Health Services Utilization in China during the COVID-19 Pandemic: Results from a Large-Scale Online Survey
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Data Collection
2.3. Statistical Analysis
3. Results
3.1. Characteristics of the Study Population
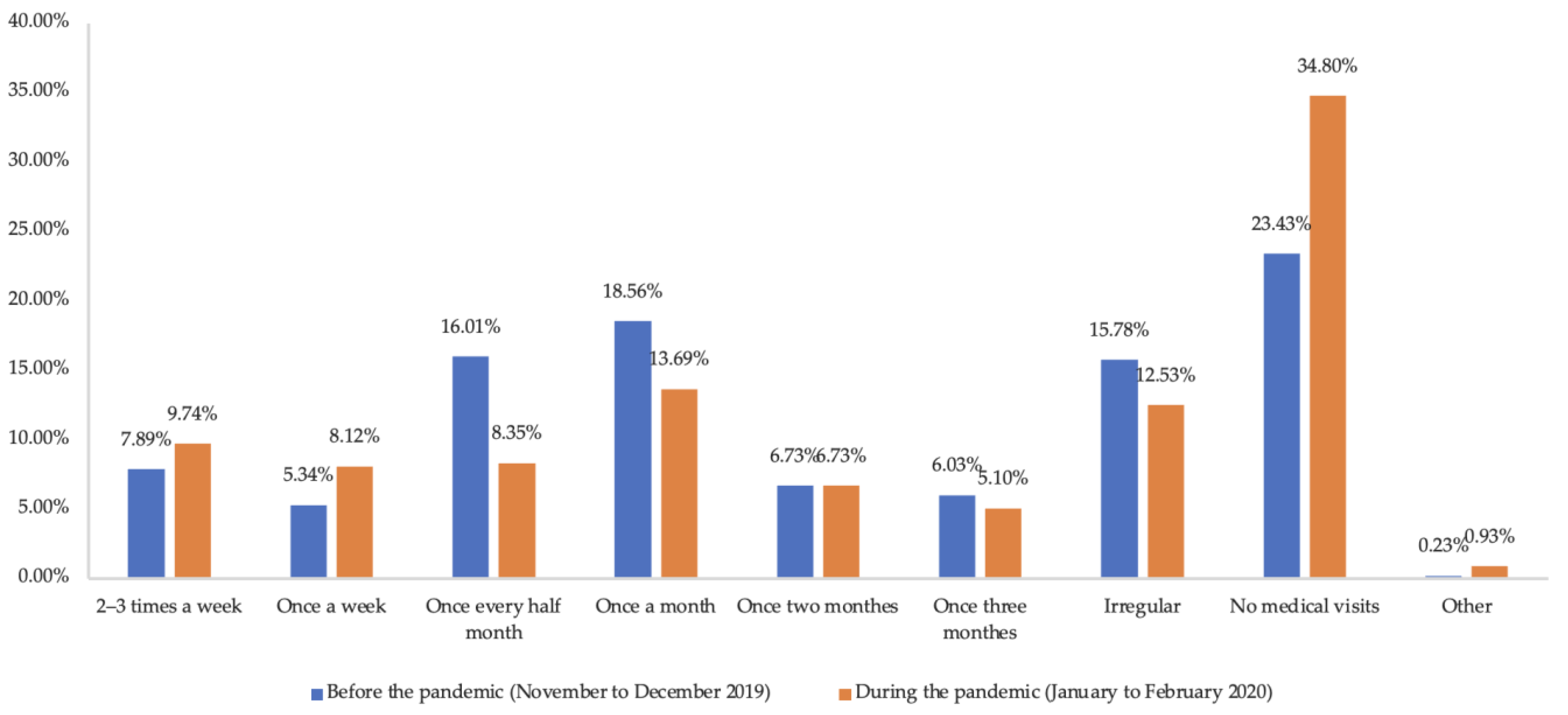
3.2. Patterns of Health Services Utilization and Related Factors
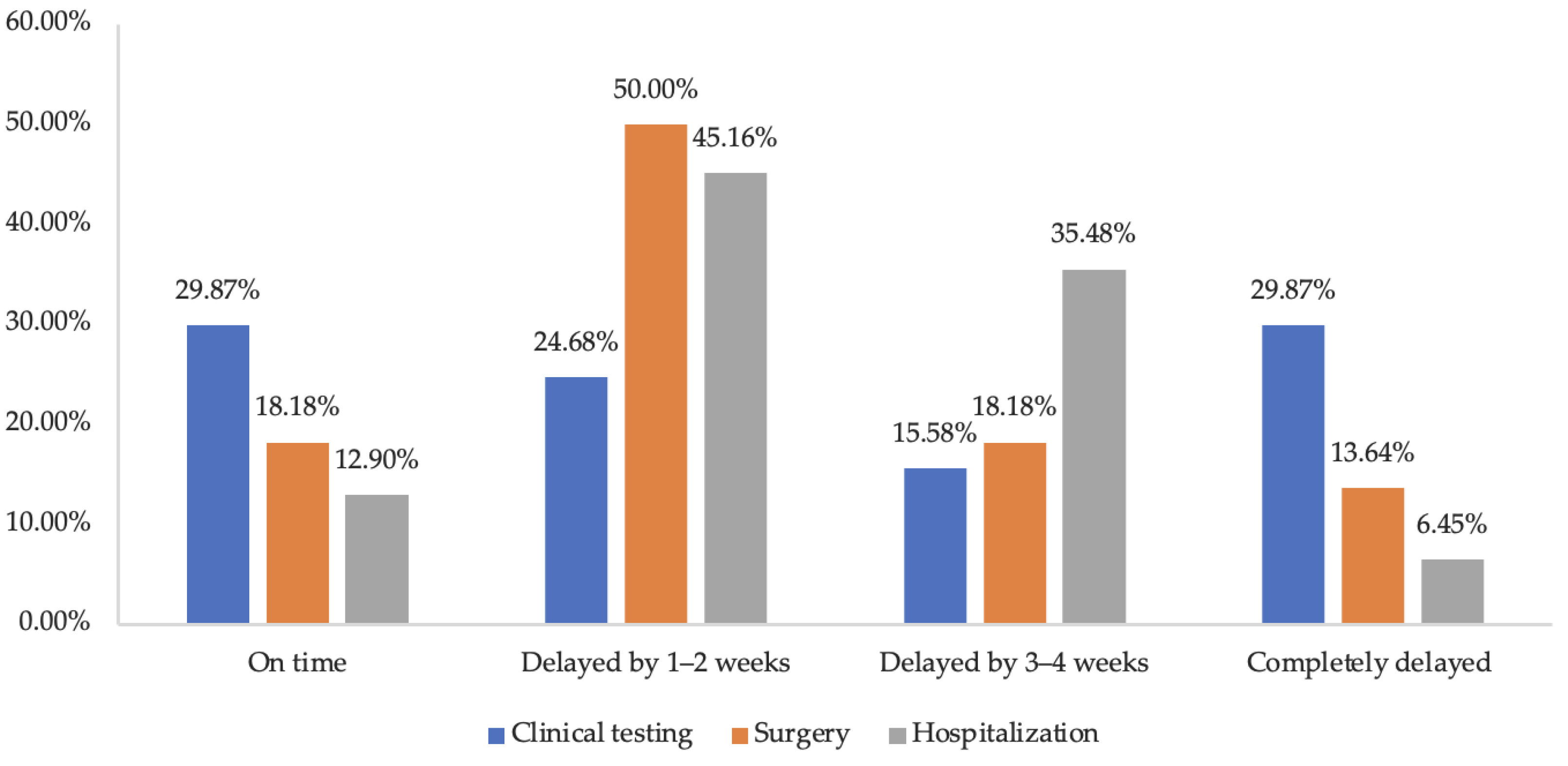
3.3. Health Services Utilization among Respondents with Chronic Diseases
4. Discussion
4.1. Findings
4.2. Interpretation
4.3. Strengths and Weaknesses
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Khan, S.; Ali, A.; Shi, H.; Siddique, R.; Shabana; Nabi, G.; Hu, J.; Wang, T.; Dong, M.; Zaman, W.; et al. COVID-19: Clinical aspects and therapeutics responses. Saudi Pharm. J. 2020, 28, 1004–1008. [Google Scholar] [CrossRef] [PubMed]
- He, X.; Hong, W.; Pan, X.; Lu, G.; Wei, X. SARS-CoV-2 Omicron variant: Characteristics and prevention. MedComm 2021, 2, 838–845. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. WHO Coronavirus (COVID-19) Dashboard. Available online: https://covid19.who.int (accessed on 14 October 2022).
