The Association among Alcohol Consumption Patterns, Drink-Driving Behaviors, and the Harm from Alcohol-Related Road Traffic Injuries Due to the Drinking of Others in Thailand
Abstract
1. Introduction
2. Materials and Methods
2.1. Data and Sample Population
2.2. Measurements
- white liquor/herbal liquor: five shots or one fourth of a large bottle or half of a middle-sized bottle, or
- distilled liquor: one fourth of a large bottle or five shots or eight glasses of distilled liquor containing a mixer, or
- beer: four cans or two large bottles, or
- wine/champagne: one large bottle or four glasses of wine, or
- cider/wine coolers: four and a half bottles or cans, or
- fermented liquor (rice liquor/locally made liquor): one large bottle or two and a half glasses).
- (1)
- In the past 12 months, have you drunk liquor/alcohol beverages before or while driving a vehicle? There were four choices of answers, including (1) frequently, (2) sometimes, (3) driven but never drank before driving, and (4) never drove. This question was asked only among current drinkers. We classified choices 1 and 2 as drink-driving and choice 3 as non-drink-driving. We also excluded those who responded with choice 4 or non-drivers from the model that included drink-driving variables in order to avoid underestimation of drink-driving effect.
- (2)
- In the past 12 months, have you been injured or had an accident due to your own drinking before or while driving a vehicle? The choices of answers were never and frequently (one time, two times, three times, or more than three times). We classified those responded “frequently” as those who reported harm from road traffic injuries due to self-drink-driving behaviors.
- (3)
- In the past 12 months, have you been injured or had an accident by other people driving a vehicle? The choices of answers were never and frequently (i.e., was a passenger with intoxicated driver, was a passenger with unintoxicated driver but the opposite party was intoxicated, was a passenger with intoxicated driver and the opposite party was also intoxicated, was a passenger but was not sure whether the driver and/or the opposite party drank alcohol, and was a pedestrian (on the road/pavement) and was hit by intoxicated driver). We classified those who responded “frequently” as those who reported road traffic injuries due to others’ drink-driving behavior.
2.3. Data Analysis
2.4. Ethical Considerations
3. Results
3.1. Demographic Characteristics, Socio-Economic Status, and Alcohol-Related Road Traffic Injuries
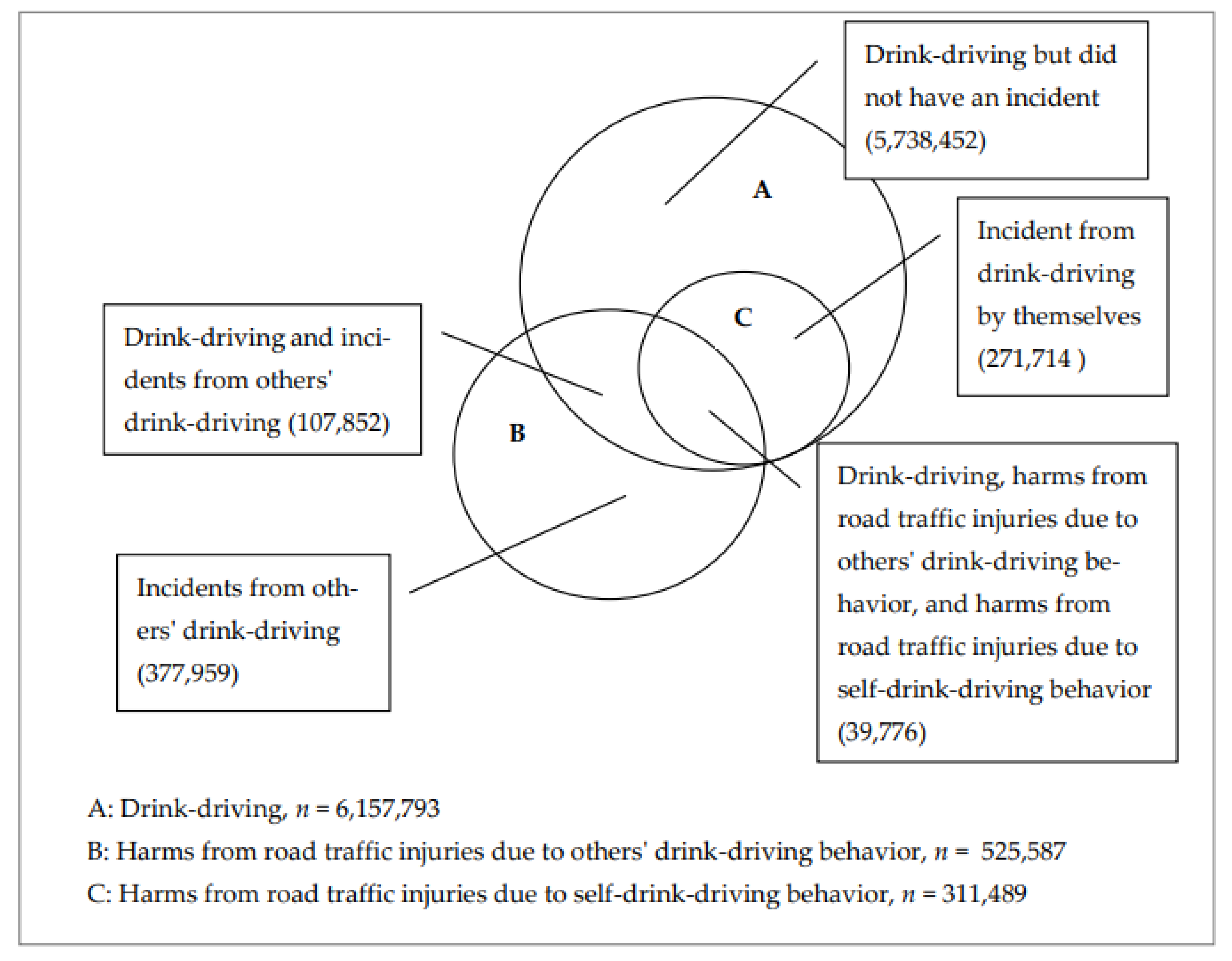
3.2. Self-Reported Drinking Behavior and Experience of Road Traffic Injury Due to Others’ Drink-Driving Behavior
