The Follow-Up of Eating Disorders from Adolescence to Early Adulthood: A Systematic Review
Abstract
1. Introduction
1.1. Clinical Course of Eating Disorders
1.2. Remission and Relapse
1.3. Comorbidities and Complications
1.4. Purpose
2. Materials and Methods
2.1. The Research Questions
- (1)
- What is the percentage of ED persistence from its onset to early adulthood considering remission, relapse, and death?
- (2)
- What kinds of psychiatric, medical disorders, and/or substance use comorbidities are associated to EDs in early adulthood?
- (3)
- What kinds of social–relational difficulties can complicate EDs in early adulthood?
2.2. Study Identification
2.3. Inclusion Criteria
2.4. Literature Search
- −
- (Anorexia OR bulimia OR eating disorder) AND (psychiatric comorbidity) AND (substance use);
- −
- (Anorexia OR bulimia) AND (outcome OR follow-up) AND (recovery OR relapse).
2.5. Statistical Analysis
2.6. Study Quality Assessment
3. Results
3.1. Study Selection
3.2. Study Characteristics and Design
3.3. Study Samples
3.4. Quantitative Analysis
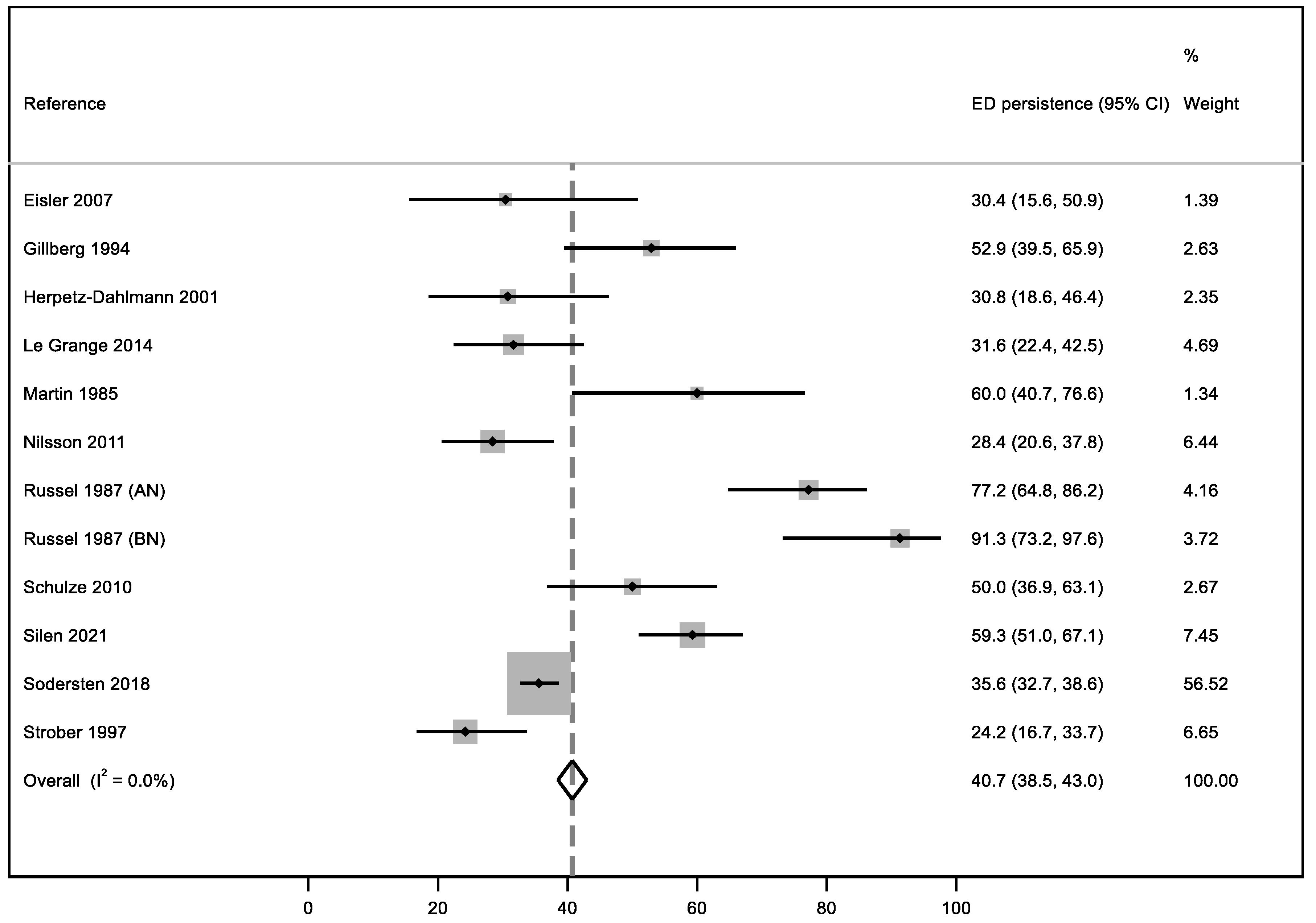
3.5. ED Persistence
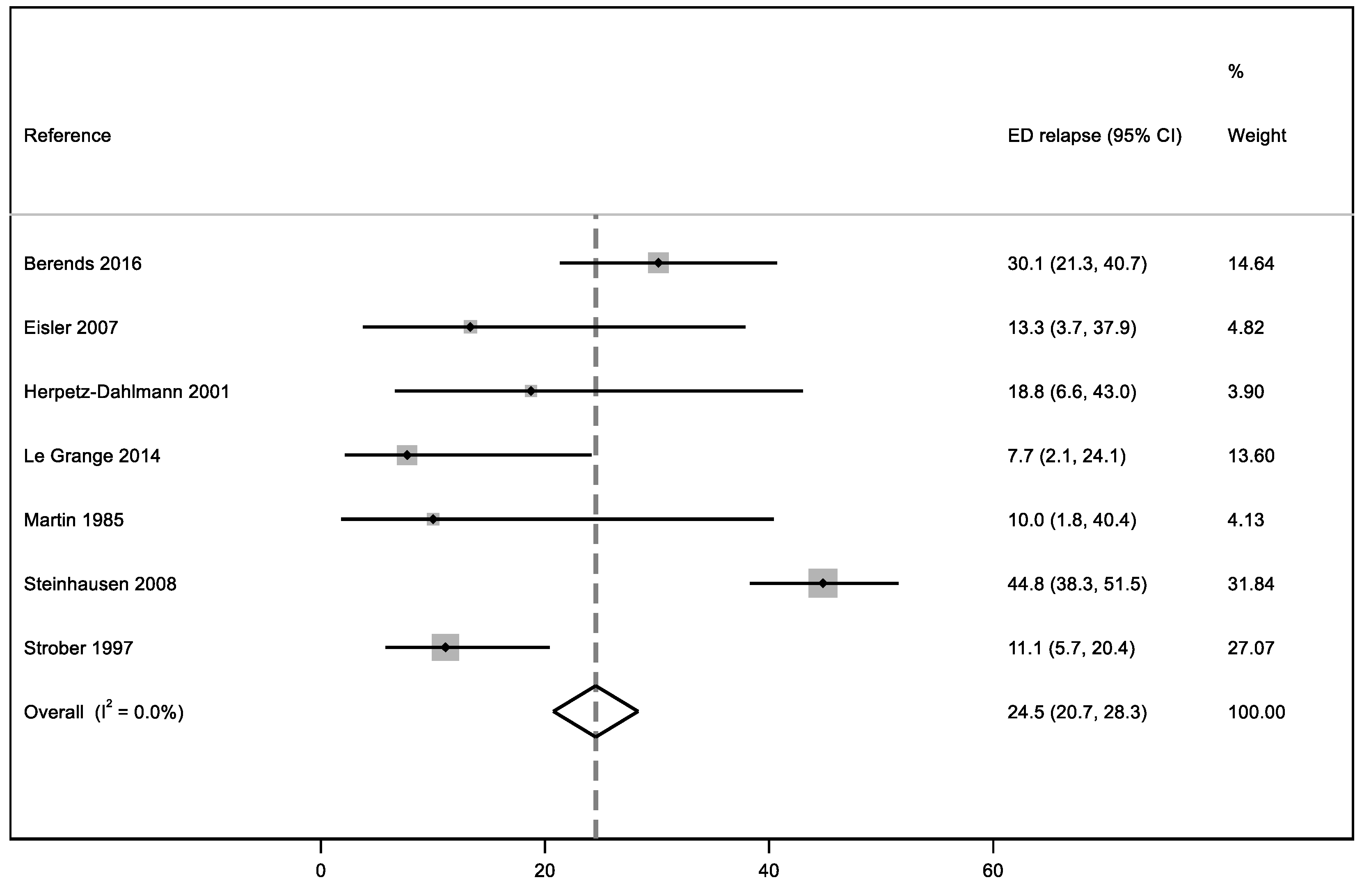
3.6. ED Relapse
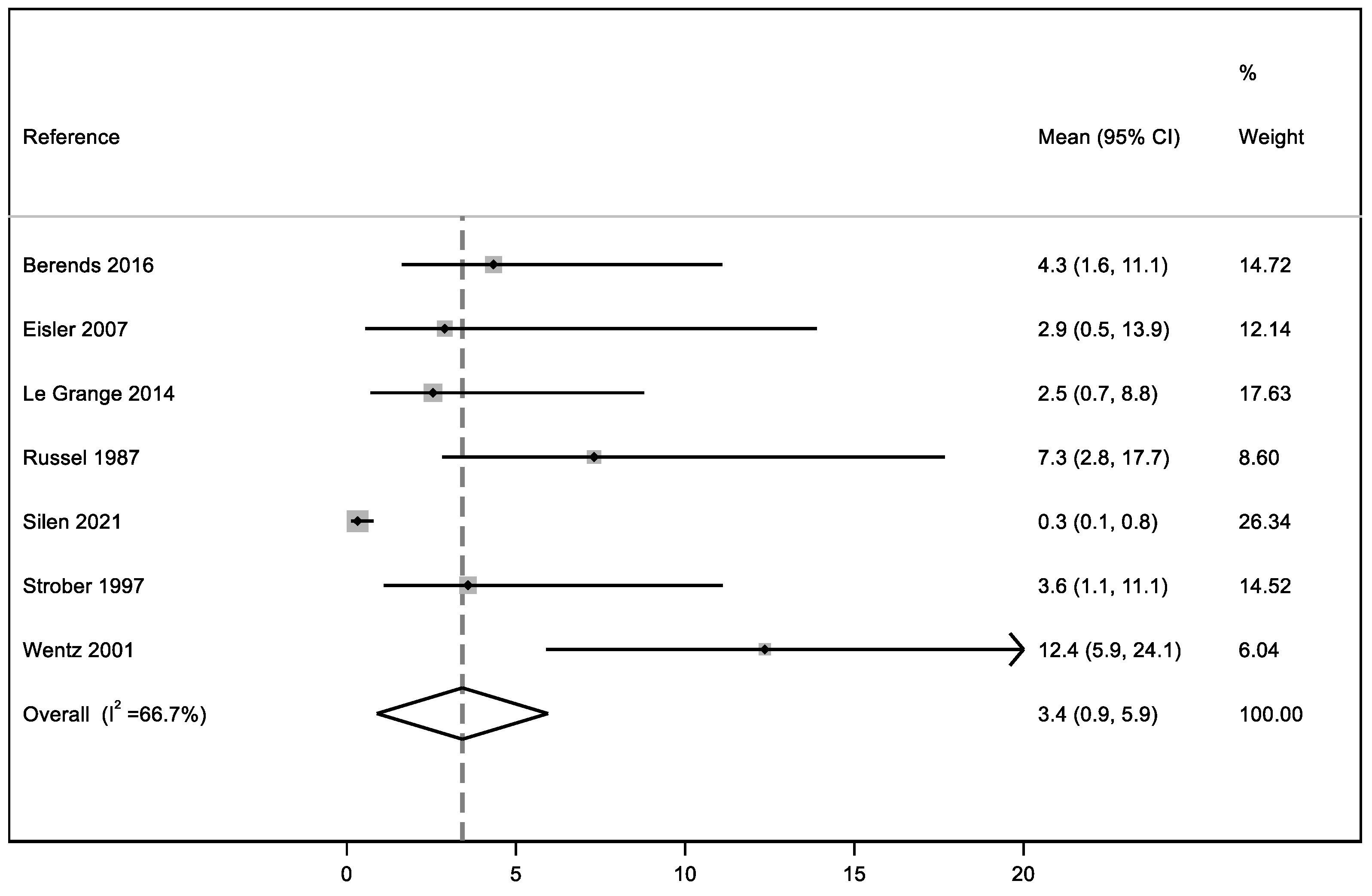
3.7. ED Mean Duration
3.8. Qualitative Outcomes
3.9. Psychiatric Comorbidities
- (1)
- In Gillberg et al. [65], the authors noted an empathy deficit, diagnosed using the Dewey Social Awareness test, usually used to evaluate the presence of Asperger’s Syndrome [78]. Patients with an empathy deficit have difficulty in understanding others’ ideas, thoughts, and feelings and report a feeling of social ineptitude. This deficit was reported in 15 out of 51 individuals, already affected by anorexia nervosa [65].
