Smoking Has No Influence on Outcomes after Repair of the Medial Meniscus in the Hypo and Avascular Zones—A Pilot Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Patients Selection and Preoperative Assessment
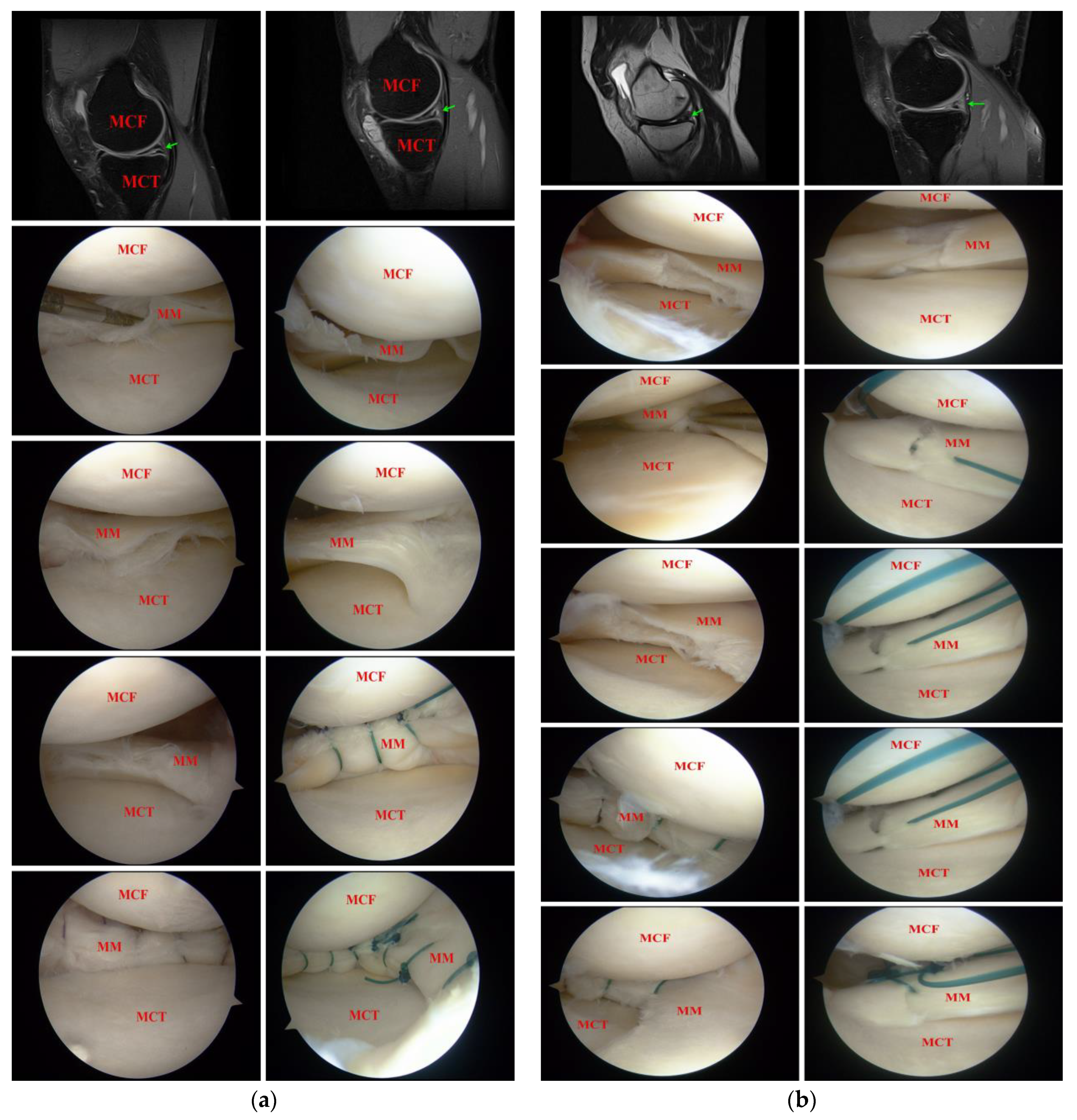
2.2. Surgical Treatment
2.3. Rehabilitation Protocol
2.4. Outcomes Assessment
2.5. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Mordecai, S.C. Treatment of Meniscal Tears: An Evidence Based Approach. WJO 2014, 5, 233. [Google Scholar] [CrossRef] [PubMed]
- Weber, J.; Koch, M.; Angele, P.; Zellner, J. The Role of Meniscal Repair for Prevention of Early Onset of Osteoarthritis. J. Exp. Ortop. 2018, 5, 10. [Google Scholar] [CrossRef] [PubMed]
- Doral, M.N.; Bilge, O.; Huri, G.; Turhan, E.; Verdonk, R. Modern Treatment of Meniscal Tears. Efort Open Rev. 2018, 3, 260–268. [Google Scholar] [CrossRef] [PubMed]
- Bryceland, J.K.; Powell, A.J.; Nunn, T. Knee Menisci: Structure, Function, and Management of Pathology. Cartilage 2017, 8, 99–104. [Google Scholar] [CrossRef] [PubMed]
- Lamplot, J.D.; Tompkins, W.P.; Friedman, M.V.; Nguyen, J.T.; Rai, M.F.; Brophy, R.H. Radiographic and Clinical Evidence for Osteoarthritis at Medium-Term Follow-up after Arthroscopic Partial Medial Meniscectomy. Cartilage 2019, 13, 588S–594S. [Google Scholar] [CrossRef]
- Xu, C.; Zhao, J. A Meta-Analysis Comparing Meniscal Repair with Meniscectomy in the Treatment of Meniscal Tears: The More Meniscus, the Better Outcome? Knee Surg. Sport. Traumatol. Arthrosc. 2015, 23, 164–170. [Google Scholar] [CrossRef]
- Saltzman, B.M.; Cotter, E.J.; Wang, K.C.; Rice, R.; Manning, B.T.; Yanke, A.B.; Forsythe, B.; Verma, N.N.; Cole, B.J. Arthroscopically Repaired Bucket-Handle Meniscus Tears: Patient Demographics, Postoperative Outcomes, and a Comparison of Success and Failure Cases. Cartilage 2020, 11, 77–87. [Google Scholar] [CrossRef]
- D’Ambrosi, R.; Meena, A.; Raj, A.; Ursino, N.; Mangiavini, L.; Herbort, M.; Fink, C. In Elite Athletes with Meniscal Injuries, Always Repair the Lateral, Think about the Medial! A Systematic Review. Knee Surg. Sport. Traumatol. Arthrosc. 2022. [Google Scholar] [CrossRef]
- Adams, B.G.; Houston, M.N.; Cameron, K.L. The Epidemiology of Meniscus Injury. Sport. Med. Arthrosc. Rev. 2021, 29, e24–e33. [Google Scholar] [CrossRef]
- McDermott, I.D.; Amis, A.A. The Consequences of Meniscectomy. J. Bone Jt. Surg. 2006, 88, 1549–1556. [Google Scholar] [CrossRef]