3.3. Factors Associated with Road Traffic-Related Injuries and Ones’ Own Alcohol Drinking Behavior
4. Discussion
4.1. Strengths and Limitations
4.2. Policy Implications
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Global Status Report on Road Safety 2018; World Health Organization: Geneva, Switzerland, 2018.
- International Health Policy Program. Thailand Burden of Diseases 2014; International Health Policy Program: Nonthaburi, Thailand, 2017.
- Stewart, K.; Silcock, D.; Wegman, F. Reducing drink driving in low- and middle-income countries: Challenges and opportunities. Traffic Inj. Prev. 2012, 13, 93–95. [Google Scholar] [CrossRef] [PubMed]
- Das, A.; Gjerde, H.; Gopalan, S.S.; Normann, P.T. Alcohol, drugs, and road traffic crashes in India: A systematic review. Traffic Inj. Prev. 2012, 13, 544–553. [Google Scholar] [CrossRef] [PubMed]
- Taylor, B.; Irving, H.; Kanteres, F.; Room, R.; Borges, G.; Cherpitel, C.; Greenfield, T.; Rehm, J. The more you drink, the harder you fall: A systematic review and meta-analysis of how acute alcohol consumption and injury or collision risk increase together. Drug Alcohol Depend. 2010, 110, 108–116. [Google Scholar] [CrossRef] [PubMed]
- Jones, A.W.; Kugelberg, F.C.; Holmgren, A.; Ahlner, J. Five-year update on the occurrence of alcohol and other drugs in blood samples from drivers killed in road-traffic crashes in Sweden. Forensic Sci. Int. 2009, 186, 56–62. [Google Scholar] [CrossRef] [PubMed]
- Cherpitel, C.J.; Bond, J.; Ye, Y.; Borges, G.; MacDonald, S.; Stockwell, T.; Giesbrecht, N.; Cremonte, M. Alcohol-related injury in the ER: A cross-national meta-analysis from the Emergency Room Collaborative Alcohol Analysis Project (ERCAAP). J. Stud. Alcohol 2003, 64, 641–649. [Google Scholar] [CrossRef] [PubMed]
- Kemnitzer, C.R.; Pope, C.N.; Nwosu, A.; Zhao, S.; Wei, L.; Zhu, M. An investigation of driver, pedestrian, and environmental characteristics and resulting pedestrian injury. Traffic Inj. Prev. 2019, 20, 510–514. [Google Scholar] [CrossRef] [PubMed]
- Ulfarsson, G.F.; Kim, S.; Booth, K.M. Analyzing fault in pedestrian–motor vehicle crashes in North Carolina. Accid. Anal. Prev. 2010, 42, 1805–1813. [Google Scholar] [CrossRef] [PubMed]
- Waleewong, O.; Jankhotkaew, J.; Thamarangsi, T.; Chaiyasong, S. Prevalence of harm from others’ alcohol drinking and the relationships with demographics and the respondents’ drinking behaviors in Thailand. J. Subst. Use 2017, 22, 605–611. [Google Scholar] [CrossRef]
- Elliott, S.; Woolacott, H.; Braithwaite, R. The prevalence of drugs and alcohol found in road traffic fatalities: A comparative study of victims. Sci. Justice 2009, 49, 19–23. [Google Scholar] [CrossRef]
