.; Rojo-Abuín, J.-M.; Forjaz, M.-J. Active ageing and quality of life: Factors associated with participation in leisure activities among institutionalized older adults, with and without dementia. Aging Ment. Health 2015, 19, 1031–1041. [Google Scholar] [CrossRef] [PubMed]
- Luo, M.; Xue, Y.; Zhang, S.; Dong, Y.; Mo, D.; Dong, W.; Qian, K.; Fang, Y.; Liang, H.; Zhang, Z. What Factors Influence Older People’s Intention to Enrol in Nursing Homes? A Cross-Sectional Observational Study in Shanghai, China. BMJ Open 2018, 8, e021741. [Google Scholar] [CrossRef] [PubMed]
- Huang, Z.; Liu, Q.; Meng, H.; Liu, D.; Dobbs, D.; Hyer, K.; Conner, K.O. Factors associated with willingness to enter long-term care facilities among older adults in Chengdu, China. PLoS ONE 2018, 13, e0202225. [Google Scholar] [CrossRef] [PubMed]
- Villeneuve, R.; Meillon, C.; Dartigues, J.-F.; Amieva, H. Trajectory of Quality of Life Before and After Entering a Nursing Home: A Longitudinal Study. J. Geriatr. Psychiatry Neurol. 2022, 35, 102–109. [Google Scholar] [CrossRef]
- Maenhout, A.; Cornelis, E.; Van de Velde, D.; Desmet, V.; Gorus, E.; Van Malderen, L.; Vanbosseghem, R.; De Vriendt, P. The relationship between quality of life in a nursing home and personal, organizational, activity-related factors and social satisfaction: A cross-sectional study with multiple linear regression analyses. Aging Ment. Health 2020, 24, 649–658. [Google Scholar] [CrossRef]
- Rodríguez-Blázquez, C.; Forjaz, M.J.; Prieto-Flores, M.E.; Rojo-Pérez, F.; Fernández-Mayoralas, F.; Martínez-Martín, F.; On Behalf of the Spanish Research Group on Quality of Life and Ageing. Health status and well-being of older adults living in the community and in residential care settings: Are differences influenced by age? Aging Ment. Health 2012, 16, 884–891. [Google Scholar] [CrossRef]
- Rodríguez Rodríguez, V. La edad de la población en la COVID-19: Controversias socio-demográficas sobre un hecho común. Boletín Asoc. Geógrafos Españoles 2021, 91, 1–47. [Google Scholar] [CrossRef]
- Dykgraaf, S.H.; Matenge, S.; Desborough, J.; Sturgiss, E.; Dut, G.; Roberts, L.; McMillan, A.; Kidd, M. Protecting Nursing Homes and Long-Term Care Facilities From COVID-19: A Rapid Review of International Evidence. J. Am. Med. Dir. Assoc. 2021, 22, 1969–1988. [Google Scholar] [CrossRef] [PubMed]
- Cazzoletti, L.; Zanolin, M.; Tocco Tussardi, I.; Alemayohu, M.; Zanetel, E.; Visentin, D.; Fabbri, L.; Giordani, M.; Ruscitti, G.; Benetollo, P.; et al. Risk Factors Associated with Nursing Home COVID-19 Outbreaks: A Retrospective Cohort Study. Int. J. Environ. Res. Public Health 2021, 18, 8434. [Google Scholar] [CrossRef]
- Zunzunegui, M.-V. COVID-19 en centros residenciales de personas mayores: La equidad será necesaria para evitar nuevas catástrofes [COVID-19 in care homes: Equity will be needed to avoid new catastrophes]. Gac. Sanit. 2022, 36, 3–5. [Google Scholar] [CrossRef] [PubMed]
- Palacios-Ceña, D.; Fernández-Peña, R.; Ortega-López, A.; Fernández-Feito, A.; Bautista-Villaécija, O.; Rodrigo-Pedrosa, O.; Arnau-Sánchez, J.; Lizcano-Álvarez, Á. Long-Term Care Facilities and Nursing Homes during the First Wave of the COVID-19 Pandemic: A Scoping Review of the Perspectives of Professionals, Families and Residents. Int. J. Environ. Res. Public Health 2021, 18, 10099. [Google Scholar] [CrossRef]
- Giri, S.; Chenn, L.M.; Romero-Ortuno, R. Nursing homes during the COVID-19 pandemic: A scoping review of challenges and responses. Eur. Geriatr. Med. 2021, 12, 1127–1136. [Google Scholar] [CrossRef] [PubMed]
- Letourneau, J.; Belanger, E.; Sia, D.; Beogo, I.; Robins, S.; Kruglova, K.; Jubinville, M.; Tchouaket, E.N. Identifying performance factors of long-term care facilities in the context of the COVID-19 pandemic: A scoping review protocol. Syst. Rev. 2022, 11, 203. [Google Scholar] [CrossRef]
- Lane, S.J.; Sugg, M.; Spaulding, T.J.; Hege, A.; Iyer, L. Southeastern United States Predictors of COVID-19 in Nursing Homes. J. Appl. Gerontol. 2022, 41, 1641–1650. [Google Scholar] [CrossRef]
- Nguyen, L.K.N.; Howick, S.; McLafferty, D.; Anderson, G.H.; Pravinkumar, S.J.; Van Der Meer, R.; Megiddo, I. Impact of visitation and cohorting policies to shield residents from COVID-19 spread in care homes: An agent-based model. Am. J. Infect. Control. 2021, 49, 1105–1112. [Google Scholar] [CrossRef]
- Konetzka, R.T.; White, E.M.; Pralea, A.; Grabowski, D.C.; Mor, V. A systematic review of long-term care facility characteristics associated with COVID-19 outcomes. J. Am. Geriatr. Soc. 2021, 69, 2766–2777. [Google Scholar] [CrossRef]
- Zunzunegui, M.-V.; Béland, F.; Rico, M.; García López, F.J. Long-Term Care Home Size Association with COVID-19 Infection and Mortality in Catalonia in March and April 2020. Epidemiologia 2022, 3, 369–390. [Google Scholar] [CrossRef]