- (2)
- Le Grange et al. [72], using the DSM-IV (1990), noted mood disorders in 8 of 79 patients and, in the same sample, found that 12 individuals were affected by anxiety disorder.
- (3)
- Martin et al. [67] in 1985 highlighted two comorbidities in 2 patients out of 22: one had a behavior disorder, while the other showed depression symptoms.
- (4)
- Wentz et al. [66] study has the highest number of psychiatric comorbidities: the most common ones were dysthymia, obsessive-compulsive disorder, and anxiety disorder; to a lesser extent, the authors found that patients with EDs suffered from major depression, panic attacks, specific and social phobias, psychotic disorders, somatoform disorders, and tic disorders. One patient also developed substance abuse.
- (5)
- Yao et al. [68], given the large sample size, found many comorbidities. The more common disorders were major depression, anxiety disorder, and substance abuse.
3.10. ED Medical Comorbidities and Death
3.11. ED Social–Relational Complications
3.12. The Quality Studies Assessment
4. Discussion
Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ferguson, C.P.; Pigott, T.A. Anorexia and bulimia nervosa: Neurobiology and pharmacotherapy. Behav. Ther. 2000, 31, 237–263. [Google Scholar] [CrossRef]
- Gull, W. Anorexia nervosa. Lancet 1888, 131, 516–517. [Google Scholar] [CrossRef][Green Version]
- Habermas, T. The psychiatric history of anorexia nervosa and bulimia nervosa: Weight concerns and bulimic symptoms in early case reports. Int. J. Eat. Disord. 1989, 8, 259–273. [Google Scholar] [CrossRef]
- World Health Organization. ICD-10: International Statistical Classification of Diseases and Related Health Problems: Tenth Revision, 2nd ed.; World Health Organization: Geneva, Switzerland, 2004. Available online: https://apps.who.int/iris/handle/10665/42980 (accessed on 19 October 2022).
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: DSM-III; American Psychiatric Association: Washington, DC, USA, 1980. [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: DS-III-R; American Psychiatric Association: Washington, DC, USA, 1987. [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: DSM-IV; American Psychiatric Association: Washington, DC, USA, 1990. [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: DSM-IV-TR; American Psychiatric Association: Washington, DC, USA, 1994. [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: DSM 5; American Psychiatric Association: Washington, DC, USA, 2013. [Google Scholar]
- Call, C.; Walsh, B.T.; Attia, E. From DSM-IV to DSM-5: Changes to eating disorder diagnoses. Curr. Opin. Psychiatry 2013, 26, 532–536. [Google Scholar] [CrossRef] [PubMed]
- Sunday, S.R.; Peterson, C.B.; Andreyka, K.; Crow, S.J.; Mitchell, J.E.; Halmi, K.A. Differences in DSM-III-R and DSM-IV diagnoses in eating disorder patients. Compr. Psychiatry 2001, 42, 448–455. [Google Scholar] [CrossRef]
- Kolar, D.R.; Rodriguez, D.L.; Chams, M.M.; Hoek, H.W. Epidemiology of eating disorders in Latin America: A systematic review and meta-analysis. Curr. Opin. Psychiatry 2016, 29, 363–371. [Google Scholar] [CrossRef]
- Keski-Rahkonen, A.; Mustelin, L. Epidemiology of eating disorders in Europe: Prevalence, incidence, comorbidity, course, consequences, and risk factors. Curr. Opin. Psychiatry 2016, 29, 340–345. [Google Scholar] [CrossRef]
- Istituto Superiore di Sanità, Epicentro. [Anoressia e Bulimia]. 2013. Available online: http://www.epicentro.iss.it/anoressia/epidemiologia (accessed on 19 October 2022).