- Al-Abdallat, I.M.; Al Ali, R.; Hudaib, A.A.; Salameh, G.A.M.; Salameh, R.J.M.; Idhair, A.K.F. The prevalence of alcohol and psychotropic drugs in fatalities of road-traffic accidents in Jordan during 2008–2014. J. Forensic Leg. Med. 2016, 39, 130–134. [Google Scholar] [CrossRef] [PubMed]
- National Statistical Office. The Smoking and Drinking Behaviours Survey 2017; National Statistical Office: Bangkok, Thailand, 2017.
- Bennett, D.A. How can I deal with missing data in my study? Aust. New Zealand J. Public Health 2001, 25, 464–469. [Google Scholar] [CrossRef]
- World Health Organization. International Guide for Monitoring Alcohol Consumption and Related Harm; World Health Organization: Geneva, Switzerland, 2000.
- Storvoll, E.E.; Moan, I.S.; Lund, I.O. Negative consequences of other people’s drinking: Prevalence, perpetrators and locations. Drug Alcohol Rev. 2016, 35, 755–762. [Google Scholar] [CrossRef]
- Moan, I.S.; Storvoll, E.E.; Sundin, E.; Lund, I.O.; Bloomfield, K.; Hope, A.; Ramstedt, M.; Huhtanen, P.; Kristjánsson, S. Experienced harm from other people’s drinking: A comparison of Northern European Countries. Subst. Abus. Res. Treat. 2015, 9 (Suppl. 2), 45–57. [Google Scholar] [CrossRef] [PubMed]
- Connor, J.; Casswell, S. The burden of road trauma due to other people′s drinking. Accid. Anal. Prev. 2009, 41, 1099–1103. [Google Scholar] [CrossRef]
- Brumback, T.; Cao, D.; King, A. Effects of alcohol on psychomotor performance and perceived impairment in heavy binge social drinkers. Drug Alcohol Depend. 2007, 91, 10–17. [Google Scholar] [CrossRef] [PubMed]
| Variable | Road Traffic Injuries Due to Others’ Drink-Driving Behavior | Drink-Driving | Harms from Road Traffic Injuries Due to Self-Drink-Driving Behavior | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Total | No | Yes | Total | No | Yes | Total | No | Yes | |
| n = 50,460,216 | n = 49,934,630 | n = 525,587 | n = 11,028,449 | n = 4,870,656 | n = 6,157,793 | n = 6,157,793 | n = 5,846,304 | n = 311,489 | |
| Demographic Characteristics | |||||||||
| Gender | |||||||||
| Female | 25,337,036 | 99.27 | 0.73 | 1,669,219 | 60.25 | 39.75 | 663,529 | 98.58 | 1.42 |
| Male | 25,123,180 | 98.65 | 1.35 | 9,359,230 | 41.30 | 58.70 | 5,494,264 | 94.50 | 5.50 |
| Age group | |||||||||
| 15–19 years | 3,188,928 | 98.92 | 1.08 | 415,342 | 33.22 | 66.78 | 277,381 | 92.88 | 7.12 |
| 20–24 years | 3,983,154 | 98.47 | 1.53 | 1,114,648 | 37.69 | 62.31 | 694,562 | 94.58 | 5.42 |
| 25–44 years | 18,282,069 | 98.98 | 1.02 | 5,219,448 | 44.88 | 55.12 | 2,876,899 | 95.19 | 4.81 |