- National Health Commission of the People’s Republic of China. The Latest Report of the COVID-19 Pandemic in China. Available online: http://www.nhc.gov.cn/xcs/yqtb/202210/4cae2dec1b394c5e8077b95bac3bdf1c.shtml (accessed on 14 October 2022).
- Zanin, M.; Xiao, C.; Liang, T.; Ling, S.; Zhao, F.; Huang, Z.; Lin, F.; Lin, X.; Jiang, Z.; Wong, S.-S. The public health response to the COVID-19 outbreak in mainland China: A narrative review. J. Thorac. Dis. 2020, 12, 4434–4449. [Google Scholar] [CrossRef] [PubMed]
- Qiu, Y.; Huang, J.; Sun, J.; Zhao, J.; Chen, A.; Chen, J.; Wu, R.; Li, S.; Teng, Z.; Tan, Y.; et al. Prevalence of Risk Factors Associated With Mental Health Symptoms Among the Outpatient Psychiatric Patients and Their Family Members in China During the Coronavirus Disease 2019 Pandemic. Front. Psychol. 2021, 12, 622339. [Google Scholar] [CrossRef]
- Hung, K.K.; Walline, J.H.; Chan, E.Y.Y.; Huang, Z.; Lo, E.S.K.; Yeoh, E.K.; Graham, C.A. Health Service Utilization in Hong Kong During the COVID-19 Pandemic—A Cross-sectional Public Survey. Int. J. Health Policy Manag. 2020, 11, 508–513. [Google Scholar] [CrossRef] [PubMed]
- Lazzerini, M.; Barbi, E.; Apicella, A.; Marchetti, F.; Cardinale, F.; Trobia, G. Delayed access or provision of care in Italy resulting from fear of COVID-19. Lancet Child Adolesc. Health 2020, 4, e10–e11. [Google Scholar] [CrossRef]
- De Rosa, S.; Spaccarotella, C.; Basso, C.; Calabrò, M.P.; Curcio, A.; Filardi, P.P.; Mancone, M.; Mercuro, G.; Muscoli, S.; Nodari, S.; et al. Reduction of hospitalizations for myocardial infarction in Italy in the COVID-19 era. Eur. Heart J. 2020, 41, 2083–2088. [Google Scholar] [CrossRef]
- Wright, A.; Salazar, A.; Mirica, M.; Volk, L.A.; Schiff, G.D. The Invisible Epidemic: Neglected Chronic Disease Management During COVID-19. J. Gen. Intern. Med. 2020, 35, 2816–2817. [Google Scholar] [CrossRef]
- Bajgain, K.T.; Badal, S.; Bajgain, B.B.; Santana, M.J. Prevalence of comorbidities among individuals with COVID-19: A rapid review of current literature. Am. J. Infect. Control. 2021, 49, 238–246. [Google Scholar] [CrossRef]
- Yang, J.; Zheng, Y.; Gou, X.; Pu, K.; Chen, Z.; Guo, Q.; Ji, R.; Wang, H.; Wang, Y.; Zhou, Y. Prevalence of comorbidities and its effects in patients infected with SARS-CoV-2: A systematic review and meta-analysis. Int. J. Infect. Dis. 2020, 94, 91–95. [Google Scholar] [CrossRef] [PubMed]
- Epidemiology Working Group for NCIP Epidemic Response; Chinese Center for Disease Control and Prevention. The epidemiological characteristics of an outbreak of 2019 novel coronavirus diseases (COVID-19) in China. Chin. J. Epidemiol. 2020, 41, 145–151. [Google Scholar]
- World Health Organization. Rapid Assessment of Service Delivery for NCDs during the COVID-19 Pandemic. 1 June 2020. Available online: https://www.who.int/publications/m/item/rapid-assessment-of-service-delivery-for-ncds-during-the-covid-19-pandemic (accessed on 3 June 2022).