- Neale, J.; Hudson, L.D. Anorexia nervosa in adolescents. Br. J. Hosp. Med. 2020, 81, 1–8. [Google Scholar] [CrossRef]
- Van Eeden, A.E.; van Hoeken, D.; Hoek, H.W. Incidence, prevalence and mortality of anorexia nervosa and bulimia nervosa. Curr. Opin. Psychiatry 2021, 34, 515–524. [Google Scholar] [CrossRef]
- Berrettini, W. The genetics of eating disorders. Psychiatry 2004, 1, 18–25. [Google Scholar]
- Grice, D.E.; Halmi, K.A.; Fichter, M.M.; Strober, M.; Woodside, D.B.; Treasure, J.T.; Kaplan, A.S.; Magistretti, P.J.; Goldman, D.; Bulik, C.M.; et al. Evidence for a susceptibility gene for anorexia nervosa on chromosome 1. Am. J. Hum. Genet. 2002, 70, 787–792. [Google Scholar] [CrossRef] [PubMed]
- Devlin, B.; Bacanu, S.A.; Klump, K.L.; Bulik, C.M.; Fichter, M.M.; Halmi, K.A.; Kaplan, A.S.; Strober, M.; Treasure, J.; Woodside, D.B.; et al. Linkage analysis of anorexia nervosa incorporating behavioral covariates. Hum. Mol. Genet. 2002, 11, 689–696. [Google Scholar] [CrossRef] [PubMed]
- Kaye, W.H.; Frank, G.K.; McConaha, C. Altered dopamine activity after recovery from restricting-type anorexia nervosa. Neuropsychopharmacology 1999, 21, 503–506. [Google Scholar] [CrossRef] [PubMed]
- Pruccoli, J.; Parmeggiani, A.; Cordelli, D.M.; Lanari, M. The role of the noradrenergic system in eating disorders: A systematic review. Int. J. Mol. Sci. 2021, 22, 11086. [Google Scholar] [CrossRef]
- Nowakowski, M.E.; McFarlane, T.; Cassin, S. Alexithymia and eating disorders: A critical review of the literature. J. Eat. Disord. 2013, 1, 21. [Google Scholar] [CrossRef]
- Nilsson, K.; Engström, I.; Hägglöf, B. Family climate and recovery in adolescent onset eating disorders: A prospective study. Eur. Eat. Disord. Rev. 2012, 20, e96–e102. [Google Scholar] [CrossRef]
- Patel, C.; Karasouli, E.; Shuttlewood, E.; Meyer, C. Food parenting practices among parents with overweight and obesity: A systematic review. Nutrients 2018, 12, 1966. [Google Scholar] [CrossRef]
- Hill, A.J. Causes and consequences of dieting and anorexia. Proc. Nutr. Soc. 1993, 52, 211–218. [Google Scholar] [CrossRef]
- Lev-Ari, L.; Zohar, A.H.; Bachner-Melman, R.; Totah Hanhart, A. Intergenerational transmission of child feeding practices. Int. J. Environ. Res. Public Health 2021, 2, 8183. [Google Scholar] [CrossRef]
- Claydon, E.A.; Lilly, C.L.; Zerwas, S.C.; Zullig, K.J.; Davidov, D.M.; Cottrell, L. An exploratory study on the intergenerational transmission of dieting proneness within an eating disorder population. Eat. Weight Disord. 2020, 25, 1171–1181. [Google Scholar] [CrossRef]
- Golden, N.H.; Schneider, M.; Wood, C. Preventing obesity and eating disorders in adolescents. Pediatrics 2016, 138, e20161649. [Google Scholar] [CrossRef] [PubMed]
- Minuchin, S.; Rosman, B.L.; Baker, L. Psychosomatic Families: Anorexia Nervosa in Context; Harvard University Press: Cambridge, MA, USA; London, UK, 2013. [Google Scholar] [CrossRef]
- Selvini Palazzoli, M. L’Anoressia Mentale. Dalla Terapia Individuale alla Terapia Familiare; Raffaello Cortina Editore: Milan, Italy, 2006. [Google Scholar]
- Russell, G.F.; Szmukler, G.I.; Dare, C.; Eisler, I. An evaluation of family therapy in anorexia nervosa and bulimia nervosa. Arch. Gen. Psychiatry 1987, 44, 1047–1056. [Google Scholar] [CrossRef] [PubMed]
- Treasure, J.; Claudino, A.M.; Zucker, N. Eating disorders. Lancet 2010, 375, 583–593. [Google Scholar] [CrossRef] [PubMed]
- Khalsa, S.S.; Portnoff, L.C.; McCurdy-McKinnon, D.; Feusner, J.D. What happens after treatment? A systematic review of relapse, remission, and recovery in anorexia nervosa. J. Eat. Disord. 2017, 5, 20. [Google Scholar] [CrossRef] [PubMed]
- Morgan, H.G.; Russell, G.F. Value of family background and clinical features as predictors of long-term outcome in anorexia nervosa: Four-year follow-up study of 41 patients. Psychol. Med. 1975, 5, 355–371. [Google Scholar] [CrossRef] [PubMed]
- Löwe, B.; Zipfel, S.; Buchholz, C.; Dupont, Y.; Reas, D.L.; Herzog, W. Long-term outcome of anorexia nervosa in a prospective 21-year follow-up study. Psychol. Med. 2001, 31, 881–890. [Google Scholar] [CrossRef] [PubMed]
- Kordy, H.; Krämer, B.; Palmer, R.L.; Papezova, H.; Pellet, J.; Richard, M.; Treasure, J. Remission, recovery, relapse, and recurrence in eating disorders: Conceptualization and illustration of a validation strategy. J. Clin. Psychol. 2002, 58, 833–846. [Google Scholar] [CrossRef]
- Stice, E.; Telch, C.F.; Rizvi, S.L. Development and validation of the eating disorder diagnostic scale: A brief self-report measure of anorexia, bulimia, and binge-eating disorder. Psychol. Assess. 2000, 12, 123–131. [Google Scholar] [CrossRef]
- Keel, P.K.; Dorer, D.J.; Franko, D.L.; Jackson, S.C.; Herzog, D.B. Postremission predictors of relapse in women with eating disorders. Am. J. Psychiatry 2005, 162, 2263–2268. [Google Scholar] [CrossRef]
- Fichter, M.M.; Quadflieg, N. Six-year course and outcome of anorexia nervosa. Int. J. Eat. Disord. 1999, 26, 359–385. [Google Scholar] [CrossRef]
- Eisler, I.; Simic, M.; Russell, G.F.; Dare, C. A randomised controlled treatment trial of two forms of family therapy in adolescent anorexia nervosa: A five-year follow-up. J. Child Psychol. Psychiatry 2007, 48, 552–560. [Google Scholar] [CrossRef] [PubMed]