| 45–59 years | 13,979,323 | 98.98 | 1.02 | 3,353,441 | 45.04 | 54.96 | 1,842,933 | 95.16 | 4.84 |
| 60+ years | 11,026,742 | 99.09 | 0.91 | 925,570 | 49.65 | 50.35 | 466,018 | 94.34 | 5.66 |
| Marital status | |||||||||
| Single | 11,908,964 | 98.83 | 1.17 | 2,663,421 | 39.85 | 60.15 | 1,602,018 | 94.03 | 5.97 |
| Married | 31,882,292 | 98.98 | 1.02 | 7,525,616 | 45.96 | 54.04 | 4,066,941 | 95.38 | 4.62 |
| Divorced/widowed/separated | 6,668,961 | 99.09 | 0.91 | 839,412 | 45.96 | 54.04 | 488,834 | 94.27 | 5.73 |
| Region | |||||||||
| Bangkok | 7,082,856 | 99.46 | 0.54 | 1,126,807 | 64.93 | 35.07 | 395,222 | 95.19 | 4.81 |
| Central | 14,854,799 | 99.18 | 0.82 | 3,172,182 | 49.89 | 50.11 | 1,589,682 | 94.96 | 5.04 |
| North | 8,628,601 | 99.13 | 0.87 | 2,447,347 | 32.53 | 67.47 | 1,651,261 | 96.82 | 3.18 |
| Northeast | 13,344,282 | 98.22 | 1.78 | 3,426,680 | 42.49 | 57.51 | 1,970,541 | 93.62 | 6.38 |
| South | 6,549,678 | 99.21 | 0.79 | 855,433 | 35.58 | 64.42 | 551,087 | 93.82 | 6.18 |
| Area | |||||||||
| Rural | 27,313,442 | 98.92 | 1.08 | 6,368,201 | 40.73 | 59.27 | 3,774,634 | 94.94 | 5.06 |
| Urban | 23,146,774 | 99.00 | 1.00 | 4,660,248 | 48.86 | 51.14 | 2,383,159 | 94.94 | 5.06 |
| Education | |||||||||
| Illiterate | 2,361,988 | 99.26 | 0.74 | 195,144 | 49.84 | 50.16 | 97,884 | 92.64 | 7.36 |
| Primary school | 22,899,870 | 98.89 | 1.11 | 4,442,968 | 41.78 | 58.22 | 2,586,780 | 93.58 | 6.42 |
| Secondary school | 8,383,518 | 98.88 | 1.12 | 2,207,363 | 42.49 | 57.51 | 1,269,560 | 94.72 | 5.28 |
| High school | 7,981,081 | 98.86 | 1.14 | 2,217,553 | 43.92 | 56.08 | 1,243,691 | 95.75 | 4.25 |
| Diploma or higher | 8,833,759 | 99.22 | 0.78 | 1,965,422 | 51.16 | 48.84 | 959,878 | 98.09 | 1.91 |
| Socio-Economic Status | |||||||||
| Employment status | |||||||||
| Unemployed | 13,058,323 | 99.19 | 0.81 | 902,748 | 46.22 | 53.78 | 485,462 | 93.11 | 6.89 |
| Employed | 37,401,894 | 98.88 | 1.12 | |10,125,701 | 43.98 | 56.02 | 5,672,331 | 95.10 | 4.90 |
| Monthly (individual) income | |||||||||
| Poorest (quintile 1) | 9,017,346 | 98.92 | 1.08 | 860,929 | 43.28 | 56.72 | 488,361 | 90.95 | 9.05 |
| Poor (quintile 2) | 11,102,039 | 98.90 | 1.10 | 2,006,246 | 39.22 | 60.78 | 1,219,418 | 95.25 | 4.75 |
| Middle (quintile 3) | 8,036,462 | 98.83 | 1.17 | 2,192,836 | 38.83 | 61.17 | 1,341,252 | 94.35 | 5.65 |
| Richer (quintile 4) | 10,443,773 | 99.02 | 0.98 | 2,759,977 | 43.88 | 56.12 | 1,548,857 | 94.47 | 5.53 |
| Richest (quintile 5) | 11,860,596 | 99.07 | 0.93 | 3,208,462 | 51.38 | 48.62 | 1,559,904 | 96.93 | 3.07 |
| Variable | Model 1: RTI and HTO n = 80,797 | Model 2: RTI and HTO n = 80,797 | Model 3: RTI and HTO n = 75,305 | Model 4: RTI and HTO n = 75,305 | ||||