- Martino, E.; Mansour, A.; Bentley, R. Housing Vulnerability and COVID-19 Outbreaks: When Crises Collide. Urban Policy Res. 2022, 1–17. [Google Scholar] [CrossRef]
- Fitzpatrick, J.M.; Rafferty, A.M.; Hussein, S.; Ezhova, I.; Palmer, S.; Adams, R.; Rees, L.; Brearley, S.; Sims, S.; Harris, R. Protecting older people living in care homes from COVID-19: A protocol for a mixed-methods study to understand the challenges and solutions to implementing social distancing and isolation. BMJ Open 2021, 11, e050706. [Google Scholar] [CrossRef]
- Giebel, C.; Hanna, K.; Cannon, J.; Shenton, J.; Mason, S.; Tetlow, H.; Marlow, P.; Rajagopal, M.; Gabbay, M. Taking the ‘care’ out of care homes: The moral dilemma of institutional long-term care provision during COVID-19. Health Ans Soc. Care Community 2022, 30, e2127–e2136. [Google Scholar] [CrossRef]
- Hartigan, I.; Kelleher, A.; McCarthy, J.; Cornally, N. Visitor restrictions during the COVID-19 pandemic: An ethical case study. Nurs. Ethics 2021, 28, 1111–1123. [Google Scholar] [CrossRef]
- Pinazo-Hernandis, S.; Galvañ Bas, A.; Dosil Diaz, C.; Pinazo-Clapés, C.; Nieto-Vieites, A.; Facal Mayo, D. El peor año de mi vida. Agotamiento emocional y burnout por la COVID-19 en profesionales de residencias. Estudio RESICOVID. Rev. Española Geriatría Gerontol. 2022, 57, 224–229. [Google Scholar] [CrossRef] [PubMed]
- Resnick, B.; Galik, E.; Holmes, S.; McPherson, R. The impact of COVID-19 in an assisted living community. Geriatr. Nurs. 2021, 42, 1151–1155. [Google Scholar] [CrossRef] [PubMed]
- Groom, L.L.; McCarthy, M.M.; Stimpfel, A.W.; Brody, A.A. Telemedicine and Telehealth in Nursing Homes: An Integrative Review. J. Am. Med. Dir. Assoc. 2021, 22, 1784–1801. [Google Scholar] [CrossRef] [PubMed]
- Leontjevas, R.; Knippenberg, I.A.H.; Bakker, C.; Koopmans, R.T.C.M.; Gerritsen, D.L. Telehealth and telecommunication in nursing homes during COVID-19 antiepidemic measures in the Netherlands. Int. Psychogeriatr. 2021, 33, 835–836. [Google Scholar] [CrossRef] [PubMed]
- Deusdad, B. El COVID-19 y la Crisis de las Residencias de Mayores en España: Edadismo y Precariedad. Res. Ageing Soc. Policy 2020, 8, 142–168. [Google Scholar] [CrossRef]
- Kusmaul, N.; Miller, V.J.; Cheon, J.H. Family member roles in long term care: Lessons for the future from COVID-19. J. Aging Stud. 2022, 62, 101060. [Google Scholar] [CrossRef]
- Chu, C.H.; Yee, A.; Stamatopoulos, V. Poor and Lost Connections: Essential Family Caregivers’ Experiences Using Technology with Family Living in Long-Term Care Homes during COVID-19. J. Appl. Gerontol. 2022, 41, 1547–1556. [Google Scholar] [CrossRef] [PubMed]
- Lombo, L.; Singh, J.; Johnson, P.A.; Johnson, J.C.; Mardon, A.A. Perceived Isolation and Health: Does isolation and feeling of loneliness pose a risk for severe SARS-CoV-2 infection? Acad. Lett. 2021, 139, 1–7. [Google Scholar] [CrossRef]
- Ferdous, F. Social Distancing vs. Social Interaction for Older Adults at Long-Term Care Facilities in the Midst of the COVID-19 Pandemic: A Rapid Review and Synthesis of Action Plans. Inquiry 2021, 58, 00469580211044287. [Google Scholar] [CrossRef] [PubMed]
- Tokazhanov, G.; Tleuken, A.; Guney, M.; Turkyilmaz, A.; Karaca, F. How is COVID-19 Experience Transforming Sustainability Requirements of Residential Buildings? A Review. Sustainability 2020, 12, 8732. [Google Scholar] [CrossRef]
- Wang, C.; He, X.; Song, X.; Chen, S.; Luo, D. Dynamic livelihood impacts of COVID-19 on different rural households in mountainous areas of China. PLoS ONE 2022, 17, e0273816. [Google Scholar] [CrossRef]
- Li, Y.; Kapri, K.P. Impact of Economic Factors and Policy Interventions on the COVID-19 Pandemic. Sustainability 2021, 13, 12874. [Google Scholar] [CrossRef]
- Nicola, M.; Alsafi, Z.; Sohrabi, C.; Kerwan, A.; Al-Jabir, A.; Iosifidis, C.; Agha, M.; Agha, R. The socio-economic implications of the coronavirus pandemic (COVID-19): A review. Int. J. Surg. 2020, 78, 185–193. [Google Scholar] [CrossRef]
- Donthu, N.; Gustafsson, A. Effects of COVID-19 on business and research. J. Bus. Res. 2020, 117, 284–289. [Google Scholar] [CrossRef]
- Clemente-Suárez, V.J.; Rodriguez-Besteiro, S.; Cabello-Eras, J.J.; Bustamante-Sanchez, A.; Navarro-Jiménez, E.; Donoso-Gonzalez, M.; Beltrán-Velasco, A.I.; Tornero-Aguilera, J.F. Sustainable Development Goals in the COVID-19 Pandemic: A Narrative Review. Sustainability 2022, 14, 7726. [Google Scholar] [CrossRef]
- Daniel, S.J. Education and the COVID-19 pandemic. PROSPECTS 2020, 49, 91–96. [Google Scholar] [CrossRef]
- Schleicher, A. The Impact of COVID-19 on Education: Insights from “Education at a Glance 2020”; OECD Publishing: Paris, France, 2020; pp. 1–30. [Google Scholar]
- Colomb, C.; Gallent, N. Post-COVID-19 mobilities and the housing crisis in European urban and rural destinations. Policy challenges and research agenda. Plan. Pract. Res. 2022, 37, 532–546. [Google Scholar] [CrossRef]