- Figueroa, J.D.; Gray, E.; Pashayan, N.; Deandrea, S.; Karch, A.; Vale, D.B.; Elder, K.; Procopio, P.; Ravesteyn, N.T.; Mutabi, M.; et al. The impact of the Covid-19 pandemic on breast cancer early detection and screening. Prev. Med. 2021, 151, 106585. [Google Scholar] [CrossRef] [PubMed]
- Doubova, S.V.; Leslie, H.H.; Kruk, M.E.; Pérez-Cuevas, R.; Arsenault, C. Disruption in essential health services in Mexico during COVID-19: An interrupted time series analysis of health information system data. BMJ Glob. Health 2021, 6, e006204. [Google Scholar] [CrossRef] [PubMed]
- Kozloff, N.; Mulsant, B.H.; Stergiopoulos, V.; Voineskos, A.N. The COVID-19 Global Pandemic: Implications for People with Schizophrenia and Related Disorders. Schizophr. Bull. 2020, 46, 752–757. [Google Scholar] [CrossRef] [PubMed]
- Triki, C.C.; Leonardi, M.; Mallouli, S.Z.; Cacciatore, M.; Karlshoej, K.C.; Magnani, F.G.; Newton, C.R.; Pilotto, A.; Saylor, D.; Westenberg, E.; et al. Global survey on disruption and mitigation of neurological services during COVID-19: The perspective of global international neurological patients and scientific associations. J. Neurol. 2022, 269, 26–38. [Google Scholar] [CrossRef]
- National Health Commission of the People’s Republic of China. China Health Statistics Yearbook; Peking Union Medical College Press: Beijing, China, 2021.
- Xiao, H.; Dai, X.; Wagenaar, B.H.; Liu, F.; Augusto, O.; Guo, Y.; Unger, J.M. The impact of the COVID-19 pandemic on health services utilization in China: Time-series analyses for 2016–2020. Lancet Reg. Health West. Pac. 2021, 9, 100122. [Google Scholar] [CrossRef]
- Zhang, Y.N.; Chen, Y.; Wang, Y.; Li, F.; Pender, M.; Wang, N.; Yan, F.; Ying, X.H.; Tang, S.L.; Fu, C.W. Reduction in healthcare services during the COVID-19 pandemic in China. BMJ Glob. Health 2020, 5, e003421. [Google Scholar] [CrossRef]
- Wong, S.Y.S.; Zhang, D.; Sit, R.W.S.; Yip, B.H.K.; Chung, R.Y.N.; Wong, C.K.M.; Chan, D.C.C.; Sun, W.; Kwok, K.O.; Mercer, S.W. Impact of COVID-19 on loneliness, mental health, and health service utilisation: A prospective cohort study of older adults with multimorbidity in primary care. Br. J. Gen. Pract. 2020, 70, e817–e824. [Google Scholar] [CrossRef]
- Woolson, R.F. Wilcoxon signed-rank test. In Wiley Encyclopedia of Clinical Trials; Wiley: Hoboken, NJ, USA, 2007; pp. 1–3. [Google Scholar]
- Moynihan, R.; Sanders, S.; Michaleff, Z.A.; Scott, A.M.; Clark, J.; To, E.J.; Jones, M.; Kitchener, E.; Fox, M.; Johansson, M.; et al. Impact of COVID-19 pandemic on utilisation of healthcare services: A systematic review. BMJ Open 2021, 11, e045343. [Google Scholar] [CrossRef]
- Modesti, P.A.; Wang, J.; Damasceno, A.; Agyemang, C.; Van Bortel, L.; Persu, A.; Zhao, D.; Jarraya, F.; Marzotti, I.; Bamoshmoosh, M.; et al. Indirect implications of COVID-19 prevention strategies on non-communicable diseases. BMC Med. 2020, 18, 256. [Google Scholar] [CrossRef]
- Madhuripan, N.; Cheung, H.M.; Cheong, L.H.A.; Jawahar, A.; Willis, M.H.; Larson, D.B. Variables Influencing Radiology Volume Recovery During the Next Phase of the Coronavirus Disease 2019 (COVID-19) Pandemic. J. Am. Coll. Radiol. 2020, 17, 855–864. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.; Wang, S.; Yu, K. COVID-19 Infection Epidemic: The Medical Management Strategies in Heilongjiang Province, China. Crit Care 2020, 24, 107. [Google Scholar] [CrossRef] [PubMed]
- Kraemer, M.U.; Yang, C.H.; Gutierrez, B.; Wu, C.H.; Klein, B.; Pigott, D.M.; Open COVID-19 Data Working Group; Plessis, L.; Faria, N.R.; Li, R.; et al. The effect of human mobility and control measures on the COVID-19 epidemic in China. Science 2020, 368, 493–497. [Google Scholar] [CrossRef] [PubMed]
- Zou, P.; Huo, D.; Li, M. The impact of the COVID-19 pandemic on firms: A survey in Guangdong Province, China. Glob. Health Res. Policy 2020, 5, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Blumenthal, D.; Fowler, E.J.; Abrams, M.; Collins, S.R. COVID-19—Implications for the Health Care System. N. Engl. J. Med. 2020, 383, 1483–1488. [Google Scholar] [CrossRef] [PubMed]
- Che, L.; Du, H.; Chan, K.W. Unequal pain: A sketch of the impact of the Covid-19 pandemic on migrants’ employment in China. Eurasian Geogr. Econ. 2020, 61, 448–463. [Google Scholar] [CrossRef]
- Qian, Y.; Fan, W. Who loses income during the COVID-19 outbreak? Evidence from China. Res. Soc. Stratif. Mobil. 2020, 68, 100522. [Google Scholar] [CrossRef]
- National Healthcare Security Administration. Notice of the National Healthcare Security Administration on Optimizing Medical Insurance Services and Promoting the COVID-19 Prevention and Control. 2 February 2020. Available online: http://www.nhsa.gov.cn/art/2020/2/2/art_37_2325.html (accessed on 3 June 2022).