|---|---|---|---|---|---|---|---|---|
| AOR | 95% CI | AOR | 95% CI | AOR | 95% CI | AOR | 95% CI | |
| Current drinking in past 12 months | ||||||||
| Non-drinker | 1 | |||||||
| Drink | 1.50 ** | (1.49–1.51) | ||||||
| Binge-drinking | ||||||||
| Non-drinker | 1 | |||||||
| Drink without binging | 0.97 ** | (0.97–0.98) | ||||||
| Binge-drinker | 2.31 ** | (2.30–2.33) | ||||||
| Drink and driving | ||||||||
| Non-drinker | 1 | |||||||
| Drink without driving | 1.20 ** | (1.19–1.21) | ||||||
| Drink-driving | 2.12 ** | (2.10–2.14) | ||||||
| Drink-driving and injury | ||||||||
| Non-drinker | 1 | |||||||
| Drink without driving | 1.20 ** | (1.99–1.21) | ||||||
| Drink-drive and no injury from self-drinking | 1.64 ** | (1.62–1.65) | ||||||
| Drink-drive and injury from self-drinking | 11.57 ** | (11.43–11.71) | ||||||
| Demographic Characteristics | ||||||||
| Gender | ||||||||
| Female | 1 | 1 | 1 | 1 | ||||
| Male | 1.53 ** | (1.52–1.54) | 1.44 ** | (1.43–1.45) | 1.60 ** | (1.59–1.61) | 1.57 ** | (1.56–1.58) |
| Age group | ||||||||
| 15–19 years | 1 | 1 | 1 | 1 | ||||
| 20–24 years | 1.35 ** | (1.33–1.37) | 1.27 ** | (1.25–1.29) | 1.38 ** | (1.36–1.40) | 1.36 ** | (1.34–1.38) |
| 25–44 years | 0.98 ** | (0.96–0.99) | 0.93 ** | (0.92–0.94) | 0.98 | (0.97–1.00) | 0.97 ** | (0.86–0.99) |
| 45–59 years | 0.90 ** | (0.88–0.91) | 0.87 ** | (0.86–0.88) | 0.90 ** | (0.88- 0.91) | 0.89 ** | (0.88–0.91) |
| 60+ years | 0.89 ** | (0.88–0.90) | 0.89 ** | (0.88–0.90) | 0.95 ** | (0.94–0.97) | 0.96 ** | (0.95–0.98) |
| Marital status | ||||||||
| Single | 1 | 1 | 1 | 1 | ||||
| Married | 0.87 ** | (0.86–0.87) | 0.89 ** | (0.88–0.90) | 0.87 ** | (0.86–0.88) | 0.89 ** | (0.88–0.90) |
| Divorced/widowed/separated | 0.95 ** | (0.94–0.96) | 0.94 ** | (0.93–0.95) | 0.96 ** | (0.96–0.98) | 0.98 ** | (0.97–1.00) |
| Region | ||||||||
| Bangkok | 1 | 1 | 1 | 1 | ||||
| Central | 1.65 ** | (1.64–1.68) | 1.65 ** | (1.63–1.67) | 1.90 ** | (1.88–1.93) | 1.91 ** | (1.89–1.94) |
| North | 1.74 ** | (1.72–1.76) | 1,73 ** | (1.71–1.75) | 1.89 ** | (1.86–1.91) | 1.96 ** | (1.93–1.99) |
| Northeast | 3.59 ** | (3.54–3.63) | 3.53 ** | (3.49–3.57) | 3.94 ** | (3.89–3.99) | 3.92 ** | (3.87–3.94) |
| South | 1.71 ** | (1.69–1.73) | 1.72 ** | (1.69–1.74) | 1.82 ** | (1.58–1.85) | 1.81 ** | (1.79–1.84) |
| Area | ||||||||
| Rural | 1 | 1 | 1 | 1 | ||||
| Urban | 1.28 ** | (1.27–1.28) | 1.28 ** | (1.28–1.29) | 1.32 ** | (1.32–1.33) | 1.30 ** | (1.30–1.31) |
| Education | ||||||||
| Illiterate | 1 | 1 | 1 | 1 | ||||
| Primary school | 1.13 ** | (1.12–1.15) | 1.13 ** | (1.11–1.15) | 0.99 | (0.97–1.01) | 0.99 | (0.98–1.01) |