- Herzog, D.B.; Dorer, D.J.; Keel, P.K.; Selwyn, S.E.; Ekeblad, E.R.; Flores, A.T.; Greenwood, D.N.; Burwell, R.A.; Keller, M.B. Recovery and relapse in anorexia and bulimia nervosa: A 7.5-year follow-up study. J. Am. Acad. Child Adolesc. Psychiatry 1999, 38, 829–837. [Google Scholar] [CrossRef] [PubMed]
- Helverskov, J.L.; Clausen, L.; Mors, O.; Frydenberg, M.; Thomsen, P.H.; Rokkedal, K. Trans-diagnostic outcome of eating disorders: A 30-month follow-up study of 629 patients. Eur. Eat. Disord. Rev. 2010, 18, 453–463. [Google Scholar] [CrossRef] [PubMed]
- Walsh, B.T.; Kaplan, A.S.; Attia, E.; Olmsted, M.; Parides, M.; Carter, J.C.; Pike, K.M.; Devlin, M.J.; Woodside, B.; Roberto, C.A.; et al. Fluoxetine after weight restoration in anorexia nervosa: A randomized controlled trial. JAMA 2006, 295, 2605–2612. [Google Scholar] [CrossRef]
- Hambleton, A.; Pepin, G.; Le, A.; Maloneym, D.; National Eating Disorder Research Consortium; Touyz, S.; Maguire, S. Psychiatric and medical comorbidities of eating disorders: Findings from a rapid review of the literature. J. Eat. Disord. 2022, 10, 132. [Google Scholar] [CrossRef]
- Micali, N.; Solmi, F.; Horton, N.J.; Crosby, R.D.; Eddy, K.T.; Calzo, J.P.; Sonneville, K.R.; Swanson, S.A.; Field, A.E. Adolescent eating disorders predict psychiatric, high-risk behaviors and weight outcomes in young adulthood. J. Am. Acad. Child Adolesc. Psychiatry 2015, 54, 652–659. [Google Scholar] [CrossRef]
- Ulfvebrand, S.; Birgegård, A.; Norring, C.; Högdahl, L.; von Hausswolff-Juhlin, Y. Psychiatric comorbidity in women and men with eating disorders results from a large clinical database. Psychiatry Res. 2015, 230, 292–299. [Google Scholar] [CrossRef]
- Chen, E.Y.; Brown, M.Z.; Harned, M.S.; Linehan, M.M. A comparison of borderline personality disorder with and without eating disorders. Psychiatry Res. 2009, 170, 86–90. [Google Scholar] [CrossRef]
- Marino, M.F.; Zanarini, M.C. Relationship between EDNOS and its subtypes and borderline personality disorder. Int. J. Eat. Disord. 2001, 29, 349–353. [Google Scholar] [CrossRef]
- Glorio, R.; Allevato, M.; De Pablo, A.; Abbruzzese, M.; Carmona, L.; Savarin, M.; Ibarra, M.; Busso, C.; Mordoh, A.; Llopis, C.; et al. Prevalence of cutaneous manifestations in 200 patients with eating disorders. Int. J. Dermatol. 2000, 39, 348–353. [Google Scholar] [CrossRef]
- Bhanji, S.; Mattingly, D. Acrocyanosis in anorexia nervosa. Postgrad. Med. J. 1991, 67, 33–35. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Kamal, N.; Chami, T.; Andersen, A.; Rosell, F.A.; Schuster, M.M.; Whitehead, W.E. Delayed gastrointestinal transit times in anorexia nervosa and bulimia nervosa. Gastroenterology 1991, 101, 1320–1324. [Google Scholar] [CrossRef] [PubMed]
- McLoughlin, D.M.; Spargo, E.; Wassif, W.S.; Newham, D.J.; Peters, T.J.; Lantos, P.L.; Russell, G.F. Structural and functional changes in skeletal muscle in anorexia nervosa. Acta Neuropathol. 1998, 95, 632–640. [Google Scholar] [CrossRef] [PubMed]
- Rosen, E.; Sabel, A.L.; Brinton, J.T.; Catanach, B.; Gaudiani, J.L.; Mehler, P.S. Liver dysfunction in patients with severe anorexia nervosa. Int. J. Eat. Disord. 2016, 49, 151–158. [Google Scholar] [CrossRef]
- De Simone, G.; Scalfi, L.; Galderisi, M.; Celentano, A.; Di Biase, G.; Tammaro, P.; Garofalo, M.; Mureddu, G.F.; de Divitiis, O.; Contaldo, F. Cardiac abnormalities in young women with anorexia nervosa. Br. Heart J. 1994, 71, 287–292. [Google Scholar] [CrossRef]
- Meyers, D.G.; Starke, H.; Pearson, P.H.; Wilken, M.K.; Ferrell, J.R. Leaflet to left ventricular size disproportion and prolapse of a structurally normal mitral valve in anorexia nervosa. Am. J. Cardiol. 1987, 60, 911–914. [Google Scholar] [CrossRef]
- Brown, N.W. Medical consequences of eating disorders. South Med. J. 1985, 78, 403–405. [Google Scholar] [CrossRef]
- Patel, K.; Tchanturia, K.; Harrison, A. An exploration of social functioning in young people with eating disorders: A qualitative study. PLoS ONE 2016, 26, e0159910. [Google Scholar] [CrossRef]
- Tchanturia, K.; Davies, H.; Harrison, A.; Fox, J.R.; Treasure, J.; Schmidt, U. Altered social hedonic processing in eating disorders. Int. J. Eat. Disord. 2012, 45, 962–969. [Google Scholar] [CrossRef]
- Harrison, A.; Tchanturia, K.; Naumann, U.; Treasure, J. Social emotional functioning and cognitive styles in eating disorders. Br. J. Clin. Psychol. 2012, 51, 261–279. [Google Scholar] [CrossRef]
- Levinson, C.A.; Rodebaugh, T.L. Social anxiety and eating disorder comorbidity: The role of negative social evaluation fears. Eat. Behav. 2012, 13, 27–35. [Google Scholar] [CrossRef] [PubMed]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, 71. [Google Scholar] [CrossRef] [PubMed]
- Lilford, R.J.; Richardson, A.; Stevens, A.; Fitzpatrick, R.; Edwards, S.; Rock, F.; Hutton, J.L. Issues in methodological research: Perspectives from researchers and commissioners. Health Technol. Assess. 2001, 5, 1–57. [Google Scholar] [CrossRef] [PubMed]
- Wells, G.A.; Shea, B.; O’Connell, D.; Peterson, J.; Welch, V.; Losos, M.; Tugwll, P. The Newcastle-Ottawa Scale (NOS) for Assessing the Quality of Non Randomized Studies in Meta-Analyses. Available online: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp (accessed on 19 October 2022).
