Physical Activity Counseling in Saudi Arabia: A Systematic Review of Content, Outcomes, and Barriers
Abstract
1. Introduction
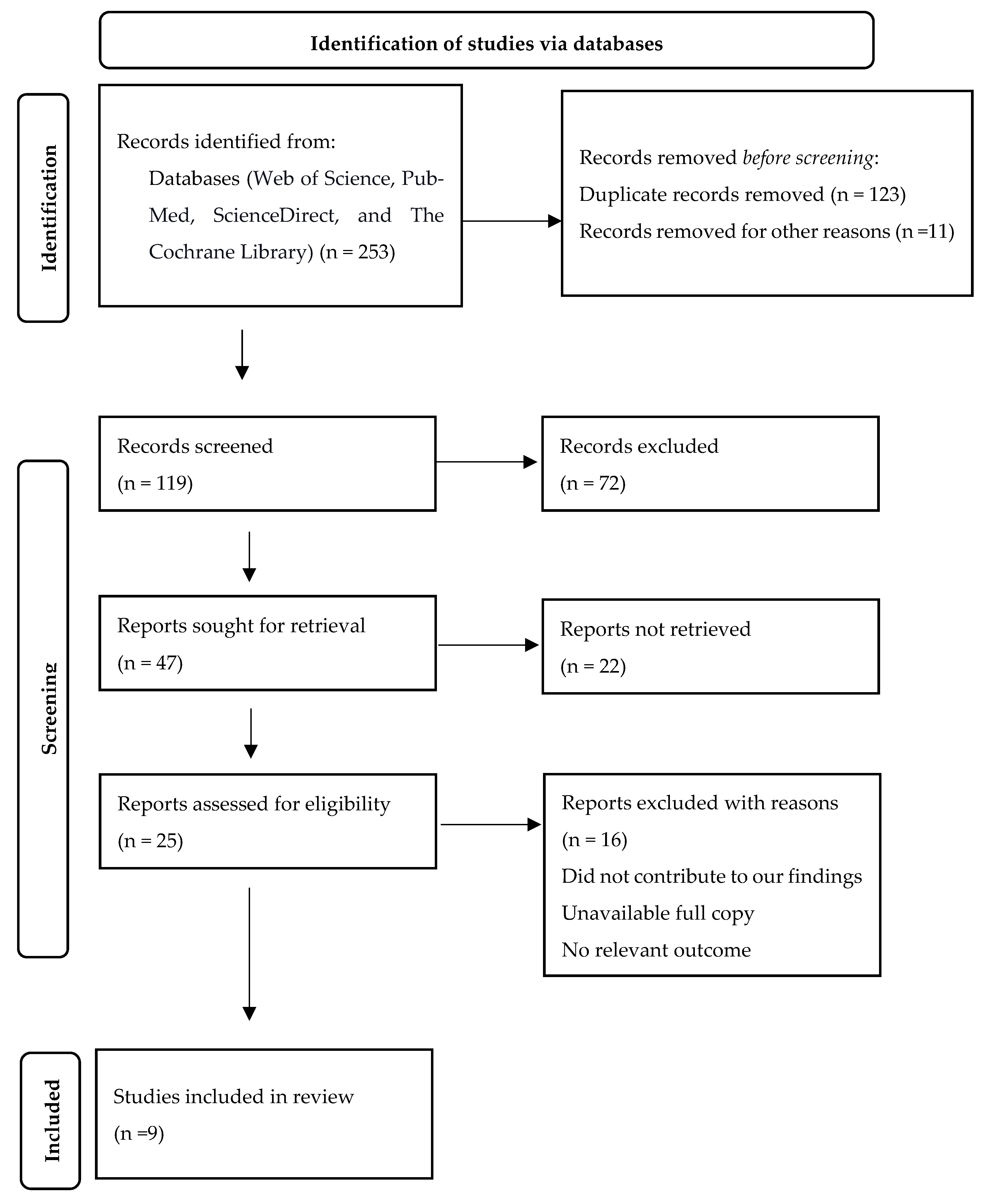
2. Materials and Methods
3. Results
3.1. PA Promotion in the Clinical Context: Characteristics, Content, and Components
3.2. Intervention Studies
3.3. Observational Studies
3.4. Knowledge, Attitudes, and Physicians’ Perceived Competence
3.5. Barriers to PA Counseling
3.6. Reported Outcomes and Efficacy of PA Counseling
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Booth, F.W.; Roberts, C.K.; Laye, M.J. Lack of exercise is a major cause of chronic diseases. Compr. Physiol. 2012, 2, 1143–1211. [Google Scholar] [CrossRef] [PubMed]
- Nieman, D.C.; Wentz, L.M. The compelling link between physical activity and the body’s defense system. J. Sport Health Sci. 2019, 8, 201–217. [Google Scholar] [CrossRef] [PubMed]
- da Silveira, M.P.; da Silva Fagundes, K.K.; Bizuti, M.R.; Starck, É.; Rossi, R.C.; de Resende e Silva, D.T. Physical exercise as a tool to help the immune system against COVID-19: An integrative review of the current literature. Clin. Exp. Med. 2021, 21, 15–28. [Google Scholar] [CrossRef] [PubMed]
- Reiner, M.; Niermann, C.; Jekauc, D.; Woll, A. Long-term health benefits of physical activity—A systematic review of longitudinal studies. BMC Public Health 2013, 13, 813. [Google Scholar] [CrossRef]
- Cerletti, P.; Keidel, D.; Imboden, M.; Schindler, C.; Probst-Hensch, N. The modifying role of physical activity in the cross-sectional and longitudinal association of health-related quality of life with physiological functioning-based latent classes and metabolic syndrome. Health Qual. Life Outcomes 2020, 18, 345. [Google Scholar] [CrossRef]
- Mandolesi, L.; Polverino, A.; Montuori, S.; Foti, F.; Ferraioli, G.; Sorrentino, P.; Sorrentino, G. Effects of Physical Exercise on Cognitive Functioning and Wellbeing: Biological and Psychological Benefits. Front. Psychol. 2018, 9, 509. [Google Scholar] [CrossRef]