| Secondary school | 1.04 ** | (1.02–1.06) | 1.02 * | (1.00–1.04) | 0.86 ** | (0.85–0.88) | 0.88 ** | (0.86–0.89) |
| High school | 1.08 ** | (1.06–1.10) | 1.08 ** | (1.06–1.10) | 0.94 ** | (0.93–0.96) | 0.98 ** | (0.97–1.00) |
| Diploma or higher | 0.85 ** | (0.83–0.86) | 0.86 ** | (0.84–0.87) | 0.77 ** | (0.76–0.79) | 0.82 ** | (0.80–0.83) |
| Socio-Economic Status | ||||||||
| Employment status | ||||||||
| Unemployed | 1 | 1 | 1 | 1 | ||||
| Employed | 0.89 ** | (1.28–1.30) | 1.28 ** | (1.27–1.29) | 1.28 ** | (1.27–1.29) | 1.30 ** | (1.28–1.31) |
| Monthly (individual) Income | ||||||||
| Poorest (quintile 1) | 1 | 1 | 1.00 | |||||
| Poor (quintile 2) | 0.89 ** | (0.88–0.90) | 0.89 ** | (0.88- 0.90) | 0.99 ** | (0.89–0.91) | 0.92 ** | (0.91–0.93) |
| Middle (quintile 3) | 0.85 ** | (0.84–0.85) | 0.85 ** | (0.84–0.86) | 0.84 ** | (0.83–0.84) | 0.85 ** | (0.84–0.86) |
| Richer (quintile 4) | 0.79 ** | (0.78–0.80) | 0.80 ** | (0.79–0.81) | 0.71 ** | (0.70–0.72) | 0.73 ** | (0.72–0.74) |
| Richest (quintile 5) | 0.93 ** | (0.92–0.94) | 0.93 ** | (0.92–0.94) | 0.92 ** | (0.91–0.93) | 0.95 ** | (0.94–0.97) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nasueb, S.; Jankhotkaew, J.; Vichitkunakorn, P.; Waleewong, O. The Association among Alcohol Consumption Patterns, Drink-Driving Behaviors, and the Harm from Alcohol-Related Road Traffic Injuries Due to the Drinking of Others in Thailand. Int. J. Environ. Res. Public Health 2022, 19, 16281. https://doi.org/10.3390/ijerph192316281
Nasueb S, Jankhotkaew J, Vichitkunakorn P, Waleewong O. The Association among Alcohol Consumption Patterns, Drink-Driving Behaviors, and the Harm from Alcohol-Related Road Traffic Injuries Due to the Drinking of Others in Thailand. International Journal of Environmental Research and Public Health. 2022; 19(23):16281. https://doi.org/10.3390/ijerph192316281
Chicago/Turabian StyleNasueb, Sopit, Jintana Jankhotkaew, Polathep Vichitkunakorn, and Orratai Waleewong. 2022. "The Association among Alcohol Consumption Patterns, Drink-Driving Behaviors, and the Harm from Alcohol-Related Road Traffic Injuries Due to the Drinking of Others in Thailand" International Journal of Environmental Research and Public Health 19, no. 23: 16281. https://doi.org/10.3390/ijerph192316281
APA StyleNasueb, S., Jankhotkaew, J., Vichitkunakorn, P., & Waleewong, O. (2022). The Association among Alcohol Consumption Patterns, Drink-Driving Behaviors, and the Harm from Alcohol-Related Road Traffic Injuries Due to the Drinking of Others in Thailand. International Journal of Environmental Research and Public Health, 19(23), 16281. https://doi.org/10.3390/ijerph192316281