- Gillberg, I.C.; Råstam, M.; Gillberg, C. Anorexia nervosa outcome: Six-year controlled longitudinal study of 51 cases including a population cohort. J. Am. Acad. Child Adolesc. Psychiatry 1994, 33, 729–739. [Google Scholar] [CrossRef] [PubMed]
- Wentz, E.; Gillberg, C.; Gillberg, I.C.; Rastam, M. Ten-year follow-up of adolescent-onset anorexia nervosa: Psychiatric disorders and overall functioning scales. J. Child Psychol. Psychiatry 2001, 42, 613–622. [Google Scholar] [CrossRef]
- Martin, F.E. The treatment and outcome of anorexia nervosa in adolescents: A prospective study and five year follow-up. J. Psychiatr. Res. 1985, 19, 509–514. [Google Scholar] [CrossRef]
- Yao, S.; Kuja-Halkola, R.; Thornton, L.M.; Runfola, C.D.; D’Onofrio, B.M.; Almqvist, C.; Lichtenstein, P.; Sjölander, A.; Larsson, H.; Bulik, C.M. Familial liability for eating disorders and suicide attempts: Evidence from a population registry in Sweden. JAMA Psychiatry 2016, 73, 284–291. [Google Scholar] [CrossRef]
- Södersten, P.; Brodin, U.; Sjöberg, J.; Zandian, M.; Bergh, C. Treatment outcomes for eating disorders in Sweden: Data from the national quality registry. BMJ Open 2019, 9, e024179. [Google Scholar] [CrossRef]
- Steinhausen, H.C.; Grigoroiu-Serbanescu, M.; Boyadjieva, S.; Neumärker, K.J.; Winkler Metzke, C. Course and predictors of rehospitalization in adolescent anorexia nervosa in a multisite study. Int. J. Eat. Disord. 2008, 41, 29–36. [Google Scholar] [CrossRef]
- Russell, G.F. Premenarchal anorexia nervosa and its sequelae. J. Psychiatr. Res. 1985, 19, 363–369. [Google Scholar] [CrossRef] [PubMed]
- Le Grange, D.; Lock, J.; Accurso, E.C.; Agras, W.S.; Darcy, A.; Forsberg, S.; Bryson, S.W. Relapse from remission at two- to four-year follow-up in two treatments for adolescent anorexia nervosa. J. Am. Acad. Child Adolesc. Psychiatry 2014, 53, 1162–1167. [Google Scholar] [CrossRef] [PubMed]
- Schulze, U.M.; Schuler, S.; Schlamp, D.; Schneider, P.; Mehler-Wex, C. Bone mineral density in partially recovered early onset anorexic patients—A follow-up investigation. Child Adolesc. Psychiatry Ment. Health 2010, 4, 20. [Google Scholar] [CrossRef] [PubMed]
- Silén, Y.; Sipilä, P.N.; Raevuori, A.; Mustelin, L.; Marttunen, M.; Kaprio, J.; Keski-Rahkonen, A. Detection, treatment, and course of eating disorders in Finland: A population-based study of adolescent and young adult females and males. Eur. Eat. Disord Rev. 2021, 29, 720–732. [Google Scholar] [CrossRef]
- Strober, M.; Freeman, R.; Morrell, W. The long-term course of severe anorexia nervosa in adolescents: Survival analysis of recovery, relapse, and outcome predictors over 10–15 years in a prospective study. Int. J. Eat. Disord. 1997, 22, 339–366. [Google Scholar] [CrossRef]
- Berends, T.; van Meijel, B.; Nugteren, W.; Deen, M.; Danner, U.N.; Hoek, H.W.; van Elburg, A.A. Rate, timing and predictors of relapse in patients with anorexia nervosa following a relapse prevention program: A cohort study. BMC Psychiatry 2016, 16, 316. [Google Scholar] [CrossRef]
- Herpertz-Dahlmann, B.; Müller, B.; Herpertz, S.; Heussen, N.; Hebebrand, J.; Remschmidt, H. Prospective 10-year follow-up in adolescent anorexia nervosa—Course, outcome, psychiatric comorbidity, and psychosocial adaptation. J. Child Psychol. Psychiatry 2001, 42, 603–612. [Google Scholar] [CrossRef]
- Dewey, M. Living with Asperger’s syndrome. In Autism and Asperger Syndrome; Frith, U., Ed.; Cambridge University Press: Cambridge, MA, USA, 1991; pp. 184–206. [Google Scholar] [CrossRef]
- Eddy, K.T.; Tabri, N.; Thomas, J.J.; Murray, H.B.; Keshaviah, A.; Hastings, E.; Edkins, K.; Krishna, M.; Herzog, D.B.; Keel, P.K.; et al. Recovery from anorexia nervosa and bulimia nervosa at 22-year follow-up. J. Clin. Psychiatry 2017, 78, 184–189. [Google Scholar] [CrossRef]
- Bodell, L.P.; Mayer, L.E. Percent body fat is a risk factor for relapse in anorexia nervosa: A replication study. Int. J. Eat. Disord. 2011, 44, 118–123. [Google Scholar] [CrossRef]