- Utkarsh; Sigala, M. A bibliometric review of research on COVID-19 and tourism: Reflections for moving forward. Tour. Manag. Perspect. 2021, 40, 100912. [Google Scholar] [CrossRef] [PubMed]
- Fouad, N.A. Editor in Chief’s Introduction to Essays on the Impact of COVID-19 on Work and Workers. J. Vocat. Behav. 2020, 119, 103441. [Google Scholar] [CrossRef] [PubMed]
- Facciola, A.; Lagana, P.; Caruso, G. The COVID-19 pandemic and its implications on the environment. Environ. Res. 2021, 201, 111648. [Google Scholar] [CrossRef]
- González-Val, R.; Sanz-Gracia, F. Urbanization and COVID-19 incidence: A cross-country investigation. Pap. Reg. Sci. 2022, 101, 399–415. [Google Scholar] [CrossRef]
- Anacker, K.B. U.S. suburbs and the lobal COVID-19 pandemic: From cleanscapes to safescapes 2.0? The case of the New York metropolitan area. Urban Geogr. 2021, 43, 1260–1267. [Google Scholar] [CrossRef]
- Frumkin, H. COVID-19, the Built Environment and Health. Environ. Health Perspect. 2021, 129, 075001–075014. [Google Scholar] [CrossRef] [PubMed]
- Rojas-Rueda, D.; Morales-Zamora, E. Built Environment, Transport, and COVID-19: A Review. Curr. Environ. Health Rep. 2021, 8, 138–145. [Google Scholar] [CrossRef] [PubMed]
- Guo, X.; Tu, X.; Huang, G.; Fang, X.; Kong, L.; Wu, J. Urban greenspace helps ameliorate people’s negative sentiments during the COVID-19 pandemic: The case of Beijing. Build. Environ. 2022, 223, 109449. [Google Scholar] [CrossRef] [PubMed]
- Valizadeh, P.; Iranmanesh, A. Inside out, exploring residential spaces during COVID-19 lockdown from the perspective of architecture students. Eur. Plan. Stud. 2022, 30, 211–226. [Google Scholar] [CrossRef]
- McCormack, G.R.; Petersen, J.; Naish, C.; Ghoneim, D.; Doyle-Baker, P.K. Neighbourhood environment facilitators and barriers to outdoor activity during the first wave of the COVID-19 pandemic in Canada: A qualitative study. Cities Health 2022, 1–13. [Google Scholar] [CrossRef]
- Ma, S.; Li, S.; Zhang, J. Diverse and nonlinear influences of built environment factors on COVID-19 spread across townships in China at its initial stage. Sci. Rep. 2021, 11, 12415. [Google Scholar] [CrossRef] [PubMed]
- Xiao, J.; Zhao, J.; Luo, Z.; Liu, F.; Greenwood, D. The impact of built environment on mental health: A COVID-19 lockdown perspective. Health Place 2022, 77, 102889. [Google Scholar] [CrossRef] [PubMed]
- Wood, G.E.R.; Pykett, J.; Stathi, A. Active and healthy ageing in urban environments: Laying the groundwork for solution-building through citizen science. Health Promot. Int. 2022, 37, daac126. [Google Scholar] [CrossRef]
- Wang, Z. Use the Environment to Prevent and Control COVID-19 in Senior-Living Facilities: An Analysis of the Guidelines Used in China. Health Environ. Res. Des. J. 2021, 14, 130–140. [Google Scholar] [CrossRef] [PubMed]
- Ayalon, L.; Avidor, S. ‘We have become prisoners of our own age’: From a continuing care retirement community to a total institution in the midst of the COVID-19 outbreak. Age Ageing 2021, 50, 664–667. [Google Scholar] [CrossRef] [PubMed]
- Shuv-Ami, A.; Toder Alon, A.; Bareket-Bojmel, L. Sheltered Housing and Independent Housing in Israel during the COVID-19 Pandemic: A Comparison of Attitudes and Feelings Among Older Adults. J. Aging Environ. 2021, 36, 304–320. [Google Scholar] [CrossRef]
- Rodríguez-Rodríguez, V.; Rojo-Perez, F.; Pérez de Arenaza Escribano, C.; Molina-Martínez, M.A.; Fernández-Mayoralas, G.; Sánchez-González, D.; Rojo-Abuín, J.M.; Rodríguez-Blázquez, C.; Forjaz, M.J.; Martín-García, S. Impact of COVID-19 in nursing homes: Study design and population description. Int. J. Environ. Res. Public Health 2022, 19. [Google Scholar]
- Zhang, Z.; Zhang, J. Perceived residential environment of neighborhood and subjective well-being among the elderly in China: A mediating role of sense of community. J. Environ. Psychol. 2017, 51, 82–94. [Google Scholar] [CrossRef]
- Rojo-Pérez, F.; Fernández-Mayoralas, G.; Forjaz, M.J.; Prieto-Flores, M.E.; Martínez-Martín, P. Residential Environment and Health Conditions Among Older-Adults in Community-Dwelling in Spain: What Influences Quality of Life? In Environmental Gerontology in Europe and Latin America. Policies and Perspectives on Environment and Aging; Sánchez-González, D., Rodríguez-Rodríguez, V., Eds.; Springer: Berlin/Heidelberg, Germany, 2016; Volume 13, pp. 149–174. [Google Scholar] [CrossRef]
- Prieto-Flores, M.E.; Lardies-Bosque, R.; Rojo-Pérez, F. Residential Environment and Active Ageing: The Role of Physical Barriers in Leisure Participation. In Handbook of Active Ageing and Quality of Later Life. From Concepts to Applications; Rojo-Pérez, F., Fernández-Mayoralas, G., Eds.; Springer: Cham, Switzerland, 2021; pp. 643–655. [Google Scholar] [CrossRef]
- Ahorsu, D.K.; Lin, C.Y.; Imani, V.; Saffari, M.; Griffiths, M.D.; Pakpour, A.H. The Fear of COVID-19 Scale: Development and Initial Validation. Int. J. Ment. Health Addict. 2022, 20, 1537–1545. [Google Scholar] [CrossRef]