- National Health Commission of the People’s Republic of China. Notice of the National Health Commission on Strengthening the Management of Health Services and Meeting the Essential Health Needs during the Prevention and Control of the COVID-19 Pandemic. 17 February 2020. Available online: http://www.nhc.gov.cn/yzygj/s7659/202002/6d5a8556c5ce46368263711698d8237a.shtml (accessed on 3 June 2022).
- National Health Commission of the People’s Republic of China. Notice of the National Health Commission on Utilising Internet-based Diagnosis and Consultation Health Services during the Prevention and Control of the COVID-19 Pandemic. 7 February 2020. Available online: http://www.nhc.gov.cn/yzygj/s7653p/202002/ec5e345814e744398c2adef17b657fb8.shtml (accessed on 3 June 2022).
- National Healthcare Security Administration and National Health Commission. Guidance of National Healthcare Security Administration and National Health Commission on the Implementation of “Internet Plus” Medical Insurance Services during the Prevention and Control of the COVID-19 Pandemic. 2 March 2020. Available online: http://www.nhsa.gov.cn/art/2020/3/2/art_37_2750.html (accessed on 3 June 2022).
- National Health Commission of the People’s Republic of China. Pilot Guideline for Primary Healthcare Facilities to Provide Health Services for the Elderly and Chronic Disease Patients during the Prevention and Control of the COVID-19 Pandemic. 24 February 2020. Available online: http://www.gov.cn/zhengce/zhengceku/2020-02/26/content_5483427.htm (accessed on 3 June 2022).
- The Financial World. Jingdong Health Launched the “Chronic Disease Care Plan” with a Number of Well-Known Pharmaceutical Companies to Meet the Essential Drug Needs in Patients with Chronic Disease during the Prevention and Control of the COVID-19 Pandemic. 9 February 2020. Available online: https://baijiahao.baidu.com/s?id=1658042416990306847&wfr=spider&for=pc (accessed on 5 June 2022).
- Zhou, Y.; Dai, G.; Zhang, K.; Huang, J.; Shen, Y.; Ma, B.; Wang, H.; Sun, J. Analysis of the changes of patterns of access to medicines of the patients with common chronic diseases after experiencing the COVID-19 epidemic in Beijing. Chin. J. Pharmacoepidemiol. 2021, 30, 326–334. [Google Scholar]
- Joint Prevention and Control Mechanism of China’s State Council. Notice on Promoting the Restoration of Essential Health Services by Division and Classification. 20 March 2020. Available online: http://www.nhc.gov.cn/yzygj/s7659/202003/c24669ab06324ad080ef7282cd26cf0a.shtml (accessed on 3 June 2022).
- World Health Organization. COVID-19 Continues to Disrupt Essential Health Services in 90% of Countries. 23 April 2021. Available online: https://www.who.int/news/item/23-04-2021-covid-19-continues-to-disrupt-essential-health-services-in-90-of-countries (accessed on 20 November 2022).