- Carter, J.C.; Mercer-Lynn, K.B.; Norwood, S.J.; Bewell-Weiss, C.V.; Crosby, R.D.; Woodside, D.B.; Olmsted, M.P. A prospective study of predictors of relapse in anorexia nervosa: Implications for relapse prevention. Psychiatry Res. 2012, 200, 518–523. [Google Scholar] [CrossRef]
- Dawson, L.; Rhodes, P.; Touyz, S. “Doing the impossible”: The process of recovery from chronic anorexia nervosa. Qual. Health Res. 2014, 24, 494–505. [Google Scholar] [CrossRef] [PubMed]
- Dawson, L.; Rhodes, P.; Touyz, S. The recovery model and anorexia nervosa. Aust. N. Z. J. Psychiatry 2014, 48, 1009–1016. [Google Scholar] [CrossRef] [PubMed]
- Gibson, D.; Workman, C.; Mehler, P.S. Medical complications of anorexia nervosa and bulimia nervosa. Psychiatr. Clin. N. Am. 2019, 42, 263–274. [Google Scholar] [CrossRef] [PubMed]
- Le Grange, D.; Lock, J.; Loeb, K.; Nicholls, D. Academy for eating disorders position paper: The role of the family in eating disorders. Int. J. Eat. Disord. 2010, 43, 1–5. [Google Scholar] [CrossRef] [PubMed]
- Miranda-Olivos, R.; Testa, G.; Lucas, I.; Sánchez, I.; Sánchez-González, J.; Granero, R.; Jiménez-Murcia, S.; Fernández-Aranda, F. Clinical factors predicting impaired executive functions in eating disorders: The role of illness duration. J. Psychiatr. Res. 2021, 144, 87–95. [Google Scholar] [CrossRef]
- Claydon, E.A.; De Fazio, C.; Lilly, C.L.; Zullig, K.J. Life satisfaction among a clinical eating disorder population. J. Eat. Disord. 2020, 8, 53. [Google Scholar] [CrossRef]
- Gorrell, S.; Murray, S.B. Eating disorders in males. Child Adolesc. Psychiatr. Clin. N. Am. 2019, 28, 641–651. [Google Scholar] [CrossRef]

| Reference Year, Country | Study Design | Follow-Up (Years) | ED Mean Duration (Years) | Sample at Baseline (N) | Sample at Follow-Up (N) | Females N (%) | Age at Baseline (Years): Mean (SD) | BMI at Baseline and End of Follow-Up | ED Subtype N (%) |
|---|---|---|---|---|---|---|---|---|---|
| Berends et al. [76], 2016, The Netherlands | Cohort | 1.5 | 3.6 | 83 | 83 | 83 (100) | 17.9 (4.45) | Start: 16.3/16.4 a End: 19.9/20.4 a | 70 = AN-R (84.3) 13 = AN-BP (15.7) |
| Eisler et al. [40], 2007, UK | RCT follow-up | 5 | 1.1 | 38 | 38 | 40 (100) | 14 (1.6) | Start: 15.4 End: 19.8 | 40 = AN (100) |
| Gillberg et al. [65], 1994, Sweden | Case–control | 5 | NR | 51 | 51 | 48 (94) | 14.3 (13.9–14.7) b | Start: 18.3 End:21.2 | 51 = AN (100) |
| Herpertz-Dahlmann et al. [77], 2001, Germany | Cohort | 3–7 | NR | 44 | 39 | 35 (90) | 14.9 (1.6) | Start: 14.3/15.7 c End: 20.2/24.6 c | 39 = AN (100) |
| Le Grange et al. [72], 2014, USA | Cohort | 3.26 | 2 | 121 | 79 | 110 (91) | 14.7 (1.6) | NR | 72 = AN (91.1) 2 = BN (2.5) 5 = EDONOS (6.%) |
| Martin et al. [67], 1985, Canada | Cohort | 5.1 | NR | 25 | 22 | 22 (88) | 14.9 (2.12) | NR | 18 = AN (72) 7 = BN (28) |
| Nilsson et al. [23], 2012, Sweden | Cohort | 3 | NR | 165 | 102 | 102 (100) | 15.86 (1.37) | Start: 18.1 End: NR | 44 = AN (43) 12 = BN (12) 46 = EDNOS (45) |
| Russell et al. [71], 1985, UK | Cohort | 9.5 | NR | 22 | 20 | 20 (100) | 12.25 | NR | 17 = AN (85) 3 = BN (15) |
| Russell et al. [31], 1987, UK | Cohort | 1 | 3.8 | 80 | 52 | 73 (91) | 17.9 (6.4) | NR | 57 = AN (71) 23 = BN (29) |
| Schulze et al. [73], 2010, Germany | Cohort | 5.23 | NR | 52 | 52 | 52 (100) | 15.5 (2.07) | Start: 14.74 End: 20.13 | 52 = AN (100) |
| Silèn et al. [74], 2021, Finland | Cohort | 5 | 4.3 | 142 | 142 | 127 (89) | 16.5 (2.9) | NR | 46 = AN (31) 18 = BN (13) 6 = BE (4) 32 = OSFED (23) 42 = NS (30) |
| Södersten et al. [69], 2018, Sweden | Cohort | 5 | NR | 12,854 | 5867 | 12,211 (95.4) | 23.1 (8.9) | NR | 3279 = AN (26) 3219 = BN (25) 3414 = BE (27) 2225 = OSFED (17) 717 = Others (7) |
| Steinhausen et al. [70], 2008, Switzerland | Cohort | 8.3 | NR | 212 | 212 | 201 (95) | 14.8 (1.7) | Start: 13.9 End: NR | 212 = AN (100) |