- Snoeker, B.A.M.; Bakker, E.W.P.; Kegel, C.A.T.; Lucas, C. Risk Factors for Meniscal Tears: A Systematic Review Including Meta-Analysis. J. Orthop. Sport. Phys. Ther. 2013, 43, 352–367. [Google Scholar] [CrossRef] [PubMed]
- Mehl, J.; Otto, A.; Baldino, J.B.; Achtnich, A.; Akoto, R.; Imhoff, A.B.; Scheffler, S.; Petersen, W. The ACL-Deficient Knee and the Prevalence of Meniscus and Cartilage Lesions: A Systematic Review and Meta-Analysis (CRD42017076897). Arch. Orthop. Trauma Surg. 2019, 139, 819–841. [Google Scholar] [CrossRef] [PubMed]
- Blackwell, R.; Schmitt, L.; Flanigan, D.C.; Magnussen, R.A. Smoking Increases the Risk of Early Meniscus Repair Failure. Orthop. J. Sport. Med. 2014, 2, 2325967114S0011. [Google Scholar] [CrossRef]
- Crema, M.D.; Guermazi, A.; Li, L.; Nogueira-Barbosa, M.H.; Marra, M.D.; Roemer, F.W.; Eckstein, F.; Hellio Le Graverand, M.P.; Wyman, B.T.; Hunter, D.J. The Association of Prevalent Medial Meniscal Pathology with Cartilage Loss in the Medial Tibiofemoral Compartment over a 2-Year Period. Osteoarthr. Cartil. 2010, 18, 336–343. [Google Scholar] [CrossRef] [PubMed]
- Ying, X.; Cheng, S.; Shen, Y.; Cheng, X.; Rompis, F.A.; Wang, W.; Lin, Z.; Chen, Q.; Zhang, W.; Kou, D.; et al. Nicotine Promotes Proliferation and Collagen Synthesis of Chondrocytes Isolated from Normal Human and Osteoarthritis Patients. Mol. Cell. Biochem. 2012, 359, 263–269. [Google Scholar] [CrossRef]
- Blyth, M.; Anthony, I.; Francq, B.; Brooksbank, K.; Downie, P.; Powell, A.; Jones, B.; MacLean, A.; McConnachie, A.; Norrie, J. Diagnostic Accuracy of the Thessaly Test, Standardised Clinical History and Other Clinical Examination Tests (Apley’s, McMurray’s and Joint Line Tenderness) for Meniscal Tears in Comparison with Magnetic Resonance Imaging Diagnosis. Health Technol. Assess. 2015, 19, 1–62. [Google Scholar] [CrossRef]
- Cinque, M.E.; DePhillipo, N.N.; Moatshe, G.; Chahla, J.; Kennedy, M.I.; Dornan, G.J.; LaPrade, R.F. Clinical Outcomes of Inside-Out Meniscal Repair According to Anatomic Zone of the Meniscal Tear. Orthop. J. Sport. Med. 2019, 7, 232596711986080. [Google Scholar] [CrossRef]
- Barber-Westin, S.D.; Noyes, F.R. Clinical Healing Rates of Meniscus Repairs of Tears in the Central-Third (Red-White) Zone. Arthrosc. J. Arthrosc. Relat. Surg. 2014, 30, 134–146. [Google Scholar] [CrossRef]