- He, Y.; Li, M.; Zhong, Q.; Li, Q.; Yang, R.; Lin, J.; Zhang, X. The Chinese Government’s Response to the Pandemic: Measures, Dynamic Changes, and Main Patterns. Healthcare 2021, 9, 1020. [Google Scholar] [CrossRef]

| All Respondents (N = 4744) | Respondents Reporting No Impact (N = 2277) | Respondents Reporting Impact (N = 2467) | z | p | ||||
|---|---|---|---|---|---|---|---|---|
| Frequency | Percentage | Frequency | Percentage | Frequency | Percentage | |||
| Age (Mean ± SD) | 31.88 | 11.44 | 32.06 | 11.63 | 31.72 | 11.25 | 0.504 | 0.615 |
| Gender | 1.103 | 0.294 | ||||||
| Male | 2319 | 48.88% | 1095 | 47.22% | 1224 | 52.78% | ||
| Female | 2425 | 51.12% | 1182 | 48.74% | 1243 | 51.26% | ||
| Education level | 9.973 | 0.019 * | ||||||
| Primary school or below | 49 | 1.03% | 32 | 65.31% | 17 | 34.69% | ||
| Middle high school | 499 | 10.52% | 228 | 45.69% | 271 | 54.31% | ||
| Senior high school | 1256 | 26.48% | 578 | 46.02% | 678 | 53.98% | ||
| Undergraduate or above | 2940 | 61.97% | 1439 | 48.95% | 1501 | 51.05% | ||
| Employment status | 5.643 | 0.060 | ||||||
| Employed | 3072 | 64.76% | 1446 | 47.07% | 1626 | 52.93% | ||
| Retired | 122 | 2.57% | 52 | 42.62% | 70 | 57.38% | ||
| Non-employed | 1550 | 32.67% | 779 | 50.26% | 771 | 49.74% | ||
| Marital status | 5.900 | 0.015 * | ||||||
| Non-married | 2070 | 43.63% | 1035 | 50.00% | 1035 | 50.00% | ||
| Married | 2674 | 56.37% | 1242 | 46.45% | 1432 | 53.55% | ||
| Household registration | ||||||||
| Urban | 2804 | 59.11% | 1302 | 46.43% | 1502 | 53.57% | 6.718 | 0.010 * |
| Rural | 1940 | 40.89% | 975 | 50.26% | 965 | 49.74% | ||
| Annual household income in 2019 (RMB) | 2.579 | 0.631 | ||||||
| ≤50,000 | 1098 | 23.15% | 531 | 48.36% | 567 | 51.64% | ||
| 50,000–100,000 | 1483 | 31.26% | 687 | 46.33% | 796 | 53.67% | ||
| 100,000–200,000 | 1305 | 27.51% | 640 | 49.04% | 665 | 50.96% | ||
| 200,000–500,000 | 605 | 12.75% | 294 | 48.60% | 311 | 51.40% | ||
| >500,000 | 253 | 5.33% | 125 | 49.41% | 128 | 50.59% | ||
| Annual household medical expenses in 2019 (RMB) | 23.139 | 0.000 *** | ||||||
| ≤1000 | 1234 | 26.01% | 654 | 53.00% | 580 | 47.00% | ||
| 1000–10,000 | 2435 | 51.33% | 1158 | 47.56% | 1277 | 52.44% | ||
| 10,000–50,000 | 841 | 17.73% | 370 | 44.00% | 471 | 56.00% | ||
| 50,000–100,000 | 163 | 3.44% | 67 | 41.10% | 96 | 58.90% | ||
| >100,000 | 71 | 1.50% | 28 | 39.44% | 43 | 60.56% | ||
| Chronic disease | 19.677 | 0.000 *** | ||||||
| No | 4313 | 90.91% | 2114 | 49.01% | 2199 | 50.99% | ||
| Yes | 431 | 9.09% | 163 | 37.82% | 268 | 62.18% | ||
| Frequently visited medical institution | 6.283 | 0.280 | ||||||
| Township health centre | 719 | 15.16% | 367 | 51.04% | 352 | 48.96% | ||
| Community health centre | 783 | 16.51% | 363 | 46.36% | 420 | 53.64% | ||
| County-level medical institution | 1232 | 25.97% | 594 | 48.21% | 638 | 51.79% | ||
| Municipal medical institution | 1310 | 27.61% | 636 | 48.55% | 674 | 51.45% | ||
| Provincial medical institution | 686 | 14.46% | 312 | 45.48% | 374 | 54.52% | ||
| Other medical institution | 14 | 0.30% | 5 | 35.71% | 9 | 64.29% | ||