- Hoyl, M.T.; Alessi, C.A.; Harker, J.O.; Josephson, K.R.; Pietruszka, F.M.; Koelfgen, M.; Mervis, J.R.; Fitten, L.J.; Rubenstein, L.Z. Development and Testing of a Five-Item Version of the Geriatric Depression Scale. J. Am. Geriatr. Soc. 1999, 47, 873–878. [Google Scholar] [CrossRef]
- Watson, D.; Clark, L.A.; Tellegen, A. Development and validation of brief measures of positive and negative affect: The PANAS scales. J. Personal. Soc. Psychol. 1988, 54, 1063–1070. [Google Scholar] [CrossRef]
- Sinclair, V.G.; Wallston, K.A. The Development and Psychometric Evaluation of the Brief Resilient Coping Scale. Assessment 2004, 11, 94–101. [Google Scholar] [CrossRef]
- Rodríguez-Rodríguez, V. Activities performance by old people in nursing homes during COVID-19. 2022. [Google Scholar]
- San Sebastián Larzabal, L. Optimización de la Medida de Calidad de Vida en Personas Mayores con Dependencia en Centros Residenciales de Guipúzcoa: Escalas FUMAT y QUALID. Ph.D. Thesis, Universidad de Valencia, Valencia, Spain, 2019. [Google Scholar]
- Lawton, M.P. The Philadelphia Geriatric Center Morale Scale: A Revision. J. Gerontol. 1975, 30, 85–89. [Google Scholar] [CrossRef]
- Jung, S.; Siedlecki, K.L. Attitude Toward Own Aging: Age Invariance and Construct Validity Across Middle-Aged, Young-Old, and Old-Old Adults. J. Adult Dev. 2018, 25, 141–149. [Google Scholar] [CrossRef]
- McGarry, B.E.; Grabowski, D.C. Nursing Homes and COVID-19: A Crisis on Top of a Crisis. Ann. Am. Acad. Political Soc. Sci. 2021, 698, 137–162. [Google Scholar] [CrossRef]
- Webber, C.; Myran, D.T.; Milani, C.; Turcotte, L.; Imsirovic, H.; Li, W.; Tanuseputro, P. Cognitive Decline in Long-term Care Residents Before and During the COVID-19 Pandemic in Ontario, Canada. JAMA 2022, 328, 1456–1458. [Google Scholar] [CrossRef] [PubMed]
- Aguilar-Palacio, I.; Maldonado, L.; Marcos-Campos, I.; Castel-Feced, S.; Malo, S.; Aibar, C.; Rabanaque, M.J. Understanding the COVID-19 Pandemic in Nursing Homes (Aragón, Spain): Sociodemographic and Clinical Factors Associated With Hospitalization and Mortality. Front. Public Health 2022, 10, 928174. [Google Scholar] [CrossRef] [PubMed]
- Del Pino, E.; Moreno Fuentes, F.J.; Cruz-Martínez, G.; Hernández-Moreno, J.; Moreno, L.; Pereira-Puga, M.; Perna, R. Informe Gestión Institucional y Organizativa de las Residencias de Personas Mayores y COVID-19: Dificultades y Aprendizajes; Instituto de Políticas y Bienes Públicos (IPP-CSIC): Madrid, Spain, 2020; pp. 1–108. [Google Scholar]
- Escribano, P.; Perez-Granda, M.J.; Alonso, R.; Catalan, P.; Alcala, L.; Serra-Rexarch, J.A.; Osuna, L.; Fernandez, A.; Conti, A.P.; Castellanos, A.; et al. High incidence of COVID-19 at nursing homes in Madrid, Spain, despite preventive measures. Rev. Esp. Quimioter. 2022, 35, 288–292. [Google Scholar] [CrossRef]
- Leao, T.; Severo, M.; Barros, H.; The Public Health Research Group. COVID-19 transmission and case fatality in long-term care facilities during the epidemic first wave. J. Am. Geriatr. Soc. 2021, 69, 3399–3401. [Google Scholar] [CrossRef]
- Tan, L.F.; Tan, M.F. Pandemic to endemic: New strategies needed to limit the impact of COVID-19 in long-term care facilities (LTCFs). J. Am. Geriatr. Soc. 2022, 70, 72–73. [Google Scholar] [CrossRef] [PubMed]
- Valent, F. Age, comorbidities, nursing home stay and outcomes of SARS-CoV-2 infection in a Northern Italian cohort. J. Gerontol. Geriatr. 2021, 69, 114–119. [Google Scholar] [CrossRef]
- Brath, H.; Kalia, S.; Li, J.M.; Lawson, A.; Rochon, P.A. Designing nursing homes with older women in mind. J. Am. Geriatr. Soc. 2022, 1–3. [Google Scholar] [CrossRef] [PubMed]
- Williams, O.; Williams, C.; Turner, D.; Bull, M.; Watkins, J.; Hurt, L. An epidemiological investigation of COVID-19 outbreaks in a group of care homes in Wales, UK: A retrospective cohort study. J. Public Health 2022, 44, 606–613. [Google Scholar] [CrossRef] [PubMed]
- Mody, L.; Gibson, K.E.; Mantey, J.; Bautista, L.; Montoya, A.; Neeb, K.; Jenq, G.; Mills, J.P.; Min, L.; Kabeto, M.; et al. Environmental contamination with SARS-CoV-2 in nursing homes. J. Am. Geriatr. Soc. 2022, 70, 29–39. [Google Scholar] [CrossRef]
- Mullen, N.; Stinchcombe, A.; Seguin, C.; Marshall, S.; Naglie, G.; Rapoport, M.J.; Tuokko, H.; Bedard, M. Perceived Community Age-friendliness is Associated With Quality of Life Among Older Adults. J. Appl. Gerontol. 2022, 41, 1274–1283. [Google Scholar] [CrossRef]
- Avidor, S.; Ayalon, L. “I Didn’t Meet My Mother; I Saw My Mother”: The Challenges Facing Long-Term Care Residents and Their Families in the Age of COVID-19. J. Appl. Gerontol. 2022, 41, 22–29. [Google Scholar] [CrossRef] [PubMed]