- AL-Bashaireh, A.M.; Haddad, L.G.; Weaver, M.; Kelly, D.L.; Chengguo, X.; Yoon, S. The Effect of Tobacco Smoking on Musculoskeletal Health: A Systematic Review. J. Environ. Public Health 2018, 2018, 4184190. [Google Scholar] [CrossRef]
- Laurendon, L.; Neri, T.; Farizon, F.; Philippot, R. Prognostic Factors for All-inside Meniscal Repair. A 87-Case Series. Orthop. Traumatol. Surg. Res. 2017, 103, 1017–1020. [Google Scholar] [CrossRef]
- Cox, C.L.; Huston, L.J.; Dunn, W.R.; Reinke, E.K.; Nwosu, S.K.; Parker, R.D.; Wright, R.W.; Kaeding, C.C.; Marx, R.G.; Amendola, A.; et al. Are Articular Cartilage Lesions and Meniscus Tears Predictive of IKDC, KOOS, and Marx Activity Level Outcomes After Anterior Cruciate Ligament Reconstruction?: A 6-Year Multicenter Cohort Study. Am. J. Sport. Med. 2014, 42, 1058–1067. [Google Scholar] [CrossRef] [PubMed]
- Uzun, E.; Misir, A.; Kizkapan, T.B.; Ozcamdalli, M.; Akkurt, S.; Guney, A. Factors Affecting the Outcomes of Arthroscopically Repaired Traumatic Vertical Longitudinal Medial Meniscal Tears. Orthop. J. Sport. Med. 2017, 5, 232596711771244. [Google Scholar] [CrossRef] [PubMed]
- Webster, K.E.; Feller, J.A.; Kimp, A.; Devitt, B.M. Medial Meniscal and Chondral Pathology at the Time of Revision Anterior Cruciate Ligament Reconstruction Results in Inferior Mid-Term Patient-Reported Outcomes. Knee Surg. Sport. Traumatol. Arthrosc. 2018, 26, 1059–1064. [Google Scholar] [CrossRef] [PubMed]
| Variables | Total | Smokers | Non-Smokers |
|---|---|---|---|
| Population | n = 50 | n = 17 | n = 33 |
| Mean age (years) | 41.68 ± 12.23 | 42.05 ± 13.03 | 41.48 ± 12.01 |
| Gender | |||
| Male | 32 | 12 | 20 |
| Female | 18 | 5 | 13 |
| Mean duration of smoking (years) | - | 7.47 ± 4.96 | - |
| Mean number of cigarettes per day | - | 11.29 ± 8.19 | - |
| Pack-years index | - | 4.9 ± 5.25 | - |
| LKSS preop. | 62.62 ± 18.63 | 54.88 ± 21.63 | 66.6 ± 15.79 |
| LKSS 3 m. postop. | 84.14 ± 10.12 | 84.76 ± 10.07 | 83.81 ± 10.29 |
| LKSS 6 m. postop. | 90.16 ± 8 | 88.58 ± 8.84 | 90.96 ± 7.54 |
| IKDC preop. | 47.31 ± 16.93 | 44.01 ± 17.99 | 49.01 ± 16.38 |
| IKDC 3 m. postop. | 71.5 ± 12.65 | 73.38 ± 10.52 | 70.53 ± 13.67 |
| IKDC 6 m. postop. | 80.8 ± 12.19 | 81.73 ± 12.88 | 81.18 ± 12.01 |
| Smokers | Non-Smokers | p Value * | |
|---|---|---|---|
| Age | |||
| <45 | 10 | 22 | 0.8132 |
| >45 | 7 | 11 | |