| Time to browse information related to the pandemic per-day | 62.115 | 0.000 *** | ||||||
| Irregular | 771 | 16.25% | 444 | 57.59% | 327 | 42.41% | ||
| Less than 1 h | 819 | 17.26% | 401 | 48.96% | 418 | 51.04% | ||
| 1–2 h | 2124 | 44.77% | 1030 | 48.49% | 1094 | 51.51% | ||
| More than 3 h | 1030 | 21.71% | 402 | 39.03% | 628 | 60.97% | ||
| Perception of COVID-19 infection risk | 252.629 | 0.000 *** | ||||||
| Very low | 933 | 19.67% | 572 | 61.31% | 361 | 38.69% | ||
| Fairly low | 1784 | 37.61% | 979 | 54.88% | 805 | 45.12% | ||
| Slightly high | 859 | 18.11% | 357 | 41.56% | 502 | 58.44% | ||
| Fairly high | 672 | 14.17% | 242 | 36.01% | 430 | 63.99% | ||
| Very high | 496 | 10.46% | 127 | 25.60% | 369 | 74.40% | ||
| Perception of the health impact of the pandemic | 690.549 | 0.000 *** | ||||||
| Nearly no | 1944 | 40.98% | 1354 | 69.65% | 590 | 30.35% | ||
| Some | 2043 | 43.06% | 773 | 37.84% | 1270 | 62.16% | ||
| Significant | 757 | 15.96% | 150 | 19.82% | 607 | 80.18% | ||
| Anxiety/depression during the pandemic | 266.151 | 0.000 *** | ||||||
| No | 2311 | 48.71% | 1366 | 59.11% | 945 | 40.89% | ||
| Occasional | 1991 | 41.97% | 808 | 40.58% | 1183 | 59.42% | ||
| Frequent | 442 | 9.32% | 103 | 23.30% | 339 | 76.70% | ||
| Variables | OR | SE | z | p > z | 95% CI | |
|---|---|---|---|---|---|---|
| Age | 0.99 | 0.004 | −1.250 | 0.210 | 0.99 | 1.00 |
| Gender (Reference: Male) | ||||||
| Female | 0.99 | 0.066 | −0.220 | 0.823 | 0.86 | 1.12 |
| Education level (Reference: Primary school or below) | ||||||
| Middle high school | 2.42 | 0.828 | 2.570 | 0.010 * | 1.23 | 4.73 |
| Senior high school | 2.17 | 0.737 | 2.280 | 0.023 * | 1.11 | 4.22 |
| Undergraduate or above | 2.06 | 0.702 | 2.120 | 0.034 * | 1.06 | 4.02 |
| Employment (Reference: Employed) | ||||||
| Retired | 1.15 | 0.264 | 0.590 | 0.557 | 0.73 | 1.80 |
| Non-employed | 0.97 | 0.080 | −0.370 | 0.708 | 0.82 | 1.14 |
| Marital status (Reference: Non-married) | ||||||
| Married | 1.28 | 0.114 | 2.820 | 0.005 ** | 1.08 | 1.53 |
| Household registration (Reference: Urban) | ||||||
| Rural | 0.89 | 0.068 | −1.570 | 0.117 | 0.76 | 1.03 |
| Annual household income in 2019 (Reference: ≤50,000 RMB) | ||||||
| 50,000–100,000 | 0.99 | 0.093 | −0.150 | 0.881 | 0.82 | 1.19 |
| 100,000–200,000 | 0.84 | 0.087 | −1.720 | 0.085 | 0.68 | 1.02 |
| 200,000–500,000 | 0.91 | 0.116 | −0.700 | 0.483 | 0.71 | 1.17 |
| >500,000 | 0.93 | 0.161 | −0.420 | 0.674 | 0.66 | 1.31 |
| Annual household medical expenses in 2019 (Reference: ≤1000 RMB) | ||||||
| 1000–10,000 | 1.10 | 0.089 | 1.160 | 0.245 | 0.94 | 1.29 |
| 10,000–50,000 | 1.06 | 0.112 | 0.540 | 0.586 | 0.86 | 1.30 |
| 50,000–100,000 | 1.17 | 0.226 | 0.800 | 0.426 | 0.80 | 1.70 |
| >100,000 | 1.07 | 0.304 | 0.230 | 0.822 | 0.61 | 1.86 |
| Chronic disease (Reference: No) | ||||||
| Yes | 1.27 | 0.155 | 1.980 | 0.048 * | 1.00 | 1.62 |
| Frequently visited medical institution (Reference: Township health centre) | ||||||
| Community health centre | 1.29 | 0.151 | 2.180 | 0.029 * | 1.03 | 1.62 |