- Bonaiuto, M.; Aiello, A.; Perugini, M.; Bonnes, M.; Ercolani, A.P. Multidimensional perception of residential environment quality and neighbourhood attachment in the urban environment. J. Environ. Psychol. 1999, 19, 331–352. [Google Scholar] [CrossRef]
- Mao, Y.; Peng, C.; Liang, Y.; Yuan, G.; Ma, J.; Bonaiuto, M. The Relationship Between Perceived Residential Environment Quality (PREQ) and Community Identity: Flow and Social Capital as Mediators. Soc. Indic. Res. 2022, 163, 771–797. [Google Scholar] [CrossRef] [PubMed]
- Bonaiuto, M.; Fornara, F.; Alves, S.; Ferreira, I.; Mao, Y.; Moffat, E.; Piccinin, G.; Rahimi, L. Urban environment and well-being: Cross-cultural studies on Perceived Residential Environment Quality Indicators (PREQIs). Cogn. Process. 2015, 16, 165–169. [Google Scholar] [CrossRef]
- Fornara, F.; Bonaiuto, M.; Bonnes, M. Cross-Validation of Abbreviated Perceived Residential Environment Quality (PREQ) and Neighborhood Attachment (NA) Indicators. Environ. Behav. 2010, 42, 171–196. [Google Scholar] [CrossRef]
- Bom, J.; Bakx, P.; Rellstab, S. Well-being right before and after a permanent nursing home admission. Health Econ. 2022, 31, 2558–2574. [Google Scholar] [CrossRef] [PubMed]
- Savci, C.; Akinci, A.C.; Usenmez, S.Y.; Keles, F. The effects of fear of COVID-19, loneliness, and resilience on the quality of life in older adults living in a nursing home. Geriatr. Nurs. 2021, 42, 1422–1428. [Google Scholar] [CrossRef] [PubMed]
- Cárdenas Soriano, P.; Rodríguez-Blázquez, C.; Forjaz, M.J.; Ayala, A.; Rojo-Perez, F.; Fernández-Mayoralas, G.; Molina-Martínez, M.A.; Pérez de Arenaza Escribano, C.; Rodríguez-Rodríguez, V. Measurement properties of the Spanish version of the Fear of COVID-19 Scale (FCV-19S) in long-term care settings. Int. J. Environ. Res. Public Health 2022, 19, 16183. [Google Scholar] [CrossRef]
- Ayaz-Alkaya, S.; Dulger, H. Fear of coronavirus and health literacy levels of older adults during the COVID-19 pandemic. Geriatr. Nurs. 2022, 43, 45–50. [Google Scholar] [CrossRef] [PubMed]
- Chura, S.; Saintila, J.; Mamani, R.; Mamani, P.G.R.; Morales-García, W.C. Predictors of Depression in Nurses During COVID-19 Health Emergency; the Mediating Role of Resilience: A Cross-Sectional Study. J. Prim. Care Community Health 2020, 13, 21501319221097075. [Google Scholar] [CrossRef]
- Lo Coco, G.; Gentile, A.; Bosnar, K.; Milovanovic, I.; Bianco, A.; Drid, P.; Pisot, S. A Cross-Country Examination on the Fear of COVID-19 and the Sense of Loneliness during the First Wave of COVID-19 Outbreak. Int. J. Environ. Res. Public Health 2021, 18, 2586. [Google Scholar] [CrossRef]
- Pedrosa, A.L.; Bitencourt, L.; Fontoura Froes, A.C.; Barreto Cazumba, M.L.; Soares de Brito, S.B.C.; Simões e Silva, A.C. Emotional, Behavioral, and Psychological Impact of the COVID-19 Pandemic. Front. Psychol. 2020, 11, 566212. [Google Scholar] [CrossRef]
- Gilbody, S.; Littlewood, E.; McMillan, D.; Chew-Graham, C.A.; Bailey, D.; Gascoyne, S.; Sloan, C.; Burke, L.; Coventry, P.; Crosland, S.; et al. Behavioural activation to prevent depression and loneliness among socially isolated older people with long-term conditions: The BASIL COVID-19 pilot randomised controlled trial. PLoS Med. 2021, 18, e1003779. [Google Scholar] [CrossRef]
- Sandín, B.; Valiente, R.M.; García-Escalera, J.; Chorot, P. Impacto psicológico de la pandemia de COVID-19: Efectos negativos y ositivos en población española asociados al periodo de confinamiento nacional. Rev. Psicopatol. Psicol. Clín. 2020, 25, 1–22. [Google Scholar] [CrossRef]
- Gismero-Gonzalez, E.; Bermejo-Toro, L.; Cagigal, V.; Roldan, A.; Martinez-Beltran, M.J.; Halty, L. Emotional Impact of COVID-19 Lockdown Among the Spanish Population. Front. Psychol. 2020, 11, 616978. [Google Scholar] [CrossRef]
- Losada-Baltar, A.; Martinez-Huertas, J.A.; Jimenez-Gonzalo, L.; Pedroso-Chaparro, M.D.S.; Gallego-Alberto, L.; Fernandes-Pires, J.; Marquez-Gonzalez, M. Longitudinal Correlates of Loneliness and Psychological Distress During the Lockdown Situation due to COVID-19. Effects of Age and Self-Perceptions of Aging. J. Gerontol. Ser. B Psychol. Sci. Soc. Sci. 2022, 77, 652–660. [Google Scholar] [CrossRef]
- Ebert, A.R.; Bernstein, L.E.; Carney, A.K.; Patrick, J.H. Emotional Well-being During the First Four Months of COVID-19 in the United States. J. Adult Dev. 2020, 27, 241–248. [Google Scholar] [CrossRef]
- Rodrigues, N.G.; Han, C.Q.Y.; Su, Y.; Klainin-Yobas, P.; Wu, X.V. Psychological impacts and online interventions of social isolation amongst older adults during COVID-19 pandemic: A scoping review. J. Adv. Nurs. 2021, 78, 609–644. [Google Scholar] [CrossRef] [PubMed]
- Cheung, G.; Bala, S.; Lyndon, M.; Mau, E.; Rivera Rodriguez, C.; Waters, D.L.; Jamieson, H.; Nada-Raja, S.; Chan, A.H.Y.; Beyene, K.; et al. Impact of the first wave of COVID-19 on the health and psychosocial well-being of Maori, Pacific Peoples and New Zealand Europeans living in aged residential care. Australas. J. Ageing 2021, 41, 293–300. [Google Scholar] [CrossRef] [PubMed]