- Pfeifer, R.A.; Aljuraiban, G.S.; AlMarzooqi, M.A.; Alghannam, A.F.; BaHammam, A.S.; Dobia, A.M.; Alothman, S.A.; Aljuhani, O.; Aljaloud, K.S. The recommended amount of physical activity, sedentary behavior, and sleep duration for healthy Saudis: A joint consensus statement of the Saudi Public Health Authority. Ann. Thorac. Med. 2021, 16, 239–244. [Google Scholar] [CrossRef]
- World Health Organization. WHO Guidelines on Physical Activity and Sedentary Behavior. 2020. Available online: https://www.who.int/publications/i/item/9789240015128 (accessed on 18 December 2019).
- Alahmed, Z.; Lobelo, F. Physical activity promotion in Saudi Arabia: A critical role for clinicians and the health care system. J. Epidemiol. Glob. Health 2018, 7 (Suppl. S1), S7–S15. [Google Scholar] [CrossRef]
- Mabry, R.; Koohsari, M.J.; Bull, F.; Owen, N. A systematic review of physical activity and sedentary behaviour research in the oil-producing countries of the Arabian Peninsula. BMC Public Health 2016, 16, 1003. [Google Scholar] [CrossRef]
- Alqahtani, B.A.; Alenazi, A.M.; Alhowimel, A.S.; Elnaggar, R.K. The descriptive pattern of physical activity in Saudi Arabia: Analysis of national survey data. Int. Health 2021, 13, 232–239. [Google Scholar] [CrossRef]
- Samara, A.; Nistrup, A.; Al-Rammah, T.Y.; Aro, A.R. Lack of facilities rather than sociocultural factors as the primary barrier to physical activity among female Saudi university students. Int. J. Womens Health 2015, 7, 279–286. [Google Scholar] [CrossRef]
- Herzallah, H.K.; Antonisamy, B.R.; Shafee, M.H.; Al-Otaibi, S.T. Temporal trends in the incidence and demographics of cancers, communicable diseases, and non-communicable diseases in Saudi Arabia over the last decade. Saudi Med. J. 2019, 40, 277–286. [Google Scholar] [CrossRef]
- The Institute for Health Metrics and Evaluation (IHME). Saudi Arabia. 20 September 2019. Available online: http://www.healthdata.org/saudi-arabia (accessed on 18 December 2019).