| County-level medical institution | 1.18 | 0.128 | 1.520 | 0.129 | 0.95 | 1.46 |
| Municipal medical institution | 1.10 | 0.125 | 0.870 | 0.387 | 0.88 | 1.38 |
| Provincial medical institution | 1.34 | 0.180 | 2.180 | 0.029 * | 1.03 | 1.74 |
| Other medical institution | 2.63 | 1.635 | 1.560 | 0.119 | 0.78 | 8.90 |
| Time to browse information related to the pandemic per-day (Reference: Irregular) | ||||||
| Less than 1 h | 1.33 | 0.148 | 2.530 | 0.011 * | 1.07 | 1.65 |
| 1–2 h | 1.09 | 0.104 | 0.940 | 0.346 | 0.91 | 1.32 |
| More than 3 h | 1.34 | 0.146 | 2.730 | 0.006 * | 1.09 | 1.66 |
| Perception of COVID-19 infection risk (Reference: Very low) | ||||||
| Fairly low | 1.15 | 0.104 | 1.600 | 0.110 | 0.97 | 1.38 |
| Slightly high | 1.43 | 0.153 | 3.320 | 0.001 ** | 1.16 | 1.76 |
| Fairly high | 1.63 | 0.190 | 4.220 | 0.000 *** | 1.30 | 2.05 |
| Very high | 2.09 | 0.287 | 5.370 | 0.000 *** | 1.60 | 2.73 |
| Perception of the health impact of the pandemic (Reference: Nearly no) | ||||||
| Some | 3.14 | 0.228 | 15.720 | 0.000 *** | 2.72 | 3.62 |
| Significant | 6.24 | 0.716 | 15.960 | 0.000 *** | 4.98 | 7.82 |
| Anxiety/depression during the pandemic (Reference: No) | ||||||
| Occasional | 1.39 | 0.098 | 4.670 | 0.000 *** | 1.21 | 1.59 |
| Frequent | 1.80 | 0.243 | 4.330 | 0.000 *** | 1.38 | 2.34 |
| N | November to December 2019 | January to February 2020 | Z | p | |
|---|---|---|---|---|---|
| Total medical expenses | 236 | 1975 (500–5000) | 1000 (300–3000) | 5.061 | 0.000 *** |
| Out-of-pocket medical expenses | 236 | 500 (200–2000) | 412 (100–1300) | 4.372 | 0.000 *** |
| Drug expenses | 236 | 600 (300–2000) | 500 (100–1000) | 4.508 | 0.000 *** |
| Out-of-pocket drug expenses | 236 | 300 (100–1000) | 228 (50–790) | 2.760 | 0.006 ** |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wei, X.; Yuan, H.; Sun, Y.; Zhang, J.; Wang, Q.; Fu, Y.; Wang, Q.; Sun, L.; Yang, L. Health Services Utilization in China during the COVID-19 Pandemic: Results from a Large-Scale Online Survey. Int. J. Environ. Res. Public Health 2022, 19, 15892. https://doi.org/10.3390/ijerph192315892
Wei X, Yuan H, Sun Y, Zhang J, Wang Q, Fu Y, Wang Q, Sun L, Yang L. Health Services Utilization in China during the COVID-19 Pandemic: Results from a Large-Scale Online Survey. International Journal of Environmental Research and Public Health. 2022; 19(23):15892. https://doi.org/10.3390/ijerph192315892
Chicago/Turabian StyleWei, Xia, Haowen Yuan, Yan Sun, Jiawei Zhang, Qingbo Wang, Yaqun Fu, Quan Wang, Li Sun, and Li Yang. 2022. "Health Services Utilization in China during the COVID-19 Pandemic: Results from a Large-Scale Online Survey" International Journal of Environmental Research and Public Health 19, no. 23: 15892. https://doi.org/10.3390/ijerph192315892
APA StyleWei, X., Yuan, H., Sun, Y., Zhang, J., Wang, Q., Fu, Y., Wang, Q., Sun, L., & Yang, L. (2022). Health Services Utilization in China during the COVID-19 Pandemic: Results from a Large-Scale Online Survey. International Journal of Environmental Research and Public Health, 19(23), 15892. https://doi.org/10.3390/ijerph192315892