- Nair, P.; Gill, J.S.; Sulaiman, A.H.; Koh, O.H.; Francis, B. Mental Health Correlates Among Older Persons Residing in Malaysian Nursing Homes During the COVID-19 Pandemic. Asia-Pac. J. Public Health 2021, 33, 940–944. [Google Scholar] [CrossRef] [PubMed]
- Barnett, M.L.; Waken, R.J.; Zheng, J.; Orav, E.J.; Epstein, A.M.; Grabowski, D.C.; Joynt Maddox, K.E. Changes in Health and Quality of Life in US Skilled Nursing Facilities by COVID-19 Exposure Status in 2020. JAMA 2022, 328, 941–950. [Google Scholar] [CrossRef]
- Silva, P.; Barbosa, F.; André, M.; Matos, A.D. Home confinement and mental health problems during the COVID-19 pandemic among the population aged 50 and older: A gender perspective. SSM—Popul. Health 2022, 17, 100999. [Google Scholar] [CrossRef]
- Anderson, D.C.; Grey, T.; Kennelly, S.; O’Neill, D. Nursing Home Design and COVID-19: Balancing Infection Control, Quality of Life, and Resilience. J. Am. Med. Dir. Assoc. 2020, 21, 1519–1524. [Google Scholar] [CrossRef]
- Brown, K.A.; Jones, A.; Daneman, N.; Chan, A.K.; Schwartz, K.L.; Garber, G.E.; Costa, A.P.; Stall, N.M. Association Between Nursing Home Crowding and COVID-19 Infection and Mortality in Ontario, Canada. JAMA Intern. Med. 2020, 181, 229–236. [Google Scholar] [CrossRef]
- Rodríguez-Rodríguez, V. Participación en actividades para envejecer activamente. In Envejecimiento Activo, Calidad de Vida y Género. Las Miradas Académica, Institucional y Social; Fernández-Mayoralas, G., Rojo-Pérez, F., Eds.; Tirant lo Blanch: Valencia, Spain, 2021; pp. 231–266. [Google Scholar]
- Rodríguez-Rodríguez, V. Comprensión del envejecimiento activo según contextos. In Envejecimiento Activo, Calidad de Vida y Género. Las Miradas Académica, Institucional y Social; Fernández-Mayoralas, G., Rojo-Pérez, F., Eds.; Tirant lo Blanch: Valencia, Spain, 2021; pp. 127–174. [Google Scholar]
- Tavares, L.M.; Marinho, A. Leisure and COVID-19: Reflections on Brazilian older adults who frequent urban public parks. World Leis. J. 2021, 63, 229–243. [Google Scholar] [CrossRef]
- Kim, E.J.; Park, S.M.; Kang, H.W. Changes in leisure activities of the elderly due to the COVID-19 in Korea. Front. Public Health 2022, 10, 966989. [Google Scholar] [CrossRef]
- Koskinen, V.K.; Leinonen, E.A. Leisure Adjustments of Older Finnish Adults during the Early Stages of the COVID-19 Pandemic. Int. J. Sociol. Leis. 2022, 5, 373–391. [Google Scholar] [CrossRef]
- Smeitink, M.M.P.; Smaling, H.J.A.; van Tol, L.S.; Haaksma, M.L.; Caljouw, M.A.A.; Achterberg, W.P. Activities for Residents of Dutch Nursing Homes during the COVID-19 Pandemic: A Qualitative Study. Int. J. Environ. Res. Public Health 2022, 19, 5465. [Google Scholar] [CrossRef] [PubMed]
- Lood, Q.; Haak, M.; Dahlin-Ivanoff, S. Everyday life in a Swedish nursing home during the COVID-19 pandemic: A qualitative interview study with persons 85 to 100 years. BMJ Open 2021, 11, e048503. [Google Scholar] [CrossRef]
- Navas-Martín, M.Á.; López-Bueno, J.A.; Oteiza, I.; Cuerdo-Vilches, T. Routines, Time Dedication and Habit Changes in Spanish Homes during the COVID-19 Lockdown. A Large Cross-Sectional Survey. Int. J. Environ. Res. Public Health 2021, 18, 12176. [Google Scholar] [CrossRef] [PubMed]
- Ng, S.I.; Lim, X.J.; Hsu, H.C.; Chou, C.C. Age-friendliness of city, loneliness and depression moderated by internet use during the COVID-19 pandemic. Health Promot. Int. 2022, 1–11. [Google Scholar] [CrossRef]
- WHO—World Health Organization. Global Age-Friendly Cities: A Guide; World Health Organization: Geneva, Switzerland, 2007; p. 82. [Google Scholar]
- Brady, C.; Fenton, C.; Loughran, O.; Hayes, B.; Hennessy, M.; Higgins, A.; Leroi, I.; Shanagher, D.; McLoughlin, D.M. Nursing home staff mental health during the Covid-19 pandemic in the Republic of Ireland. Int. J. Geriatr. Psychiatry 2021, 37, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Zollner-Schwetz, I.; Konig, E.; Krause, R.; Pux, C.; Laubreiter, L.; Schippinger, W. Analysis of COVID-19 outbreaks in 3 long-term care facilities in Graz, Austria. Am. J. Infect. Control 2021, 49, 1350–1353. [Google Scholar] [CrossRef]
- Titley, H.K.; Young, S.; Savage, A.; Thorne, T.; Spiers, J.; Estabrooks, C.A. Cracks in the foundation: The experience of care aides in long-term care homes during the COVID-19 pandemic. J. Am. Geriatr. Soc. 2022, 1–8. [Google Scholar] [CrossRef]
- Dupuis-Blanchard, S.; Maillet, D.; Theriault, D.; LeBlanc, F.; Bigonnesse, C. “Be Their Advocate”: Families’ Experience with a Relative in LTC during the COVID-19 Pandemic. Can. J. Aging-Rev. Can. Vieil. 2021, 40, 628–638. [Google Scholar] [CrossRef]
- ILC-BR—International Longevity Centre Brazil. Active Ageing: A Policy Framework in Response to the Longevity Revolution; International Longevity Centre Brazil: Rio de Janeiro, Brazil, 2015; p. 116. [Google Scholar]