- Florindo, A.A.; Mielke, G.I.; de Oliveira Gomes, G.A.; Ramos, L.R.; Bracco, M.M.; Parra, D.C.; Simoes, E.J.; Lobelo, F.; Hallal, P.C. Physical activity counseling in primary health care in Brazil: A national study on prevalence and associated factors. BMC Public Health 2013, 13, 794. [Google Scholar] [CrossRef]
- Wattanapisit, A.; Tuangratananon, T.; Thanamee, S. Physical activity counseling in primary care and family medicine residency training: A systematic review. BMC Med. Educ. 2018, 18, 159. [Google Scholar] [CrossRef]
- Sousa Junior, A.E.; Macêdo, G.A.D.; Schwade, D.; Sócrates, J.; Alves, J.W.; Farias-Junior, L.F.; Freire, Y.A.; Lemos, T.M.A.M.; Browne, R.A.V.; Costa, E.C. Physical Activity Counseling for Adults with Hypertension: A Randomized Controlled Pilot Trial. Int. J. Environ. Res. Public Health 2020, 17, 6076. [Google Scholar] [CrossRef]
- Lin, J.S.; O’Connor, E.A.; Evans, C.V.; Senger, C.A.; Rowland, M.G.; Groom, H.C. Behavioral Counseling to Promote a Healthy Lifestyle for Cardiovascular Disease Prevention in Persons with Cardiovascular Risk Factors: An Updated Systematic Evidence Review for the U.S. Preventive Services Task Force; National Library of Medicine: Bethesda, MD, USA, 2014. [Google Scholar]
- Oloo, M.O.; Wamukoya, E.K.; Wanzala, M. Efficacy of Physical Activity Counselling Interventions Delivered in Primary Care: A Systematic Review And Meta-Analysis. Eur. J. Phys. Educ. Sport Sci. 2020. [Google Scholar] [CrossRef]
- Lee, L.L.; Arthur, A.; Avis, M. Evaluating a community-based walking intervention for hypertensive older people in Taiwan: A randomized controlled trial. Prev. Med. 2007, 44, 160–166. [Google Scholar] [CrossRef] [PubMed]
- Lee, C.J.; Kim, J.Y.; Shim, E.; Hong, S.H.; Lee, M.; Jeon, J.Y.; Park, S. The Effects of Diet Alone or in Combination with Exercise in Patients with Prehypertension and Hypertension: A Randomized Controlled Trial. Korean Circ. J. 2018, 48, 637–651. [Google Scholar] [CrossRef] [PubMed]
- Füzéki, E.; Weber, T.; Groneberg, D.A.; Banzer, W. Physical Activity Counseling in Primary Care in Germany—An Integrative Review. Int. J. Environ. Res. Public Health 2020, 17, 5625. [Google Scholar] [CrossRef]
- Rasinaho, M.; Hirvensalo, M.; Törmäkangas, T.; Leinonen, R.; Lintunen, T.; Rantanen, T. Effect of physical activity counseling on physical activity of older people in Finland (ISRCTN 07330512). Health Promot. Int. 2012, 27, 463–474. [Google Scholar] [CrossRef] [PubMed]
- Al-Hazzaa, H.M.; AlMarzooqi, M.A. Descriptive Analysis of Physical Activity Initiatives for Health Promotion in Saudi Arabia. Front. Public Health 2018, 6, 329. [Google Scholar] [CrossRef] [PubMed]
- Sharaf, F. Impact of health education on compliance among patients of chronic diseases in Al Qassim, Saudi Arabia. Int. J. Health Sci. 2010, 4, 139–148. [Google Scholar]
- Alahmed, Z.; Lobelo, F. Correlates of physical activity counseling provided by physicians: A cross-sectional study in Eastern Province, Saudi Arabia. PLoS ONE 2019, 14, e0220396. [Google Scholar] [CrossRef]
- Alfawaz, H.; Naeef, A.F.; Wani, K.; Khattak, M.N.K.; Sabico, S.; Alnaami, A.M.; Al-Daghri, N.M. Improvements in Glycemic, Micronutrient, and Mineral Indices in Arab Adults with Pre-Diabetes Post-Lifestyle Modification Program. Nutrients 2019, 11, 2775. [Google Scholar] [CrossRef]