| Strober et al. [75], 1997, USA | Cohort | 12.5 | 2.4 | 95 | 95 | 85 (89.5) | Range: 12–17 | Start: 14.1 End: NR | 18 = AN-BP (18.9) 77 = AN-R (81.1) |
| Wentz et al. [66], 2001, Sweden | Case–control | 10 | 10.2 | 88 | 51 | 48 (94) | AN: 13 (3) BN: 14 (6) | NR | 37 = AN (73) 6 = BN (12) 8 = OSFED (16) |
| Yao et al. [68], 2016, Sweden | Cohort | 30 | NR | 16,448 | 16,448 | 15,457 (94) | 18.4 (4.0) | NR | 8133 = AN (49) 3410 = BN (21) 4945 = Others (30) |
| Reference, Year | Psychiatric Comorbidities N (%) | Substance Use N (%) | Medical Comorbidities N (%) | Social–Relational Complications N (%) | Deaths N (%) |
|---|---|---|---|---|---|
| Gillberg et al. [65], 1994 | 17 (33%) Empathy Deficit | NR | 4 (8%) Amenorrhea, Malnutrition | 17 (34%) Social issues out of family 9 (18%) Family emancipation issues | NR |
| Le Grange et al. [72], 2014 | 8 (10%) Affective Disorders 2 (15%) Anxiety Disorders | NR | NR | NR | NR |
| Martin et al. [67], 1985 | 1 (4%) Behavior disorders 1 (4%) Depressive symptoms | NR | NR | NR | NR |
| Schulze et al. [73], 2010 | NR | NR | 26 (50%) Amenorrhea 6 (11.5%) Osteopenia | NR | 2 (2%) |
| Wentz et al. [66], 2001 | 27 (53%) Major Depressive Episode 3 (6%) Bipolar Disorder 19 (37%): Dysthymia 2 (4%) Panic Attack 7 (14%) Specific Phobia 3 (6%) Social Phobia 18 (35%) Obsessive-compulsive Disorder 11 (21.5%) Generalized Anxiety Disorder 4 (8%) Psychotic Disorders 2 (4%) Somatoform Disorder | 1 (2%) Substance use | 7 (14%) Tic Disorders 6 (12%) Malnutrition 24 (50% of female sample) Amenorrhea | 31 (61%) Social issues 18 (35%) Work issues | NR |
| Yao et al. [68], 2016 | 5247 (31.9%) Major Depressive Episode 3742 (22.8%) Anxiety Disorders | 1731 (10.5%) Substance use | NR | NR | 48 (0.29%) |
| Cohort Studies | Selection | Comparability | Outcome | Total |
|---|---|---|---|---|
| Berends et al. [76], 2016 | 3 | 1 | 3 | 7 |
| Eisler t al [40], 2007 | 4 | 2 | 3 | 9 |
| Herpertz-Dahlmann et al. [77], 2001 | 3 | 2 | 3 | 8 |
| Le Grange et al. [72], 2014 | 3 | 1 | 3 | 7 |
| Martin et al. [67], 1985 | 3 | 1 | 3 | 7 |
| Nilsson et al. [23], 2011 | 2 | 2 | 3 | 7 |
| Russell et al. [71], 1985 | 3 | 1 | 3 | 7 |
| Russell et al. [31], 1987 | 3 | 2 | 3 | 8 |
| Schulze et al. [73], 2010 | 3 | 2 | 3 | 8 |
| Silèn et al. [74], 2021 | 3 | 2 | 3 | 8 |
| Södersten et al. [69], 2018 | 2 | 1 | 1 | 4 |
| Steinhausen et al. [70], 2008 | 3 | 2 | 2 | 7 |
| Strober et al. [75], 1997 | 3 | 2 | 2 | 7 |
| Yao et al. [68], 2016 | 4 | 2 | 3 | 9 |
| Case–Control Studies | Selection | Comparability | Exposure | Total |
| Gillberg et al. [65], 1994 | 3 | 1 | 3 | 7 |
| Wentz et al. [66], 2001 | 3 | 1 | 3 | 7 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Filipponi, C.; Visentini, C.; Filippini, T.; Cutino, A.; Ferri, P.; Rovesti, S.; Latella, E.; Di Lorenzo, R. The Follow-Up of Eating Disorders from Adolescence to Early Adulthood: A Systematic Review. Int. J. Environ. Res. Public Health 2022, 19, 16237. https://doi.org/10.3390/ijerph192316237
Filipponi C, Visentini C, Filippini T, Cutino A, Ferri P, Rovesti S, Latella E, Di Lorenzo R. The Follow-Up of Eating Disorders from Adolescence to Early Adulthood: A Systematic Review. International Journal of Environmental Research and Public Health. 2022; 19(23):16237. https://doi.org/10.3390/ijerph192316237
Chicago/Turabian StyleFilipponi, Caterina, Chiara Visentini, Tommaso Filippini, Anna Cutino, Paola Ferri, Sergio Rovesti, Emanuela Latella, and Rosaria Di Lorenzo. 2022. "The Follow-Up of Eating Disorders from Adolescence to Early Adulthood: A Systematic Review" International Journal of Environmental Research and Public Health 19, no. 23: 16237. https://doi.org/10.3390/ijerph192316237
APA StyleFilipponi, C., Visentini, C., Filippini, T., Cutino, A., Ferri, P., Rovesti, S., Latella, E., & Di Lorenzo, R. (2022). The Follow-Up of Eating Disorders from Adolescence to Early Adulthood: A Systematic Review. International Journal of Environmental Research and Public Health, 19(23), 16237. https://doi.org/10.3390/ijerph192316237