- Fernández-Mayoralas, G. Seguridad, envejecimiento activo y calidad de vida [Security, Active Ageing and Quality of Life]. In Envejecimiento Activo, Calidad de Vida y Género. Las Miradas Académica, Institucional y Social; Fernández-Mayoralas, G., Rojo-Pérez, F., Eds.; Tirant lo Blanch: Valencia, Spain, 2021; pp. 267–306. [Google Scholar]
| Aspects | Assessment (%) | N | |
|---|---|---|---|
| Well/Very Well | Badly/Very Badly | ||
| 10.How well their residential home has managed during the COVID-19 pandemic period | 96.1 | 0.9 | 431 |
| 7. Their perception of safety in the residential home | 95.9 | 0.7 | 434 |
| 2. Relationships with nursing-home workers | 95.2 | 1.1 | 435 |
| 9. Having a space for privacy (having a single room or other personal space so as not to be disturbed) | 93.8 | 2.8 | 435 |
| 3. Relationships with family members (e.g., visits in person, by phone, email, other means) | 93.7 | 3.1 | 415 |
| 8. Characteristics and quality of the residential home’s amenities; (e.g., room size and design, natural lighting, noise level, temperature, green areas) | 93.1 | 1.8 | 437 |
| 4. Relationships with friends (e.g., visits in person, by phone, email, other means) | 89.2 | 3.7 | 323 |
| 1. Friendships with other residents | 87.0 | 2.3 | 431 |
| 5. Getting around easily within the residential home (e.g., a lack of obstacles or barriers, ramps, stairs) (indoor accessibility) | 85.5 | 5.9 | 422 |
| 6. The chance to go outside the residential home for different activities (e.g., walking around the neighbourhood or town, shopping, doing other leisure activities, visiting friends) (outdoor accessibility) | 76.9 | 13.2 | 416 |
| 95% C. I. for EXP(B) | |||||||
|---|---|---|---|---|---|---|---|
| Variables in the Equation | Categories | B | Sig. | Exp(B) | Exp(B) Increment (%) | Lower | Upper |
| P.6. The Positive and Negative Affects Schedule (PANAS Balance) | 0.08 | 0.011 | 1.08 | 8.15% | 1.02 | 1.15 | |
| P.4. Fear of developing COVID-19, according to the FCV-19S scale | 0.06 | 0.004 | 1.06 | 5.67% | 1.02 | 1.10 | |
| P.16. Global Quality of Life (the FUMAT-24 scale adapted for elderly people without severe cognitive impairment in nursing homes) | 0.04 | 0.050 | 1.04 | 3.85% | 1.00 | 1.08 | |
| P14A- The Abbreviated Geriatric Depression Scale-Yesavage, 5 items | −0.29 | 0.039 | 0.75 | −25.43% | 0.56 | 0.99 | |
| P.9. Clusters of subjects according to leisure activities performed | (Reference: Inactivity cluster) | 0.001 | |||||
| 1: Use of mobile devices | −0.15 | 0.828 | 0.86 | 0.23 | 3.23 | ||
| 2: Rewarding activities, volunteering | 1.30 | 0.001 | 3.67 | 267.32% | 1.67 | 8.09 | |
| 3: Religious practice | −1.14 | 0.033 | 0.32 | −68.09% | 0.11 | 0.91 | |
| P.10. Room availability | (Reference: Individual/private room) | 0.032 | |||||
| 1: Room shared with my husband/wife/partner/other relative | −0.22 | 0.695 | 0.80 | 0.26 | 2.45 | ||
| 2: Room shared with other resident | −0.79 | 0.009 | 0.46 | −54.48% | 0.25 | 0.82 | |
| P.11. Where did you spend most of your time during the lockdown? | (Reference: Always in my room) | ||||||
| 1: Limited use of different areas, unrestricted use of all spaces in care home | −0.78 | 0.016 | 0.46 | −54.18% | 0.24 | 0.87 | |
| Constant | −2.39 | 0.13 | 0.09 | ||||
| Percentage of cases correctly classified: 77.5 | |||||||
| R Square: Cox and Snell: 0.215; Nagelkerke: 0.311 | |||||||
| Hosmer and Lemeshow test: chi-square: 5.592; df: 8; Sig: 0.693 | |||||||
| In bold, non-significant categories | |||||||
| Variables entered in step: 1: Global Quality of Life (the FUMAT scale, 24 items); 2: Clusters of subjects according to leisure activities performed; 3: Where did you spend most of your time during the lockdown? 4: The Positive and Negative Affects Schedule (PANAS Balance); 5: Fear of developing COVID-19, according to the FCV-19S scale; 6: Room availability; 7: The Abbreviated Geriatric Depression Scale-Yesavage. | |||||||
| 95% C. I. for EXP(B) | |||||||
|---|---|---|---|---|---|---|---|
| Variables in the Equation | Categories | B | Sig. | Exp(B) | Exp(B) Increment (%) | Lower | Upper |
| P.17. Devices or mobile systems used to maintain relationships with your family or friends (e.g., PC, tablet, telephone, mobile) | (Reference: Yes, through my own devices) | 0.019 | |||||
| 1: Yes, through other residents/staff’s devices | 1.32 | 0.010 | 3.75 | 274.63% | 1.37 | 10.25 | |
| 2: No, I do not have access to those devices | −0.60 | 0.371 | 0.55 | 0.15 | 2.05 | ||
| P.22. Gender | (Reference: Male) | ||||||
| 1: Female | 1.18 | 0.004 | 3.25 | 224.57% | 1.45 | 7.29 | |
| P.13. Self-perception of the stay in the nursing home in comparative perspective (before and during the COVID-19 pandemic) | 1.04 | 0.000 | 2.82 | 182.13% | 1.61 | 4.94 | |
| P14A- The Abbreviated Geriatric Depression Scale-Yesavage, 5 items | 0.35 | 0.017 | 1.42 | 41.73% | 1.06 | 1.89 | |