- Khouja, J.H.; Al Jasir, B.; Bargawi, A.A.; Kutbi, M. Lifestyle Intervention for Cardiovascular Disease Risk Factors in Jeddah. Saudi Arabia. Cureus 2020, 12, e11791. [Google Scholar] [CrossRef]
- Al-Ghamdi, S.; Alajmi, M.; Al-Gonaim, A.; Al-Juhayyim, S.; Al-Qasem, S.; Al-Tamimi, I. Perceptions and attitudes of primary healthcare providers in Riyadh City, Saudi Arabia, toward the promotion of physical activity. Int. J. Health Promot. Educ. 2018, 56, 105–119. [Google Scholar] [CrossRef]
- Midhet, F.M.; Al-Mohaimeed, A. Impact of indoor education on the lifestyles of patients with chronic disease in a secondary hospital in Qassim, Kingdom of Saudi Arabia. J. Taibah Univ. Med. Sci. 2013, 8, 44–49. [Google Scholar] [CrossRef]
- Midhet, F.M.; Sharaf, F.K. Impact of health education on lifestyles in central Saudi Arabia. Saudi Med. J. 2011, 32, 71–76. [Google Scholar]
- Al Shammari, M. Are Family Medicine Residents Physically Active? And Do They Counsel Their Chronically Ill Patients about Physical Activity? A Cross-Sectional Study among Residents of the Family Medicine Joint Program, Eastern Province, Saudi Arabia. Int. J. Med. Sci. Public Health 2016, 5, 1948–1955. [Google Scholar] [CrossRef]
- Al Rashidi, M. Attitudes and Barriers of Primary Care Physicians toward Promoting Physical Activity to Patients in Prince Sultan Military Medical City, Riyadh, Saudi Arabia. Saudi J. Oral Dent. Res. (SJODR) 2018, 3, 135–141. [Google Scholar] [CrossRef]
- Geidl, W.; Wais, J.; Fangmann, C.; Demisse, E.; Pfeifer, K.; Sudeck, G. Physical activity promotion in daily exercise therapy: The perspectives of exercise therapists in German rehabilitation settings. BMC Sports Sci. Med. Rehabil. 2019, 11, 28. [Google Scholar] [CrossRef] [PubMed]
- Gnanendran, A.; Pyne, D.B.; Fallon, K.E.; Fricker, P.A. Attitudes of medical students, clinicians and sports scientists towards exercise counselling. J. Sports Sci. Med. 2011, 10, 426–431. [Google Scholar] [PubMed]
- Solmundson, K.; Koehle, M.; McKenzie, D. Are we adequately preparing the next generation of physicians to prescribe exercise as prevention and treatment? Residents express the desire for more training in exercise prescription. Can. Med. Educ. J. 2016, 7, e79–e96. [Google Scholar] [CrossRef] [PubMed]
- Hébert, E.T.; Caughy, M.O.; Shuval, K. Primary care providers’ perceptions of physical activity counseling in a clinical setting: A systematic review. Br. J. Sports Med. 2012, 46, 625–631. [Google Scholar] [CrossRef]
- Huijg, J.M.; Gebhardt, W.A.; Verheijden, M.W.; Phillips, E.M. Factors influencing primary health care professionals’ physical activity promotion behaviors: A systematic review. Int. J. Behav. Med. 2015, 22, 32–50. [Google Scholar] [CrossRef]
- Estabrooks, P.A.; Glasgow, R.E.; Dzewaltowski, D.A. Physical activity promotion through primary care. JAMA 2003, 289, 2913–2916. [Google Scholar] [CrossRef]
- Meriwether, R.A.; Lee, J.A.; Lafleur, A.S.; Wiseman, P. Physical activity counseling. Am. Fam. Physician 2008, 77, 1129–1136. [Google Scholar]
- Peterson, J.A. Get moving! Physical activity counseling in primary care. J. Am. Acad. Nurse Pract. 2007, 19, 349–357. [Google Scholar] [CrossRef]
- Antognoli, E.L.; Seeholzer, E.L.; Gullett, H.; Jackson, B.; Smith, S.; Flocke, S.A. Primary care resident training for obesity, nutrition, and physical activity counseling: A mixed-methods study. Health Promot. Pract. 2017, 18, 672–680. [Google Scholar] [CrossRef]