| Tear Morphology | |||
| Simple | 6 | 17 | 0.4291 |
| Complex | 11 | 16 | |
| No. of Sutures | |||
| ≤2 | 5 | 7 | 0.7691 |
| >2 | 12 | 26 | |
| LKSS 6 m. | |||
| <83 | 3 | 6 | 0.7324 |
| ≥83 | 14 | 27 | |
| IKDC 6 m. | |||
| <83 | 11 | 16 | 0.4291 |
| ≥83 | 6 | 17 | |
| Cartilage defect | |||
| No defect | 12 | 30 | 0.1472 |
| Defect present | 5 | 3 |
 0–9 patients;
0–9 patients;  10–19 patients;
10–19 patients;  20–29 patients;
20–29 patients;  ≥30 patients.
≥30 patients.| LKSS Preop. | LKSS 3 m. Postop. | LKSS 6 m. Postop. | IKDC Preop. | IKDC 3 m. Postop. | IKDC 6 m. Postop. | |
|---|---|---|---|---|---|---|
| Smoking-years | 0.1524 | 0.4946 | 0.7230 | 0.2003 | 0.7792 | 0.8711 |
| No. of cigarettes | 0.1079 | 0.4360 | 0.6058 | 0.4488 | 0.6409 | 0.7489 |
| Pack-year index | 0.1458 | 0.4326 | 0.6600 | 0.3421 | 0.7333 | 0.8058 |
| Age | 0.0987 | 0.7985 | 0.9918 | 0.1468 | 0.3733 | 0.1027 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zabrzyński, J.; Paczesny, Ł.; Zabrzyńska, A.; Huri, G.; Graboń, K.; Pielak, T.; Kruczyński, J.; Łapaj, Ł. Smoking Has No Influence on Outcomes after Repair of the Medial Meniscus in the Hypo and Avascular Zones—A Pilot Study. Int. J. Environ. Res. Public Health 2022, 19, 16127. https://doi.org/10.3390/ijerph192316127
Zabrzyński J, Paczesny Ł, Zabrzyńska A, Huri G, Graboń K, Pielak T, Kruczyński J, Łapaj Ł. Smoking Has No Influence on Outcomes after Repair of the Medial Meniscus in the Hypo and Avascular Zones—A Pilot Study. International Journal of Environmental Research and Public Health. 2022; 19(23):16127. https://doi.org/10.3390/ijerph192316127
Chicago/Turabian StyleZabrzyński, Jan, Łukasz Paczesny, Agnieszka Zabrzyńska, Gazi Huri, Kamil Graboń, Tomasz Pielak, Jacek Kruczyński, and Łukasz Łapaj. 2022. "Smoking Has No Influence on Outcomes after Repair of the Medial Meniscus in the Hypo and Avascular Zones—A Pilot Study" International Journal of Environmental Research and Public Health 19, no. 23: 16127. https://doi.org/10.3390/ijerph192316127
APA StyleZabrzyński, J., Paczesny, Ł., Zabrzyńska, A., Huri, G., Graboń, K., Pielak, T., Kruczyński, J., & Łapaj, Ł. (2022). Smoking Has No Influence on Outcomes after Repair of the Medial Meniscus in the Hypo and Avascular Zones—A Pilot Study. International Journal of Environmental Research and Public Health, 19(23), 16127. https://doi.org/10.3390/ijerph192316127