| P.9. Clusters of subjects according to leisure participation | (Reference: Inactivity cluster) | 0.005 | |||||
| 1: Use of mobile devices | 0.32 | 0.701 | 1.37 | 0.27 | 6.95 | ||
| 2: Rewarding activities, volunteering | −1.74 | 0.005 | 0.17 | −82.53% | 0.05 | 0.60 | |
| 3: Religious practice | 1.12 | 0.054 | 3.05 | 0.98 | 9.51 | ||
| Constant | −5.49 | 0.000 | 0.00 | ||||
| Percentage correctly classified: 87.1 | |||||||
| R Square: Cox and Snell: 0.166; Nagelkerke: 0.291 | |||||||
| Hosmer and Lemeshow test: chi-square: 6.681; df: 7; Sig: 0.463 | |||||||
| In bold, non-significant categories | |||||||
| Variables entered in step: 1: Self-perception of the stay in the nursing home in comparative perspective (before and during the COVID-19 pandemic) 2: Clusters of subjects according to leisure participation; 3: Gender; 4: Devices or mobile systems used to maintain relationships with your family or friends (e.g., PC, tablet, telephone, mobile); 5: The Abbreviated Geriatric Depression Scale-Yesavage. | |||||||
| 95% C. I. for EXP(B) | |||||||
|---|---|---|---|---|---|---|---|
| Variables in the Equation | Categories | B | Sig. | Exp(B) | Exp(B) Increment (%) | Lower | Upper |
| P.11. Where did they spend most of their time during the lockdown? | (Reference: Always in my room) | ||||||
| 1: Limited use of different areas, unrestricted use of all spaces in care home | 1.95 | 0.000 | 7.01 | 600.60% | 3.12 | 15.75 | |
| P.23. Marital status | (Reference: Married/living with partner) | 0.003 | |||||
| 1: Separated/Divorced | 0.87 | 0.222 | 2.39 | 0.59 | 9.66 | ||
| 2: Single | 1.84 | 0.001 | 6.29 | 528.74% | 2.05 | 19.25 | |
| 3: Widow/widower | 1.40 | 0.002 | 4.06 | 305.82% | 1.69 | 9.77 | |
| P.3. Satisfaction with life in comparative perspective (before and during the COVID-19 pandemic) | 1.20 | 0.001 | 3.33 | 233.18% | 1.59 | 7.00 | |
| P.16. Quality of life as a whole (the FUMAT-24 scale adapted for elderly people without severe cognitive impairment in nursing homes) | −0.07 | 0.004 | 0.93 | −6.75% | 0.89 | 0.98 | |
| P.6. The Positive and Negative Affects Schedule (PANAS Balance) | −0.12 | 0.010 | 0.89 | −11.04% | 0.81 | 0.97 | |
| P.13. Self-perception of the stay in the nursing home in comparative perspective (before and during the COVID-19 pandemic) | −1.50 | 0.000 | 0.22 | −77.75% | 0.11 | 0.44 | |
| Constant | 3.18 | 0.102 | 24.16 | ||||
| Percentage of cases correctly classified: 91.0 | |||||||
| R Square: Cox and Snell: 0.207; Nagelkerke: 0.394 | |||||||
| Hosmer and Lemeshow test: chi-square: 6.760; df: 8; Sig: 0.563 | |||||||
| In bold, non-significant categories | |||||||
| Variables entered in step: 1: Where did they spend most of their time during the lockdown? 2: Self-perception of the stay in the nursing home in comparative perspective (before and during the COVID-19 pandemic); 3: Global Quality of Life (the FUMAT scale, 24 items); 4: Marital status; 5: Satisfaction with life in comparative perspective (before and during the COVID-19 pandemic); 6: The Positive and Negative Affects Schedule (PANAS Balance). | |||||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rojo-Perez, F.; Rodriguez-Rodriguez, V.; Fernandez-Mayoralas, G.; Sánchez-González, D.; Perez de Arenaza Escribano, C.; Rojo-Abuin, J.-M.; Forjaz, M.J.; Molina-Martínez, M.-Á.; Rodriguez-Blazquez, C. Residential Environment Assessment by Older Adults in Nursing Homes during COVID-19 Outbreak. Int. J. Environ. Res. Public Health 2022, 19, 16354. https://doi.org/10.3390/ijerph192316354
Rojo-Perez F, Rodriguez-Rodriguez V, Fernandez-Mayoralas G, Sánchez-González D, Perez de Arenaza Escribano C, Rojo-Abuin J-M, Forjaz MJ, Molina-Martínez M-Á, Rodriguez-Blazquez C. Residential Environment Assessment by Older Adults in Nursing Homes during COVID-19 Outbreak. International Journal of Environmental Research and Public Health. 2022; 19(23):16354. https://doi.org/10.3390/ijerph192316354
Chicago/Turabian StyleRojo-Perez, Fermina, Vicente Rodriguez-Rodriguez, Gloria Fernandez-Mayoralas, Diego Sánchez-González, Carmen Perez de Arenaza Escribano, Jose-Manuel Rojo-Abuin, Maria João Forjaz, María-Ángeles Molina-Martínez, and Carmen Rodriguez-Blazquez. 2022. "Residential Environment Assessment by Older Adults in Nursing Homes during COVID-19 Outbreak" International Journal of Environmental Research and Public Health 19, no. 23: 16354. https://doi.org/10.3390/ijerph192316354
APA StyleRojo-Perez, F., Rodriguez-Rodriguez, V., Fernandez-Mayoralas, G., Sánchez-González, D., Perez de Arenaza Escribano, C., Rojo-Abuin, J.-M., Forjaz, M. J., Molina-Martínez, M.-Á., & Rodriguez-Blazquez, C. (2022). Residential Environment Assessment by Older Adults in Nursing Homes during COVID-19 Outbreak. International Journal of Environmental Research and Public Health, 19(23), 16354. https://doi.org/10.3390/ijerph192316354