- Malatskey, L.; Bar Zeev, Y.; Tzuk-Onn, A.; Polak, R. Lifestyle medicine course for family medicine residents: Preliminary assessment of the impact on knowledge, attitudes, self-efficacy and personal health. Postgrad. Med. J. 2017, 93, 549–554. [Google Scholar] [CrossRef]
- Omura, J.D.; Bellissimo, M.P.; Watson, K.B.; Loustalot, F.; Fulton, J.E.; Carlson, S.A. Primary care providers’ physical activity counseling and referral practices and barriers for cardiovascular disease prevention. Prev. Med. 2018, 108, 115–122. [Google Scholar] [CrossRef] [PubMed]
- Saller, F.V. Qualitative Analysis of Psycho-Social Factors of Potential Influence on Physical Activity and Dietary Practice of Patients with Diabetes and Cardiovascular Disease in Saudi Arabia. Saudi J. Nurs. Health Care 2021, 4, 99–113. [Google Scholar] [CrossRef]
- Saller, F.V.; Mohammed, A.; Al Dhaferi, F. Physical activity and behavioral regulations for exercise in patients with noncommunicable disease in central Saudi Arabia. Saudi J. Sports Med. 2020, 20, 13. [Google Scholar] [CrossRef]
- Fleming, J.; Bryce, C.; Parsons, J.; Wellington, C.; Dale, J. Engagement with and delivery of the ‘parkrun practice initiative’ in general practice: A mixed methods study. Br. J. Gen. Pract. 2020, 70, e573–e580. [Google Scholar] [CrossRef]
| Author and Year | Methodological Appraisal Score | Participant | Region/City | Program/Training | Outcome | |
|---|---|---|---|---|---|---|
| 1 | Alahmed et al., 2019 [26] | 75 | 147 physicians | Eastern Province, SA (Al-Khobar, Dammam, Qatif, and Safwa) | KAP study of PA counseling | Only 21.8% had received training about PA counseling during medical school or their residency program. Almost 60% of physicians believed that PA promotion to patients was their responsibility and felt confident in their ability to provide PA counseling. Lack of time, inadequate referral services for PA, and inadequate training in PA counseling were considered barriers to providing PA counseling. |
| 2 | Alfawaz et al., 2019 [27] | 75 | 160 Saudis with prediabetes | Riyadh | Two-armed lifestyle modification program | A significant improvement was found in the glycemic indices of the intervention group after a 6-month lifestyle modification program. Additionally, significant improvements in dietary habits and physical activity levels were more apparent in the intervention group than the control group. |
| 3 | Khouja et al., 2020 [28] | 75 | Women ≥30 years old with a moderate to high risk of CVD | Jeddah | Three-month intervention involving lifestyle modification and physical activity with standard care | The lifestyle intervention program significantly reduced systolic blood pressure (−9.2 mmHg), blood glucose (−45 mg/dL), and Framingham risk score (−13.6). |
| 4 | Al-Ghamdi et al., 2018 [29] | 75 | 803 healthcare providers | Riyadh | KAP study of PA counseling | A significant difference in the opinions of healthcare professionals regarding their perceptions of PA levels among the general population was observed. The data showed that most primary care staff were quite enthusiastic about promoting physical activity among their patients and revealed that they routinely discussed and advised their patients about the benefits of physical fitness. However, there were some factors that acted as barriers to promoting PA, such as lack of time, lack of educational materials for patients, lack of proper training and protocols, lack of patient cooperation, and lack of financial incentive. |
| 5 | Midhet (2013) [30] | 75 | 169 patients | Al Qasim | Patient health education | Health education sessions were significantly associated with healthier diet and regular exercise of patients. |
| 6 | Midhet (2011) [31] | 75 | Baseline (n = 1254) and follow-up (n = 1011) attendees in PHCC centers | Al Qasim | Trained the PHCC staff in health education skills and introduced health education seminars | Compared to the baseline, male respondents in the follow-up survey were less likely to smoke and more likely to do regular exercise (such as doing brisk walks and playing football). |
| 7 | Sharaf (2011) [25] | 75 | Patients with chronic diseases (e.g., coronary artery disease) | Al Qassim Region | The intervention included refresher training for PHC centers’ staff to improve communication skills and the use of health education materials | Among chronic disease patients, significant improvements in smoking, diet, and exercise habits were observed at the end-line survey compared to the baseline. |
| 8 | Al Shammari (2016) [32] | 75 | 80 family medicine residents | Al Khobar | KAP study of PA counseling | The majority of the participants counseled their patients about physical activity, especially if the patient had diabetes. Residents of the joint family medicine program of the eastern province of the KSA self-reported that while they were not physically active themselves, they were active in in-patient counseling regarding the importance of physical activity to achieve global health and well-being. |
| 9 | AlRashdi (2015) [33] | 75 | 80 primary care physicians | Riyadh | Attitudes and perceived = barriers of primary care physicians | Advice to increase physical activity was given to patients by most participants, and most considered themselves effective health promoters. Lack of time, patients ignoring physician recommendations, and insufficient educational materials for patients were the most frequently perceived barriers by primary care physicians regarding promoting physical activity. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
AlMarzooqi, M.A.; Saller, F. Physical Activity Counseling in Saudi Arabia: A Systematic Review of Content, Outcomes, and Barriers. Int. J. Environ. Res. Public Health 2022, 19, 16350. https://doi.org/10.3390/ijerph192316350
AlMarzooqi MA, Saller F. Physical Activity Counseling in Saudi Arabia: A Systematic Review of Content, Outcomes, and Barriers. International Journal of Environmental Research and Public Health. 2022; 19(23):16350. https://doi.org/10.3390/ijerph192316350
Chicago/Turabian StyleAlMarzooqi, Mezna A., and Franziska Saller. 2022. "Physical Activity Counseling in Saudi Arabia: A Systematic Review of Content, Outcomes, and Barriers" International Journal of Environmental Research and Public Health 19, no. 23: 16350. https://doi.org/10.3390/ijerph192316350
APA StyleAlMarzooqi, M. A., & Saller, F. (2022). Physical Activity Counseling in Saudi Arabia: A Systematic Review of Content, Outcomes, and Barriers. International Journal of Environmental Research and Public Health, 19(23), 16350. https://doi.org/10.3390/ijerph192316350








